Abstract
Summary:
There have been no studies examining the level of understanding age-related macular degeneration (ARMD) patients have about their disease, or their perceptions about intraocular injections as treatment. In this study, patient knowledge about ARMD risk factors was low but patients appeared more optimistic than fearful when confronted with intraocular antivascular endothelial growth factor (anti-VEGF) injections as treatment.
Purpose:
In recent years there has been an increase in our understanding of wet ARMD, and a dramatic shift in the treatment paradigm. However, to our knowledge, no studies have examined how much ARMD patients understand their disease, or how they feel about receiving intraocular injections as treatment. The primary objectives of this study are to identify areas in which ARMD patients may be uninformed about their disease, and to recognize specific fears or expectations that patients may have regarding treatment with intraocular anti-VEGF injections.
Design:
Prospective, survey-based study.
Methods:
This is a prospective survey-based study. An anonymous 32-item questionnaire was compiled and distributed to patients with wet ARMD who underwent at least one intraocular anti-VEGF injection. Eighty-three patients from a retina practice in a suburban setting completed the questionnaire that gauged both their knowledge of ARMD and their perspectives on its treatment. Data was analyzed using chi-square testing.
Results:
Seventy-eight percent of patients received most of their knowledge of ARMD from their physician. Eighty-nine percent of patients prefer to receive more information on ARMD, if needed, directly from their physician. Only 21%, 48%, 37%, 48%, and 36%, respectively, correctly identified how diet, special vitamins, high blood pressure, family history, and smoking can affect ARMD. Sixty percent felt somewhat afraid or very afraid about getting their first intraocular injection but this did not correlate with pain or discomfort during treatment (P = 0.075, P = 0.117). Eighty-nine percent were very satisfied and 11% were somewhat satisfied with the explanation their physician gave them about the injections. Eighty percent reported feeling hopeful (significantly more than any other emotion) when they were first told they needed an intraocular injection for treatment of their disease.
Conclusions:
Knowledge of risk factors and risk factor modification among patients with ARMD is low. Since the vast majority of ARMD patients prefer to receive information directly from their physician, patient education is crucial in improving risk factor modification and alleviating fears of treatment. With the advent of anti-VEGF agents, patients appear more hopeful of regaining vision than they are fearful of treatment with intraocular injections.
Keywords: age-related macular degeneration, patient education, fear of needles, anti-VEGF, macular degeneration risk factors, macular degeneration treatment, ranibizumab
Introduction
The number of adults with ARMD is expected to increase by 50% to 3 million people by the year 2020.1 Rein et al recently published a study on ARMD prevalence in the United States and predicted 17.8 million cases by the year 2050.2 This surge in ARMD cases will be largely due to the significant increase in the population of Americans aged 65 years and older, which is projected to exceed 82 million by the year 2050.3
Previously, treatments for ARMD (such as laser) were ineffective and visual loss was inevitable. However, the emergence of intraocular injections of VEGF inhibitors has been effective in neovascular macular degeneration which is responsible for the most severe vision loss that occurs in ARMD patients. In many cases, these revolutionary anti-VEGF inhibitors have actually been shown to improve vision in some patients.4–8
Studies have long established the impact of ARMD on the quality of life. The National Eye Institute (NEI) generated a questionnaire (Visual Functioning Questionnaire 25) that measured activities of daily living, mental health, and quality of life among patients diagnosed with varying degrees of ARMD.9,10 The severity of disease was found to be directly proportional to the decrease in quality of life. Hence, the diagnosis of ARMD can be grim for patients, but there are several modifiable risk factors such as smoking and diet that can impact or impede the progression of ARMD.11–27 However, no studies to our knowledge have evaluated how much patients with ARMD understand about their disease. Additionally, although the advent of anti-VEGF injection therapies has given new hope for patients with ARMD, no studies have investigated how patients view such treatments. The thought of any injection with a needle instills fear and uncertainty in many patients.28 The neovascular ARMD patient in particular is often expected to make frequent visits for repeat injections (with risks such as infection, bleeding, and vision loss in and of itself), and undergo multiple tests for monitoring the condition without guarantee of vision preservation. Furthermore, health care plans often do not completely cover these treatments, thereby leaving some patients with significant financial burden and possible reluctance to begin or continue therapy. We wonder if the above issues may influence therapeutic outcomes. This proposed study also aims to elucidate specific areas in which clinicians may need to better educate and counsel their patients with ARMD.
Methods
A 32-item questionnaire approved by the SUMMA Institutional Review Board and compliant with the Health Insurance Portability and Accountability Act (HIPAA) was given to neovascular ARMD patients who had received at least one anti-VEGF injection. Patients were asked to participate in the survey while awaiting their scheduled appointment in the retina clinic. The retina clinic is a three-physician private practice group located in a suburban setting. The main objective of the questionnaire was to gauge patients’ knowledge of ARMD, and their feelings and expectations regarding treatment with intraocular anti-VEGF injections. The questions were divided into three sections and represented patient demographics, patient knowledge, and patient perspectives. The survey instrument excluded personally identifying information. Completed questionnaires were randomly placed into a closed box to ensure privacy.
Inclusion criteria consisted of any patient diagnosed with wet macular degeneration who had already received a minimum of one anti-VEGF injection. Patients who received past, alternative treatments for macular degeneration, such as laser or surgery, were also considered as long as they had met the inclusion criteria indicated above. Exclusion criteria were patients who did not have the wet form of macular degeneration, or patients with wet macular degeneration who had not yet received an injection. Patients qualifying for the study who completed a questionnaire received reimbursement (US $10) to improve compliance. Questionnaire responses were recorded at the end of survey collection and analyzed for descriptive and associative analysis with chi-square testing.
Results
Demographic information of the study group is presented in Table 1. The average age of the patients was 82 years with a range between 58 and 96 years. Sixty-eight percent of respondents were female and over 96% were Caucasian. All patients reported English as being their primary language. Of the patients included in the study, 75% had someone drive them to their appointments, 18% walked or drove themselves, and 5% took public transportation. Twelve percent of patients reported having ARMD for less than a year, 58% had the disease for between 1 and 5 years, 17% for 5–10 years, and 6% for more than 10 years. The duration of disease did not correlate with appropriate knowledge of disease. Furthermore, less than 46% (45.8%) of patients reported taking vitamins for their ARMD and 4.8% were current smokers. Females appeared more likely to take daily vitamins for their ARMD (P = 0.013). Sixty percent reported that ARMD had mildly or moderately affected their quality of life and 16% reported that it had extremely affected their quality of life.
Table 1.
Basic patient demographic information
| % of patients | |
|---|---|
| Sex | |
| Male | 32 |
| Female | 68 |
| Age group | |
| 50–60 | 1 |
| 60–70 | 4 |
| 70–80 | 31 |
| >80 | 64 |
| Ethnicity | |
| Caucasian | 96.4 |
| Other | 1.2 |
| Duration of ARMD | |
| <1 year | 12 |
| 1–5 years | 57.8 |
| 5–10 years | 16.9 |
| >10 years | 6 |
| Smoking | |
| Yes | 4.8 |
| No | 92.8 |
| ARMD vitamins taken daily | |
| Yes | 45.8 |
| No | 51.8 |
| Live alone | |
| Yes | 47 |
| No | 53 |
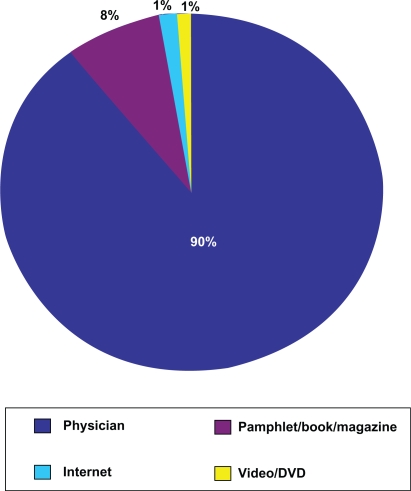
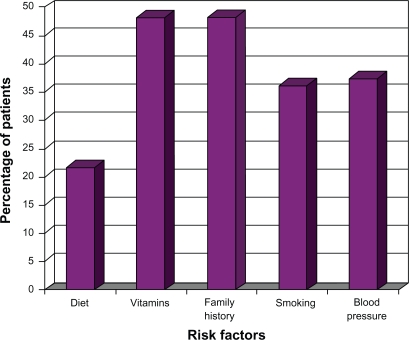
Figure 1 demonstrates how most patients received their knowledge of ARMD. By far, most patients (78.3%) learned about ARMD primarily from their doctor. Although 77% felt they were moderately or very knowledgeable about ARMD, only 21%, 48%, 37%, 48%, and 36%, of patients respectively, correctly identified how diet, special vitamins, high blood pressure, family history, and smoking can affect ARMD (Figure 2). The vast majority of patients (89%) preferred to receive more information about macular degeneration from their retinal physician than any other source (eg, internet, videos/DVD, pamphlet).
Figure 1.
How did you get most of your knowledge on ARMD?
Figure 2.
Patient knowledge of ARMD risk factors.
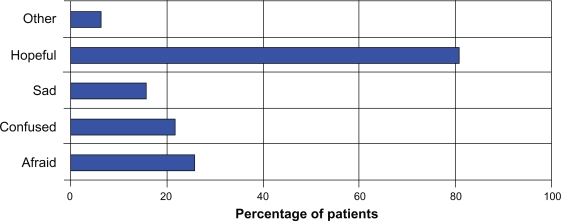
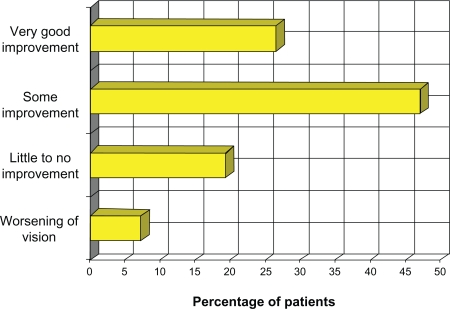
Eighty-nine percent of patients were very satisfied with the counseling given by the retinal physician prior to the intravitreal injection. Figure 3 summarizes how patients felt when they were first told they needed an intraocular injection to treat the ARMD. By far the most common emotion was “hopeful” (80%). Only 6% and 22% respectively felt that any of the injections were painful or uncomfortable and this feeling did not correlate with being “afraid” or “very afraid” upon learning that an injection was needed in the eye. There were also no statistically significant correlations between feeling pain or discomfort with sex, age, or living alone. Although 51% were “somewhat afraid” and 10% were “very afraid” about getting their first injection, no patients reported missing appointments because of trepidation of receiving an injection into the eye. Most patients (75%) actually had a better than expected experience when receiving their first injection. Over 66% of patients also reported that they were less afraid before going in for their second injection. In terms of visual outcome, 47% of patients reported some improvement in vision, and 27% claimed very good improvement in vision since receiving the injections (Figure 4). Finally, 58% of patients would prefer taking pills at home as opposed to receiving injections in the office if such a treatment were available. Not surprisingly, patients who reported pain or discomfort during the injection were more likely to want to take pills for their ARMD instead of injections (P = 0.03).
Figure 3.
How did you feel when you were first told you needed an injection into the eye?
Figure 4.
How would you describe the improvement in your vision since getting the injection(s)?
Discussion
Although the advent of new anti-VEGF agents such as ranibizumab and bevacizumab has given renewed hope to ARMD patients, there should also be emphasis on risk factor modification to enhance the ability of these new agents, and to prevent further progression of disease (including in the contralateral eye). Risk factor modification takes into account smoking, blood pressure control, antioxidant vitamin intake, and diet. Several studies have demonstrated that smoking is a very strong risk factor for progression of ARMD but less than 35% of patients in this study recognized it as a risk factor.15–18 In a more recent Beaver Dam Eye Study, an increase in systolic blood pressure greater than 5 mm Hg resulted in an increased risk of advanced ARMD by fivefold.29 In addition, reports of the Age-Related Eye Disease Study (AREDS) established that the intake of omega-3 fatty acids, fish, and sources of lutein and zeaxanthine (dark green leafy vegetables) decreased progression to advanced ARMD by 39% and 54% respectively.23,24 However, only 37% of patients in this study identified blood pressure as a risk factor, and even fewer (22%) were aware of diet as a risk factor. AREDS also reported that patients with moderate disease can significantly decrease (by 25%) the progression of ARMD by taking a specific combination (AREDS formulation) of vitamin C, vitamin E, beta-carotene, zinc, and copper in pill form every day.29 Again, only 48% of patients in our study were aware of this, and the number may be even lower as some patients may have mistaken it for a simple multivitamin. In fact, the studies that have investigated patient use of AREDS-formulation vitamins have found that a significant number who do report vitamin usage actually use suboptimal dosages.30–33 Although elevated cholesterol has been reported as a risk factor there are conflicting studies in the literature and therefore this was not included in the questionnaire.34,35
The results of this study suggest that the knowledge of risk factors and risk factor modification among ARMD patients is low and may be important in disease progression or prevention. Our questionnaire asked the patients about ways that they would prefer to improve knowledge about their ARMD. Since the vast majority of ARMD patients (90%) preferred to receive information directly from their physician, patient education by physicians may be crucial in improving risk factor modification. This may be more challenging with hearing-impaired elderly patients and in settings that limit appointment times. It is recommended that the patient be given a simplified explanation of the disease process and its risk factors by the physician, and to also involve family members in the discussion. Using a pamphlet may facilitate the discussion, and can serve the patient and his or her family members as a point of reference after they leave the office. The physicians in this retina practice generally used this method of patient education but our results suggest that greater emphasis be placed on risk factor modification in future patient discussions. Although the style of patient education naturally differs between the physicians in this practice, all used a standardized pamphlet from the American Academy of Ophthalmology as a teaching aid as well as a customary intravitreal injection consent form that detailed all the risks and benefits of the procedure. Serious risks were outlined including infection, vitreous hemorrhage, retinal tear or detachment, cataract, and glaucoma. Other less serious risks such as subconjunctival hemorrhage, eye pain, corneal abrasion, floaters, and inflammation of the eye were also detailed in the consent form.
As mentioned previously, the introduction of anti-VEGF agents has revolutionized its treatment. However, of frequent concern is how the injections are administered. In this study a significant number of patients (60%) appeared to show some level of trepidation prior to receiving these injections. To the best of our knowledge no studies have evaluated the fear of needles in ophthalmology patients. There are, however, studies demonstrating decreased compliance with treatment in patients requiring injections in other specialties.22,36,37 Although none of the patients in this study reported missing an appointment for fear of the injection (or cost for that matter), the inherent sampling bias of an in-office questionnaire, as well as small sample size, precludes these from being noteworthy findings.
A large percentage (89%) reported being “very satisfied” with the explanation that was given by their physician on how the injections were given. Before assuming adequacy it should be noted that ARMD focus group studies find that most elderly patients tend to provide very positive reviews in an effort to please their physicians.38 However, given the fact that the respondents were anonymous, this was still a reassuring percentage. Although only a small minority of patients reported pain or discomfort from receiving the injections it still appeared that the majority (58%) would prefer to take a pill at home as opposed to receiving injections in the office. We wondered why this number was not higher and postulated that most of these were elderly patients who were more likely to be on multiple pill regimens. Thus, having an injection into the eye not only decreased the need to take one additional daily pill but it also guaranteed direct delivery into the diseased site with minimal systemic side effects. One surprising result was that by far the most prevalent emotion upon hearing the need for an injection was “hopeful” (even more so than “afraid”). This result can be explained in part by a study done by Owsley et al which found that people with ARMD are generally more optimistic in an effort to improve their depression and well-being.39 However, that study was completed before the widespread use of anti-VEGF agents in ARMD. For a disease that has a potentially crushing impact on quality of life, previous treatments (laser photocoagulation, photodynamic therapy) were rather disappointing and rarely resulted in visual improvement. The currently approved anti-VEGF agent ranibizumab has demonstrated significant visual improvement in 25%–30% of patients, and over 90% of patients maintain their vision or have some improvement.40 This unprecedented success in ARMD treatment has greatly contributed to patients being much more hopeful of regaining vision than they are fearful of treatment with intraocular injections. A recent summary of clinical trials has determined that there was a greater visual benefit in administering ranibizumab injections on a monthly basis.41 This increased frequency makes it even more important to gauge patients’ attitudes towards these injections and improve risk factor modification to ensure that patients are maximizing treatment outcome.
This study has some limitations. One of the goals of the study was to determine if patients felt the injections as being painful or uncomfortable. Hence the inclusion criteria required that a patient must have undergone at least one injection anytime during their treatment. Some patient responses may have been biased as a result of the retrospective nature of the question. Furthermore, there was no questionnaire given to patients prior to their first injection, and no attempt was made to contact patients who may have refused injections. This information would have been useful in possibly obtaining less-biased responses as well as pinpointing specific reasons for refusing treatment. We also found that over 70% of our patients come to their appointments by having someone else drive them. Nevertheless, in this study, compliance did not appear to be affected by cost of treatment, fear of treatment, or lack of access to resources or care. This is to be generally expected in a suburban private practice with mostly insured patients. However, we wonder if the above issues may be of more concern in a different setting where access to facilities is problematic (family members unable to drive and sit with patients for frequent exams and injections), and lack of resources may preclude patients from obtaining the care that they need. Perhaps a multicentric study design that would reduce bias, and include a larger and more diverse socioeconomic population may help provide the answers to those questions.
Acknowledgments
Presented as a poster presentation at the Association for Research in Vision and Ophthalmology, May 3, 2009, Ft. Lauderdale, FL, USA. This study was funded by a SUMMA Foundation Grant.
Footnotes
Disclosures
The authors have no proprietary interest in any materials discussed in this article.
References
- 1.Friedman DS, O’Colmain B, Munoz B, et al. Prevalence of age-related macular degeneration in the United States. Arch Ophthalmol. 2004;122(4):564–572. doi: 10.1001/archopht.122.4.564. [DOI] [PubMed] [Google Scholar]
- 2.Rein DB, Wittenborn JS, Zhang X, et al. Forecasting age-related macular degeneration through the year 2050. Arch Ophthalmol. 2009;127(4):533–540. doi: 10.1001/archophthalmol.2009.58. [DOI] [PubMed] [Google Scholar]
- 3.US Census Bureau . National Population Projections, Summary Tables: (NP-T4) Projections of the total resident population by 5-year age groups, race, and Hispanic origin with special age categories: middle series, 1999 to 2100. Washington, DC: U Census Bureau; 2000. Population Division. [Google Scholar]
- 4.Rosenfeld PJ, Brown DM, Heier JS, et al. Ranimizumab for neovascular age-related macular degeneration. N Engl J Med. 2006;355(14):1419–1431. doi: 10.1056/NEJMoa054481. [DOI] [PubMed] [Google Scholar]
- 5.Brown DM, Kaiser PK, Michels M, et al. Ranimizumab versus verteporfin for neovascular age-related macular degeneration. N Engl J Med. 2006;355(14):1432–1444. doi: 10.1056/NEJMoa062655. [DOI] [PubMed] [Google Scholar]
- 6.Avery RL, Pieramici DJ, Rabena MD, et al. Intravitreal bevacizumab (Avastin) for neovascular age-related macular degeneration. Ophthalmology. 2006;113(3):363–372. doi: 10.1016/j.ophtha.2005.11.019. [DOI] [PubMed] [Google Scholar]
- 7.Spaide RF, Laud K, Fine HF, et al. Intravitreal bevacizumab treatment of choroidal neovascularization secondary to age-related macular degeneration. Retina. 2006;26(4):388–390. doi: 10.1097/01.iae.0000238561.99283.0e. [DOI] [PubMed] [Google Scholar]
- 8.Bashshur ZF, Bazarbachi A, Schakal A, et al. Intravitreal bevacizumab for the management of choroidal neovascularization in age-related macular degeneration. Am J Ophthalmol. 2006;142(1):1–9. doi: 10.1016/j.ajo.2006.02.037. [DOI] [PubMed] [Google Scholar]
- 9.Mangione CM, Lee PP, Gutierrez PR, et al. Development of the 25-item National Eye Institute Visual Function Questionnaire. Arch Ophthalmol. 2001;119(7):1050–1058. doi: 10.1001/archopht.119.7.1050. [DOI] [PubMed] [Google Scholar]
- 10.Clemons TE, Chew EY, Bressler SB, et al. National Eye Institute Visual Function Questionnaire in the Age-Related Eye Disease Study (AREDS): AREDS Report No. 10. Arch Ophthalmol. 2003;121(2):211–217. doi: 10.1001/archopht.121.2.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Klein R, Klein BE, Linton KL. Prevalence of age-related maculopathy. The Beaver Dam Eye Study. Ophthalmology. 1992;99(6):933–943. doi: 10.1016/s0161-6420(92)31871-8. [DOI] [PubMed] [Google Scholar]
- 12.Clemons TE, Milton RC, Klein R, et al. Risk factors for the incidence of advanced age-related macular degeneration in the Age-Related Eye Disease Study (AREDS): Report No. 19. Ophthalmology. 2005;112(4):533–539. doi: 10.1016/j.ophtha.2004.10.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Risk factors for neovascular age-related macular degeneration. The Eye Disease Case-Control Study Group. Arch Ophthalmol. 1992;110(12):1701–1708. doi: 10.1001/archopht.1992.01080240041025. [DOI] [PubMed] [Google Scholar]
- 14.Mitchell P, Wang JJ, Foran S, et al. Five-year incidence of age-related maculopathy lesions: The Blue Mountain Eye Study. Ophthalmology. 2002;109(6):1092–1097. doi: 10.1016/s0161-6420(02)01055-2. [DOI] [PubMed] [Google Scholar]
- 15.Tan JS, Mitchell P, Kifley A, et al. Smoking and the long-term incidence of age-related macular degeneration: the Blue Mountains Eye Study. Arch Ophthalmol. 2007;125(8):1089–1095. doi: 10.1001/archopht.125.8.1089. [DOI] [PubMed] [Google Scholar]
- 16.Thornton J, Edwards R, Mitchell P, et al. Smoking and age-related macular degeneration: A review of association. Eye (Lond) 2005;19(9):935–944. doi: 10.1038/sj.eye.6701978. [DOI] [PubMed] [Google Scholar]
- 17.DeAngelis MM, Ji F, Kim IK, et al. Cigarette smoking, CH, APOE, ELOVL4, and risk of neovascular age-related macular degeneration. Arch Ophthalmol. 2007;125(1):49–54. doi: 10.1001/archopht.125.1.49. [DOI] [PubMed] [Google Scholar]
- 18.Seddon JM, George S, Rosner B. Cigarette smoking, fish consumption, omega-3 fatty acid intake, and associations with age-related macular degeneration: the US Twin Study of Age-Related Macular Degeneration. Arch Ophthalmol. 2006;124(7):995–1001. doi: 10.1001/archopht.124.7.995. [DOI] [PubMed] [Google Scholar]
- 19.Klaver CC, Wolfs RC, Assink JJ, et al. Genetic risk of age-related maculopathy. Population-based familial aggregation study. Arch Ophthalmol. 1998;116(12):1646–1651. doi: 10.1001/archopht.116.12.1646. [DOI] [PubMed] [Google Scholar]
- 20.Klein BE, Klein R, Lee KE, et al. Risk of incident age-related eye disease in people with an affected sibling: The Beaver Dam Eye Study. Am J Epidemiol. 2001;154(3):207–211. doi: 10.1093/aje/154.3.207. [DOI] [PubMed] [Google Scholar]
- 21.Seddon JM, Ajani UA, Mitchell BD. Familial aggregation of age-related maculopathy. Am J Ophthalmol. 1997;123(6):199–206. doi: 10.1016/s0002-9394(14)71036-0. [DOI] [PubMed] [Google Scholar]
- 22.Schaumberg DA, Hankinson SE, Guo Q, et al. A prospective study of 2 major age-related macular degeneration susceptibility alleles and interactions with modifiable risk factors. Arch Ophthalmol. 2007;125(1):55–62. doi: 10.1001/archopht.125.1.55. [DOI] [PubMed] [Google Scholar]
- 23.SanGiovanni JP, Chew EY, Clemons TE, et al. Age-Related Eye Disease Study Research Group The relationship of dietary lipid intake and age-related macular degeneration in a case-control study. AREDS Report No. 20. Arch Ophthalmol. 2007;125(5):671–679. doi: 10.1001/archopht.125.5.671. [DOI] [PubMed] [Google Scholar]
- 24.Age-Related Eye Disease Study Research Group. SanGiovanni JP, Chew EY, Clemons TE, et al. The relationship of dietary carotenoids with age-related macular degeneration in a case-control study. AREDS Report No. 22. Arch Ophthalmol. 2007;125(9):1225–1232. doi: 10.1001/archopht.125.9.1225. [DOI] [PubMed] [Google Scholar]
- 25.Hyman L, Schachat AP, He Q, et al. Hypertension, cardiovascular disease, and age-related macular degeneration. Age-related Macular Degeneration Risk Factors Study Group. Arch Ophthalmol. 2000;117(3):351–358. doi: 10.1001/archopht.118.3.351. [DOI] [PubMed] [Google Scholar]
- 26.van Leeuwen R, Ikram MK, Vingerling JR, et al. Blood pressure, atherosclerosis, and the incidence of age-related maculopathy: The Rotterdam Study. Invest Ophthalmol Vis Sci. 2003;44(9):3771–3777. doi: 10.1167/iovs.03-0121. [DOI] [PubMed] [Google Scholar]
- 27.Klein R, Klein BE, Tommy SE, et al. The association of cardiovascular disease with the long-term incidence of age-related maculopathy: The Beaver Dam Eye Study. Ophthalmology. 2003;110(6):1273–1280. doi: 10.1016/S0161-6420(03)00599-2. [DOI] [PubMed] [Google Scholar]
- 28.Wright S, Yelland M, Heathcote K, et al. Fear of needles – nature and prevalence in general practice. Australian Family Physician. 2009;38(3):172–176. [PubMed] [Google Scholar]
- 29.Age-Related Eye Disease Study Research Group A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS Report No.8. Arch Ophthalmol. 2001;119(10):1417–1436. doi: 10.1001/archopht.119.10.1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Charkoudian LD, Gower EW, Solomon SD, et al. Vitamin usage patterns in the prevention of age-related macular degeneration. Ophthalmology. 2008;115(6):1032–1038. doi: 10.1016/j.ophtha.2007.08.003. [DOI] [PubMed] [Google Scholar]
- 31.Klein BE, Knudtson MD, Lee KE, et al. Supplements and age-related eye conditions: the Beaver Dam Study. Ophthalmology. 2008;115(7):1203–1208. doi: 10.1016/j.ophtha.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 32.Chang CW, Chu G, Hinz BJ, et al. Current use of dietary supplementation in patients with age-related macular degeneration. Can J Ophthalmol. 2003;38(1):27–32. doi: 10.1016/s0008-4182(03)80005-4. [DOI] [PubMed] [Google Scholar]
- 33.Ng WT, Goggin M. Awareness of and compliance with recommended dietary supplement among age-related macular degeneration patients. Clin Experiment Ophthlmol. 2006;34(1):9–14. doi: 10.1111/j.1442-9071.2006.01141.x. [DOI] [PubMed] [Google Scholar]
- 34.van Leeuwen R, Klaver CC, Vingerling JR, et al. Cholesterol and age-related macular degeneration: is there a link? Am J Ophthalmol. 2004;137(4):750–752. doi: 10.1016/j.ajo.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 35.Tomany SC, Wang JJ, van Leeuwen R. Risk factors for incident age-related macular degneration: pooled findings from three continents. Ophthalmology. 2004;111(7):1280–1287. doi: 10.1016/j.ophtha.2003.11.010. [DOI] [PubMed] [Google Scholar]
- 36.Fu AZ, Qiu Y, Radican L. Impact of fear of insulin or fear of injection on treatment outcomes of patients with diabetes. Curr Med Res Opin. 2009;25(6):1413–1420. doi: 10.1185/03007990902905724. [DOI] [PubMed] [Google Scholar]
- 37.Crockett M, Keystone J. “I hate needles” and other factors impacting on travel vaccine uptake. J Travel Med. 2005;(12 Suppl 1):S41–S46. doi: 10.2310/7060.2005.12056. [DOI] [PubMed] [Google Scholar]
- 38.Dahlin-Ivanoff S, Klepp KI, Sjostrand J, et al. Development of a health education programme for elderly with age-related macular degeneration. Patient Educ Counse. 1998;34(1):63–73. doi: 10.1016/s0738-3991(98)00041-x. [DOI] [PubMed] [Google Scholar]
- 39.Owsley C, McGwin G, Scilley K, et al. Focus groups with persons who have age-related macular degeneration: Emotional issues. Rehabil Psychol. 2006;51(1):23–29. [Google Scholar]
- 40.Michels S, Rosenfeld PJ. Treatment of neovascular age-related macular degeneration with ranibizumab/Lucentis®. Klin Monatsbl Augenheilkd. 2005;222(6):480–484. doi: 10.1055/s-2005-858315. [DOI] [PubMed] [Google Scholar]
- 41.Mitchell P, Korobelnik JF, Lanzetta P, et al. Ranibizumab (Lucentis) in neovascular age-related macular degeneration: Evidence from clinical trials. Br J Ophthalmol. 2010;92(1):2–13. doi: 10.1136/bjo.2009.159160. [DOI] [PubMed] [Google Scholar]