Abstract
In response to infection or injury, a ubiquitous nucleosomal protein, HMGB1 is secreted actively by innate immune cells, and / or released passively by injured/damaged cells. Subsequently, extracellular HMGB1 alerts, recruits, and activates various innate immune cells to sustain a rigorous inflammatory response. A growing number of HMGB1 inhibitors ranging from neutralizing antibodies, endogenous hormones, to medicinal herb-derived small molecule HMGB1 inhibitors (such as nicotine, glycyrrhizin, tanshinones, and EGCG) are proven protective against lethal infection and ischemic injury. Here we review emerging evidence that support extracellular HMGB1 as a proinflammatory alarmin(g) danger signal, and discuss a wide array of HMGB1 inhibitors as potential therapeutic agents for sepsis and ischemic injury.
Keywords: innate immune cells, phagocytes, inflammation, cytokines, sepsis, antibodies, HMGB1, tanshinones
1. INTRODUCTION
The innate immune cells (such as monocytes and neutrophils) continuously patrol the body to search for invading pathogens or damaged tissues. Equipped with pattern recognition receptors (such as Toll-like receptors, TLR 2, 4, and 9) [1–3], they can recognize various pathogen-associated molecular patterns (PAMPs, e.g., bacterial peptidoglycan, endotoxin, and CpG-DNA) [3–6], or damage-associated molecular patterns (DAMPs, such as HMGB1) [7–9]. Subsequently, innate immune cells infiltrate into infected/injured tissues [10], and release various cytokines (such as TNF, IL-1, IL-6, and IL-12) and chemokines (such as IL-8, MIP-1s, MIP-2 and MCP-1) [11–13]. These biological responses to microbial infection or injury, collectively termed “inflammation” (“set on fire”, in Greek), serve to remove invading pathogens and to heal the wound [14]. In case of severe infection or injury, the inflammatory responses may become dys-regulated, resulting in excessive accumulation of potentially injurious proinflammatory mediators (such as HMGB1). Here we briefly review evidence to support extracellular HMGB1 as a potential therapeutic target for inflammatory diseases.
2. NUCLEAR HMGB1 AS A TRANSCRIPTION FACTOR
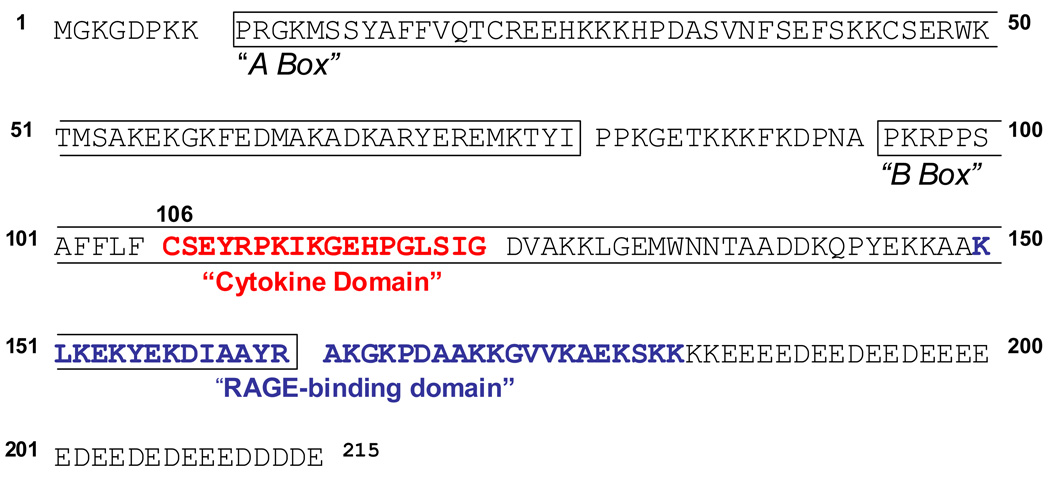
HMG-1 was first purified from nuclei in the 1970’s, and termed “high mobility group” (HMG) protein to reflect its rapid mobility on SDS-PAGE electrophoresis gels [15]. Recently, HMG-1 was renamed as high mobility group box 1 (HMGB1) by a nomenclature committee [16]. It is constitutively expressed in many types of cells, and a large “pool” of preformed HMGB1 is stored in the nucleus, possibly due to the presence of two lysine-rich nuclear localization sequences [17]. As an evolutionarily conserved protein, HMGB1 shares 100% homology (in amino acid sequence) between mouse and rat, and a 99% homology between rodent and human [18–20]. It contains two internal repeats of positively charged domains (“HMG boxes” known as “A box” and “B box”) in the N-terminus (Figure 1), and a continuous stretch of negatively charged (aspartic and glutamic acid) residues in the C-terminus. These HMG boxes enable HMGB1 to bind chromosomal DNA, and fulfill its nuclear functions including determination of nucleosomal structure and stability, and regulation of gene expression [21]. The tertiary structure of full-length HMGB1 is still unknown, because the highly charged properties of the C-terminal tail make it difficult to crystallize the full-length protein.
Figure 1. Amino acid sequence of human HMGB1.
The N-terminus of HMGB1 comprises two repeats of a positively charged domain of about 80 amino acids (termed HMG box A and B) (shown in box). The cytokine-stimulating motif (“Cytokine Domain”, shown in bold text) does not overlap with its RAGE-binding site (bold textg), supporting the potential involvement of other cell surface receptors (such as TLR4) in HMGB1-mediated inflammatory responses.
3. ACTIVE RELEASE
In response to exogenous microbial products (such as endotoxin or CpG-DNA) [5, 6], or endogenous host stimuli (e.g., TNF, IFN-γ, or hydrogen peroxide) [5, 22, 23], innate immune cells actively release HMGB1 into the extracellular space. Lacking a leader signal sequence, HMGB1 can not be actively secreted via the classical ER-Golgi secretory pathway [5]. Instead, activated macrophages/monocytes acetylate lysine residues within the nuclear localization sequences, leading to sequestration of HMGB1 within cytoplasmic vesicles and subsequent release [17, 22, 24]. In addition, phosphorylation of serine residues may also be important for endotoxin-induced nucleo-cytoplasmic translocation of HMGB1 [25]. This process is potentially mediated by protein kinases such as the Calcium/Calmodulin-Dependent Protein Kinase (CaMK) IV [26] and calcium-dependent protein kinase C (cPKC) [27].
In vivo, bacterial infection induced HMGB1 nucleo-cytoplasmic shuttling in tissue (alveolar) macrophages, which was associated with a decrease in TNF production [28], a phenomenon termed “macrophage suppression”. This immunosuppression may be attributable to HMGB1 depletion from the nucleus, where HMGB1 regulates TNF gene transcription by binding to a cis-acting regulatory element (spanning from −157 to −137 bp of the 5’-flanking region) of the TNF gene [29].
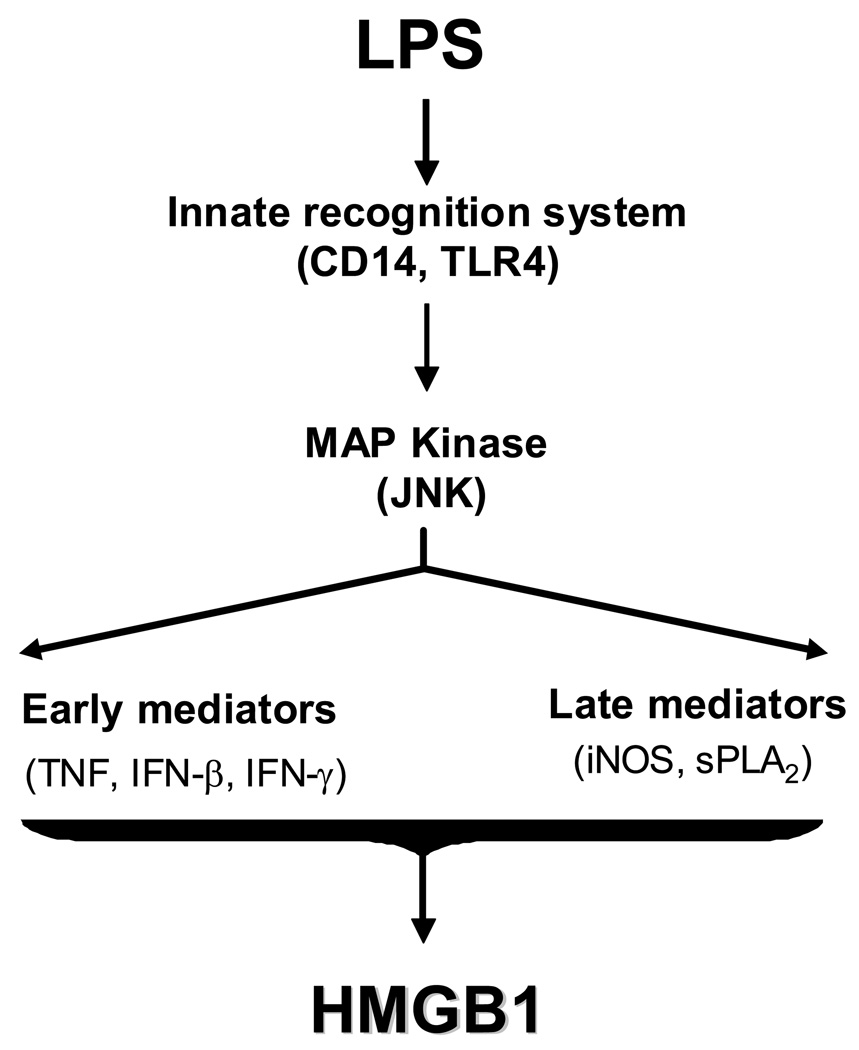
The mechanisms underlying the regulation of endotoxin-induced HMGB1 release are poorly understood. The important roles for endotoxin receptors (such as CD14 and TLR4) are supported by the observations that endotoxin induced less HMGB1 release in CD14-deficient Balb/C or TLR4-defective C3H/HeJ murine macrophages (Figure 2) [5, 27]. The JNK mitogen-activated protein kinase (MAPK) has been implicated in the regulation of HMGB1 release, because specific inhibitors for JNK (but not p38 and ERK1/2) MAPK partly attenuated endotoxin- or hydrogen peroxide-induced HMGB1 release [30, 31]. Early proinflammatory cytokines (e.g., TNF, IFN-γ or IFN-β) may contribute to HMGB1 release, because inhibition of their expression (by gene knock-out) or activities (by neutralizing antibodies) partially attenuates endotoxin-induced HMGB1 release (Figure 2) [31–33]. Although some late proinflammatory mediators [e.g., the 14 kDa phospholipase A2 (PLA2) and inducible nitric oxide synthase (iNOS)]) have also been implicated in the regulation of endotoxin-induced HMGB1 release [24, 30, 34–36], it is not yet known whether endotoxin induced less HMGB1 release in PLA2- or iNOS-deficient macrophages. Conversely, HMGB1 could activate expression of PLA2, and consequently enhance production of lipid mediators (such as prostaglandin E2) in vascular smooth muscle cells [37]. The HMGB1-mediated activation of lipid mediator pathways became more dramatic if these cells were pre-sensitized with proinflammatory cytokines (such as IL-1β), which elevated expression of HMGB1 receptors [including the receptor for advanced glycation end products (RAGE), and toll-like receptors 2 (TLR2 and TLR4)] in these vascular smooth muscle cells [37].
Figure 2. Mechanisms underlying the regulation of endotoxin-induced HMGB1 release.
The potential involvement of several signaling molecules (receptors and MAP kinases) and proinflammatory mediators in endotoxin-induced HMGB1 release is summarized.
4. PASSIVE LEAKAGE
In addition, HMGB1 can be passively released from necrotic cells [38], or cells infected by viruses (e.g., West Nile, Salmon anemia, Dengue, and influenza viruses) [39–42] or mycobacteria [43, 44]. It is possible that HMGB1 passively released by necrotic cells functions as a damage-associated molecular pattern (DAMP) that allows innate immune cells to respond to injury. Notably, necrotic cells also release other HMG box-containing proteins such as the mitochondrial transcription factor A, TFAM, which has recently been shown to similarly amplify innate immune response to necrotic cells [45].
5. EXTRACELLULAR HMGB1 AS AN ALARMIN SIGNAL
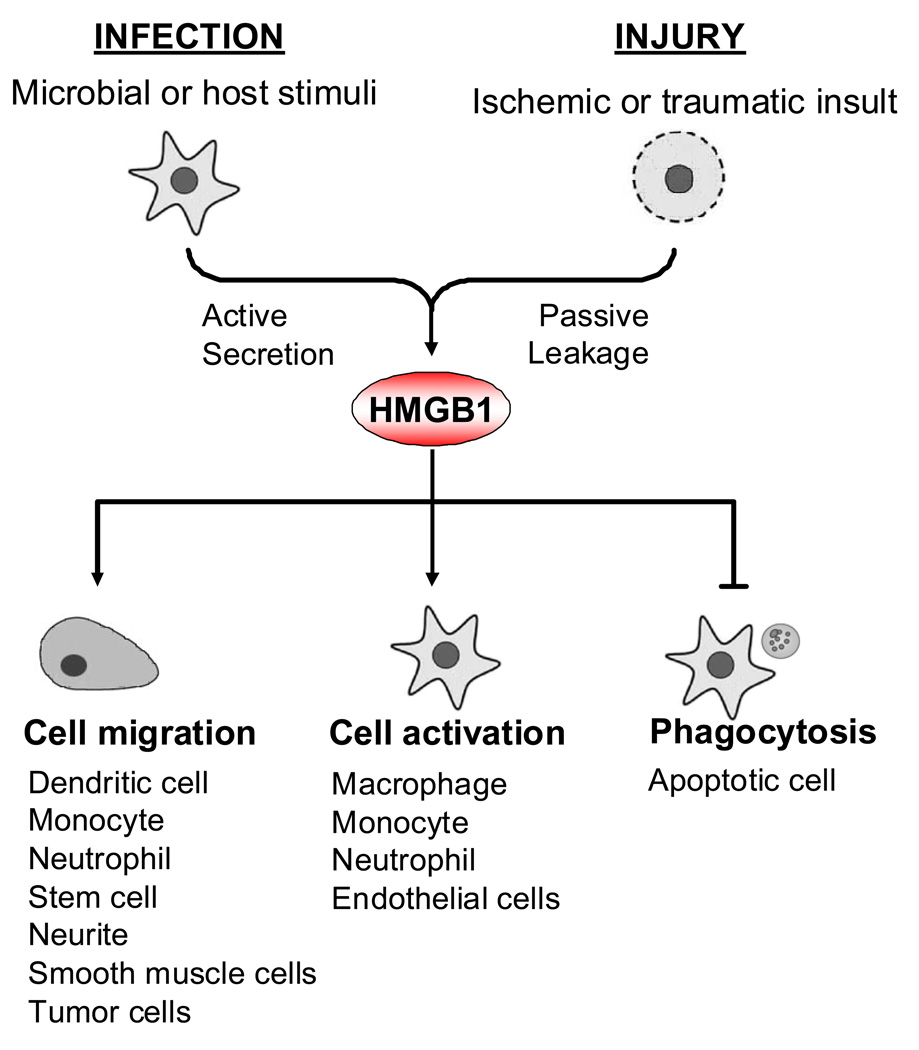
Recently, a number of ubiquitous, structurally and functionally diverse host proteins [such as HMGB1 and heat shock protein 72 (Hsp72)] have been categorized as “alarmins” based on the following shared properties [46] (Figure 3).
Figure 3. Extracellular HMGB1 functions as an alarmin signal.
HMGB1 is actively secreted by innate immune cells and passively released by damaged cells, and orchestrates an inflammatory response by: 1) stimulating cell migration; 2) facilitating innate recognition of bacterial products; 3) activating various innate immune cells; and 4) suppressing phagocytosis of apoptotic cells. Consequently, HMGB1 functions as an alarmin signal to recruit, alert and activate innate immune cells, thereby sustaining potentially injurious inflammatory response during infection or injury.
5.1. Stimulating cell migration
Accumulating evidence indicate that HMGB1 can stimulate migration of various types of cells including neurite [47], smooth muscle cells [48], tumor cells [49], mesoangioblast stem cells [50, 51], monocytes [52], dendritic cells [53, 54], and neutrophils [55, 56] (Figure 3). It raises a possibility that extracellular HMGB1 may facilitate recruitment of innate immune cells to sites of infection or injury [57], thereby functioning as a potential host cell-derived chemotactic factor [58].
5.2. Facilitating innate recognition of microbial products
Emerging evidence have suggested that HMGB1 can bind and facilitate innate recognition of various bacterial products (e.g., CpG-DNA or LPS) by innate immune cells (such as macrophages and dendritic cells) to ensure a more pronounced inflammatory response [6, 59, 60]. For instance, HMGB1 co-localizes with TLR9 and CpG-DNA in macrophage cytoplasmic vesicles [6], and augments CpG-DNA-driven cytokine production in macrophage cultures [6, 59]. It thus appears that innate immune cells have evolved a mechanism to utilize HMGB1 to detect low levels of bacterial products to initiate a rigorous inflammatory response. In addition, HMGB1 may also bind many endogenous molecules such as thrombomodulin [61], immunoglobulin (e.g., IgG1) [62], IL-1 [63], or nucleosomes derived from apoptotic cells [64]. Different host factors, on the other hand, affect HMGB1-mediated inflammatory responses in a negative [61] or positive fashion [63, 64].
5.3. Activating innate immune cells
A number of studies have suggested that extracellular HMGB1 binds to the receptor for advanced glycation end products (RAGE), and pattern-recognition receptors such as TLR2 and TLR4 [65, 66]. Consequently, HMGB1 activates innate immune cells [29, 65–69] or endothelial cells [70, 71] to produce proinflammatory cytokines, chemokines [69], tissue factor [72] and adhesion molecules (Figure 3). In vitro, one of the DNA-binding domains of HMGB1, the “A box”, functions as an antagonist of HMGB1 [73–75]. In contrast, another DNA-binding domain, the “B box”, recapitulates the cytokine activity of full length HMGB1 [8, 76]. Interestingly, oxidation of HMGB1 by reactive oxygen species (ROS) enables formation of disulfide bond involving thiol group of Cys106, Cys23 or Cys45, and consequently abolishes HMGB1-mediated immunostimulatory activities [77]. Because Cys106 is located within the 18-amino acid cytokine domain of HMGB1 B box (Figure 1), it will be important to investigate whether oxidization similarly affects HMGB1-mediated cytokine production.
In addition to RAGE [78] and TLR2/4 [66, 67], HMGB1 can also interact with other cell surface receptors such as CD24 [9], and this interaction enables innate immune cells to distinguish between DAMP- versus PAMP-elicited inflammatory response [9]. Furthermore, phage display assays revealed that HMGB1 can recognize peptide motifs in several oncogenes including p53 and the retinoblastoma susceptibility protein (pRb) [79, 80]. The HMGB1-RB interaction is critical for HMGB1-mediated inhibition of tumor cell proliferation, because HMGB1 mutant lacking the Rb-binding consensus sequence (LXCXE) lost its anti-tumor properties [80]. Thus, HMGB1 may be involved in the stabilization and/or assembly of many multifunctional complexes through protein-protein interactions.
5.4. Inhibiting phagocytotic elimination of apoptotic neutrophils
During infection or injury, macrophages are also responsible for eliminating apoptotic cells, and rely on cell surface receptors for phosphatidylserine (PS) to recognize them. Interestingly, HMGB1 could interact with PS on cell surface of apoptotic neutrophils, and consequently inhibit phagocytotic elimination of apoptotic neutrophils by macrophages (Figure 3) [81]. Inefficient elimination of apoptotic cells may lead to excessive accumulation of late apoptotic and/or secondary necrotic cells, which may cause passive leakage of HMGB1 and other DAMPs [82]. Considered together, these studies indicate that extracellular HMGB1 can function as an alarmin signal to recruit, alert and activate innate immune cells, thereby sustaining a potentially injurious inflammatory response during infection or injury.
6. HMGB1 AS A LATE MEDIATOR OF EXPERIMENTAL SEPSIS
Sepsis refers to a systemic inflammatory response syndrome resulting from a microbial infection. A wide array of pro-inflammatory cytokines including TNF [83], IL-1 [84], IFN-γ [85], and macrophage migration inhibitory factor (MIF) [86, 87] individually or in combination, contribute to the pathogenesis of lethal systemic inflammation. For instance, neutralizing antibodies against TNF [83], reduces lethality in an animal model of endotoxemic/bacteremic shock. However, the early kinetics of systemic TNF accumulation makes it difficult to target in clinical setting [83], prompting the investigation of other late proinflammatory mediators (such as HMGB1) as potential therapeutic target for inflammatory diseases.
6.1. Delayed systemic HMGB1 accumulation
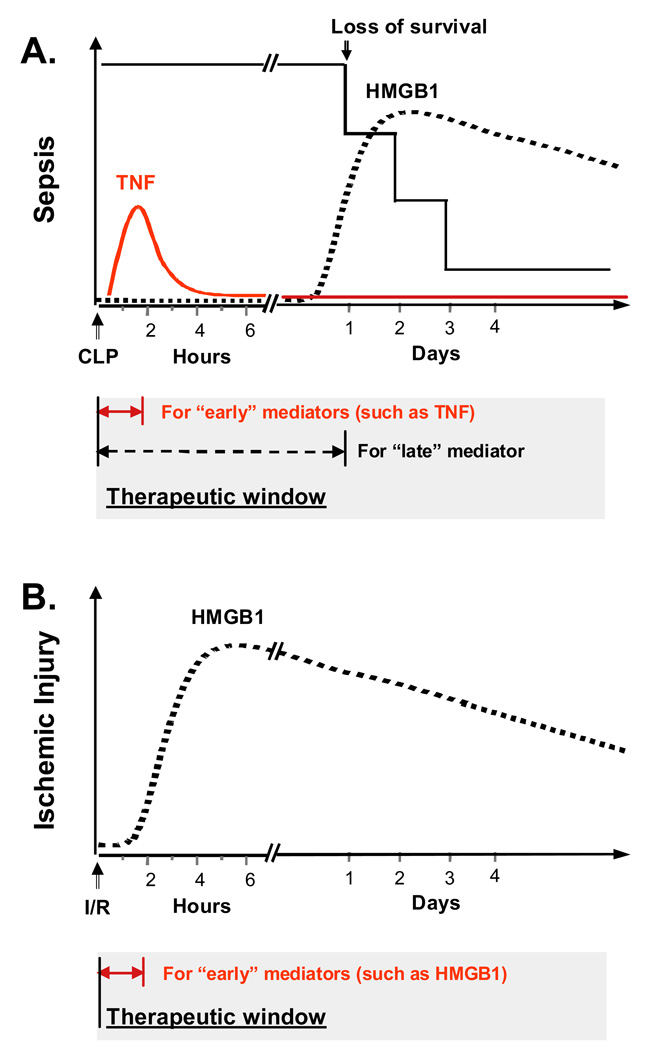
The prevailing theories of sepsis as a dys-regulated systemic inflammatory response are supported by extensive studies employing various animal models of sepsis, including endotoxemia and peritonitis induced by cecal ligation and puncture (CLP) [14, 88]. In murine models of endotoxemia and sepsis, HMGB1 is first detectable in the circulation eight hours after the onset of diseases, subsequently increasing to plateau levels from 16 to 32 hours [5, 73]. Meanwhile, tissue HMGB1 mRNA levels are increased in various tissues such as muscle, liver, and lung during endotoxemia [89] or burn-induced sepsis [90]. This late appearance of circulating HMGB1 precedes and parallels with the onset of animal lethality from endotoxemia or sepsis, and distinguishes itself from TNF and other early proinflammatory cytokines [91] (Figure 4). Although circulating HMGB1 levels in un-fractionated crude serum of septic patients did not correlate with disease severity [92, 93], its levels in the < 100 kDa sub-fraction (following ultrafiltration through filters with M.W. cut-off) correlated well with the lethal outcome of human sepsis [5, 14]. It supported the notion that HMGB1 can interact with other serum components such as thrombomodulin [61], immunoglobulin (e.g., IgG1) [62] to form large (> 100 kDa) complexes [14].
Figure 4. HMGB1 functions as late of sepsis, but an early mediator of ischemic injury.
A). HMGB1 as a late mediator of experimental sepsis. Mice subjected to experimental sepsis (such as cecal ligation and puncture, CLP) succumb at latencies of up to 1–3 days, long after early proinflammatory cytokines (such as TNF) reach plateau levels in the circulation. In contrast, HMGB1 reach peak levels in the circulation in a delayed fashion, which parallels with septic lethality, thereby providing HMGB1 with a wider therapeutic window. B). HMGB1 as an early mediator of ischemic injury. Immediately following ischemic insult, HMGB1 is rapidly released by injured cells, and accumulates in the circulation within a few hours. Consequently, the therapeutic window for HMGB1-targeting strategies is relatively narrower as opposed to experimental sepsis.
6.2. HMGB1-mediated injurious inflammatory responses
Administration of exogenous HMGB1 to mice recapitulates many clinical signs of sepsis including fever [94], derangement of intestinal barrier function [95], and tissue injury [96–99]. In the brain, exogenous HMGB1 induces the release of proinflammatory cytokines [100] and excitatory amino acids (such as glutamate) [101] and fever [94]. In the lung, HMGB1 induces neutrophil infiltration and acute injury [96–99]. Focal administration of HMGB1 near the sciatic nerve induces unilateral and bilateral low threshold mechanical allodynia [102]. Similarly, intraperitoneal injection of HMGB1 induces peritoneal infiltration of neutrophils [56], and accumulation of cytokines (e.g., TNF and IL-6) and chemokines (e.g., MCP-1).
6.3. Protective effects of anti-HMGB1 antibodies
The pathogenic role of HMGB1 as a late mediator of lethal endotoxemia was previously examined using HMGB1-specific neutralizing antibodies, which conferred a dose-dependent protection against lethal endotoxemia [5], and reversed endotoxin-induced gut barrier dysfunction [103]. In a more clinically relevant animal model of sepsis (induced by CLP), delayed administration of HMGB1-specific neutralizing antibodies beginning 24 h after the onset of sepsis, dose-dependently rescued mice from lethal sepsis [73, 104]. Taken together, these experimental data establish extracellular HMGB1 as a critical late mediator of experimental sepsis, with a wider therapeutic window than early proinflammatory cytokines (Figure 4).
7. HMGB1 AS AN EARLY MEDIATOR OF ISCHEMIC INJURY
Emerging evidence have suggested that HMGB1 can be released from ischemic, damaged, or dying cells and tissues during ischemia/reperfusion, and trigger a potentially injurious innate immune response [105] (Figure 4). In contrast to the delayed systemic HMGB1 accumulation in experimental sepsis, HMGB1 release occurs quickly in patients with hemorrhagic shock [106] or traumatic injury [107]. Consequently, circulating HMGB1 levels are elevated within 2–6 hours after onset of hemorrhagic shock and traumatic injury [102, 103]. In animal models of hepatic ischemic/reperfusion injury, prophylactic administration of HMGB1-neutralizing antibody conferred protection against hepatic I/R injury in mice [108–112]. Similarly, treatment with HMGB1 antagonist (such as HMGB1 box A) significantly reduced myocardial [113] and cerebral [114, 115] ischemic injury. Notably, anti-HMGB1 agents are not protective in TLR4-defective [111] or RAGE-deficient mutants [113, 116], indicating a potential role for TLR4 or RAGE in HMGB1-mediated ischemic injury. The potential involvement of RAGE in HMGB1-mediated ischemic injury was further supported by the observation that genetic RAGE deficiency and the decoy soluble RAGE receptor similarly reduced cerebral ischemic injury [115].
In addition, HMGB1-specific neutralizing antibodies have been proven protective against ventilator-induced acute lung injury [117], severe acute pancreatitis [118], and hemorrhagic shock [106], supporting a pathogenic role for extracellular HMGB1 in various inflammatory diseases. Although elevated serum HMGB1 levels were associated with adverse clinical outcomes in patients with myocardial infarction [119], prolonged blockade of HMGB1 with neutralizing antibodies (for 7 days) impaired healing process in animal models of myocardial ischemia/reperfusion. Therefore, like other cytokines, there may be protective advantages of extracellular HMGB1 when released at low amounts [120, 121]. Indeed, HMGB1 is capable of attracting stem cells [50], and may be important for tissue repair and regeneration [14, 120]. It is thus important to pharmacologically modulate, rather than abrogate, systemic HMGB1 accumulation to facilitate resolution of potentially injurious inflammatory response.
8. POTENTIAL HMGB1-INHIBITING THERAPEUTIC AGENTS
With a limited number of effective therapies available for inflammatory diseases, it is important to search for other agents capable of inhibiting clinically accessible mediators. Below is a list of agents that have been proven protective against experimental sepsis and ischemic injury partly through attenuating systemic or local HMGB1 accumulation (Table 1).
Table 1.
Protective effects of HMGB1-inhibiting agents in animal models of endotoxemia and sepsis.
| Agents | Animal model of systemic inflammation |
Via inhibiting HMGB1 |
References |
|---|---|---|---|
| Antibodies | |||
| Anti-IFN-γ | Sepsis | release | 32 |
| Anti-HMGB1 | Endotoxemia and Sepsis | activity | 5,73, 104 |
| Intravenous immunoglobulin (IVIG) | Sepsis | release | 122 |
| Anti-coagulant agents | |||
| Anti-thrombin III | Endotoxemia | release | 124 |
| Thrombomodulin | Endotoxemia | activity | 61, 125 |
| Endogenous hormones | |||
| Insulin | Endotoxemia | release | 126, 128 |
| Vasoactive intestinal peptide | Endotoxemia and Sepsis | release | 127, 129 |
| Ghrelin | Sepsis | release | 130–133 |
| Vagus nerve stimulation | |||
| Electrical | Endotoxemia and Sepsis | release | 134, 135 |
| Chemical (nicotine, GTS-21, choline) | Endotoxemia and Sepsis | release | 137–139 |
| Mechanical (transcutaneous) | Endotoxemia and Sepsis | release | 136 |
| Chinese herbal components | |||
| Danshen (TSN IIA-SS) | Endotoxemia and Sepsis | release | 36 |
| Green tea (EGCG) | Endotoxemia and Sepsis | release | 143, 144 |
| Others | |||
| Ethyl pyruvate | Endotoxemia and Sepsis | release | 148, 149 |
| Cisplatin | Sepsis | release | 150 |
| Spermine | Sepsis | release and activity | 155 |
8.1. Potential therapeutic agents for sepsis
8.1.1. Antibodies
In animal model of sepsis, intravenous administration of IFN-γ antibodies (1.2 mg/kg), immediately or 24 h after CLP decreased peritoneal and serum HMGB1 levels, and consequently attenuated CLP-induced animal mortality [32]. It suggests that specific inhibition of HMGB1-stimulating proinflammatory cytokines may attenuate sepsis-induced HMGB1 accumulation, thereby protecting animals against lethal sepsis.
In addition to cytokine-specific neutralizing antibodies, immunoglobulins (IgG, antibodies) pooled from the plasma of many healthy blood donors, the intravenous immunoglobulin (IVIG), have also been shown to be protective against sepsis-induced lung injury and lethality by attenuating systemic HMGB1 release [122]. Because human IgGs may potentially interact with HMGB1 in vitro [62], it is not known whether IVIG attenuates systemic HMGB1 accumulation, or merely interfere with ELISA detection of HMGB1 [14].
8.1.2. Anti-coagulant agents
Antithrombin inhibits the pro-coagulant activities of thrombin upon interaction with heparin or related glycosaminoglycans. Although anti-thrombin III (AT-III) failed to reduce mortality rate in large sepsis clinical trial [123], a recent study suggested that AT-III attenuated endotoxin-induced systemic HMGB1 accumulation, and reduced endotoxemic lethality [124]. Another anti-coagulant protein, thrombomodulin can bind thrombin to inhibit its pro-coagulant activities, and enhance its capacities to activate a plasma anticoagulant, activated protein C. Interestingly, soluble human thrombomodulin (ART-123) is capable of binding to HMGB1 protein [61], thereby inhibiting HMGB1-mediated inflammatory response. Furthermore, ART-123 conferred significant protection against lethal endotoxemia [61, 125], and endotoxin-induced acute liver injury [125]. However, it is not yet known whether ART-123 is protective in clinically relevant animal models of sepsis.
8.1.3. Endogenous hormones
A number of endogenous hormones such as insulin [126], neuropeptides [e.g., vasoactive intestinal peptide (VIP), the pituitary adenylate cyclase-activating polypeptide (PACAP), and urocortin] [127], and ghrelin have been shown to be protective against lethal endotoxemia or sepsis partly by attenuating systemic HMGB1 accumulation. For instance, acute infusion of insulin conferred protection against lethal endotoxemia [126], although it is not yet known whether the protective effects are dependent on insulin’s anti-inflammatory activities or glucose-modulating properties [128]. In animal models of sepsis induced by CLP, administration of VIP or urocortin attenuated systemic HMGB1 accumulation, and consequently reduced animal lethality [127]. Another member of the VIP family, the PACAP, was recently shown to be protective against lethal endotoxemia via a HMGB1-inhibitinig mechanisms [129].
Ghrelin is a stomach-derived hormone responsible for regulating the appetite – increasing it before food intake and decreasing it afterward. Plasma ghrelin levels are decreased in septic animals [130], whereas administration of exogenous ghrelin promoted a dose-dependent protection against sepsis-induced acute lung injury and lethality [130–132]. Notably, ghrelin exerts its protective effects through multiple mechanisms, such as by attenuating systemic HMGB1 release, and by facilitating bacterial elimination [132, 133]. Furthermore, ghrelin attenuates systemic accumulation of proinflammatory cytokines partly via the vagus nerve [131, 133], supporting the notion that pharmacologic stimulation of the vagus nerve may be an effective therapy for experimental sepsis.
8.1.5. Vagus nerve stimulation
It has recently been suggested that the brain can attenuate peripheral innate immune response through efferent vagus nerve signals to tissue-resident macrophages [134]. This effect is mediated by the principle neurotransmitter of the vagus nerve, acetylcholine, which de-activates macrophages via nicotinic cholinergic receptors [134]. Indeed, stimulation of the vagus nerve by physical methods (e.g., electrical or mechanical) [135, 136] or chemical agents (such as cholinergic agonists, nicotine, choline and GTS-21) [137–139] conferred protection against lethal endotoxemia and sepsis partly by attenuating systemic HMGB1 accumulation.
A chemical derivative of choline, stearoyl lysophosphatidylcholine, was proven protective against experimental sepsis by stimulating neutrophils to destroy ingested bacteria in an H2O2-dependent mechanism [140]. However, stearoyl LPC also conferred protection against lethal endotoxemia [140], implying that it might exert protective effects through an additional, bactericidal-independent mechanism [141]. We found that administration of stearoyl LPC significantly attenuated circulating HMGB1 levels [34], indicating that stearoyl LPC protects against experimental sepsis partly by facilitating elimination of invading pathogens, and partly by attenuating systemic HMGB1 accumulation [141].
8.1.6. Chinese medicinal herbs
Traditional herbal medicine has formed the basis of folk remedies for various inflammatory ailments. After screening several dozens of commonly used Chinese herbs [142], we found that aqueous extracts of Danggui (Angelica sinensis), Green tea (Camellia sinensis), and Danshen (Saliva miltorrhiza) efficiently inhibited endotoxin-induced HMGB1 release, and protected animals against lethal endotoxemia and sepsis [35, 36, 143].
8.1.6.1. Danggui
Danggui has been regarded as the “ginseng” for women, and traditionally used to treat many gynecological disorders. We found that its aqueous extract dose-dependently inhibited LPS-induced HMGB1 release in macrophage and monocyte cultures, partly by interfering with HMGB1 cytoplasmic translocation [35]. Furthermore, Danggui extract rescued mice from lethal sepsis even when the first dose was given at 24 h post onset of disease [35]. The active components responsible for these beneficial effects remain to be characterized.
8.1.6.2. Green tea
Brewed from the leaves of the plant, Camellia sinensis, Green tea contains a class of biologically active polyphenols called catechins. As a major catechin, the epigallocatechin (EGCG), effectively inhibited endotoxin-induced HMGB1 release, and attenuated HMGB1-mediated production of nitric oxide by preventing accumulation/clustering of exogenous HMGB1 on macrophage cell surface [143]. Repeated administration of EGCG conferred a dose-dependent protection against lethal endotoxemia, and rescued animals from lethal sepsis even when the first dose of EGCG was given at +24 h after onset of sepsis [143, 144]. The protective effects were associated with a decrease in circulating levels of HMGB1, as well as two surrogate markers of experimental sepsis (such as IL-6 and KC) [143, 145].
8.1.6.3. Danshen
Danshen, a medicinal herb widely used in China for patients with cardiovascular disorders [146, 147], contains abundant red pigments (termed tanshinone I, tanshinone IIA, and cryptotanshinone). These tanshinones selectively attenuated LPS-induced HMGB1 release in macrophage cultures in a glucocoticoid receptor-independent mechanism [36], despite a structural resemblance (i.e., the presence of a four-fused-ring structure) between tanshinones and steroidal anti-inflammatory drugs (such as dexamethasone and cortisone). Administration of a water-soluble derivative (sodium sufphonate) of tanshinone IIA, TSN IIA-SS, beginning at +24 h, followed by additional doses at +48, +72 and + 96 h after the onset of sepsis, dose-dependently rescued mice from lethal sepsis [36]. Administration of TNS IIA-SS dose-dependently attenuated circulating HMGB1 levels in septic mice [36], suggesting that TSN IIA-SS confers protection partly by inhibiting systemic HMGB1 accumulation.
8.1.7. Others
Ethyl pyruvate (EP) is an aliphatic ester derived from pyruvic acid, a final product of glycolysis [148]. Like other HMGB1 inhibitors, EP dose-dependently inhibits LPS-induced HMGB1 release, and rescued mice from lethal sepsis even when the first dose was given at 24 hours after the onset of disease [149]. A platinum-based chemotherapy drug, cisplatin, can be converted into [PtCl(H2O)(NH3)2]+, which can covalently binds to DNA and triggers apoptotic cell death. In a murine model of CLP-induced sepsis, early administration of cisplatin attenuated systemic HMGB1 accumulation, and reduced animal lethality [150]. A ubiquitous biogenic molecule, spermine, is passively released by damaged cells, and functions as a local feedback anti-inflammatory mechanism at sites of infection or injury [151–154]. Intriguingly, it confers significant protection against lethal sepsis only when the first dose was given immediately (0.5 h) post CLP [155]. The protective effects were associated with a significant reduction in peritoneal levels of HMGB1 and several surrogate markers of sepsis, including IL-6, KC, MCP-1, MIP-2, TIMP-1, and sTNFRs [155].
8.2. Potential therapeutic agents for ischemic injury
Many agents capable of inhibiting infection-elicited HMGB1 release are also protective against ischemia-elicited inflammatory responses. For instance, cisplatin was shown to be protective in a murine model of hepatic ischemia/reperfusion injury (Table 2) [156]. Similarly, ethyl pyruvate was also found to be protective against spinal cord ischemic injury [157] and kidney ischemia-reperfusion injury [158] partly through a HMGB1-inhibiting mechanism. In addition, a growing number of herbal components are shown to be effective in inhibiting HMGB1 release, and protecting animals against ischemic injury. For example, a major sweet component of a Chinese medicinal herb, liquorice, glycyrrhizin, protected rats against hepatic ischemia/reperfusion-in injury [159] partly by reducing ischemia-elicited leukocyte adherence and neutrophil infiltration into ischemic liver tissue [159]. Similarly, cannabidiol, CBD, a non-psychoactive cannabinoid of Marijuana (Cannabis), was shown to be protective against cerebral ischemic injury partly by reducing circulating HMGB1 levels [160].
Table 2.
Protective effects of HMGB1-inhibiting agents in animal models of ischemia.
| Agents | Animal model of Ischemia |
References |
|---|---|---|
| Antibodies | ||
| Anti-HMGB1 | Hepatic Ischemia/Reperfusion | 108–112 |
| Cerebral Ischemia | 114, 115 | |
| Antagonist (A box) | ||
| Myocardial Ischemia | 113 | |
| Cerebral Ischemia | 114, 115 | |
| Chinese herbal components | ||
| Glycyrrhizin | Hepatic Ischemia | 159 |
| Cannabidiol | Cerebral Ischemia | 160 |
| Others | ||
| Ethyl pyruvate | Spinal Cord Ischemia | 157 |
| Renal Ischemia | 158 | |
| Cisplatin | Hepatic Ischemia/Reperfusion | 156 |
9. CONCLUSIONS AND PERSPECTIVES
Seemingly unrelated conditions, such as infection and injury, can converge on common processes such as inflammation that is orchestrated by various inflammatory mediators. Extensive pre-clinical animal studies have established HMGB1 as an early mediator of ischemic injury [107–110], and a late mediator of experimental sepsis [5, 161, 162]. Although the therapeutic window for HMGB1-inhibiting agents is rather narrow for ischemia-elicited inflammatory responses, many HMGB1-inhibiting agents could rescue mice from lethal experimental sepsis even when given in a delayed fashion (e.g., 24 h after onset of sepsis) (Figure 4). It is thus important to determine whether HMGB1 will ever become a clinically feasible therapeutic target for human sepsis in future clinical studies.
For complex systemic inflammatory diseases such as sepsis, it appears difficult to translate successful animal studies into clinical applications [14]. For instance, although neutralizing antibodies against cytokines (e.g., TNF) [83, 163] are protective in animal models of endotoxemia, these agents failed in sepsis clinical trials [164–166]. This failure partly reflects the complexity of the underlying pathogenic mechanisms of sepsis, and the consequent heterogeneity of the patient population [167, 168]. It may also be attributable to pitfalls in the selection of: 1) feasible therapeutic targets or drugs; 2) optimal doses and timing of drugs; and 3) non-realistic clinical outcome measures (such as mortality rates) [14, 167–169].
One of the HMGB1 inhibitor, TSN IIA-SS, has been shown protective in animal models of myocardial ischemia/reperfusion injury [170], as well as transient or permanent focal cerebral ischemia [171, 172]. Consequently, it has been widely used in China as a medicine for patients with cardiovascular disorders [146]. In animal models of sepsis, TSN IIA-SS reduced total peripheral vascular resistance, and yet increased cardiac stroke volume and cardiac output [36]. The dual effects of TSN IIA-SS in attenuating late inflammatory response and improving cardiovascular function make it a promising therapeutic agent for sepsis. It is thus important to further investigate the intricate mechanisms by which various agents attenuate systemic HMGB1 release, and explore their therapeutic potential in future clinical studies.
Acknowledgments of funding
Work in authors’ laboratory was supported by grants from the National Institutes of Health, National Institute of General Medical Science (R01GM063075, R01GM070817, to HW).
Footnotes
Conflict of interest: A.E.S. and H.W. are co-inventors of patent applications related to HMGB1 inhibitors as potential therapeutic agents for sepsis.
REFERENCES
- 1.Brightbill HD, Libraty DH, Krutzik SR, Yang RB, Belisle JT, Bleharski JR, Maitland M, Norgard MV, Plevy SE, Smale ST, Brennan PJ, Bloom BR, Godowski PJ, Modlin RL. Host defense mechanisms triggered by microbial lipoproteins through toll-like receptors. Science. 1999;285:732–736. doi: 10.1126/science.285.5428.732. [DOI] [PubMed] [Google Scholar]
- 2.Poltorak A, He X, Smirnova I, Liu MY, Huffel CV, Du X, Birdwell D, Alejos E, Silva M, Galanos C, Freudenberg M, Ricciardi-Castagnoli P, Layton B, Beutler B. Defective LPS signaling in C3H/HeJ and C57BL/10ScCr mice: mutations in Tlr4 gene. Science. 1998;282:2085–2088. doi: 10.1126/science.282.5396.2085. [DOI] [PubMed] [Google Scholar]
- 3.Hemmi H, Takeuchi O, Kawai T, Kaisho T, Sato S, Sanjo H, Matsumoto M, Hoshino K, Wagner H, Takeda K, Akira S. A Toll-like receptor recognizes bacterial DNA. Nature. 2000;408:740–745. doi: 10.1038/35047123. [DOI] [PubMed] [Google Scholar]
- 4.Krieg AM. CpG motifs in bacterial DNA and their immune effects. Annu. Rev. Immunol. 2002;20:709–760. doi: 10.1146/annurev.immunol.20.100301.064842. [DOI] [PubMed] [Google Scholar]
- 5.Wang H, Bloom O, Zhang M, Vishnubhakat JM, Ombrellino M, Che J, Frazier A, Yang H, Ivanova S, Borovikova L, Manogue KR, Faist E, Abraham E, Andersson J, Andersson U, Molina PE, Abumrad NN, Sama A, Tracey KJ. HMG-1 as a late mediator of endotoxin lethality in mice. Science. 1999;285:248–251. doi: 10.1126/science.285.5425.248. [DOI] [PubMed] [Google Scholar]
- 6.Ivanov S, Dragoi AM, Wang X, Dallacosta C, Louten J, Musco G, Sitia G, Yap GS, Wan Y, Biron CA, Bianchi ME, Wang H, Chu WM. A novel role for HMGB1 in TLR9-mediated inflammatory responses to CpG-DNA. Blood. 2007;110:1970–1981. doi: 10.1182/blood-2006-09-044776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Andersson U, Wang H, Palmblad K, Aveberger AC, Bloom O, Erlandsson-Harris H, Janson A, Kokkola R, Zhang M, Yang H, Tracey KJ. High Mobility Group 1 Protein (HMG-1) Stimulates Proinflammatory Cytokine Synthesis in Human Monocytes. J. Exp. Med. 2000;192:565–570. doi: 10.1084/jem.192.4.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li J, Kokkola R, Tabibzadeh S, Yang R, Ochani M, Qiang X, Harris HE, Czura CJ, Wang H, Ulloa L, Wang H, Warren HS, Moldawer LL, Fink MP, Andersson U, Tracey KJ, Yang H. Structural basis for the proinflammatory cytokine activity of high mobility group box 1. Mol. Med. 2003;9:37–45. [PMC free article] [PubMed] [Google Scholar]
- 9.Chen GY, Tang J, Zheng P, Liu Y. CD24 and Siglec-10 Selectively Repress Tissue Damage-Induced Immune Responses. Science. 2009;323:1722–1725. doi: 10.1126/science.1168988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Luster AD, Alon R, von Andrian UH. Immune cell migration in inflammation: present and future therapeutic targets. Nat. Immunol. 2005;6:1182–1190. doi: 10.1038/ni1275. [DOI] [PubMed] [Google Scholar]
- 11.Akira S, Takeda K. Toll-like receptor signalling. Nat. Rev. Immunol. 2004;4:499–511. doi: 10.1038/nri1391. [DOI] [PubMed] [Google Scholar]
- 12.Baggiolini M, Loetscher P. Chemokines in inflammation and immunity. Immunol. Today. 2000;21:418–420. doi: 10.1016/s0167-5699(00)01672-8. [DOI] [PubMed] [Google Scholar]
- 13.Balkwill F. Cytokines--soluble factors in immune responses. Curr. Opin. Immunol. 1988;1:241–249. doi: 10.1016/0952-7915(88)90008-8. [DOI] [PubMed] [Google Scholar]
- 14.Wang H, Zhu S, Zhou R, Li W, Sama AE. Therapeutic potential of HMGB1-targeting agents in sepsis. Expert. Rev. Mol. Med. 2008;10:e32. doi: 10.1017/S1462399408000884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johns EW. History, Definitions and Problems. In: Johns EW, editor. The HMG Chromosomal Proteins. London: Academic Press Inc. (London) Ltd; 1982. pp. 1–8. [Google Scholar]
- 16.Bustin M. Revised nomenclature for high mobility group (HMG) chromosomal proteins. Trends Biochem. Sci. 2001;26:152–153. doi: 10.1016/s0968-0004(00)01777-1. [DOI] [PubMed] [Google Scholar]
- 17.Bonaldi T, Talamo F, Scaffidi P, Ferrera D, Porto A, Bachi A, Rubartelli A, Agresti A, Bianchi ME. Monocytic cells hyperacetylate chromatin protein HMGB1 to redirect it towards secretion. EMBO J. 2003;22:5551–5560. doi: 10.1093/emboj/cdg516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ferrari S, Ronfani L, Calogero S, Bianchi ME. The mouse gene coding for high mobility group 1 protein (HMG1) J. Biol. Chem. 1994;269:28803–28808. [PubMed] [Google Scholar]
- 19.Paonessa G, Frank R, Cortese R. Nucleotide sequence of rat liver HMG1 cDNA. Nucleic Acids Res. 1987;15:9077. doi: 10.1093/nar/15.21.9077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wen L, Huang JK, Johnson BH, Reeck GR. A human placental cDNA clone that encodes nonhistone chromosomal protein HMG-1. Nucleic Acids Res. 1989;17:1197–1214. doi: 10.1093/nar/17.3.1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bustin M. At the crossroads of necrosis and apoptosis: signaling to multiple cellular targets by HMGB1. Sci. STKE. 2002:E39. doi: 10.1126/stke.2002.151.pe39. 2002. [DOI] [PubMed] [Google Scholar]
- 22.Rendon-Mitchell B, Ochani M, Li J, Han J, Wang H, Yang H, Susarla S, Czura C, Mitchell RA, Chen G, Sama AE, Tracey KJ, Wang H. IFN-gamma Induces High Mobility Group Box 1 Protein Release Partly Through a TNF-Dependent Mechanism. J. Immunol. 2003;170:3890–3897. doi: 10.4049/jimmunol.170.7.3890. [DOI] [PubMed] [Google Scholar]
- 23.Tang D, Shi Y, Kang R, Li T, Xiao W, Wang H, Xiao X. Hydrogen peroxide stimulates macrophages and monocytes to actively release HMGB1. J Leukoc. Biol. 2007;81:741–747. doi: 10.1189/jlb.0806540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gardella S, Andrei C, Ferrera D, Lotti LV, Torrisi MR, Bianchi ME, Rubartelli A. The nuclear protein HMGB1 is secreted by monocytes via a non-classical, vesicle-mediated secretory pathway. EMBO Rep. 2002;3:955–1001. doi: 10.1093/embo-reports/kvf198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Youn JH, Shin JS. Nucleocytoplasmic shuttling of HMGB1 is regulated by phosphorylation that redirects it toward secretion. J. Immunol. 2006;177:7889–7897. doi: 10.4049/jimmunol.177.11.7889. [DOI] [PubMed] [Google Scholar]
- 26.Zhang X, Wheeler D, Tang Y, Guo L, Shapiro RA, Ribar TJ, Means AR, Billiar TR, Angus DC, Rosengart MR. Calcium/calmodulin-dependent protein kinase (CaMK) IV mediates nucleocytoplasmic shuttling and release of HMGB1 during lipopolysaccharide stimulation of macrophages. J. Immunol. 2008;181:5015–5023. doi: 10.4049/jimmunol.181.7.5015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Oh YJ, Youn JH, Ji Y, Lee SE, Lim KJ, Choi JE, Shin JS. HMGB1 is phosphorylated by classical protein kinase C and is secreted by a calcium-dependent mechanism. J. Immunol. 2009;182:5800–5809. doi: 10.4049/jimmunol.0801873. [DOI] [PubMed] [Google Scholar]
- 28.Pahuja M, Tran C, Wang H, Yin K. Alveolar macrophage suppression in sepsis is associated with high mobility group box 1 transmigration. Shock. 2008;29:754–760. doi: 10.1097/shk.0b013e31815d0c8f. [DOI] [PubMed] [Google Scholar]
- 29.Yamoah K, Brebene A, Baliram R, Inagaki K, Dolios G, Arabi A, Majeed R, Amano H, Wang R, Yanagisawa R, Abe E. High-mobility group box proteins modulate tumor necrosis factor-alpha expression in osteoclastogenesis via a novel deoxyribonucleic acid sequence. Mol. Endocrinol. 2008;22:1141–1153. doi: 10.1210/me.2007-0460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jiang W, Pisetsky DS. The Role of IFN-{alpha} and Nitric Oxide in the Release of HMGB1 by RAW 264.7 Cells Stimulated with Polyinosinic-Polycytidylic Acid or Lipopolysaccharide. J Immunol. 2006;177:3337–3343. doi: 10.4049/jimmunol.177.5.3337. [DOI] [PubMed] [Google Scholar]
- 31.Chen G, Li J, Ochani M, Rendon-Mitchell B, Qiang X, Susarla S, Ulloa L, Yang H, Fan S, Goyert SM, Wang P, Tracey KJ, Sama AE, Wang H. Bacterial endotoxin stimulates macrophages to release HMGB1 partly through CD14- and TNF-dependent mechanisms. J Leukoc. Biol. 2004;76:994–1001. doi: 10.1189/jlb.0404242. [DOI] [PubMed] [Google Scholar]
- 32.Yin K, Gribbin E, Wang H. Interferon-gamma inhibition attenuates lethality after cecal ligation and puncture in rats: implication of High Mobility Group Box-1. Shock. 2005;24:396–401. doi: 10.1097/01.shk.0000175556.03300.c6. [DOI] [PubMed] [Google Scholar]
- 33.Kim JH, Kim SJ, Lee IS, Lee MS, Uematsu S, Akira S, Oh KI. Bacterial endotoxin induces the release of high mobility group box 1 via the IFN-beta signaling pathway. J. Immunol. 2009;182:2458–2466. doi: 10.4049/jimmunol.0801364. [DOI] [PubMed] [Google Scholar]
- 34.Chen G, Li J, Qiang X, Czura CJ, Ochani M, Ochani K, Ulloa L, Yang H, Tracey KJ, Wang P, Sama AE, Wang H. Suppression of HMGB1 release by stearoyl lysophosphatidylcholine:an additional mechanism for its therapeutic effects in experimental sepsis. J. Lipid Res. 2005;46:623–627. doi: 10.1194/jlr.C400018-JLR200. [DOI] [PubMed] [Google Scholar]
- 35.Wang H, Li W, Li J, Rendon-Mitchell B, Ochani M, Ashok M, Yang L, Yang H, Tracey KJ, Wang P, Sama AE. The Aqueous Extract of a Popular Herbal Nutrient Supplement, Angelica sinensis, Protects Mice against Lethal Endotoxemia and Sepsis. J. Nutr. 2006;136:360–365. doi: 10.1093/jn/136.2.360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li W, Li J, Ashok M, Wu R, Chen D, Yang L, Yang H, Tracey KJ, Wang P, Sama AE, Wang H. A cardiovascular drug rescues mice from lethal sepsis by selectively attenuating a late-acting proinflammatory mediator, high mobility group box 1. J. Immunol. 2007;178:3856–3864. doi: 10.4049/jimmunol.178.6.3856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jaulmes A, Thierry S, Janvier B, Raymondjean M, Marechal V. Activation of sPLA2-IIA and PGE2 production by high mobility group protein B1 in vascular smooth muscle cells sensitized by IL-1beta. FASEB J. 2006;20:1727–1729. doi: 10.1096/fj.05-5514fje. [DOI] [PubMed] [Google Scholar]
- 38.Scaffidi P, Misteli T, Bianchi ME. Release of chromatin protein HMGB1 by necrotic cells triggers inflammation. Nature. 2002;418:191–195. doi: 10.1038/nature00858. [DOI] [PubMed] [Google Scholar]
- 39.Chu JJ, Ng ML. The mechanism of cell death during West Nile virus infection is dependent on initial infectious dose. J. Gen. Virol. 2003;84:3305–3314. doi: 10.1099/vir.0.19447-0. [DOI] [PubMed] [Google Scholar]
- 40.Joseph T, Cepica A, Brown L, Ikede BO, Kibenge FS. Mechanism of cell death during infectious salmon anemia virus infection is cell type-specific. J. Gen. Virol. 2004;85:3027–3036. doi: 10.1099/vir.0.80091-0. [DOI] [PubMed] [Google Scholar]
- 41.Chen LC, Yeh TM, Wu HN, Lin YY, Shyu HW. Dengue virus infection induces passive release of high mobility group box 1 protein by epithelial cells. J. Infect. 2008;56:143–150. doi: 10.1016/j.jinf.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 42.Alleva LM, Budd AC, Clark IA. Systemic release of high mobility group box 1 protein during severe murine influenza. J. Immunol. 2008;181:1454–1459. doi: 10.4049/jimmunol.181.2.1454. [DOI] [PubMed] [Google Scholar]
- 43.Hofner P, Seprenyi G, Miczak A, Buzas K, Gyulai Z, Medzihradszky KF, Rouhiainen A, Rauvala H, Mandi Y. High mobility group box 1 protein induction by Mycobacterium bovis BCG. Mediators Inflamm. 2007:53805. doi: 10.1155/2007/53805. 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Grover A, Taylor J, Troudt J, Keyser A, Sommersted K, Schenkel A, Izzo AA. Mycobacterial infection induces the secretion of high-mobility group box 1 protein. Cell Microbiol. 2008;10:1390–1404. doi: 10.1111/j.1462-5822.2008.01135.x. [DOI] [PubMed] [Google Scholar]
- 45.Crouser ED, Shao G, Julian MW, Macre JE, Shadel GS, Tridandapani S, Huang Q, Wewers MD. Monocyte activation by necrotic cells is promoted by mitochondrial proteins and formyl peptide receptors. Crit. Care Med. 2009;37:2000–2009. doi: 10.1097/CCM.0b013e3181a001ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Oppenheim JJ, Yang D. Alarmins: chemotactic activators of immune responses. Curr. Opin. Immunol. 2005;17:359–365. doi: 10.1016/j.coi.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 47.Fages C, Nolo R, Huttunen HJ, Eskelinen E, Rauvala H. Regulation of cell migration by amphoterin. J. Cell Sci. 2000;113:611–620. doi: 10.1242/jcs.113.4.611. [DOI] [PubMed] [Google Scholar]
- 48.Degryse B, Bonaldi T, Scaffidi P, Muller S, Resnati M, Sanvito F, Arrigoni G, Bianchi ME. The high mobility group (HMG) boxes of the nuclear protein HMG1 induce chemotaxis and cytoskeleton reorganization in rat smooth muscle cells. J. Cell Biol. 2001;152:1197–1206. doi: 10.1083/jcb.152.6.1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Huttunen HJ, Fages C, Kuja-Panula J, Ridley AJ, Rauvala H. Receptor for advanced glycation end products-binding COOH-terminal motif of amphoterin inhibits invasive migration and metastasis. Cancer Res. 2002;62:4805–4811. [PubMed] [Google Scholar]
- 50.Palumbo R, Sampaolesi M, De Marchis F, Tonlorenzi R, Colombetti S, Mondino A, Cossu G, Bianchi ME. Extracellular HMGB1, a signal of tissue damage, induces mesoangioblast migration and proliferation. J. Cell Biol. 2004;164:441–449. doi: 10.1083/jcb.200304135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Palumbo R, Galvez BG, Pusterla T, De Marchis F, Cossu G, Marcu KB, Bianchi ME. Cells migrating to sites of tissue damage in response to the danger signal HMGB1 require NF-kappaB activation. J. Cell Biol. 2007;179:33–40. doi: 10.1083/jcb.200704015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rouhiainen A, Kuja-Panula J, Wilkman E, Pakkanen J, Stenfors J, Tuominen RK, Lepantalo M, Carpen O, Parkkinen J, Rauvala H. Regulation of monocyte migration by amphoterin (HMGB1) Blood. 2004;104:1174–1182. doi: 10.1182/blood-2003-10-3536. [DOI] [PubMed] [Google Scholar]
- 53.Yang D, Chen Q, Yang H, Tracey KJ, Bustin M, Oppenheim JJ. High mobility group box-1 protein induces the migration and activation of human dendritic cells and acts as an alarmin. J. Leukoc. Biol. 2007;81:59–66. doi: 10.1189/jlb.0306180. [DOI] [PubMed] [Google Scholar]
- 54.Dumitriu IE, Bianchi ME, Bacci M, Manfredi AA, Rovere-Querini P. The secretion of HMGB1 is required for the migration of maturing dendritic cells. J. Leukoc. Biol. 2007;81:84–91. doi: 10.1189/jlb.0306171. [DOI] [PubMed] [Google Scholar]
- 55.Orlova VV, Choi EY, Xie C, Chavakis E, Bierhaus A, Ihanus E, Ballantyne CM, Gahmberg CG, Bianchi ME, Nawroth PP, Chavakis T. A novel pathway of HMGB1-mediated inflammatory cell recruitment that requires Mac-1-integrin. EMBO J. 2007;26:1129–1139. doi: 10.1038/sj.emboj.7601552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.van Zoelen MA, Yang H, Florquin S, Meijers JC, Akira S, Arnold B, Nawroth PP, Bierhaus A, Tracey KJ, van der PT. Role of TOLL-like receptors 2 and 4, and the receptor for advanced glycation end products (RAGE) in HMGB1-induced inflammation in vivo. Shock. 2009 doi: 10.1097/SHK.0b013e318186262d. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Degryse B, Bonaldi T, Scaffidi P, Muller S, Resnati M, Sanvito F, Arrigoni G, Bianchi ME. The high mobility group (HMG) boxes of the nuclear protein HMG1 induce chemotaxis and cytoskeleton reorganization in rat smooth muscle cells. J. Cell Biol. 2001;152:1197–1206. doi: 10.1083/jcb.152.6.1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Degryse B, de Virgilio M. The nuclear protein HMGB1, a new kind of chemokine? FEBS Lett. 2003;553:11–17. doi: 10.1016/s0014-5793(03)01027-5. [DOI] [PubMed] [Google Scholar]
- 59.Tian J, Avalos AM, Mao SY, Chen B, Senthil K, Wu H, Parroche P, Drabic S, Golenbock D, Sirois C, Hua J, An LL, Audoly L, La Rosa G, Bierhaus A, Naworth P, Marshak-Rothstein A, Crow MK, Fitzgerald KA, Latz E, Kiener PA, Coyle AJ. Toll-like receptor 9-dependent activation by DNA-containing immune complexes is mediated by HMGB1 and RAGE. Nat. Immunol. 2007;8:487–496. doi: 10.1038/ni1457. [DOI] [PubMed] [Google Scholar]
- 60.Silva E, Arcaroli J, He Q, Svetkauskaite D, Coldren C, Nick JA, Poch K, Park JS, Banerjee A, Abraham E. HMGB1 and LPS induce distinct patterns of gene expression and activation in neutrophils from patients with sepsis-induced acute lung injury. Intensive Care Med. 2007;33:1829–1839. doi: 10.1007/s00134-007-0748-2. [DOI] [PubMed] [Google Scholar]
- 61.Abeyama K, Stern DM, Ito Y, Kawahara K, Yoshimoto Y, Tanaka M, Uchimura T, Ida N, Yamazaki Y, Yamada S, Yamamoto Y, Yamamoto H, Iino S, Taniguchi N, Maruyama I. The N-terminal domain of thrombomodulin sequesters high-mobility group-B1 protein, a novel antiinflammatory mechanism. J. Clin. Invest. 2005;115:1267–1274. doi: 10.1172/JCI22782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Urbonaviciute V, Furnrohr BG, Weber C, Haslbeck M, Wilhelm S, Herrmann M, Voll RE. Factors masking HMGB1 in human serum and plasma. J. Leukoc. Biol. 2007;81:67–74. doi: 10.1189/jlb.0306196. [DOI] [PubMed] [Google Scholar]
- 63.Sha Y, Zmijewski J, Xu Z, Abraham E. HMGB1 develops enhanced proinflammatory activity by binding to cytokines. J. Immunol. 2008;180:2531–2537. doi: 10.4049/jimmunol.180.4.2531. [DOI] [PubMed] [Google Scholar]
- 64.Urbonaviciute V, Furnrohr BG, Meister S, Munoz L, Heyder P, De Marchis F, Bianchi ME, Kirschning C, Wagner H, Manfredi AA, Kalden JR, Schett G, Rovere-Querini P, Herrmann M, Voll RE. Induction of inflammatory and immune responses by HMGB1-nucleosome complexes: implications for the pathogenesis of SLE. J. Exp. Med. 2008;205:3007–3018. doi: 10.1084/jem.20081165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Park JS, Svetkauskaite D, He Q, Kim JY, Strassheim D, Ishizaka A, Abraham E. Involvement of TLR 2 and TLR 4 in cellular activation by high mobility group box 1 protein (HMGB1) J. Biol. Chem. 2004;279:7370–7377. doi: 10.1074/jbc.M306793200. [DOI] [PubMed] [Google Scholar]
- 66.Yu M, Wang H, Ding A, Golenbock DT, Latz E, Czura CJ, Fenton MJ, Tracey KJ, Yang H. HMGB1 signals through Toll-like receptor (TLR) 4 and TLR2. Shock. 2006;26:174–179. doi: 10.1097/01.shk.0000225404.51320.82. [DOI] [PubMed] [Google Scholar]
- 67.Park JS, Gamboni-Robertson F, He Q, Svetkauskaite D, Kim JY, Strassheim D, Sohn JW, Yamada S, Maruyama I, Banerjee A, Ishizaka A, Abraham E. High mobility group box 1 protein interacts with multiple Toll-like receptors. Am. J. Physiol. Cell Physiol. 2006;290:C917–C924. doi: 10.1152/ajpcell.00401.2005. [DOI] [PubMed] [Google Scholar]
- 68.Kokkola R, Andersson A, Mullins G, Ostberg T, Treutiger CJ, Arnold B, Nawroth P, Andersson U, Harris RA, Harris HE. RAGE is the Major Receptor for the Proinflammatory Activity of HMGB1 in Rodent Macrophages. Scand. J. Immunol. 2005;61:1–9. doi: 10.1111/j.0300-9475.2005.01534.x. [DOI] [PubMed] [Google Scholar]
- 69.Pedrazzi M, Patrone M, Passalacqua M, Ranzato E, Colamassaro D, Sparatore B, Pontremoli S, Melloni E. Selective proinflammatory activation of astrocytes by high-mobility group box 1 protein signaling. J. Immunol. 2007;179:8525–8532. doi: 10.4049/jimmunol.179.12.8525. [DOI] [PubMed] [Google Scholar]
- 70.Fiuza C, Bustin M, Talwar S, Tropea M, Gerstenberger E, Shelhamer JH, Suffredini AF. Inflammation-promoting activity of HMGB1 on human microvascular endothelial cells. Blood. 2003;101:2652–2660. doi: 10.1182/blood-2002-05-1300. [DOI] [PubMed] [Google Scholar]
- 71.Treutiger CJ, Mullins GE, Johansson AS, Rouhiainen A, Rauvala HM, Erlandsson-Harris H, Andersson U, Yang H, Tracey KJ, Andersson J, Palmblad JE. High mobility group 1 B-box mediates activation of human endothelium. J. Intern. Med. 2003;254:375–385. doi: 10.1046/j.1365-2796.2003.01204.x. [DOI] [PubMed] [Google Scholar]
- 72.Lv B, Wang H, Tang Y, Fan Z, Xiao X, Chen F. High-mobility group box 1 protein induces tissue factor expression in vascular endothelial cells via activation of NF-kappaB and Egr-1. Thromb. Haemost. 2009;102:352–359. doi: 10.1160/TH08-11-0759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Yang H, Ochani M, Li J, Qiang X, Tanovic M, Harris HE, Susarla SM, Ulloa L, Wang H, DiRaimo R, Czura CJ, Wang H, Roth J, Warren HS, Fink MP, Fenton MJ, Andersson U, Tracey KJ. Reversing established sepsis with antagonists of endogenous high-mobility group box 1. Proc. Natl. Acad. Sci. USA. 2004;101:296–301. doi: 10.1073/pnas.2434651100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kokkola R, Li J, Sundberg E, Aveberger AC, Palmblad K, Yang H, Tracey KJ, Andersson U, Harris HE. Successful treatment of collagen-induced arthritis in mice and rats by targeting extracellular high mobility group box chromosomal protein 1 activity. Arthritis Rheum. 2003;48:2052–2058. doi: 10.1002/art.11161. [DOI] [PubMed] [Google Scholar]
- 75.Yang H, Wang H, Tracey KJ. HMG-1 rediscovered as a cytokine. Shock. 2001;15:247–253. doi: 10.1097/00024382-200115040-00001. [DOI] [PubMed] [Google Scholar]
- 76.Messmer D, Yang H, Telusma G, Knoll F, Li J, Messmer B, Tracey KJ, Chiorazzi N. High mobility group box protein 1: an endogenous signal for dendritic cell maturation and Th1 polarization. J. Immunol. 2004;173:307–313. doi: 10.4049/jimmunol.173.1.307. [DOI] [PubMed] [Google Scholar]
- 77.Kazama H, Ricci JE, Herndon JM, Hoppe G, Green DR, Ferguson TA. Induction of immunological tolerance by apoptotic cells requires caspase-dependent oxidation of high-mobility group box-1 protein. Immunity. 2008;29:21–32. doi: 10.1016/j.immuni.2008.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Rauvala H, Rouhiainen A. RAGE as a receptor of HMGB1 (Amphoterin): roles in health and disease. Curr. Mol. Med. 2007;7:725–734. doi: 10.2174/156652407783220750. [DOI] [PubMed] [Google Scholar]
- 79.Dintilhac A, Bernues J. HMGB1 interacts with many apparently unrelated proteins by recognizing short amino acid sequences. J. Biol. Chem. 2002;277:7021–7028. doi: 10.1074/jbc.M108417200. [DOI] [PubMed] [Google Scholar]
- 80.Jiao Y, Wang HC, Fan SJ. Growth suppression and radiosensitivity increase by HMGB1 in breast cancer. Acta. Pharmacol. Sin. 2007;28:1957–1967. doi: 10.1111/j.1745-7254.2007.00669.x. [DOI] [PubMed] [Google Scholar]
- 81.Liu G, Wang J, Park YJ, Tsuruta Y, Lorne EF, Zhao X, Abraham E. High Mobility Group Protein-1 Inhibits Phagocytosis of Apoptotic Neutrophils through Binding to Phosphatidylserine. J. Immunol. 2008;181:4240–4246. doi: 10.4049/jimmunol.181.6.4240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Bell CW, Jiang W, Reich CF, Pisetsky DS. The Extracellular Release of HMGB1 during Apoptotic Cell Death. Am. J. Physiol. Cell Physiol. 2006;291:C1318–C1325. doi: 10.1152/ajpcell.00616.2005. [DOI] [PubMed] [Google Scholar]
- 83.Tracey KJ, Fong Y, Hesse DG, Manogue KR, Lee AT, Kuo GC, Lowry SF, Cerami A. Anti-cachectin/TNF monoclonal antibodies prevent septic shock during lethal bacteraemia. Nature. 1987;330:662–664. doi: 10.1038/330662a0. [DOI] [PubMed] [Google Scholar]
- 84.Dinarello CA, Thompson RC. Blocking IL-1: interleukin 1 receptor antagonist in vivo and in vitro. Immunol. Today. 1991;12:404–410. doi: 10.1016/0167-5699(91)90142-G. [DOI] [PubMed] [Google Scholar]
- 85.Heinzel FP. The role of IFN-gamma in the pathology of experimental endotoxemia. J. Immunol. 1990;145:2920–2924. [PubMed] [Google Scholar]
- 86.Calandra T, Echtenacher B, Roy DL, Pugin J, Metz CN, Hultner L, Heumann D, Mannel D, Bucala R, Glauser MP. Protection from septic shock by neutralization of macrophage migration inhibitory factor. Nat. Med. 2000;6:164–170. doi: 10.1038/72262. [DOI] [PubMed] [Google Scholar]
- 87.Bozza M, Satoskar AR, Lin G, Lu B, Humbles AA, Gerard C, David JR. Targeted disruption of migration inhibitory factor gene reveals its critical role in sepsis. J. Exp. Med. 1999;189:341–346. doi: 10.1084/jem.189.2.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Wichterman KA, Baue AE, Chaudry IH. Sepsis and septic shock--a review of laboratory models and a proposal. J. Surg. Res. 1980;29:189–201. doi: 10.1016/0022-4804(80)90037-2. [DOI] [PubMed] [Google Scholar]
- 89.Lang CH, Silvis C, Deshpande N, Nystrom G, Frost RA. Endotoxin stimulates in vivo expression of inflammatory cytokines tumor necrosis factor alpha, interleukin-1beta, −6, and high-mobility-group protein-1 in skeletal muscle. Shock. 2003;19:538–546. doi: 10.1097/01.shk.0000055237.25446.80. [DOI] [PubMed] [Google Scholar]
- 90.Fang WH, Yao YM, Shi ZG, Yu Y, Wu Y, Lu LR, Sheng ZY. The significance of changes in high mobility group-1 protein mRNA expression in rats after thermal injury. Shock. 2002;17:329–333. doi: 10.1097/00024382-200204000-00016. [DOI] [PubMed] [Google Scholar]
- 91.Wang H, Yang H, Czura CJ, Sama AE, Tracey KJ. HMGB1 as a Late Mediator of Lethal Systemic Inflammation. Am. J. Respir. Crit. Care Med. 2001;164:1768–1773. doi: 10.1164/ajrccm.164.10.2106117. [DOI] [PubMed] [Google Scholar]
- 92.Sunden-Cullberg J, Norrby-Teglund A, Rouhiainen A, Rauvala H, Herman G, Tracey KJ, Lee ML, Andersson J, Tokics L, Treutiger CJ. Persistent elevation of high mobility group box-1 protein (HMGB1) in patients with severe sepsis and septic shock. Crit. Care Med. 2005;33:564–573. doi: 10.1097/01.ccm.0000155991.88802.4d. [DOI] [PubMed] [Google Scholar]
- 93.Angus DC, Yang L, Kong L, Kellum JA, Delude RL, Tracey KJ, Weissfeld L. Circulating high-mobility group box 1 (HMGB1) concentrations are elevated in both uncomplicated pneumonia and pneumonia with severe sepsis. Crit. Care Med. 2007;35:1061–1067. doi: 10.1097/01.CCM.0000259534.68873.2A. [DOI] [PubMed] [Google Scholar]
- 94.O'Connor KA, Hansen MK, Rachal PC, Deak MM, Biedenkapp JC, Milligan ED, Johnson JD, Wang H, Maier SF, Tracey KJ, Watkins LR. Further characterization of high mobility group box 1 (HMGB1) as a proinflammatory cytokine: central nervous system effects. Cytokine. 2003;24:254–265. doi: 10.1016/j.cyto.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 95.Sappington PL, Yang R, Yang H, Tracey KJ, Delude RL, Fink MP. HMGB1 B box increases the permeability of Caco-2 enterocytic monolayers and impairs intestinal barrier function in mice. Gastroenterology. 2002;123:790–802. doi: 10.1053/gast.2002.35391. [DOI] [PubMed] [Google Scholar]
- 96.Abraham E, Arcaroli J, Carmody A, Wang H, Tracey KJ. HMG-1 as a mediator of acute lung inflammation. J. Immunol. 2000;165:2950–2954. doi: 10.4049/jimmunol.165.6.2950. [DOI] [PubMed] [Google Scholar]
- 97.Ueno H, Matsuda T, Hashimoto S, Amaya F, Kitamura Y, Tanaka M, Kobayashi A, Maruyama I, Yamada S, Hasegawa N, Soejima J, Koh H, Ishizaka A. Contributions of high mobility group box protein in experimental and clinical acute lung injury. Am. J. Respir. Crit Care Med. 2004;170:1310–1316. doi: 10.1164/rccm.200402-188OC. [DOI] [PubMed] [Google Scholar]
- 98.Lin X, Yang H, Sakuragi T, Hu M, Mantell LL, Hayashi S, Al Abed Y, Tracey KJ, Ulloa L, Miller EJ. {alpha}-Chemokine receptor blockade reduces high mobility group box 1 protein-induced lung inflammation and injury and improves survival in sepsis. Am. J. Physiol. Lung Cell Mol. Physiol. 2005;289:L583–L590. doi: 10.1152/ajplung.00091.2005. [DOI] [PubMed] [Google Scholar]
- 99.Rowe SM, Jackson PL, Liu G, Hardison M, Livraghi A, Solomon GM, McQuaid DB, Noerager BD, Gaggar A, Clancy J, O’Neal W, Sorscher EJ, Abraham E, Blalock JE. Potential Role of High Mobility Group Box 1 in Cystic Fibrosis Airway Disease. Am. J. Respir. Crit. Care Med. 2008;178:822–831. doi: 10.1164/rccm.200712-1894OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Agnello D, Wang H, Yang H, Tracey KJ, Ghezzi P. HMGB1, a DNA-binding protein with cytokine activity, induces brain TNF and IL-6 production, and mediates anorexia and taste aversion. Cytokine. 2002;18:231–236. doi: 10.1006/cyto.2002.0890. [DOI] [PubMed] [Google Scholar]
- 101.Pedrazzi M, Raiteri L, Bonanno G, Patrone M, Ledda S, Passalacqua M, Milanese M, Melloni E, Raiteri M, Pontremoli S, Sparatore B. Stimulation of excitatory amino acid release from adult mouse brain glia subcellular particles by high mobility group box 1 protein. J. Neurochem. 2006;99:827–838. doi: 10.1111/j.1471-4159.2006.04120.x. [DOI] [PubMed] [Google Scholar]
- 102.Chacur M, Milligan ED, Gazda LS, Armstrong C, Wang H, Tracey KJ, Maier SF, Watkins LR. A new model of sciatic inflammatory neuritis (SIN): induction of unilateral and bilateral mechanical allodynia following acute unilateral peri-sciatic immune activation in rats. Pain. 2001;94:231–244. doi: 10.1016/S0304-3959(01)00354-2. [DOI] [PubMed] [Google Scholar]
- 103.Yang R, Miki K, Oksala N, Nakao A, Lindgren L, Killeen ME, Mennander A, Fink MP, Tenhunen J. Bile high-mobility group box 1 contributes to gut barrier dysfunction in experimental endotoxemia. Am. J. Physiol Regul. Integr. Comp. Physiol. 2009;297:R362–R369. doi: 10.1152/ajpregu.00184.2009. [DOI] [PubMed] [Google Scholar]
- 104.Qin S, Wang H, Yuan R, Li H, Ochani M, Ochani K, Rosas-Ballina M, Czura CJ, Huston JM, Miller E, Lin X, Sherry B, Kumar A, Larosa G, Newman W, Tracey KJ, Yang H. Role of HMGB1 in apoptosis-mediated sepsis lethality. J Exp. Med. 2006;203:1637–1642. doi: 10.1084/jem.20052203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Kaczorowski DJ, Tsung A, Billiar TR. Innate immune mechanisms in ischemia/reperfusion. Front Biosci. (Elite. Ed) 2009;1:91–98. doi: 10.2741/E10. [DOI] [PubMed] [Google Scholar]
- 106.Yang R, Harada T, Mollen KP, Prince JM, Levy RM, Englert JA, Gallowitsch-Puerta M, Yang L, Yang H, Tracey KJ, Harbrecht BG, Billiar TR, Fink MP. Anti-HMGB1 neutralizing antibody ameliorates gut barrier dysfunction and improves survival after hemorrhagic shock. Mol. Med. 2006;12:105–114. doi: 10.2119/2006-00010.Yang. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Peltz ED, Moore EE, Eckels PC, Damle SS, Tsuruta Y, Johnson JL, Sauaia A, Silliman CC, Banerjee A, Abraham E. HMGB1 is markedly elevated within 6 hours of mechanical trauma in humans. Shock. 2009;32:17–22. doi: 10.1097/shk.0b013e3181997173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Wu H, Chen G, Wyburn KR, Yin J, Bertolino P, Eris JM, Alexander SI, Sharland AF, Chadban SJ. TLR4 activation mediates kidney ischemia/reperfusion injury. J. Clin. Invest. 2007;117:2847–2859. doi: 10.1172/JCI31008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Liu K, Mori S, Takahashi HK, Tomono Y, Wake H, Kanke T, Sato Y, Hiraga N, Adachi N, Yoshino T, Nishibori M. Anti-high mobility group box 1 monoclonal antibody ameliorates brain infarction induced by transient ischemia in rats. FASEB J. 2007;21:3904–3916. doi: 10.1096/fj.07-8770com. [DOI] [PubMed] [Google Scholar]
- 110.Tsung A, Sahai R, Tanaka H, Nakao A, Fink MP, Lotze MT, Yang H, Li J, Tracey KJ, Geller DA, Billiar TR. The nuclear factor HMGB1 mediates hepatic injury after murine liver ischemia-reperfusion. J. Exp. Med. 2005;201:1135–1143. doi: 10.1084/jem.20042614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Tsung A, Klune JR, Zhang X, Jeyabalan G, Cao Z, Peng X, Stolz DB, Geller DA, Rosengart MR, Billiar TR. HMGB1 release induced by liver ischemia involves Toll-like receptor 4 dependent reactive oxygen species production and calcium-mediated signaling. J. Exp. Med. 2007;204:2913–2923. doi: 10.1084/jem.20070247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Watanabe T, Kubota S, Nagaya M, Ozaki S, Nagafuchi H, Akashi K, Taira Y, Tsukikawa S, Oowada S, Nakano S. The role of HMGB-1 on the development of necrosis during hepatic ischemia and hepatic ischemia/reperfusion injury in mice. J. Surg. Res. 2005;124:59–66. doi: 10.1016/j.jss.2004.10.019. [DOI] [PubMed] [Google Scholar]
- 113.Andrassy M, Volz HC, Igwe JC, Funke B, Eichberger SN, Kaya Z, Buss S, Autschbach F, Pleger ST, Lukic IK, Bea F, Hardt SE, Humpert PM, Bianchi ME, Mairbaurl H, Nawroth PP, Remppis A, Katus HA, Bierhaus A. High-mobility group box-1 in ischemia-reperfusion injury of the heart. Circulation. 2008;117:3216–3226. doi: 10.1161/CIRCULATIONAHA.108.769331. [DOI] [PubMed] [Google Scholar]
- 114.Liu K, Mori S, Takahashi HK, Tomono Y, Wake H, Kanke T, Sato Y, Hiraga N, Adachi N, Yoshino T, Nishibori M. Anti-high mobility group box 1 monoclonal antibody ameliorates brain infarction induced by transient ischemia in rats. FASEB J. 2007;21:3904–3916. doi: 10.1096/fj.07-8770com. [DOI] [PubMed] [Google Scholar]
- 115.Muhammad S, Barakat W, Stoyanov S, Murikinati S, Yang H, Tracey KJ, Bendszus M, Rossetti G, Nawroth PP, Bierhaus A, Schwaninger M. The HMGB1 receptor RAGE mediates ischemic brain damage. J. Neurosci. 2008;28:12023–12031. doi: 10.1523/JNEUROSCI.2435-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Zeng S, Dun H, Ippagunta N, Rosario R, Zhang QY, Lefkowitch J, Yan SF, Schmidt AM, Emond JC. Receptor for advanced glycation end product (RAGE)-dependent modulation of early growth response-1 in hepatic ischemia/reperfusion injury. J. Hepatol. 2009;50:929–936. doi: 10.1016/j.jhep.2008.11.022. [DOI] [PubMed] [Google Scholar]
- 117.Ogawa EN, Ishizaka A, Tasaka S, Koh H, Ueno H, Amaya F, Ebina M, Yamada S, Funakoshi Y, Soejima J, Moriyama K, Kotani T, Hashimoto S, Morisaki H, Abraham E, Takeda J. Contribution of high-mobility group box-1 to the development of ventilator-induced lung injury. Am. J. Respir. Crit. Care Med. 2006;174:400–407. doi: 10.1164/rccm.200605-699OC. [DOI] [PubMed] [Google Scholar]
- 118.Sawa H, Ueda T, Takeyama Y, Yasuda T, Shinzeki M, Nakajima T, Kuroda Y. Blockade of high mobility group box-1 protein attenuates experimental severe acute pancreatitis. World J. Gastroenterol. 2006;12:7666–7670. doi: 10.3748/wjg.v12.i47.7666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Kohno T, Anzai T, Naito K, Miyasho T, Okamoto M, Yokota H, Yamada S, Maekawa Y, Takahashi T, Yoshikawa T, Ishizaka A, Ogawa S. Role of high-mobility group box 1 protein in post-infarction healing process and left ventricular remodelling. Cardiovasc. Res. 2009;81:565–573. doi: 10.1093/cvr/cvn291. [DOI] [PubMed] [Google Scholar]
- 120.Li W, Sama AE, Wang H. Role of HMGB1 in cardiovascular diseases. Curr. Opin. Pharmacol. 2006;6:130–135. doi: 10.1016/j.coph.2005.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Takahashi K, Fukushima S, Yamahara K, Yashiro K, Shintani Y, Coppen SR, Salem HK, Brouilette SW, Yacoub MH, Suzuki K. Modulated inflammation by injection of high-mobility group box 1 recovers post-infarction chronically failing heart. Circulation. 2008;118:S106–S114. doi: 10.1161/CIRCULATIONAHA.107.757443. [DOI] [PubMed] [Google Scholar]
- 122.Hagiwara S, Iwasaka H, Hasegawa A, Asai N, Noguchi T. High-dose intravenous immunoglobulin G improves systemic inflammation in a rat model of CLP-induced sepsis. Intensive Care Med. 2008;34:1812–1819. doi: 10.1007/s00134-008-1161-1. [DOI] [PubMed] [Google Scholar]
- 123.Abraham E, Reinhart K, Opal S, Demeyer I, Doig C, Rodriguez AL, Beale R, Svoboda P, Laterre PF, Simon S, Light B, Spapen H, Stone J, Seibert A, Peckelsen C, De Deyne C, Postier R, Pettila V, Artigas A, Percell SR, Shu V, Zwingelstein C, Tobias J, Poole L, Stolzenbach JC, Creasey AA. Efficacy and safety of tifacogin (recombinant tissue factor pathway inhibitor) in severe sepsis: a randomized controlled trial. JAMA. 2003;290:238–247. doi: 10.1001/jama.290.2.238. [DOI] [PubMed] [Google Scholar]
- 124.Hagiwara S, Iwasaka H, Matsumoto S, Noguchi T. High dose antithrombin III inhibits HMGB1 and improves endotoxin-induced acute lung injury in rats. Intensive Care Med. 2008;34:361–367. doi: 10.1007/s00134-007-0887-5. [DOI] [PubMed] [Google Scholar]
- 125.Nagato M, Okamoto K, Abe Y, Higure A, Yamaguchi K. Recombinant human soluble thrombomodulin decreases the plasma high-mobility group box-1 protein levels, whereas improving the acute liver injury and survival rates in experimental endotoxemia. Crit. Care Med. 2009;37:2181–2186. doi: 10.1097/CCM.0b013e3181a55184. [DOI] [PubMed] [Google Scholar]
- 126.Hagiwara S, Iwasaka H, Hasegawa A, Koga H, Noguchi T. Effects of hyperglycemia and insulin therapy on high mobility group box 1 in endotoxin-induced acute lung injury in a rat model. Crit. Care Med. 2008;36:2407–2413. doi: 10.1097/CCM.0b013e318180b3ba. [DOI] [PubMed] [Google Scholar]
- 127.Chorny A, Delgado M. Neuropeptides rescue mice from lethal sepsis by down-regulating secretion of the late-acting inflammatory mediator high mobility group box 1. Am. J. Pathol. 2008;172:1297–1307. doi: 10.2353/ajpath.2008.070969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Wang H, Zhu S, Ward MF, Gong J, Sama AE. Hyperglycemia aggravates endotoxin-induced high mobility group box 1 protein release: yet another reason not to be too sweet. Crit. Care Med. 2008;36:2475–2476. doi: 10.1097/CCM.0b013e318181159c. [DOI] [PubMed] [Google Scholar]
- 129.Tang Y, Lv B, Wang H, Zuo X, Xiao X. PACAP inhibit the release and cytokine activity of HMGB1 and improve the survival during lethal endotoxemia. Int. Immunopharmacol. 2008;8:1646–1651. doi: 10.1016/j.intimp.2008.07.014. [DOI] [PubMed] [Google Scholar]
- 130.Wu R, Dong W, Zhou M, Zhang F, Marini CP, Ravikumar TS, Wang P. Ghrelin attenuates sepsis-induced acute lung injury and mortality in rats. Am. J. Respir. Crit. Care Med. 2007;176:805–813. doi: 10.1164/rccm.200604-511OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Wu R, Dong W, Cui X, Zhou M, Simms HH, Ravikumar TS, Wang P. Ghrelin down-regulates proinflammatory cytokines in sepsis through activation of the vagus nerve. Ann. Surg. 2007;245:480–486. doi: 10.1097/01.sla.0000251614.42290.ed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Chorny A, Anderson P, Gonzalez-Rey E, Delgado M. Ghrelin Protects against Experimental Sepsis by Inhibiting High-Mobility Group Box 1 Release and by Killing Bacteria. J. Immunol. 2008;180:8369–8377. doi: 10.4049/jimmunol.180.12.8369. [DOI] [PubMed] [Google Scholar]
- 133.Wu R, Dong W, Qiang X, Wang H, Blau SA, Ravikumar TS, Wang P. Orexigenic hormone ghrelin ameliorates gut barrier dysfunction in sepsis in rats. Crit. Care Med. 2009;37:2421–2426. doi: 10.1097/CCM.0b013e3181a557a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Borovikova LV, Ivanova S, Zhang M, Yang H, Botchkina GI, Watkins LR, Wang H, Abumrad N, Eaton JW, Tracey KJ. Vagus nerve stimulation attenuates the systemic inflammatory response to endotoxin. Nature. 2000;405:458–462. doi: 10.1038/35013070. [DOI] [PubMed] [Google Scholar]
- 135.Huston JM, Ochani M, Rosas-Ballina M, Liao H, Ochani K, Pavlov VA, Gallowitsch-Puerta M, Ashok M, Czura CJ, Foxwell B, Tracey KJ, Ulloa L. Splenectomy inactivates the cholinergic antiinflammatory pathway during lethal endotoxemia and polymicrobial sepsis. J. Exp. Med. 2006;203:1623–1628. doi: 10.1084/jem.20052362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Huston JM, Gallowitsch-Puerta M, Ochani M, Ochani K, Yuan R, Rosas-Ballina M, Ashok M, Goldstein RS, Chavan S, Pavlov VA, Metz CN, Yang H, Czura CJ, Wang H, Tracey KJ. Transcutaneous vagus nerve stimulation reduces serum high mobility group box 1 levels and improves survival in murine sepsis. Crit. Care Med. 2007;35:2762–2768. doi: 10.1097/01.CCM.0000288102.15975.BA. [DOI] [PubMed] [Google Scholar]
- 137.Wang H, Liao H, Ochani M, Justiniani M, Lin X, Yang L, Al Abed Y, Wang H, Metz C, Miller EJ, Tracey KJ, Ulloa L. Cholinergic agonists inhibit HMGB1 release and improve survival in experimental sepsis. Nat. Med. 2004;10:1216–1221. doi: 10.1038/nm1124. [DOI] [PubMed] [Google Scholar]
- 138.Pavlov VA, Ochani M, Yang LH, Gallowitsch-Puerta M, Ochani K, Lin X, Levi J, Parrish WR, Rosas-Ballina M, Czura CJ, Larosa GJ, Miller EJ, Tracey KJ, Al Abed Y. Selective alpha7-nicotinic acetylcholine receptor agonist GTS-21 improves survival in murine endotoxemia and severe sepsis. Crit. Care Med. 2007;35:1139–1144. doi: 10.1097/01.CCM.0000259381.56526.96. [DOI] [PubMed] [Google Scholar]
- 139.Parrish WR, Rosas-Ballina M, Gallowitsch-Puerta M, Ochani M, Ochani K, Yang LH, Hudson L, Lin X, Patel N, Johnson SM, Chavan S, Goldstein RS, Czura CJ, Miller EJ, Al Abed Y, Tracey KJ, Pavlov VA. Modulation of TNF release by choline requires alpha7 subunit nicotinic acetylcholine receptor-mediated signaling. Mol. Med. 2008;14:567–574. doi: 10.2119/2008-00079.Parrish. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Yan JJ, Jung JS, Lee JE, Lee J, Huh SO, Kim HS, Jung KC, Cho JY, Nam JS, Suh HW, Kim YH, Song DK. Therapeutic effects of lysophosphatidylcholine in experimental sepsis. Nat. Med. 2004;10:161–167. doi: 10.1038/nm989. [DOI] [PubMed] [Google Scholar]
- 141.Wang H, Czura CJ, Tracey KJ. Lipid unites disparate syndromes of sepsis. Nat. Med. 2004;10:124–125. doi: 10.1038/nm0204-124. [DOI] [PubMed] [Google Scholar]
- 142.Zhu S, Li W, Li J, Sama AE, Wang H. Caging a beast in the inflammation arena: use of Chinese medicinal herbs to inhibit a late mediator of lethal sepsis, HMGB1. Intern. J. Clin. Exp. Med. 2008;1:64–79. [PMC free article] [PubMed] [Google Scholar]
- 143.Li W, Ashok M, Li J, Yang H, Sama AE, Wang H. A Major Ingredient of Green Tea Rescues Mice from Lethal Sepsis Partly by Inhibiting HMGB1. PLoS ONE. 2007;2:e1153. doi: 10.1371/journal.pone.0001153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Wheeler DS, Lahni PM, Hake PW, Denenberg AG, Wong HR, Snead C, Catravas JD, Zingarelli B. The green tea polyphenol epigallocatechin-3-gallate improves systemic hemodynamics and survival in rodent models of polymicrobial sepsis. Shock. 2007;28:353–359. doi: 10.1097/shk.0b013e3180485823. [DOI] [PubMed] [Google Scholar]
- 145.Osuchowski MF, Welch K, Siddiqui J, Remick DG. Circulating cytokine/inhibitor profiles reshape the understanding of the SIRS/CARS continuum in sepsis and predict mortality. J. Immunol. 2006;177:1967–1974. doi: 10.4049/jimmunol.177.3.1967. [DOI] [PubMed] [Google Scholar]
- 146.Ji XY, Tan BK, Zhu YZ. Salvia miltiorrhiza and ischemic diseases. Acta Pharmacol. Sin. 2000;21:1089–1094. [PubMed] [Google Scholar]
- 147.Cheng TO. Cardiovascular effects of Danshen. Int. J. Cardiol. 2007;121:9–22. doi: 10.1016/j.ijcard.2007.01.004. [DOI] [PubMed] [Google Scholar]
- 148.Fink MP. Ethyl pyruvate: a novel treatment for sepsis. Curr. Drug Targets. 2007;8:515–518. [PubMed] [Google Scholar]
- 149.Ulloa L, Ochani M, Yang H, Tanovic M, Halperin D, Yang R, Czura CJ, Fink MP, Tracey KJ. Ethyl pyruvate prevents lethality in mice with established lethal sepsis and systemic inflammation. Proc. Natl. Acad. Sci. USA. 2002;99:12351–12356. doi: 10.1073/pnas.192222999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Pan P, Cardinal J, Dhupar R, Rosengart MR, Lotze MT, Geller DA, Billiar TR, Tsung A. Low-dose cisplatin administration in murine cecal ligation and puncture prevents the systemic release of HMGB1 and attenuates lethality. J. Leukoc. Biol. 2009;86:625–632. doi: 10.1189/JLB.1108713. [DOI] [PubMed] [Google Scholar]
- 151.Zhang M, Wang H, Tracey KJ. Regulation of macrophage activation and inflammation by spermine: a new chapter in an old story. Crit. Care Med. 2000;28:N60–N66. doi: 10.1097/00003246-200004001-00007. [DOI] [PubMed] [Google Scholar]
- 152.Zhang M, Caragine T, Wang H, Cohen PS, Botchkina G, Soda K, Bianchi M, Ulrich P, Cerami A, Sherry B, Tracey KJ. Spermine inhibits proinflammatory cytokine synthesis in human mononuclear cells: a counterregulatory mechanism that restrains the immune response. J. Exp. Med. 1997;185:1759–1768. doi: 10.1084/jem.185.10.1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Zhang M, Borovikova LV, Wang H, Metz C, Tracey KJ. Spermine inhibition of monocyte activation and inflammation. Mol. Med. 1999;5:595–605. [PMC free article] [PubMed] [Google Scholar]
- 154.Wang H, Zhang M, Bianchi M, Sherry B, Sama A, Tracey KJ. Fetuin (alpha2-HS-glycoprotein) opsonizes cationic macrophagedeactivating molecules. Proc. Natl. Acad. Sci. USA. 1998;95:14429–14434. doi: 10.1073/pnas.95.24.14429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Zhu S, Ashok M, Li J, Li W, Yang H, Wang P, Tracey KJ, Sama AE, Wang H. Spermine protects mice against lethal sepsis partly by attenuating surrogate inflammatory markers. Mol. Med. 2009;15:275–282. doi: 10.2119/molmed.2009.00062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Cardinal J, Pan P, Dhupar R, Ross M, Nakao A, Lotze M, Billiar T, Geller D, Tsung A. Cisplatin prevents high mobility group box 1 release and is protective in a murine model of hepatic ischemia/reperfusion injury. Hepatology. 2009;50:565–574. doi: 10.1002/hep.23021. [DOI] [PubMed] [Google Scholar]
- 157.Wang Q, Ding Q, Zhou Y, Gou X, Hou L, Chen S, Zhu Z, Xiong L. Ethyl pyruvate attenuates spinal cord ischemic injury with a wide therapeutic window through inhibiting high-mobility group box 1 release in rabbits. Anesthesiology. 2009;110:1279–1286. doi: 10.1097/ALN.0b013e3181a160d6. [DOI] [PubMed] [Google Scholar]
- 158.Chung KY, Park JJ, Kim YS. The role of high-mobility group box-1 in renal ischemia and reperfusion injury and the effect of ethyl pyruvate. Transplant. Proc. 2008;40:2136–2138. doi: 10.1016/j.transproceed.2008.06.040. [DOI] [PubMed] [Google Scholar]
- 159.Mabuchi A, Wake K, Marlini M, Watanabe H, Wheatley AM. Protection by glycyrrhizin against warm ischemia-reperfusion-induced cellular injury and derangement of the microcirculatory blood flow in the rat liver. Microcirculation. 2009;16:364–376. doi: 10.1080/10739680902796917. [DOI] [PubMed] [Google Scholar]
- 160.Hayakawa K, Mishima K, Irie K, Hazekawa M, Mishima S, Fujioka M, Orito K, Egashira N, Katsurabayashi S, Takasaki K, Iwasaki K, Fujiwara M. Cannabidiol prevents a post-ischemic injury progressively induced by cerebral ischemia via a high-mobility group box1-inhibiting mechanism. Neuropharmacology. 2008;55:1280–1286. doi: 10.1016/j.neuropharm.2008.06.040. [DOI] [PubMed] [Google Scholar]
- 161.Mantell LL, Parrish WR, Ulloa L. Hmgb-1 as a therapeutic target for infectious and inflammatory disorders. Shock. 2006;25:4–11. doi: 10.1097/01.shk.0000188710.04777.9e. [DOI] [PubMed] [Google Scholar]
- 162.Wang H, Yang H, Tracey KJ. Extracellular role of HMGB1 in inflammation and sepsis. J Intern. Med. 2004;255:320–331. doi: 10.1111/j.1365-2796.2003.01302.x. [DOI] [PubMed] [Google Scholar]
- 163.Beutler B, Milsark IW, Cerami AC. Passive immunization against cachectin/tumor necrosis factor protects mice from lethal effect of endotoxin. Science. 1985;229:869–871. doi: 10.1126/science.3895437. [DOI] [PubMed] [Google Scholar]
- 164.Ziegler EJ, Fisher CJ, Jr, Sprung CL, Straube RC, Sadoff JC, Foulke GE, Wortel CH, Fink MP, Dellinger RP, Teng NN. Treatment of gram-negative bacteremia and septic shock with HA-1A human monoclonal antibody against endotoxin. A randomized, double-blind, placebo-controlled trial. The HA-1A Sepsis Study Group. N. Engl. J. Med. 1991;324:429–436. doi: 10.1056/NEJM199102143240701. [DOI] [PubMed] [Google Scholar]
- 165.Ziegler EJ, McCutchan JA, Fierer J, Glauser MP, Sadoff JC, Douglas H, Braude AI. Treatment of gram-negative bacteremia and shock with human antiserum to a mutant Escherichia coli. N. Engl. J. Med. 1982;307:1225–1230. doi: 10.1056/NEJM198211113072001. [DOI] [PubMed] [Google Scholar]
- 166.Abraham E, Wunderink R, Silverman H, Perl TM, Nasraway S, Levy H, Bone R, Wenzel RP, Balk R, Allred R. Efficacy and safety of monoclonal antibody to human tumor necrosis factor alpha in patients with sepsis syndrome. A randomized, controlled, double-blind, multicenter clinical trial. TNF-alpha MAb Sepsis Study Group. JAMA. 1995;273:934–941. [PubMed] [Google Scholar]
- 167.Cohen J. Adjunctive therapy in sepsis: a critical analysis of the clinical trial programme. Br. Med. Bull. 1999;55:212–225. doi: 10.1258/0007142991902222. [DOI] [PubMed] [Google Scholar]
- 168.Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, Reinhart K, Angus DC, Brun-Buisson C, Beale R, Calandra T, Dhainaut JF, Gerlach H, Harvey M, Marini JJ, Marshall J, Ranieri M, Ramsay G, Sevransky J, Thompson BT, Townsend S, Vender JS, Zimmerman JL, Vincent JL. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit. Care Med. 2008;36:296–327. doi: 10.1097/01.CCM.0000298158.12101.41. [DOI] [PubMed] [Google Scholar]
- 169.Wang H, Ward MF, Sama AE. Novel HMGB1-inhibiting therapeutic agents for experimental sepsis. Shock. 2009;32:348–357. doi: 10.1097/SHK.0b013e3181a551bd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Wu TW, Zeng LH, Fung KP, Wu J, Pang H, Grey AA, Weisel RD, Wang JY. Effect of sodium tanshinone IIA sulfonate in the rabbit myocardium and on human cardiomyocytes and vascular endothelial cells. Biochem. Pharmacol. 1993;46:2327–2332. doi: 10.1016/0006-2952(93)90624-6. [DOI] [PubMed] [Google Scholar]
- 171.Lam BY, Lo AC, Sun X, Luo HW, Chung SK, Sucher NJ. Neuroprotective effects of tanshinones in transient focal cerebral ischemia in mice. Phytomedicine. 2003;10:286–291. doi: 10.1078/094471103322004776. [DOI] [PubMed] [Google Scholar]
- 172.Dong K, Xu W, Yang J, Qiao H, Wu L. Neuroprotective effects of Tanshinone IIA on permanent focal cerebral ischemia in mice. Phytother. Res. 2009;23:608–613. doi: 10.1002/ptr.2615. [DOI] [PubMed] [Google Scholar]