Abstract
Objectives
Subthreshold depressive disorder is one of the best established risk factors for the onset of full-syndrome depressive disorders. However, many youths with subthreshold depressive disorder do not develop full-syndrome depression. We examined predictors of escalation to full-syndrome depressive disorders in a community sample of 225 adolescents with subthreshold depressive disorder.
Method
Criteria for subthreshold depressive disorder were an episode of depressed mood or loss of interest or pleasure lasting at least 1 week and at least two of the seven other DSM-IV-associated symptoms for major depression. Participants were assessed four times from mid-adolescence to age 30 years using semistructured diagnostic interviews.
Results
The estimated risk for escalation to full-syndrome depressive disorders was 67%. Five variables accounted for unique variance in predicting escalation: severity of depressive symptoms, medical conditions/symptoms, history of suicidal ideation, history of anxiety disorder, and familial loading for depression. Adolescents with three or more risk factors had an estimated 90% chance of escalating to full-syndrome depressive disorder, compared with 47% of adolescents with fewer than three risk factors.
Conclusions
These data may be useful in identifying a subgroup of youths with subthreshold depressive disorder who are at especially high risk for escalating to full-syndrome depressive disorders.
There is growing recognition of the significance of subthreshold depressive disorders in children, adolescents, and adults.1-3 These conditions have been referred to using a variety of terms (e.g., subthreshold depression, minor depression, recurrent brief depression, subsyndromal symptomatic depression) and defined in a variety of ways (e.g., minimum number of symptoms range from 2 to 4; minimum durations range from several days to 2 weeks).3,4
Despite the lack of consensus regarding terminology and criteria, subthreshold depressive disorders seem to be common in children and adolescents; the 12-month prevalence ranges from 3% to 7%,1,5,6 and the lifetime prevalence through late adolescence is as high as 26%.7 Subthreshold depressive disorder in youths is associated with substantial functional impairment 2,5,8 and a twofold to fourfold increase in the risk for developing full threshold depressive disorders.1,6,8-10
In light of these findings, prevention and early intervention programs often target youths with subthreshold depressive disorders.11,12 Although intervention may be indicated for youngsters with subthreshold depression who experience significant impairment regardless of their risk for escalation, the major goal of most such programs is to prevent the development of full-syndrome depression. However, many youths with subthreshold depression do not develop full-syndrome depressive disorders even after years of follow-up.1,2,6 Hence, it may be useful to identify factors that predict the escalation from subthreshold to full-syndrome depressive disorders to refine the selection of candidates for targeted early intervention.12 In addition, information about predictors of escalation in youths with subthreshold depressive disorder could provide clues regarding protective factors that might inform new interventions and suggest hypotheses about neurobiological and psychosocial processes involved in the transition between subthreshold and full-syndrome depressive states.
To our knowledge, only two studies have examined predictors of escalation from subthreshold to full-syndrome depressive disorders, both focusing on adults. Cuijpers et al.13 explored this issue in a 1-year follow-up of a sample of adults in primary care. Subthreshold depression was defined as endorsing at least one core and three depressive symptoms in a screening interview but failing to meet criteria for a mood disorder in a structured diagnostic interview. Severity of depressive symptoms, family history of depression, and having a chronic general medical illness predicted the subsequent onset of major depressive disorder (MDD). Cuijpers et al.14 examined a community sample of older adults with elevated scores on a self-report screening inventory who did not meet criteria for MDD or dysthymia. They found that low appetite and trouble sleeping predicted the onset of MDD or dysthymic disorder within the next 6 years.
The present study examines predictors of escalation from subthreshold depressive disorder in mid- to late adolescence to full-syndrome depressive disorders in young adulthood in a large community sample. We selected predictors that were associated with escalation in previous studies with adults 13,14 and/or are likely to be included in routine clinical evaluations or screening programs. Subthreshold depressive disorder was defined as an episode of depressed mood or loss of interest or pleasure lasting at least 1 week, and at least two of the seven other DSM-IV-associated 15 MDD symptoms, yielding a total of at least three depressive symptoms.7 A previous history of full-syndrome mood disorder was an exclusion criterion. Given the lack of an accepted definition of subthreshold depressive disorder, these criteria were chosen to strike a balance between the broad and narrow definitions in the literature with respect to both the number and duration of symptoms.3,4
METHOD
Participants
We used data from the Oregon Adolescent Depression Project,16 a longitudinal study of high school students who were assessed twice during adolescence, a third time at approximately age 24 years, and a fourth time at approximately age 30 years. Participants were randomly selected for the initial assessment from nine senior high schools representative of urban and rural districts in Western Oregon. A total of 1,709 adolescents (mean age 16.6, SD 1.2) completed the initial (T1) assessment between 1987 and 1989. The participation rate at T1 was 61% (details provided in Lewinsohn et al.16).
Approximately 1 year later, 1,507 of the adolescents (88%) returned for a second evaluation (T2). Differences between the sample and the larger population from which it was selected, and between participants and those who declined to participate at T2, were small.16
All the adolescents with a history of psychopathology by T2 (n = 644) and a random sample of adolescents with no history of psychopathology by T2 (n = 457) were invited to participate in a third (T3) evaluation. All nonwhite T2 participants were retained to maximize ethnic diversity. Of the 1,101 T2 participants selected for a T3 interview, 941 (85%) completed the evaluation at age 24 years. T2 diagnosis was not associated with participation at T3. At age 30 years, all the T3 participants were asked to complete the T4 assessment. Of the 941 who participated in the T3 evaluation, 816 (87%) completed the T4 assessment. T1 subthreshold depressive disorder was not associated with completion of one or more follow-up assessments.
During the T3 evaluation, we also assessed lifetime psychopathology in first-degree relatives. Of the 941 probands with T3 data, diagnostic data for relatives were available for 803 (85%). Diagnostic data were also obtained for the relatives of 37 probands who were selected for, but did not complete, the T3 evaluation. Written informed consent was obtained from each participating proband and relative (and guardian when the participant was younger than 18 years).
The present sample includes the 225 Oregon Adolescent Depression Project participants with a lifetime history of subthreshold depressive disorder (and no full-threshold MDD or dysthymic disorder) by the T1 assessment who completed at least one follow-up assessment, had diagnostic data on relatives, and had no lifetime diagnosis of a psychotic or bipolar disorder through their last follow-up. The participants were drawn from both the psychopathology and no psychopathology groups selected for the T3 follow-up. Two hundred sixteen adolescents who met criteria for lifetime subthreshold depressive disorder by T1 were excluded from the present report: 48 did not complete any of the follow-up assessments; 166 lacked family history data because they were not selected for, or declined to participate in, the T3 assessment; and 2 developed bipolar disorder during the follow-up. The participants with T1 subthreshold depressive disorder who were and were not included in this report differed significantly on only two of the 24 predictors in Table 1. Compared with the 216 participants who were not included, the 225 participants included in this report were more likely to be female (63.1% versus 52.3%, [chi]21 = 5.27, p <.05) and less likely to have a history of anxiety disorders by T1 (87.6% versus 95.4%, [chi]21 = 8.55, p <.01). Of the 225 participants included in this report, 82.7% completed the T2, T3, and T4 assessments; 12.4% completed only T2 and T3; and 4.9% completed only the T2 evaluation.
Table1.
| Did NOt Escalate to Full-Syndrome (n = 109) |
Escalated to Full-Syndrome (n = 116) |
Hazards Ratio (95% CI) |
Generalized R2 | |
|---|---|---|---|---|
| Demographic variables | ||||
| Female | 53.7% | 73.0% | 1.80 (1.14–2.84) | 0.0339 |
| Age (SD), y | 16.57 (1.11 ) | 16.58 (1.12) | 0.93 (0.78–1.11) | 0.0028 |
| White | 94.4% | 93.6% | 0.84 (0.43–1.62) | 0.0008 |
| No. of biological parents living at home | 1.56 (0.55) | 1.54 (0.58) | 0.88 (0.6 1–1.27) | 0.0022 |
| Depressive symptomsb | 0.0008 | |||
| Depressed mood | 96.9% | 95.7% | O.81 (0.29–2.27) | |
| Loss of interest or pleasure | 67.5% | 61.3% | 0.83 (0.55–1.26) | 0.0037 |
| Appetite or weight disturbance | 46.3% | 44.0% | 0.92 (0.61–1.3S) | 0.0007 |
| Sleep disturbance | 57.5% | 56.3% | 0.93 (0.62–1.40) | 0.0005 |
| Psychomotor disturbance | 45. 1% | 29.3% | 0.58 (0.38–0.91) | 0.0292 |
| Loss of energy | 48.8% | 54.6% | 1.09 (0.73–1.65) | 0.0009 |
| Worthlessness or guilt | 38.7% | 47.9% | 1.36 (0.91–2.01) | 0.0110 |
| Trouble concentrating/indecisiveness | 63.2% | 59.6% | 0.90 (0.59–1.36) | 0.0011 |
| Thoughts of death or suicide | 14.8% | 24.1% | 1.89 (1.19–3.01) | 0.0299 |
| Depression severity (BDI) (SD) | 6.21 (6.91) | 9.44 (6.58) | 1.05 (1.02–1.07) | 0.0545 |
| Lifetime comorbidity at T1 | ||||
| Anxiety | 4.3% | 14.9% | 2.19 (1.38–3.49) | 0.0295 |
| Disruptive behavior (ODD or conduct) | 4.9% | 2.8% | 0.83 (0.25–2.68) | 0.0049 |
| ADHD | 1.9% | 2.1% | 1.37 (0.44–4.24) | 0.0008 |
| Alcohol use | 4.3% | 4.3% | 1.14 (0.51–2.53) | 0.0003 |
| Drug use | 4.3% | 2.1% | 0.64 (0.20–2.03) | 0.0022 |
| Medical/health symptoms (SD) | 9.10 (5.75) | 13.49 (8.05) | 1.06 (1.04–1.09) | 0.0990 |
| Percent of family members with conditionc | ||||
| Depressive disorders (SD) | 24.6% (26.3%) | 33.6% (31.3%) | 2.70 (1.40–5.22) | 0.0648 |
| Anxiety disorders (SD) | 13.9% {19.4%) | 10.2% (20.2%) | 0.69 (0.21–2.26) | 0.0311 |
| Alcohol use disorders (SD) | 30.0% (28.6%) | 29.8% (30.0%) | 1.15 (0.57–2.37) | 0.0299 |
| Drug use disorders (SD) | 15.2% (22.3%) | 17.8% (25.4%) | 1.77 (0.81–3.88) | 0.0372 |
Note: Statistically significant associations are in bold. ADHD = attention-deficit/hyperactivity disorder; BDI = Beck Depression Inventory; CI = confidence interval; ODD = oppositional defiant disorder.
Percentages/hazards ratios/R2 values are weighted by probability of participation in T3.
All symptoms are lifetime, except for depression severity, which was assessed at T1.
These analyses include three covariates—percentage of family members directly interviewed, percentage of parents (versus Siblings), and percentage of female.
Diagnostic Measures
At T1 and T2, participants were interviewed with a version of the Schedule for Affective Disorders and Schizophrenia for School-Age Children (K-SADS),17 which combined features of the Epidemiologic and Present Episode versions, and included additional items to derive DSM-III-R18 diagnoses. Follow-up assessments at T2 and T3 were jointly administered with the Longitudinal Interval Follow-Up Evaluation (LIFE).19 The K-SADS/LIFE procedure provided information regarding the onset and course of disorders since the previous interview. The T4 interview consisted of a joint administration of the LIFE and the Structured Clinical Interview for DSM-IV20 to probe for new or continuing episodes since T3. Diagnoses were based on DSM-III-R criteria for T1 to T3 and DSM-IV criteria for T4. Interviews at T3 and T4 were conducted by telephone, which generally yields comparable results to face-to-face interviews.21,22
Diagnostic interviewers had advanced degrees in a mental health field and had completed a 70-hour course in diagnostic interviewing. At each of the four evaluations, audiotapes of a randomly selected sample of interviews were rated by another diagnostician. Interrater reliabilities for all full-threshold diagnoses used in this article were good to excellent.16,23 [kappa] for subthreshold depressive disorder was 0.79.7
The participants also completed a battery of questionnaires at the T1 assessment.24 This included the Beck Depression Inventory (BDI),25 a 21-item measure of current depressive symptoms, and a checklist of 88 medical conditions/symptoms (e.g., broken bones, ulcers, double vision) experienced in the past 12 months.24
Parents and siblings aged 18 years or older were interviewed with the nonpatient edition of the Structured Clinical Interview for DSM-IV.20 Siblings aged 14 to 18 years were interviewed with the K-SADS.17 Interviewers were unaware of probands’ diagnoses. Family history data were collected from the proband and, for relatives who could not be directly interviewed, from another relative. Informants were interviewed with the Family Informant Schedule and Criteria,26 supplemented with items necessary to derive DSM-IV diagnoses.
Of the 733 first-degree relatives with diagnostic information, direct interviews were obtained from 451 (62%; 265 parents, 186 siblings). At least two sources of data were available for 594 family members (81%). Of the family history interviews, 92.1% were conducted with the proband, 4.6% with the proband’s mother, 1.7% with the proband’s father, and 1.7% with a sibling of the proband.
Two senior diagnosticians, blind to proband diagnoses, reviewed all available data for each relative and independently derived lifetime best-estimate diagnoses 27 using DSM-IV criteria. Disagreements were resolved by consensus. The interrater reliability of diagnoses from direct interviews with relatives, family history interviews, and best estimates were good to excellent.28
Data Analyses
As the participants with no history of psychopathology were undersampled in the T3 follow-up, the participants were weighted as a function of the probability of selection at T3 in all analyses. Predictors included four demographic variables (age at T1, sex, race/ethnicity, and number of biological parents in the home at T1), 10 depressive symptom variables (lifetime occurrence by T1 of each of the nine DSM-IV symptom groups for MDD as assessed by the K-SADS and total score on the BDI at T1), six variables reflecting nonmood psychiatric disorders or medical problems (K-SADS diagnoses of lifetime anxiety, disruptive behavior [oppositional defiant or conduct], attention-deficit/hyperactivity, alcohol use, or drug use disorders through T1 and number of medical conditions/symptoms in the 12 months before T1), and four family history variables (familial loading for depressive, anxiety, alcohol use, and drug use disorders in first-degree relatives). Familial loading was indexed by computing the proportion of first-degree relatives with the disorder in each family. None of the 225 adolescents had missing values for any of the predictors, with the exception of medical conditions/symptoms (n = 13). Using an expectation maximization algorithm, these missing values were replaced with values imputed from demographic and questionnaire variables that correlated with the health measure.
The rate of escalation by age 30 years was estimated using Kaplan-Meier survival analysis. The participants who escalated to full-syndrome depressive disorders were more likely to have been followed through T4 than those who did not escalate (92% versus 72%, [chi]21 = 13.97, p <.001). Therefore, to examine predictors of escalation, we used Cox proportional hazards (PH) models to take differential follow-up into account by treating dropouts as censored observations.
Predictors were entered as independent variables, and time to escalation was used as the dependent variable in univariate Cox PH models. The proportional hazards assumption was tested by including a time-by-predictor interaction term in each Cox model. None of the interactions were significant, indicating that the proportional hazards assumption was met.29 Significant univariate predictors were combined in a multivariate Cox PH model. The percentages of relatives in each family who had direct interviews, were female, and were parents (versus siblings) were included as covariates in models involving family history. As a standardized effect size, we used Allison’s generalized R2.30
RESULTS
Risk of Escalation
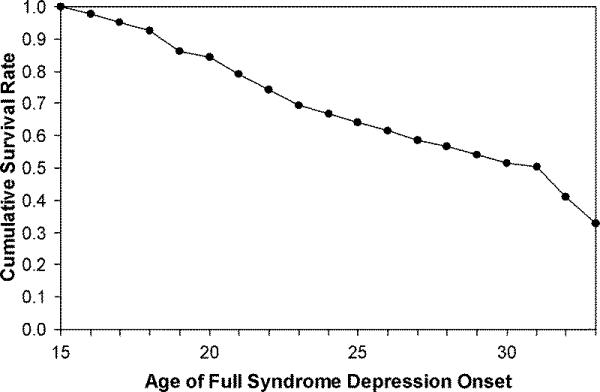
Of the 225 adolescents with subthreshold depressive disorder and no previous history of mood disorder by T1, 116 (weighted percentage of 46.5%) developed a full-syndrome depressive disorder by their last follow-up (115 developed MDD and 1 developed dysthymic disorder). The risk of escalation increased linearly with time (Fig. 1). The Kaplan-Meier estimated risk of escalation by the end of follow-up was 67.3% (SD 8.4%). The estimated risks of escalation by ages 21 and 25 years were 21.3% and 36.5%, respectively. The weighted mean and median ages of escalation for the 116 adolescents who developed full-syndrome depressive disorders were 22.2 (SD 4.2) and 21.8 years, respectively.
Figure1.
Univariate Analyses
In the univariate Cox PH analyses, seven variables predicted escalation (Table 1). Female sex, higher BDI scores, more medical conditions/symptoms, lifetime suicidal ideation, lifetime anxiety disorder, and greater familial liability for depressive disorder significantly predicted escalation to full-syndrome depressive disorder. Surprisingly, the participants with a history of psychomotor disturbance (agitation or retardation) had a significantly lower risk for escalation.
Multivariate Model
The significant univariate predictors were entered into a multivariate Cox PH model, with the exception of psychomotor disturbance as it was in the nonpredicted direction. (When psychomotor disturbance was included, it was not significant, and the effects of the other predictors did not change.) The correlations between the six independent variables in the multivariate model were uniformly low, ranging from −0.08 to 0.20 (mean r = 0.06). All six variables except sex accounted for unique variance in predicting escalation to full-syndrome depressive disorder (Table 2).
Table2.
| Hazards Ratio (95% CI) |
Generalized R2 | |
|---|---|---|
| Female | 1.370 (0.858–2.188) | 0.0085 |
| General medical conditions/symptoms |
1.049 (1.024–1.075) | 0.0512 |
| Lifetime thoughts of death or suicide |
1.877 (1.224–2.879) | 0.0288 |
| Depression severity (BDI) | 1.031 (1.005–1.057) | 0.0241 |
| Lifetime anxiety disorder | 1.978 (1.277–3.064) | 0.0226 |
| Family history of depressionb |
2.216 (1.084–4.530) | 0.0207 |
Note: BDI = Beck Depression Inventory; CI = confidence interval.
Hazards ratios/ R2 values are weighted by probability of participation in T3.
percentage of family members with condition. The analysis includes three covariates—percentage of family members directly interviewed, percentage of parents (versus siblings), and percentage of female.
Classification Rates
To provide an indication of clinical use, we tallied the number of significant univariate risk factors that were present for each of the 225 participants, omitting psychomotor change because it was in the nonpredicted direction. Thus, each participant had a range of 0 to 6 risk factors. For dichotomous variables (e.g., sex) and family history, we simply counted whether the risk factor was present. For BDI and medical/health problems, we used receiver operating curve analyses to determine the cut-point that maximized sensitivity and specificity in predicting escalation (>=6 for the BDI and >=10 for medical/health problems). We then determined the cutoff score on the risk factor tally that optimized sensitivity, specificity, and overall classification rate.
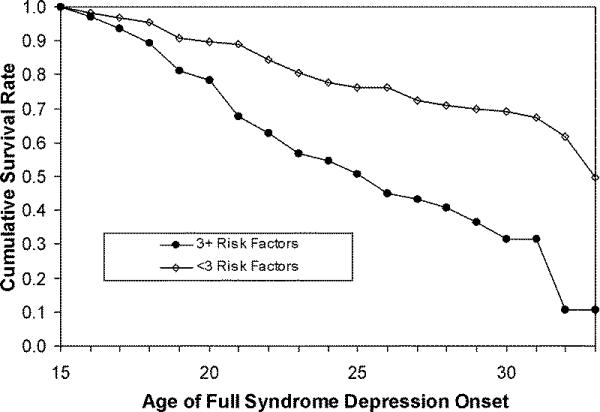
A cutoff of three or more risk factors yielded the optimal overall classification rate of 70.0%, with a sensitivity of 73.8% and a specificity of 66.7%. Increasing the cutoff to four risk factors increased specificity to 87.0% but decreased sensitivity to 39.0% (overall classification rate = 64.7%). Decreasing the cutoff to two or more risk factors reduced specificity to 48.6% but increased sensitivity to 91.5% (overall classification rate = 60.1%). Taking attrition into account, the Kaplan-Meier estimated risks for escalation to full-syndrome depressive disorder in the participants with three or more and fewer than three risk factors were 90.1% and 46.6%, respectively (Fig. 2).
Figure2.
Stable Versus Unstable Subthreshold Depressive Disorder
Of adolescents with a history of subthreshold depressive disorder by T1, 26.3% met criteria for subthreshold depression again during the T1-T2 interval, 11.0% escalated to a full-syndrome depressive disorder, and 62.7% did not exhibit either subthreshold or full-threshold depression (percentages weighted as a function of probability of selection at T3). It is reasonable to hypothesize that the youths who met criteria for subthreshold depressive disorder again during T1 to T2 would have a greater risk for escalation during T2 to T4 than the youths without subthreshold depression during T1 to T2. Excluding the adolescents who escalated to full-syndrome depressive disorders during T1 to T2, 54.4% of the youths who met criteria for subthreshold depressive disorder again during the T1-T2 interval converted to full-syndrome depressive disorder between T2 and T4, compared with 34.0% of adolescents without subthreshold depression during T1 to T2 (hazards ratio [HR] 2.29; 95% confidence interval [CI] 1.40-3.73, p =.001).
Proximal Versus Distal Predictors of Escalation
In the final set of analyses, we examined whether predictors of proximal and distal escalation differed. The adolescents who developed full-syndrome depressive disorders during the follow-up were divided into those who escalated between T1 and T2; (early escalators, n = 33) and those who escalated after T2 (later escalators, n = 83). Each of the predictors in Table 1 was entered into univariate Cox regression models comparing the two groups with each other and with adolescents who did not escalate during the follow-up (n = 109).
Predictors of early and later escalation were generally similar. Compared with nonescalators, early escalators exhibited greater suicidal ideation before T1 (HR 2.55; 95% CI 1.19-5.44, p <.05), more depressive symptoms (HR 1.05; 95% CI 1.01-1.08, p <.05) and general medical symptoms at T1 (HR 1.10; 95% CI 1.05-1.15, p <.001), and a greater familial loading for depressive disorders (HR 6.59; 95% CI 1.84-23.66, p <.01). Compared with nonescalators, late escalators were more likely to be female (HR 2.27; 95% CI 1.30-3.96, p <.01); less likely to report psychomotor disturbance (HR 0.49; 95% CI 0.29-0.92, p <.01), were more likely to exhibit suicidal ideation (HR 1.78; 95% CI 1.01-3.13, p <.05), and an anxiety disorder before T1 (HR 2.50; 95% CI 1.46-4.27, p <.001); had more severe depressive symptoms (HR 1.05; 95% CI 1.02-1.08, p <.001) and general medical symptoms at T1 (HR 1.07; 95% CI 1.04-1.10, p <.001); and had a greater familial loading of depressive disorders (HR 2.57; 95% CI 1.16-5.67, p <.05). Of the 24 predictors examined, early and late escalators differed on only one: early escalators were more likely to report appetite/weight disturbance before T1 (HR 2.14; 95% CI 1.03-4.46, p <.05).
DISCUSSION
Almost half of the adolescents with subthreshold depressive disorder in this community sample developed full-syndrome depressive disorder by their early 30s; when attrition was taken into account, the estimated risk was 67%. The survival function was linear, indicating that risk persisted long after the T1 assessment. This highlights the potency of subthreshold depressive disorder as an enduring risk factor for full-syndrome depressive disorders and its use for selecting a subgroup of adolescents at high risk for mood disorders. However, our data also indicated that even after 10 to 15 years of follow-up, at least one third of the adolescents with subthreshold depressive disorder did not experience a full-syndrome depressive episode. This underscores the importance of identifying predictors of escalation within this high-risk subgroup to further refine risk prediction.
Seven variables significantly predicted escalation to full-syndrome depressive disorder among adolescents with subthreshold depressive disorder: female sex; greater severity of depressive symptoms, and more medical conditions/symptoms at T1; histories of suicidal ideation, anxiety disorder, and no psychomotor disturbance through T1; and a greater familial loading for depressive disorders. When these variables were included in a multivariate model, severity of depression and medical conditions/symptoms at T1, lifetime suicidal ideation and anxiety disorder, and familial loading for depression continued to make significant unique contributions.
Interestingly, the predictors of proximal (1 year) and more distal (>1 year) escalation were generally similar. Moreover, a direct comparison of predictors of proximal and distal escalation revealed few differences. Although most of the predictors we examined occurred before the baseline assessment, we also explored whether persistent/recurrent subthreshold depressive disorder (reported in both the T1 and T2 assessments) was associated with a greater risk for escalation after T2. Indeed, the adolescents reporting subthreshold depressive disorders in both assessments had a twofold greater risk for escalation than the youths who reported subthreshold depression in the T1 assessment only.
Our findings were consistent with those of Cuijpers et al.,13 who also found that severity of depression, family history of depression, and chronic medical illness predicted escalation from subthreshold to full-syndrome depressive disorder in an adult primary care sample. However, findings regarding specific depressive symptoms have been inconsistent. Thus, Cuijpers et al.14 found that, in older adults with subthreshold depression, low appetite and sleeping problems predicted the subsequent onset of a full-syndrome depressive disorder. In the present study, suicidal ideation and the absence of psychomotor disturbance predicted escalation. Because the latter finding was unexpected, we do not believe that it should be interpreted until it has been replicated. Female sex predicted escalation in univariate, but not multivariate, analyses. This suggests that its influence was mediated by other variables in the model. Exploring this further, we found that sex lost its effect only when medical conditions/symptoms were included in the model. Thus, sex seems to influence escalation through increasing health problems/complaints in adolescence.
Several of the variables that predicted escalation from subthreshold to full-syndrome depressive disorder, particularly severity of depressive symptoms, history of anxiety disorders, and familial loading of depression, also predict who has not been selected for subthreshold depression 1,31,32 and the persistence and recurrence of depression in youths with MDD.2,33 Although there is some evidence for differences in the processes involved in onset and recurrence,34 these data suggest that there may also be common processes involved in the onset, maintenance, and recurrence of depression.
The present findings have implications for prevention/early intervention. We computed a simple index of the risk for escalation by summing the number of risk factors present for each adolescent. We chose not to weight any specific predictor to make it more useful for clinicians and because unit (equal) weights generalize better to other samples.35 A cutoff of three or more risks factors optimized prediction. Taking attrition into account, the Kaplan-Meier estimated risk for escalation through the end of the follow-up period was 90.1% for subthreshold cases with three or more risk factors compared with 46.6% for those with fewer than three risk factors. Thus, the risk for escalation among the adolescents with subthreshold depressive disorder and three or more of the risk factors identified in this study is extremely high and seems to warrant targeted preventive intervention.12
This study has a number of strengths, including a large sample of adolescents with subthreshold depressive disorder from the community and a prospective design with three follow-ups for 15 years. However, it also has a number of limitations.
First, because of the sampling design at T3 and attrition, a number of adolescents with subthreshold depressive disorders by T1 were not included in this report. However, cases that were and were not included differed significantly on only two of the 24 baseline variables examined in the study.
Second, our sample included adolescents with current and past subthreshold depressive disorders at T1. Unfortunately, onset and offset dates were not obtained for episodes that failed to meet criteria for full-syndrome diagnoses; hence we could not examine the associations of age of onset and duration of subthreshold depression and duration of remission with risk for escalation. However, as T1 BDI scores predicted the subsequent onset of full-threshold depressive disorders, it seems that current subthreshold depressive symptoms are associated with a greater risk for escalation.
Third, the family psychopathology assessments were not truly prospective in that they were undertaken as part of the T3 assessment. Thus, it is possible that the direction of causality could be reversed (i.e., parental depression could be a consequence of escalation in the adolescent). However, 82.6% of depressed relatives had their onset before the proband’s escalation to MDD, with a median difference of 9.25 years. In addition, we reran the analyses conservatively treating relatives who reported an onset of depression after T1 as nonaffected. Familial loading for depression continued to predict escalation (HR 2.42; 95% CI 1.22-4.80, p =.01).
Fourth, we examined multiple predictors and did not correct for the number of analyses. Hence, replication is needed. Fifth, the classification rates may be inflated because of capitalizing on chance and should be cross-validated. Sixth, despite the use of a prospective, longitudinal design, the assessments at each wave were necessarily retrospective. Hence, the onset dates for full-syndrome depressive disorders may not be precise.
Finally, we focused on distal predictors of escalation. It will be important for future research to explore the processes that mediate the effects of the predictors we identified; investigate risk factors in other domains, such as interpersonal relationships, information processing biases, and biological and genetic markers; and identify proximal factors that trigger escalation.
In conclusion, although subthreshold depressive disorder is one of the best established risk factors for the onset of full-syndrome depressive disorders, at least a third of the youths with subthreshold depression did not develop full-syndrome depressions in up to 15 years of follow-up. We identified five variables that accounted for unique variance in predicting the escalation of subthreshold depressive disorder: severity of depressive symptoms, medical conditions/symptoms, lifetime suicidal ideation, lifetime anxiety disorder, and familial loading for depression. Adolescents with three or more risk factors had an estimated 90.1% chance of escalating to full-syndrome depressive disorder, compared with 46.6% of the adolescents with fewer than three risk factors. These data may be useful in identifying a subgroup of youths with subthreshold depressive disorder who are at especially high risk for escalating to full-syndrome depressive disorders and may be candidates for prevention/early intervention programs.12
Acknowledgments
Supported by the National Institute of Mental Health Grants R01-MH66023 (D.K.), R01-MH40501, R01-MH50522, and R01-MH52858 (P.L.).
Footnotes
Disclosure: The authors report no conflicts of interest.
REFERENCES
- 1.Fergusson DM, Horwood LJ, Ridder EM, Beautrais AL. Subthreshold depression in adolescence and mental health outcomes in adulthood. Arch Gen Psychiatry. 2005;62:66–72. doi: 10.1001/archpsyc.62.1.66. [DOI] [PubMed] [Google Scholar]
- 2.Lewinsohn PM, Solomon A, Seeley JR, Zeiss A. Clinical implications of “subthreshold” depressive symptoms. J Abnorm Psychol. 2000;109:345–351. [PubMed] [Google Scholar]
- 3.Pincus HA, Davis WW, McQueen LE. “Subthreshold” mental disorders. A review and synthesis of studies on minor depression and other “brand names”. Br J Psychiatry. 1999;174:288–296. doi: 10.1192/bjp.174.4.288. [DOI] [PubMed] [Google Scholar]
- 4.Sadek N, Bona J. Subsyndromal symptomatic depression: a new concept. Depress Anxiety. 2000;12:30–39. doi: 10.1002/1520-6394(2000)12:1<30::AID-DA4>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 5.Gonzáles-Tejera G, Canino G, Ramírez R, et al. Examining minor and major depression in adolescents. J Child Psychol. 2005;46:888–899. doi: 10.1111/j.1469-7610.2005.00370.x. [DOI] [PubMed] [Google Scholar]
- 6.Oldehinkel AJ, Wittchen HU, Schuster P. Prevalence, 20-month incidence and outcome of unipolar depressive disorder in a community sample of adolescents. Psychol Med. 1999;29:655–668. doi: 10.1017/s0033291799008454. [DOI] [PubMed] [Google Scholar]
- 7.Lewinsohn PM, Shankman SA, Gau JM, Klein DN. The prevalence and co-morbidity of subthreshold psychiatric conditions. Psychol Med. 2004;34:613–622. doi: 10.1017/S0033291703001466. [DOI] [PubMed] [Google Scholar]
- 8.Gotlib IH, Lewinsohn PM, Seeley JR. Symptoms versus a diagnosis of depression: differences in psychosocial functioning. J Consult Clin Psychol. 1995;63:90–100. doi: 10.1037//0022-006x.63.1.90. [DOI] [PubMed] [Google Scholar]
- 9.Keenan K, Hipwell A, Feng X, et al. Subthreshold symptoms of depression in preadolescent girls are stable and predictive of depressive disorders. J Am Acad Child Adolesc Psychiatry. 2008;47:1433–1442. doi: 10.1097/CHI.0b013e3181886eab. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pine DS, Cohen E, Cohen P, Brook J. Adolescent depressive symptoms as predictors of adult depression: moodiness or mood disorder? Am J Psychiatry. 1999;156:133–135. doi: 10.1176/ajp.156.1.133. [DOI] [PubMed] [Google Scholar]
- 11.Horowitz JL, Garber J. The prevention of depressive symptoms in children and adolescents: a meta-analytic review. J Consult Clin Psychol. 2006;74:401–415. doi: 10.1037/0022-006X.74.3.401. [DOI] [PubMed] [Google Scholar]
- 12.Merry SN, Spence SH. Attempting to prevent depression in youth: a systematic review of the evidence. Early Interv Psychiatry. 2007;1:128–137. [Google Scholar]
- 13.Cuijpers P, Smit F, Willemse G. Predicting the onset of major depression in subjects with subthreshold depression in primary care: a prospective study. Acta Psychiatr Scand. 2005;111:133–138. doi: 10.1111/j.1600-0447.2004.00416.x. [DOI] [PubMed] [Google Scholar]
- 14.Cuijpers P, Beekman A, Smit F, Deeg D. Predicting the onset of major depressive disorder in older adults with subthreshold depression: a community based study. Int J Geriatr Psychiatry. 2006;21:811–818. doi: 10.1002/gps.1565. [DOI] [PubMed] [Google Scholar]
- 15.American Psychological Association . Diagnostic and Statistical Manual of Mental Disorders. 4th ed American Psychological Association; Washington, DC: 1994. [Google Scholar]
- 16.Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III-R disorders in high school students. J Abnorm Psychol. 1993;102:133–144. doi: 10.1037//0021-843x.102.1.133. [DOI] [PubMed] [Google Scholar]
- 17.Orvaschel H, Puig-Antich J, Chambers WJ, Tabrizi MA, Johnson R. Retrospective assessment of prepubertal major depression with the Kiddie-SADS-E. J Am Acad Child Psychiatry. 1982;21:392–397. doi: 10.1016/s0002-7138(09)60944-4. [DOI] [PubMed] [Google Scholar]
- 18.American Psychological Association . Diagnostic and Statistical Manual of Mental Disorders. Third Edition-Revised American Psychological Association; Washington, DC: 1987. [Google Scholar]
- 19.Keller MB, Lavori PW, Friedman B, et al. The Longitudinal Interval Follow-up Evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- 20.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders. Non-Patient Edition (SCID-NP, Version 2.0) Biometrics Research Department, New York State Psychiatric Institute; New York: 1996. [Google Scholar]
- 21.Rohde P, Lewinsohn PM, Seeley JR. Comparability of telephone and face-to-face interviews in assessing axis I and II disorders. Am J Psychiatry. 1997;154:1593–1598. doi: 10.1176/ajp.154.11.1593. [DOI] [PubMed] [Google Scholar]
- 22.Sobin C, Weissman MM, Goldstein RB, et al. Diagnostic interviewing for family studies: comparing telephone and face-to-face methods for the diagnosis of lifetime psychiatric disorders. Psychiatr Genet. 1993;3:227–233. [Google Scholar]
- 23.Rohde P, Lewinsohn PM, Seeley JF, Klein DN, Andrews JA, Small J. Psychosocial functioning of adults who experienced substance use disorders as adolescents. Psychol Addict Behav. 2007;21:155–164. doi: 10.1037/0893-164X.21.2.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lewinsohn PM, Roberts RE, Seeley JR, Rohde P, Gotlib IH, Hops H. Adolescent psychopathology: II. Psychosocial risk factors for depression. J Abnorm Psychol. 1994;103:302–315. doi: 10.1037//0021-843x.103.2.302. [DOI] [PubMed] [Google Scholar]
- 25.Beck AT, Ward H, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 26.Mannuzza S, Fyer AJ. Family Informant Schedule and Criteria (FISC) New York State Psychiatric Institute; New York: 1990. [Google Scholar]
- 27.Klein DN, Ouimette PC, Kelly HS, Ferro T, Riso LP. Test-retest reliability of team consensus best-estimate diagnoses of Axis I and II disorders in a family study. Am J Psychiatry. 1994;151:1043–1047. doi: 10.1176/ajp.151.7.1043. [DOI] [PubMed] [Google Scholar]
- 28.Klein DN, Lewinsohn PM, Seeley JR, Rohde P. A family study of major depressive disorder in a community sample of adolescents. Arch Gen Psychiatry. 2001;58:13–20. doi: 10.1001/archpsyc.58.1.13. [DOI] [PubMed] [Google Scholar]
- 29.Singer JD, Willett JB. Modeling the days of our lives: using survival analysis when designing and analyzing longitudinal studies of duration and the timing of events. Psychol Bull. 1991;110:268–290. [Google Scholar]
- 30.Allison PD. Survival Analysis Using SAS: A Practical Guide. SAS Institute; Cary, NC: 1995. [Google Scholar]
- 31.Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- 32.Klein DN, Lewinsohn PM, Rohde P, Seeley JR, Olino TM. Psychopathology in the adolescent and young adult offspring of a community sample of mothers and fathers with major depression. Psychol Med. 2005;35:353–365. doi: 10.1017/s0033291704003587. [DOI] [PubMed] [Google Scholar]
- 33.Birmaher B, Arbelaez C, Brent D. Course and outcome of child and adolescent major depressive disorder. Child Adolesc Psychiatr Clin N Am. 2002;11:619–637. doi: 10.1016/s1056-4993(02)00011-1. [DOI] [PubMed] [Google Scholar]
- 34.Lewinsohn PM, Allen NB, Seeley JR, Gotlib IH. First onset versus recurrence of depression: differential processes of psychosocial risk. J Abnorm Psychol. 1999;108:483–489. doi: 10.1037//0021-843x.108.3.483. [DOI] [PubMed] [Google Scholar]
- 35.Dawes RM. The robust beauty of improper linear models in decision making. Am Psychol. 1979;34:571–582. [Google Scholar]


