Abstract
The purpose of this paper is to review both main findings and secondary analyses from studies of abstinence incentives conducted in the National Drug Abuse Treatment Clinical Trials Network (CTN). Previous research has supported the efficacy of tangible incentives provided contingent on evidence of recent drug abstinence. CTN conducted the first multi-site effectiveness trial of this novel intervention. Study participants were stimulant abusers (N = 803) participating in treatment at 14 clinical sites and randomly assigned to treatment as usual (TAU) with or without a prize draw incentive program. Study participants could earn up to $400 over 3 months for submission of drug- urine and breath (BAL) specimens. 3-month retention was significantly improved by incentives offered to psychosocial counseling clients (50% incentive vs 35% control retained) while on-going stimulant drug use was significantly reduced in methadone maintenance clients (54.4% incentive vs 38.7% control samples testing stimulant negative). In both settings, duration of continuous abstinence achieved was improved in the incentive condition. These studies support effectiveness of one abstinence incentive intervention and highlight the different outcomes that can be expected with application in methadone maintenance versus psychosocial counseling treatment settings. Secondary analyses have shown the importance of early treatment positive versus negative urine screens in moderating the outcome of abstinence incentives and have explored both safety and cost-effectiveness of the intervention. Implications for the use of motivational incentive methods in clinical practice are discussed.
Introduction
The National Drug Abuse Treatment Clinical Trials Network (CTN) has supported several important lines of research during its 10 year history in an effort to identify clinical interventions, originally developed and tested in small-scale research studies, that are effective when implemented in real world clinic settings. This paper reviews one such line of research, that investigating the impact of abstinence-contingent incentives on the clinical outcomes of stimulant abusers. The use of contingent incentives is especially relevant for stimulant abusers, as there is no medication yet identified to aid in the treatment of this disorder. Thus, treatment relies exclusively on behavioral interventions and findings have important implications for interventions with this large group of drug abusers. Main findings on effectiveness from the CTN studies of abstinence incentives in stimulant abusers have also been greatly enriched by secondary analyses conducted with the data. These analyses have examined predictors of outcome, effectiveness in special populations such as methamphetamine users, differential impact in those with more versus less severe drug use at study intake and potential adverse side-effects of the intervention. This paper brings together all the research on abstinence incentives for stimulant users conducted in the CTN and examines clinical implications of the findings. The paper should be useful both to researchers who can formulate additional questions based on CTN study findings and to clinicians who may find important practice implications that if adopted, could improve treatment outcomes.
History of Contingency Management Research
Contingency management is a modern approach to behavior change that is grounded in the well-established learning principles of operant conditioning, as originally formulated by B.F. Skinner (Skinner, 1938). The application of contingency management to the treatment of drug abuse dates back to at least the mid 1970's, when small sample demonstration studies were conducted with drug abuse treatment clients who displayed on-going use of illicit drugs (opioids, stimulants or benzodiazepines) during methadone maintenance treatment (Stitzer, Bigelow & Liebson, 1979, 1980; Stitzer, Bigelow, Liebson & Hawthorne, 1982). In these studies, participants were offered tangible incentives based on evidence of recent abstinence from their identified on-going drug of abuse. At least temporary discontinuation of this use was clearly demonstrated as a result. The approach began to receive greater attention during the 1990's after publication of convincing research findings that demonstrated the efficacy of abstinence-based incentives in the treatment of primary stimulant abusers (Higgins, Budney, Bickel, Hughes, Foerg, & Badger, 1993; Higgins, Budney, Bickel, Foerg Donham, & Badger, 1994; Higgins, Wong, Badger, Ogden, & Dantona, 2000). This was an especially important advance because stimulant abuse was then and remains a condition whose treatment is reliant on behavioral interventions due to the absence of efficacious medications.
The original research with stimulant abusers conducted by Higgins and colleagues (1993, 1994) utilized a voucher incentive protocol in which points with cash value were awarded upon submission of stimulant negative urines. The points could then be traded for tangible goods selected by eligible clients and purchased by treatment staff. This voucher reinforcement intervention as originally implemented, was highly efficacious (see Luissier, Heil, Mongeon, Badger, & Higgins, 2006) but costly both in value of the goods offered as reinforcers and in staff time needed for coordination and individualized purchase of reinforcers.
A second protocol for reinforcement of recent abstinence devised by Petry (Petry, Martin, Coony & Kranzler, 2000) utilized principles of intermittent reinforcement that could potentially reduce the cost of abstinence incentive interventions. In this procedure, clients could draw tickets from a bowl when they submitted a drug negative specimen. Some of the tickets (usually 50%) indicated that a prize had been won but the value of the prize varied, with smaller prizes (worth about $1) more likely than larger prizes (usually worth about $20). In addition, a single ticket was included indicating that a “jumbo” prize, usually worth $80-$100, had been won. By changing the value and probability of prize wins, this system has a great deal of flexibility for altering the overall cost of a reinforcement program.
The prize draw system is consistent with operant principles of reinforcement in that considerable amounts of behavior (in this case, sustained abstinence) can generally be supported by delivery of intermittent tangible reinforcement. Reinforcing potency of the intervention may be enhanced by having a stock of desirable prizes on visible display at the treatment program so that clients can readily see the prizes they are “working for”.
Research using the prize draw system with stimulant users demonstrated efficacy in that the intervention produced increased durations of sustained abstinence when total possible value of prizes to be won was around $250-$400 in an 8-12 week intervention (Petry & Martin, 2002; Petry, Tedford, Austin, Nich, Carroll, & Rounsaville, 2004). This is considerably less monetary value than had been offered in previous voucher reinforcement programs, a feature that makes the approach potentially appealing to clinicians. Thus, several contingency management procedures had been developed and well researched before the CTN began to select interventions for effectiveness research. Further, considerable amounts of data had been amassed supporting efficacy of these interventions in relation to usual care or other comparison conditions.
The CTN Motivational Incentives study
Because of the substantial research base extant in the scientific literature demonstrating efficacy of an abstinence incentive approach, contingency management treatments were well poised for adoption by the CTN in fulfillment of their mission to research effectiveness of evidence-based practices when implemented in real world community based treatment programs. Thus, two of the first CTN multi-site studies developed (CTN 0006 and 0007) were titled MIEDAR, an acronym for Motivational Incentives to Enhance Drug Abuse Recovery. The term Motivational Incentives was coined and used rather than Contingency Management to describe the abstinence reinforcement intervention because the former terminology was felt to better capture in clinically relevant parlance the motivational enhancing intent of the interventions.
MIEDAR Methods
Because of its appeal to clinicians, CTN adopted the prize draw procedure in order to test the efficacy of abstinence incentives for improving treatment outcomes of stimulant users. Two parallel protocols were developed and implemented. One enrolled stimulant users newly admitted to outpatient psychosocial counseling programs (N = 8 programs) while the other enrolled stimulant users who had been in treatment at a methadone maintenance program for between 30 days and 3 years (N = 6 programs). The participating programs were regionally diverse and the study sample contained a well- balanced mixture of White and Black racial groups as well as men and women (see Table 1). Furthermore, both cocaine and methamphetamine use was represented among clients from the psychosocial counseling programs (See Table 1).
Table 1.
Miedar Participant Characteristics
| Methadone Maintenance | Psychosocial Counseling | |
|---|---|---|
| N = 388 | N = 415 | |
| Women (%) | 45 | 55 |
| Minority (%)ˆ | 49 | 58 |
| Age (mean years ± SD) | 42 (9) | 36 (9) |
| Education (mean years ± SD) | 12 (2) | 12 (2) |
| Employed at study start (%) | 32 | 35 |
| Probation or parole (%) | 16 | 36 |
| Methadone dose (mean mg ± SD) | 86 (27) | --- |
| Primary methamphetamine abuse (%) | 4 | 27 |
| Time in Tx at study start (mean months) | 9 | 1 |
| First study urine (% stimulant positive) | 75 | 25 |
in both modalities, minority participants were primarily Black (40-50% of entire sample) with a much smaller percentage endorsing Hispanic (12-16% of entire sample) or “other” (7-10% of entire sample) racial categories.
Methods for the MIEDAR study have been extensively described elsewhere (Petry, Peirce, Stitzer, Blaine, Roll, et al., 2005; Peirce, Petry, Stitzer, Blaine, Kellogg, et al., 2006; Stitzer & Kellogg, 2008). In brief, research volunteers were randomly assigned to receive usual care at their participating clinic with or without the abstinence incentives during a 12-week intervention period. All were requested to submit urine samples twice weekly. Control participants received feedback on their urine test results but no consequences. Incentive participants were awarded draws from the prize bowl under an escalating schedule in which number of draws increased by 1 for each consecutive week of stimulant (negative amphetamine, methamphetamine and cocaine) and alcohol (negative BAL) abstinence. Number of draws reset if a positive urine or no urine was submitted during a given week. When they tested negative for stimulants, participants could also receive bonus draws for opioid and marijuana negative urines. In this way, the main emphasis was placed on stimulant abstinence, but abstinence from other important drugs of abuse was also acknowledged and reinforced.
During-treatment outcomes
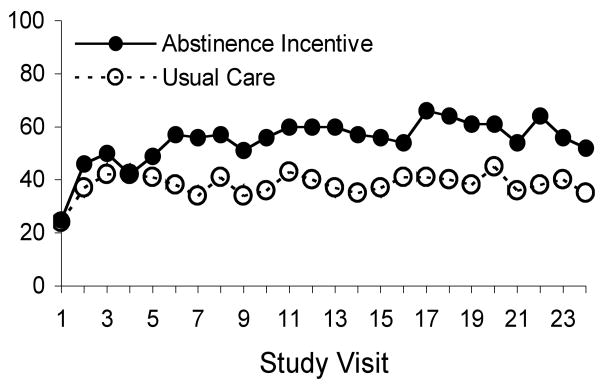
Main results from the studies have been previously published (Petry et al., 2005; Peirce et al, 2006). Results from the two parallel studies highlighted the differences in demographic and drug use profiles as well as impact of abstinence incentive procedures for stimulant users enrolled in methadone maintenance versus psychosocial counseling programs. As had been previously demonstrated (Silverman, Higgins, Brooner, Montoya, Cone, Schuster, & Preston, 1996; Silverman, Robles, Mudric, Bigelow, & Stitzer, 2004), incentives were effective at reducing on-going drug use among methadone maintained stimulant abusers (Peirce et al., 2006). Overall percent of stimulant negative urines was 54.4% for incentive versus 38.7% for control participants (OR = 1.89; CI = 1.35-2.63). GEE analysis with group and time as factors confirmed that the odds of submitting stimulant negative urines during treatment were doubled for incentive as compared to control participants (see Fig. 1).
Figure 1.
Percent of submitted samples testing negative for stimulants and alcohol. Data are shown for stimulant abusers enrolled in methadone maintenance treatment and randomly assigned to receive usual care with (n = 198) or without (n = 190) a prize draw abstinence incentive intervention. The intervention was implemented over a 12-week period with two study visits scheduled per week. from Peirce et al., 2006.
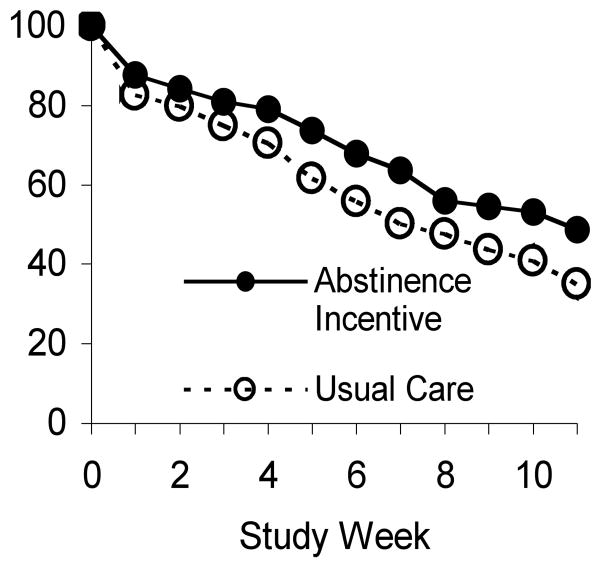
In contrast, there was no direct effect on the proportion of stimulant negative urines for stimulant users enrolled in psychosocial counseling treatment, primarily because very few positive urines were ever submitted. In fact, over 85% of the submitted samples tested negative for drugs, as stimulant abusers who relapse are likely to drop out of psychosocial treatment programs. Instead, the intervention exerted its primary impact on treatment retention and duration of documented during-treatment abstinence. As shown in Fig. 2, the odds of being retained in treatment for 12 weeks were 1.64 times greater for incentive than for control participants (50% versus 35% retained). In addition, longest duration of abstinence achieved was significantly higher among patients randomized to the incentive condition (4.4 weeks versus 2.6 weeks).
Figure 2.
Percent of participants retained. Data are shown for stimulant abusers enrolled in psychosocial counseling treatment and randomly assigned to receive usual care treatment with (n = 209) or without (n = 206) a prize-based abstinence incentive intervention. The intervention was implemented over a 12-week period with two study visits scheduled per week. adapted from Petry et al., 2005
Long-term follow up
Three and six-month follow-ups were conducted as part of the MIEDAR study. In methadone patients, follow-up rates of 81% and 74% at 3- and 6-months, respectively, were considered adequate to support analysis. However, no analyses were conducted for the psychosocial counseling study due to relatively low 6-month follow-up rates (62% incentive, 55% control). In the methadone study (reported at the Annual meeting of the CPDD, 2005), incentive versus control participants showed a statistically significant difference at the 3-month end of treatment evaluation on a stringent measure of abstinence that required submitting a stimulant negative urine and reporting no stimulant use in the 30 days prior to the evaluation. This measure showed 25% incentive versus 15% control participants self-reported and were verified abstinent (p < .01). However, the group difference narrowed somewhat at the 6-month evaluation and was no longer statistically significant (21% vs 15% abstinent; p < .10).
Overall, the CTN MIEDAR study supported the during-treatment effectiveness of one abstinence incentive intervention when used to improve treatment outcomes of stimulant users. This finding was true whether the stimulant users were enrolled in methadone maintenance or psychosocial counseling programs. However, the study findings illustrate the differential impact of incentives that may be expected in these two sub-populations based on the very different patterns of on-going drug use that are typically found. When stimulant use is on-going and robust in the study sample, as frequently seen in methadone maintenance clients, abstinence incentives can be a potent intervention for motivating reductions in this use. In contrast, when on-going stimulant use is infrequent or absent, as frequently seen in psychosocial counseling clientele, incentives can be useful for promoting better treatment retention and prolonging durations of drug-free treatment participation. It should be noted that the conclusions from any particular study apply only to the study conditions and populations used in that study. Thus, different findings might emerge if different schedules or magnitudes of reinforcement were employed or if a different study population was targeted. Additional questions also remain about how the effects of abstinence incentives can be sustained for longer-term impact on recovery of drug users. Nevertheless, the CTN study provided convincing evidence that is consistent with a large body of previous research about the efficacy of abstinence incentives, and that extends previous research to show that these interventions can be highly effective for improving during-treatment outcomes when applied in real world community treatment programs.
Secondary analyses of MIEDAR data: Outcomes and clinical implications
The data-base from large multi-site studies provides an invaluable resource for secondary analysis, and several interesting and important issues have been addressed to date from secondary analyses of the MIEDAR data. These issues include: the correlates of good versus poor outcomes in the study sample, the influence of specific participant clinical characteristics on outcome, the safety of abstinence incentive procedures and their cost-effectiveness.
Effectiveness of incentives in methamphetamine users
Because of the critical importance of identifying effective treatment for methamphetamine users, one of the first questions asked in secondary analysis was whether the MIEDAR abstinence incentives –were effective for users of methamphetamine. This question could be addressed in the psychosocial counseling study due to the substantial number of methamphetamine users enrolled (N = 113; see Table 1). Analysis of the outcome for methamphetamine users showed that the abstinence incentive intervention was indeed effective for improving treatment outcomes in this subgroup (Roll, Petry, Stitzer, Brecht, Peirce, McCann, Blaine, MacDonald, DiMaria, Lucero, & Kellogg, 2006). For example, 12-week retention in treatment was 55% for methamphetamine users assigned to incentive versus 39% for those assigned to usual care control conditions, although this difference did not reach conventional levels of statistical significance in this smaller study subsample (X2=2.95, df=1, p=0.86). Importantly, however, there was a significant difference between incentive and control participants in detected drug use during treatment. Those assigned to abstinence incentives submitted more stimulant and alcohol negative samples (mean = 13.9, SD = 8.8) than did participants receiving usual care treatment (mean = 9.9, SD = 8.0) (t=2.55, df =110, p=0.01) and this significant finding was confirmed by GEE analysis taking time as well as group into account. Additionally, 17.6% of incentive participants versus 6.5% of control participants were abstinent throughout the trial (X2=3.44, df=1, p=.06). Detailed examination of the data suggested that the between group difference was due both to better retention and to submission of fewer methamphetamine positive samples during treatment in the incentive compared to control participants.
Correlates of treatment outcome
An important exploratory analysis for any treatment outcome study is an examination of the client or treatment variables that are associated with good versus poor outcomes. One secondary analysis (Killeen, Carter, Copersino, Petry & Stitzer, 2007) showed that incentives were equally effective in psychosocial counseling participants with and without a more extensive (>1 episode) history of drug abuse treatment. A comprehensive predictor analysis was also conducted (Peirce, Petry, Roll, Kolodner, Krasnansky, Stabile, Brown & Stitzer, 2009) that included 775 study participants (those with missing data excluded) from both methadone and psychosocial counseling treatment modalities. Twenty-three variables, whose selection was based on a priori hypotheses regarding indicators of drug use severity, were entered simultaneously into the full regression model. The variables entered included treatment modality and study condition, a variety of demographic features (e.g. age, gender, race, employment and marital status), and indicators of criminal justice involvement (currently on parole or probation), of current psychiatric distress (from Brief Symptom Inventory Global Symptom Index) and of drug use status at treatment entry (urine positive versus negative for stimulant drugs). The dependent variable was the number of stimulant and alcohol negative samples submitted during the 12-week study.
The results of the analysis were striking and clear. The single most powerful predictor of outcome was drug use status at start of treatment with those submitting urine sample testing positive for stimulants having significantly poorer outcome than those submitting stimulant negative urines at study entry (B = -7.93; p < .001). Further, this relationship held when stratified analyses were conducted for the two treatment modalities separately, despite a substantial and dramatic difference in percent of participants submitting a stimulant positive urine sample at study entry (25% of psychosocial counseling participants versus 75% of methadone maintenance participants). Cannabis positive urine at study intake predicted poorer outcomes in both modalities (full sample B = -3.37, p < .001). Other associations noted were smaller in magnitude and modality-specific. Higher psychiatric severity was associated with poorer outcome (B = -2.03; P < .05) and endorsement of “usually employed” with better outcome (B = 1.96; p < .025) in psychosocial counseling participants. Endorsement of both “currently employed” (B = -2.31; p < .015) and “living with another drug user” (B = -1.76; p < .036) were associated with poorer outcomes in methadone maintenance participants.
Drug use at study entry: Interaction with incentive interventions
The finding that treatment outcome is powerfully predicted by drug use versus abstinence detected at treatment entry is not a new observation. Rather, this relationship has been previously noted in a variety of treatment contexts (Alterman, Kampman, Boardman, Cacciola, Rutherford, McKay & Maany, 1997; Alterman, McKay, Mulvaney, & McLellan, 1996; Ehrman, Robbins & Cornish, 2001; Petry et al., 2004; Petry, Alessi, Marx, Austin & Tardif, 2005; Petry, Alessi, Carroll, Hanson, MacKinnon, Rounsaville & Sierra, 2006; Sofuoglu, Gonzalez, Poling & Kosten, 2003). Nevertheless, the MIEDAR study provided the opportunity to extend analyses in order to determine whether this clinical prognostic factor interacts with incentive interventions or operates independently of them. For example, it may be that incentives are able to remediate or reverse the generally poor prognosis conferred by drug use at entry.
Two parallel analyses were conducted using data from methadone maintenance (Stitzer, Peirce, Petry, Kriby, Roll, Krasnansky, Cohen, Blaine, Vandrey, Kolodner & Li, 2007) and psychosocial counseling (Stitzer, Petry, Peirce, Kirby, Killeen, Roll, Hamilton, Stabile, Sterling, Brown, Kolodner & Li, 2007) samples. An independent analysis by modality is consistent with the very different outcome patterns produced by abstinence incentives in the two modalities, as previously discussed. Analyses indicated that incentives (urine positive versus negative at treatment entry) in methadone maintenance clients were effective independent of drug use status. That is, outcomes were improved both for those who entered the study with stimulant positive (N = 292) and negative (N = 94) urines although the magnitude of the effect appears greater for the stimulant negative participants (Figure 3). In contrast, as shown in Figure 4, incentives improved outcomes only for those entering psychosocial counseling treatment with a stimulant negative urine sample (n = 306) but not for the smaller subgroup entering the study with a stimulant positive urine (n = 108).
Figure. 3.
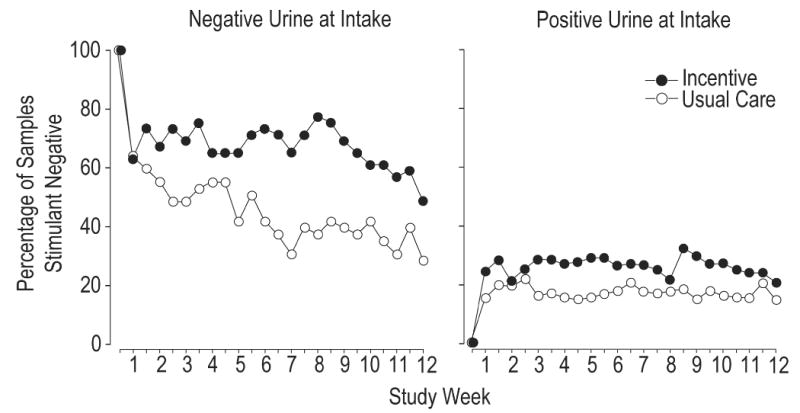
Percent of stimulant and alcohol negative samples submitted at each of 24 study visits during a 12-week intervention with missing samples coded as positive. Data is shown separately for methadone maintained participants who tested stimulant negative (left-hand panel; N = 94) versus stimulant positive (right-hand panel; N = 292) at study intake. Data in each panel is shown separately for participants exposed to usual care with (closed symbols) or without (open symbols) an added prize draw abstinence incentive procedure. from Stitzer, Peirce, et al., 2007.
Figure 4.
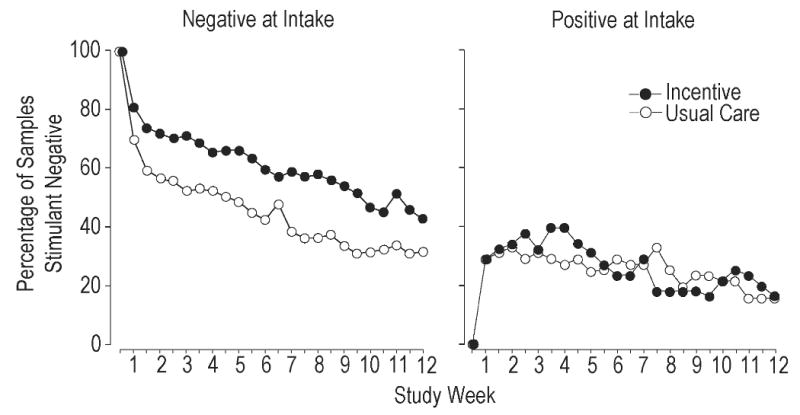
Percent of stimulant and alcohol negative samples submitted at each of 24 study visits during a 12-week intervention with missing samples coded as positive. Data is shown separately for psychosocial counseling participants who tested stimulant negative (left-hand panel; N = 306) versus stimulant positive (right-hand panel; N = 108) at study intake. Data in each panel is shown separately for participants exposed to usual care with (closed symbols) or without (open symbols) an added prize draw abstinence incentive procedure. from Stitzer, Petry, et al., 2007.
These findings have important implications for clinical practice. They highlight the importance of conducting urine drug screens at treatment intake. Further, they suggest that abstinence incentives may be usefully offered to all stimulant abusing methadone maintenance clients. However, finding suggest that different interventions may be needed to engage the minority of psychosocial counseling clients who are actively using drugs at treatment entry versus the larger number who have, for whatever reason and duration, achieved abstinence prior to treatment and require primarily relapse prevention services. Again, it should be noted that these conclusions could depend on the particular abstinence incentive intervention used and that potentially different findings might emerge if a different schedule or magnitude of abstinence reinforcement had been employed or a different population studied.
Monitoring of Serious Adverse Events (SAE's)
Clinical trials of behavioral and psychosocial interventions are generally required to take strict precautions in order to safeguard the protection of human subjects. Because there are no tailored guidelines for safety standards in behavioral trials, these studies adhere to the general human subjects protection guidelines developed and utilized for pharmaceutical clinical trials. Specifically, these requirements involve detailed tracking of any medical adverse event, particularly serious adverse events, defined as events requiring hospitalization or extension of a current hospitalization. Thus, detailed reporting and follow-up to resolution is required for any hospitalization, even if the reason is not remotely related to study procedures (e.g. hospitalization for delivery of a baby by a participant in a behavioral treatment study). In the case of behavioral studies with drug users, the frequency of medical adverse events may be relatively high due to the chaotic lifestyle, poor nutrition, inadequate primary medical care, exposure to violence and other untoward factors inherent in the lifestyles of many drug users. This necessitates substantial expenditure of study staff time and effort to conduct adverse event tracking and reporting. This point was highlighted in a secondary analysis study (Petry, Roll, Rounsaville, Ball, Stitzer, Peirce, Blaine, Kirby, McCarty & Carroll, 2008) that examined serious adverse event data from two types of CTN multi-site trials (Ball et al., 2007; Carroll et al., 2006; Pierce et al., 2006; Petry et al., 2005) enrolling a combined total of 1,687 participants with a total of 27,198 person-weeks of follow-up. The study found that 12% of participants experienced one or more serious adverse events (SAE's) for a total of 260 SAE's. None were judged by the data and safety monitoring board for these studies to be study-related and there was no significant difference in SAE incidence between experimental and control study arms. These data provide an important perspective. They demonstrate the high incidence of SAE's that may be expected in studies that enroll drug users. Further, they underscore the need to reconsider the rationale behind, and appropriate methods for, monitoring medical safety parameters during behavioral and psychosocial therapy trials in general and such studies conducted in populations of drug users in particular.
Gambling behavior
In addition to consideration of appropriate medical safety monitoring criteria, it is also important to understand safety outcome for any specific study-related harms that may be present. During development of the MIEDAR project, a clinical concern was raised that the prize draw procedure might stimulate gambling behavior due to the elements of chance involved in the procedure. To address this concern, the protocol specified that any treatment clients currently in recovery from a gambling problem be excluded, although no such individuals were detected. In addition, the study collected data on gambling behavior at baseline and at 1, 3 and 6-month follow-up time points. Analysis of these data (Petry, Kolodner, Li, Peirce, Roll, Stitzer & Hamilton, 2006) found that the percentage of study participants who reported any gambling behavior in the past 30 days was somewhat higher in methadone maintenance (20-25%) than in psychosocial counseling (13-18%) participants. Among those who did report any gambling, median amounts wagered in the 30 days prior to the study were $10 for psychosocial counseling and $20 for methadone maintenance participants. The percentage reporting gambling as well as median amount wagered remained stable across the follow-up periods, and importantly, there were no differences in gambling behavior among those receiving incentive versus control treatments.
These data on gambling behavior, obtained in the context of procedures used in the CTN MIEDAR study, have been extremely useful for addressing the concerns of clinicians. They highlight the value of collecting data on potential protocol-specific adverse events in any behavioral and psychosocial clinical trials where there are any safety concerns raised. Such data are particularly valuable when there is no data available to judge the importance and validity of concerns raised during the protocol development process.
Cost-effectiveness studies
In addition to efficacy (the treatment can work under ideal circumstances) effectiveness (the treatment does work in a real world setting) and safety support for a new treatment intervention, it is also beneficial to have cost-effectiveness and cost-benefit data in order to judge the utility of more wide-spread adoption in community treatment programs. Data from the MIEDAR study were examined to determine the cost-effectiveness of an incentive program in relation to the added benefits in improved outcome for the psychosocial counseling (Olmstead, Sindelar & Petry, 2007a) and methadone maintenance (Sindelar, Olmstead & Peirce, 2007) samples. Compared to usual care, the incremental cost of using this particular prize-based incentive program to lengthen abstinence duration by 1 week in psychosocial counseling clients was $258 (CI = $191 - $401), with considerable variability across clinics (Olmstead, Sindelar & Petry, 2007b). In the methadone maintenance sample, this value for an added week of abstinence was $141 (CI - $105 - $193). These results suggest that the abstinence incentive program examined in the MIEDAR study is more cost-effectively applied in methadone maintenance than in psychosocial counseling programs. This conclusion is consistent with the fact that the incentive program had a direct and visible impact on the outcome measure used (increased abstinence) in methadone clients (Fig. 1). In contrast, the impact of abstinence incentives on the defined beneficial outcome (abstinence) in psychosocial counseling client is more indirect, where it seems to be mediated by prolonged treatment retention (Fig. 2). While the cost-benefit analyses focused exclusively on increased drug abstinence, there may be other indirect benefits that were not included in the analysis. These might include reduced need for ancillary services due to improved psychosocial functioning in methadone maintenance participants who reduce or stop stimulant use, increased billing opportunities and reduced client turnover dur to better client retention in psychosocial counseling programs. Thus, as the authors note, policy decisions to support the addition of incentive programs to existing drug abuse treatment will depend on the willingness of society in general and specific payers in particular to subsidize the cost of the new intervention in a given situation given the degree and type of outcome improvement to be expected.
Dissemination of motivational incentive treatments
With study results in hand that clearly demonstrate effectiveness of an abstinence incentive treatment, NIDA sponsored the convening of a Blending Team to develop a clinical training package for dissemination of this evidence-based treatment technology. The Blending Team working under leadership of the Great Lakes Addiction Technology Transfer Center (ATTC), developed a multi-media package of support materials for clinicians. The main intent of the package is promoting awareness of this intervention, a step that was hoped to enhance uptake of a little used but clearly evidence-based practice. The Blending Team Product is titled Promoting Awareness of Motivational Incentives (PAMI). It consists of a video presentation on the history, rationale and clinical impact of incentives, a power point presentation about the supporting research and methods, and materials to help providers implement incentive interventions. The PAMI blending product can be found either through the ATTC (www.attcnetwork.org) or NIDA dissemination library (ctndisseminationlibrary.org) websites.
While no formal evaluation of the dissemination effort has been undertaken, it is hoped and expected that this dissemination effort will further stimulate adoption and utilization of this potentially very powerful treatment intervention tool (see also Kellogg, Burns, Coleman, Stitzer, Wale, & Kreek, 2007; Stitzer & Kellogg, 2009 for descriptive examples of current incentive adoption activities). There are still some barriers to be addressed that impede wide-spread use of abstinence incentive interventions, particularly the cost of incentives themselves. Nevertheless, the MIEDAR study and subsequent CTN dissemination activities have been enormously influential in promoting the adoption of this highly effective approach to behavioral treatment for stimulant users.
Summary and Conclusions
This paper has reviewed the CTN MIEDAR studies of abstinence incentives for stimulant users, highlighting both main findings and secondary analyses. Overall, the main findings demonstrate effectiveness of the particular prize-based intervention employed in the CTN trial, one in which incentive participants could earn up to $400 in prizes over a 12-week period by submitting drug- and alcohol-free biological specimens. It was notable that this particular intervention was shown to be effective since the efficacy of abstinence incentives is known to depend on magnitude of reinforcement offered (Lussier et al., 2006) and the MIEDAR study employed a relatively low reinforcement magnitude. These findings support both the clinical utility and potential feasibility of adoption for these types of interventions.
The CTN MIEDAR studies highlighted the differential impact of the abstinence incentive program in methadone maintained stimulant users versus those enrolled in psychosocial counseling treatment, while secondary analyses noted the differential implications for cost-effectiveness of the intervention in these two populations. Clinicians and policy makers must decide what cost is acceptable in order to obtain the benefits of a particular abstinence incentive program. Also of clinical importance was the key role played by on-going stimulant use at the start of treatment, a clinical characteristic that may be associated with severity of drug dependence. The observation that individuals entering psychosocial treatment with active stimulant use (as revealed by urinalysis testing) did not respond well to this particular abstinence incentive program highlights the need to examine moderators of treatment response and tailor treatments to meet the needs of those who may not respond to a particular intervention.
One study can never provide definitive answers to every question of interest with regard to the effectiveness and utility of a particular clinical intervention. More research is always beneficial to establish the generality and size of intervention effects across different schedules and magnitudes of abstinence reinforcement and in different populations. Nevertheless, an important advance in knowledge was made when the CTN MIEDAR study demonstrated effectiveness of one abstinence incentive intervention in a large-scale mulit-site clinical trial conducted at community treatment programs. The outcome data support adoption of this abstinence incentive intervention across a wide range of stimulant users while secondary analyses provide reassurance about the safety of the intervention as well as important clues about subgroups of clients for whom additional intervention tailoring may be needed.
Acknowledgments
Preparation of this paper and research reported therein was supported by U10 13034 Cooperative Agreement from the National Institute on Drug Abuse, and P30-DA023918.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Alterman AI, Kampman K, Boardman CR, Cacciola JS, Rutherford MJ, McKay JR, Maany I. A cocaine-positive baseline urine predicts outpatient treatment attrition and failure to attain initial abstinence. Drug and Alcohol Dependence. 1997;46:79–85. doi: 10.1016/s0376-8716(97)00049-5. [DOI] [PubMed] [Google Scholar]
- Alterman AI, McKay JR, Mulvaney FD, McLellan AT. Prediction of attrition from day hospital treatment in lower socioeconomic cocaine-dependent men. Drug and alcohol Dependence. 1996;40:227–233. doi: 10.1016/0376-8716(95)01212-5. [DOI] [PubMed] [Google Scholar]
- Ball S, Martino S, Nich C, Frankforter T, Van Horn D, Crits-Christoph P, Woody GE, Obert JL, Farentinos C, Carroll KM. Site matters: Multisite randomized trial of Motivational Enhancement Therapy in drug abuse clinics. Journal of Consulting and Clinical Psychology. 2007;75:556–567. doi: 10.1037/0022-006X.75.4.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Ball SA, Nich C, Martino S, Frankforter TL, Farentinos C, Kunkel LE, Mikulich-Gilbrtson SK, Morgenstern J, Obert JL, Polcin D, Snead N, Woody GE. Motivational interviewing to improve treatment engagement and outcome in individuals seeking treatment for substance abuse: A multisite effectiveness study. Drug and Alcohol Dependence. 2006;81:301–312. doi: 10.1016/j.drugalcdep.2005.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehrman RN, Robbins SJ, Cornish JW. Results of a baseline urine test predict levels of cocaine use during treatment. Drug and Alcohol Dependence. 2001;62:1–7. doi: 10.1016/s0376-8716(00)00137-x. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Budney AJ, Bickel WK, Hughes JR, Foerg F, Badger G. Achieving cocaine abstinence with a behavioral approach. American Journal of Psychiatry. 1993;150:763–769. doi: 10.1176/ajp.150.5.763. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Budney AJ, Bickel WK, Foerg FE, Donham R, Badger GJ. Incentives improve outcome in outpatient behavioral treatment of cocaine dependence. Archives of General Psychiatry. 1994;51:568–576. doi: 10.1001/archpsyc.1994.03950070060011. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Wong CJ, Badger GJ, Ogden DE, Dantona RA. Contingent reinforcement increases cocaine abstinence during outpatient treatment and 1 year of follow-up. Journal of Consulting and Clinical Psychology. 2000;68:64–72. doi: 10.1037//0022-006x.68.1.64. [DOI] [PubMed] [Google Scholar]
- Kellogg SH, Burns M, Coleman P, Stitzer M, Wale JB, Kreek MJ. Something of value: The introduction of contingency management interventions into New York City Health and Hospital Addiction Treatment Services. Journal of Substance Abuse Treatment. 2005;28:57–65. doi: 10.1016/j.jsat.2004.10.007. [DOI] [PubMed] [Google Scholar]
- Killeen T, Carter R, Copersino M, Petry N, Stitzer M. Effectiveness of motivational incentives in stimulant abusing outpatients with different treatment histories. The American Journal of Drug and Alcohol Abuse. 2007;33:129–137. doi: 10.1080/00952990601091101. [DOI] [PubMed] [Google Scholar]
- Lussier JP, Heil LH, Mongeon JA, Badger GJ, Higgins ST. A meta-analysis of voucher-based reinforcement therapy for substance use disorders. Addiction. 2006;101:192–203. doi: 10.1111/j.1360-0443.2006.01311.x. [DOI] [PubMed] [Google Scholar]
- Olmstead TA, Sindelar JL, Petry NM. Cost-effectiveness of prize-based incentives for stimulant abusers in outpatient psychosocial treatment programs. Drug and Alcohol Dependence. 2007a;87:175–182. doi: 10.1016/j.drugalcdep.2006.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olmstead TA, Sindelar JL, Petry NM. Clinic variation in the cost-effectiveness of contingency management. The American Journal on Addictions. 2007b;16:457–460. doi: 10.1080/10550490701643062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peirce JM, Petry NM, Stitzer ML, Blaine J, Kellogg S, Satterfield F, Schwartz M, Kraznansky J, Pencer E, Silva-Vasquez L, Kirby KC, Royer-Malvestuto C, Roll JM, Cohen A, Copersino ML, Kolodner K, Li R. Effects of lower-cost incentives on stimulant abstinence in methadone maintenance treatment. Archives of General Psychiatry. 2006;63:201–208. doi: 10.1001/archpsyc.63.2.201. [DOI] [PubMed] [Google Scholar]
- Peirce JM, Petry NM, Roll JM, Kolodner K, Krasnansky J, Stabile PQ, Brown C, Stitzer ML. Correlates of stimulant treatment outcome across treatment modalities. The American Joural of Drug and Alcohol Abuse. 2009;35:48–53. doi: 10.1080/00952990802455444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Alessi SM, Carroll KM, Hanson T, MacKinnon S, Rounsaville B, Sierra S. Contingency management treatments: reinforcing abstinence versus adherence with goal-related activities. Journal of Consulting and Clinical Psychology. 2006;74:592–601. doi: 10.1037/0022-006X.74.3.592. [DOI] [PubMed] [Google Scholar]
- Petry NM, Alessi SM, Marx J, Austin M, Tardif M. Vouchers versus prizes: contingency management treatment of substance abusers in community settings. Journal of Consulting and Clinical Psychology. 2005;73:1005–1014. doi: 10.1037/0022-006X.73.6.1005. [DOI] [PubMed] [Google Scholar]
- Petry NM, Kolodner KB, Li R, Peirce JM, Roll JM, Stitzer ML, Hamilton JA. Prize-based contingency management does not increase gambling. Drug and Alcohol Dependence. 2006;83:269–273. doi: 10.1016/j.drugalcdep.2005.11.023. [DOI] [PubMed] [Google Scholar]
- Petry NM, Martin B. Low-cost contingency management for treating cocaine- and opioid- abusing methadone patients. Journal of Consulting and Clinical Psychology. 2002;70:398–405. doi: 10.1037//0022-006x.70.2.398. [DOI] [PubMed] [Google Scholar]
- Petry NM, Martin B, Cooney JL, Kranzler HR. Give them prizes and they will come: Variable-ratio contingency management for treatment of alcohol dependence. Journal of Consulting and Clinical Psychology. 2000;68:250–257. doi: 10.1037//0022-006x.68.2.250. [DOI] [PubMed] [Google Scholar]
- Petry NM, Peirce JM, Stitzer ML, Blaine J, Roll JM, Cohen A, Obert J, Killeen T, Saladin ME, Cowell M, Kirby KC, Sterling R, Royer-Malvestuto C, Hamilton J, Booth RE, Macdonald M, Liebert M, Rader L, Burns R, DiMaria J, Copersino M, Stabile PQ, Kolodner K, Li R. Effect of prize-based incentives on outcomes in stimulant abusers in outpatient psychosocial treatment programs: a national drug abuse treatment clinical trials network study. Archives of General Psychiatry. 2005;62:1148–1156. doi: 10.1001/archpsyc.62.10.1148. [DOI] [PubMed] [Google Scholar]
- Petry NM, Roll JM, Rounsaville BJ, Ball SA, Stitzer M, Peirce JM, Blaine J, Kirby K, McCarty D, Carroll KM. Serious adverse events in randomized psychosocial treatment studies: Safety or arbitrary edicts? Journal of Consulting and Clinical Psychology. 2008;76:1076–1082. doi: 10.1037/a0013679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Tedford J, Austin M, Nich C, Carroll KM, Rounsaville BJ. Prize reinforcement contingency management for treatment of cocaine abusers: How low can we go, and with whom? Addiction. 2004;99:349–360. doi: 10.1111/j.1360-0443.2003.00642.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roll JM, Petry NM, Stitzer ML, Brecht ML, Peirce JM, McCann MJ, Blaine J, MacDonald M, DiMaria J, Lucero L, Kellogg S. Contingency management for the treatment of methamphetamine use disorders. American Journal of Psychiatry. 2006;163:1993–1999. doi: 10.1176/ajp.2006.163.11.1993. [DOI] [PubMed] [Google Scholar]
- Silverman K, Higgins ST, Brooner RK, Montoya ID, Cone EF, Schuster CR, Preston KL. Sustained cocaine abstinence in methadone maintenance patients through voucher-based reinforcement therapy. Archives of General Psychiatry. 1996;53:409–415. doi: 10.1001/archpsyc.1996.01830050045007. [DOI] [PubMed] [Google Scholar]
- Silverman K, Robles E, Mudric T, Bigelow GE, Stitzer ML. A randomized trial of long-term reinforcement of cocaine abstinence in methadone-maintained patients who inject drugs. Journal of Consulting and Clinical Psychology. 2004;72:839–854. doi: 10.1037/0022-006X.72.5.839. [DOI] [PubMed] [Google Scholar]
- Sindelar JL, Olmstead TA, Peirce JM. Cost-effectiveness of prize-based contingency management iu methadone maintenance treatment programs. Addiction. 2007;102:1463–1471. doi: 10.1111/j.1360-0443.2007.01913.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stitzer ML, Bigelow GE, Liebson I. Reducing benzodiazepine self-administration with contingent reinforcement. Addictive Behaviors. 1979;4:245–252. doi: 10.1016/0306-4603(79)90034-0. [DOI] [PubMed] [Google Scholar]
- Stitzer ML, Bigelow GE, Liebson I. Reducing drug use among methadone maintenance clients: Contingent reinforcement for morphine-free urines. Addictive Behaviors. 1980;5:333–340. doi: 10.1016/0306-4603(80)90007-6. [DOI] [PubMed] [Google Scholar]
- Stitzer ML, Bigelow GE, Liebson IA, Hawthorne JW. Contingent reinforcement for benzodiazepine-free urines: Evaluation of a drug abuse treatment intervention. Journal of Applied Behavior Analysis. 1982;15:493–503. doi: 10.1901/jaba.1982.15-493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stitzer ML, Kellogg S. Large-Scale Dissemination Efforts in Drug Abuse Treatment Clinics. In: Higgins ST, Silverman K, Heil SH, editors. Contingency Management in the Treatment of Substance Use Disorders: A Science-Based Treatment Innovation. New York: Guilford Press; 2008. pp. 241–260. [Google Scholar]
- Stitzer ML, Peirce J, Petry NM, Kirby K, Roll J, Krasnansky J, Cohen A, Blaine J, Vandrey R, Kolodner K, Li R. Abstinence-based incentives in methadone maintenance: Interaction with intake stimulant test results. Experimental and Clinical Psychopharmacology. 2007;15:344–350. doi: 10.1037/1064-1297.15.4.344. [DOI] [PubMed] [Google Scholar]
- Stitzer ML, Petry N, Peirce J, Kirby K, Killeen T, Roll J, Hamilton J, Stabile PQ, Sterling R, Brown C, Kolodnter K, Li R. Effectiveness of abstinence-based incentives: Interaction with intake stimulant test results. Journal of Consulting and Clinical Psychology. 2007;75:805–811. doi: 10.1037/0022-006X.75.5.805. [DOI] [PubMed] [Google Scholar]
- Skinner BF. The behavior of organisms: an experimental analysis. New York: Appleton-Century Company, Inc.; 1938. [Google Scholar]
- Sofuoglu M, Gonzalez G, Poling J, Kosten TR. Prediction of treatment outcome by baseline urine cocaine results and self-reported cocaine use for cocaine and opioid dependence. The American Journal of Drug and Alcohol Abuse. 2003;29:713–727. doi: 10.1081/ada-120026256. [DOI] [PubMed] [Google Scholar]