Abstract
Objectives. We conducted “geobehavioral” analyses by race to understand how distances among injection drug users' (IDUs') residences, drug purchase and use locations, and syringe exchange programs (SEPs) are associated with injection behaviors.
Methods. Data were from the HIV Prevention Trial Network 037 (2002–2006) site in Philadelphia, Pennsylvania, a randomized study evaluating the efficacy of a network-oriented HIV prevention intervention for IDUs. At prescreening, participants were asked the nearest intersections to their residence, where they buy and use drugs, and about their injection behaviors.
Results. Geographic distances had independent and interactive effects on injection risk behaviors and SEP use. Blacks, regardless of distance, were less likely than Whites to inject in public places (odds ratio [OR] = 0.62; 95% confidence interval [CI] = 0.43, 0.90), to use syringes after someone else (OR = 0.27; 95% CI = 0.19, 0.38), and to access syringes from SEPs (OR = 2.08; 95% CI = 1.48, 2.92). Latinos' injection behaviors were more distance-dependent than Blacks' or Whites'.
Conclusions. Distances among IDUs' homes, drug purchase and injecting sites, and prevention resources affected safe injection practices differentially by race. Understanding individuals' geographic relation to the risks and resources that surround them is an important aspect of understanding effects of the environment on health and behavior and the development of targeted interventions.
Geography has become increasingly important in understanding the epidemiology of HIV, as cities across the country observe geographic clustering of incident and prevalent cases in some neighborhoods but not in others. Injection-related HIV risk, in particular, has been demonstrated to be susceptible to place effects. For example, at the micro level, research has shown that injection drug users (IDUs) who inject in public locations, such as parks or vacant properties, are more likely to engage in riskier practices and more likely to acquire HIV and HCV.1–4 Limited access to sterile prevention supplies, such as unused syringes, bleach, or clean rinse water, in public places is a factor of increased risk in these places.1
At a more macro level, local area effects of neighborhoods also affect injection practices. Results from a study examining neighborhood differences in syringe access, use, and discard revealed that IDUs living in more economically advantaged neighborhoods were less likely to inject in public places, more likely to have a single source for syringes, and more likely to more appropriately discard syringes.5 Additionally, neighborhood characteristics such as perceived social disorder, heightened police presence, and socioeconomic disadvantage have been shown to increase injection-related risks.6–9
Geography has also gained attention in light of persistent racial disparities in HIV. Recent epidemiological evidence shows that HIV prevalence and incidence rates are significantly higher for Blacks than they are for Whites despite Blacks engaging in less HIV risk behavior.10–12 Blacks tend to live and carry out daily functions, including selection of drug and sexual partners, in neighborhoods with higher backgrounds of HIV prevalence, and, thus, are more likely to be embedded in networks that have higher HIV prevalence.13,14 Along with having higher HIV prevalence, Black neighborhoods also tend to have other characteristics that increase injection risk, including poverty, abandoned properties, and racial targeting by police.15–17 Although neighborhood studies have broadened our understanding of area effects on injection drug use, they represent only 1 means of examining geographic context on risk behavior.
We examined geographic distances between places of relevance to IDUs as an example of what we term “geobehavioral” analyses, to connote analyses by using geographic data to understand behavior and relationships and their spatial localization.18 Whereas place represents lived, meaningful environments, geography also encompasses studies of space, or the relative position between locations.19–21 The approach we employed is distinct from the study of behaviors in which analyses fix individuals within a place by using a single point location—typically, one's own residential address. For drug users, where they buy and use drugs are at least equally relevant locations of interest for understanding risk.
We examined geographic distances between places of relevance to IDUs in geobehavioral analyses—analyses using geographic data to understand the spatial localization of behavior, risk, resources, and their associations. Geographic distance is a dimension of accessibility, and represents the ease with which individuals can reach needed services.22 Thus, understanding the effects of distance also has implications for placement and utilization of prevention programs such as syringe exchange programs (SEPs). We examined how (1) distances between IDUs' residences, drug use locations, and drug purchase locations are related to place of injection (public or private); (2) distances between SEPs, IDUs' residences, drug use locations, and drug purchase locations are associated with syringe source and receptive syringe sharing; and (3) race modifies the effect of distances on injection risk to illuminate potential explanations for existing racial disparities in HIV.
METHODS
Data were from the prescreening database of the HIV Prevention Trials Network 037 conducted in Philadelphia, Pennsylvania. Data were collected from 2002 through 2006. The HIV Prevention Trials Network 037 is a phase III randomized study evaluating the efficacy of a network-oriented peer educator intervention for HIV prevention among IDUs and their network members. Prospective index participants were identified through a community-based recruitment model that employed ethnography and outreach in zip codes with a high prevalence of individuals living with HIV/AIDS as reported by the Philadelphia Department of Public Health. Outreach workers disseminated information about the study, and provided verbal and written study descriptions to prospective participants who were encouraged to consider being prescreened to determine eligibility.
Prescreening interviews were conducted in mobile assessment units that were parked in close proximity to risk pockets within the target zip code areas.23 Those who appeared eligible at prescreening were invited to complete additional screening to determine study eligibility. Details about the study intervention are reported elsewhere.24
Measures
Prescreened participants (n = 3078) were asked the address of their current residence; individuals who reported having injected drugs within the previous 6 months (n = 2599) were asked to provide the intersection nearest to where they typically purchased drugs and where they most recently injected drugs. Intersections were defined as the place where the nearest 2 cross streets meet. We determined latitudes and longitudes for intersections by using ArcView version 3.2 geographic software (Environmental Systems Research Institute Inc, Redlands, CA) and we calculated Manhattan distances (miles) between each pair of points (2-point distances) for which data were available.19 Manhattan distances are calculated along axes of right angles by using the shortest paths available by street to get from one point to another. For 2-point distances, we calculated the distances between injectors' homes and drug purchase (buy) locations, between their homes and injection (use) locations, and between their buy and use locations. Similar calculations were performed for distances between each of these locations and the location of Philadelphia's SEP sites. We also calculated 3-point and 4-point distances that combine the 2-point distances in either “geographic paths” or “average distances” among points. For example, for geographic paths, we calculated the sum of the distances from injectors' homes to drug buy locations and from drug buy to drug use locations (3-point path distance) or from home to SEP to drug buy locations to drug use locations (4-point path distance). So, paths measured routes injectors might take to procure and use drugs. For average distances, we calculated the mean distance among 3 or 4 points as a more general distance measure.
For race, participants were asked their race and whether they considered themselves to be of Latino/Hispanic (hereafter “Latino”) ethnicity. Respondents were coded as White if they indicated White race and African American if they indicated African American race, both irrespective of the response on ethnicity. Less than 5% who reported White or African American race also reported Latino origin. Those who reported Latino ethnicity predominantly classified themselves as “other” race.
Primary outcomes were place of most recent injection, usual source for obtaining syringes, and any receptive sharing of syringes and other injection equipment in the past 3 months. Place of most recent injection was recoded into 3 nominal categories: own, family's, or friend's residence (reference category); shooting gallery (1); or public place (2), which included cars, abandoned houses, or “other public places.” Syringe source was recoded into 2 categories: SEP (reference) and non-SEP. Receptive sharing of syringes, cookers, cottons, or rinse water (past 3 months) refers to sharing equipment after someone else has used it. This variable was recoded into 3 ordinal categories: never or almost never (reference), less than 12 times (about once per week; 1), and 12 times or more (more than once per week; 2).
Analysis
We analyzed data from participants who reported having injected drugs in the past 6 months (n = 2599). Exploratory data analysis included inspection of variables for missingness, frequency distributions, and geomapping of all point locations. Of the address locations that were collected from injectors, we were able to successfully geocode 1790 home addresses, 2360 drug purchase locations, and 2256 injection drug use locations. Therefore, the final sample sizes for analyses varied according to completeness of each individual point location, geocoding success, and completeness after we combined point locations to create the distance measures.
The primary outcomes—place of most recent injection, syringe source, and receptive sharing—were discrete variables, whereas the primary independent variable, distance, was continuous. In our preliminary analyses, we used analysis of variance to test for differences between the discrete levels of each of the outcomes by distance (miles) and racial differences by distance. Next, we performed multiple regression analysis to model the effects of distance and race, and their interaction, on each outcome. Place of most recent injection was a nominal outcome, so we performed multinomial regression with private residence serving as the reference level to which shooting gallery and public place were compared. We used logistic regression for the dichotomous outcome, syringe source (SEP vs non-SEP); SEP use was the reference level.
After testing the proportional odds assumption, we performed ordinal regression for the outcome variable measuring frequency of receptive sharing, with “never or almost never” serving as the reference level. In all models, we adjusted for age, gender, education, and partner status (whether someone considers himself or herself to be in a sexual relationship) and included interaction terms for distance by race. We initially adjusted for HIV status, but it consistently had no effect, so we removed it from all models. Self-reported HIV prevalence in the prescreening sample was around 2%. Among those who were behaviorally eligible for the intervention and subsequently tested (n = 829), HIV prevalence was 8.2% overall—5% for Whites, 13% for Blacks, and 7% for those who self-identified as Latino. Additionally, depending on the outcome being examined, we included other pertinent covariates, such as with whom one injected, or unstable housing, defined as living in a shelter, group home, rental room, or homeless. We used Stata/SE version 8 (StataCorp LP, College Station, TX) for all statistical analysis.
RESULTS
Of the 2599 individuals who reported having injected drugs in the past 6 months, 41% were White, 45% were Black, and 14% were Latino. The mean age was 39 years and ranged from 18 to 75 years. Seventy-five percent of the sample were men and 68% reported having a high school diploma or equivalent. A little more than half (54%) reported having a primary sexual partner. For outcome variables, 54% reported injecting in a private residence at their most recent injection, whereas 34% reported injecting in public venues, and 12% attended a shooting gallery. Thirty-seven percent of the sample regularly used SEPs as their usual source for syringes. Thirty-four percent reported receptive syringe sharing and 44% had used water, cotton, or cookers after someone else.
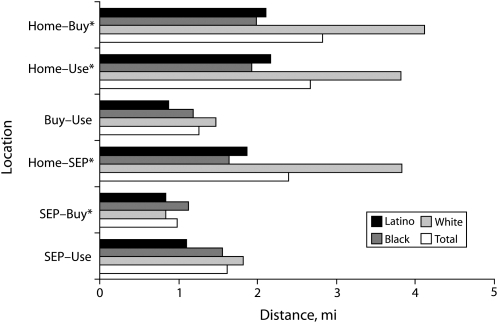
Figure 1 shows mean distances (miles) between location pairs for the total sample and by race. When place of residence is included in the location pair, we see that distances traveled for Whites to buy (F2,1635 = 47.89; P < .001) and use (F2,1562 = 24.69; P < .001) drugs, and access SEPs (F2,1775 = 81.61; P < .001), is on average twice the distance traveled for Blacks and Latinos. Thus, Blacks and Latinos live closer to where they buy and use drugs than do Whites. The distance between where drugs are bought and used was a relatively short distance for all race groups. Finally, SEPs in Philadelphia appear to be very appropriately placed. On average, they are less than 1 mile away from drug purchasing locations and an average of 1.6 miles from injection drug use locations.
FIGURE 1.
Two-point Manhattan distances of paths between injection drug users' homes, purchase locations, use locations, and syringe exchange programs (SEPs), by race: Philadelphia, PA, 2002–2006.
Note. Manhattan distances are calculated along axes of right angles by using the shortest paths available by street to get from one point to another.
*P < .05.
Race, Distance, and Place of Most Recent Injection
We fit models examining the effects of 2 distances on place of most recent injection—the path from home to buy location to use location, “pathhbu,” and the average distance among these same locations. Table 1 shows results from the model with pathhbu as the primary predictor of injecting in a shooting gallery, public venue, or private residence (reference). No significant associations were observed between path distance and shooting gallery use, between race and shooting gallery use, nor between a distance by race interaction term and shooting gallery use. Blacks, however, were significantly less likely than were Whites to inject in public places as path distance increased (odds ratio [OR] = 0.94; 95% confidence interval [CI] = 0.90, 0.98). We fit a similar model by using average distance, rather than path, and with a few exceptions, observed similar results. The effects of average distances were in the same direction, but greater in magnitude than those of pathhbu.
TABLE 1.
Multinomial Regression Results of Main and Interaction Effects of Path Distance in Miles and Race on Place of Most Recent Injection: Philadelphia, PA, 2002–2006
| Variables | Shooting Gallerya, OR (95% CI) | Public Place, OR (95% CI) |
| Pathhbu | 1.05 (1.00, 1.10) | 1.07 (1.03, 1.10) |
| Race/ethnicity | ||
| White (Ref) | 1.00 | 1.00 |
| Black | 1.41 (0.84, 2.36) | 0.62 (0.43, 0.90) |
| Latino | 0.90 (0.49, 2.11) | 0.83 (0.50, 1.36) |
| Pathhbu × race | ||
| Black | 0.96 (0.90, 1.02) | 0.94 (0.90, 0.98) |
| Latino | 1.03 (0.91, 1.17) | 1.02 (0.92, 1.12) |
| Most frequently inject with | ||
| Alone (Ref) | 1.00 | 1.00 |
| Partner, family, or friends | 1.69 (1.14, 2.49) | 0.85 (0.65, 1.12) |
| Other users | 6.98 (4.26, 11.45) | 2.72 (1.80, 4.10) |
| Housingb | ||
| Stable (Ref) | 1.00 | 1.00 |
| Unstable | 1.21 (0.72, 2.04) | 2.20 (1.56, 3.11) |
| Age | 0.96 (0.94, 0.98) | 0.96 (0.94, 0.97) |
| Gender | ||
| Men (Ref) | 1.00 | 1.00 |
| Women | 0.35 (0.22, 0.57) | 0.61 (0.45, 0.83) |
| Education | ||
| No high school diploma or equivalent (Ref) | 1.00 | 1.00 |
| High school diploma or equivalent | 0.79 (0.55, 1.14) | 1.02 (0.77, 1.34) |
| Have a primary sexual partner | ||
| No (Ref) | 1.00 | 1.00 |
| Yes | 0.59 (0.42, 0.83) | 0.69 (0.54, 0.89) |
Note. CI = confidence interval; HBU = home–buy–use; OR = odds ratio. The sample size was N = 1443. Reference level for outcome is private residence (i.e., own residence or residence of family or friend).
A place, typically an abandoned building, where injectors gather to inject drugs. In some cases, drugs and equipment can be acquired at the shooting gallery.
Stable housing is having one's own place or living with family or friend. Unstable housing is living in a rented room, shelter, halfway house, no fixed address, or other.
Race, Distance, and Regular Syringe Source
Table 2 shows the associations of distances between the nearest SEP site and home, buy, and use locations; race; and regular source of syringes. All models tested the main and multiplicative effects of race and distance on the regular use of non-SEP sources. The 3 models differ with respect to the distance measure used. Model 1 uses the distance between the nearest SEP site and injectors' homes (SEP–home); model 2 uses the distance between the nearest SEP site and drug buy location (SEP–buy); and model 3 uses the distance between the nearest SEP site and use location (SEP–use). Each model adjusts for age, gender, education, and partner status. The most common non-SEP sources used were “works sellers” (34%), friends (11%), patients with diabetes (11%), and [drug] dealers and other users (8%).
TABLE 2.
Logistic Regression Results of Main and Interaction Effects of Path Distance in Miles and Race on Regular Use of Non-SEP Sources for Syringes: Philadelphia, PA, 2002–2006
| Variables | Model 1 (n = 1776), OR (95% CI) | Model 2 (n = 1617), OR (95% CI) | Model 3 (n = 1542), OR (95% CI) |
| Pathsh | 1.06 (1.02, 1.10) | ||
| Race/ethnicity | |||
| White (Ref) | 1.00 | ||
| Black | 1.65 (1.22, 2.25) | ||
| Latino | 1.57 (1.03, 2.39) | ||
| Pathsh × race/ethnicity | |||
| Black | 1.10 (0.99, 1.22) | ||
| Latino | 1.14 (0.95, 1.37) | ||
| Pathsb | 1.57 (1.25, 1.97) | ||
| Race/ethnicity | |||
| White (Ref) | 1.00 | ||
| Black | 2.08 (1.48, 2.92) | ||
| Latino | 0.80 (0.46, 1.38) | ||
| Psb × race/ethnicity | |||
| Black | 0.80 (0.60, 1.07) | ||
| Latino | 6.70 (2.32, 19.4) | ||
| Pathsu | 1.06 (1.00, 1.12) | ||
| Race/ethnicity | |||
| White (Ref) | 1.00 | ||
| Black | 1.84 (1.39, 2.44) | ||
| Latino | 0.63 (0.37, 1.06) | ||
| Pathsu × race/ethnicity | |||
| Black | 1.00 (0.92, 1.08) | ||
| Latino | 5.35 (2.53, 11.3) | ||
Note. CI = confidence interval; OR = odds ratio; SB = SEP–buy; SEP = syringe exchange program; SH = SEP–home; SU = SEP–use. Reference level for outcome is regular SEP use. Non-SEP syringe sources include works sellers, patients with diabetes, friends, drug dealers, and other users. Model 1 analyzed the distance between the nearest SEP site and injectors' homes (SEP–home), model 2 analyzed the distance between the nearest SEP site and drug buy location (SEP–buy), and model 3 analyzed the distance between the nearest SEP site and drug use location (SEP–use). Each model is adjusted for age, gender, education, and partner status (whether the individual has a primary sexual partner).
In model 1, because there were no significant interaction effects, we interpreted the main effects of race and distance as independent effects. We found that for each mile of increased distance between SEPs and IDUs' homes, there was a 6% increased likelihood of using non-SEP sources for syringe access. In this same model, results showed that both Blacks (OR = 1.65; 95% CI = 1.22, 2.25) and Latinos (OR = 1.57; 95% CI = 1.03, 2.39) were significantly more likely than were Whites to access syringes from sources other than SEPs. In models 2 and 3, we found evidence for significant interactions with distance for Latinos, but not for Blacks. As distances increased, Latinos were more likely to use non-SEP sources to access syringes; distance did not affect where Blacks acquired syringes. In both models 2 and 3, we found that the greater the distance between SEP and buy locations (OR = 6.70; 95% CI = 2.32, 19.4) and use locations (OR = 5.35; 95% CI = 2.53, 11.3), Latinos were much more likely than were Whites to access syringes from non-SEP sources.
Race, Distance, and Receptive Sharing of Injection Equipment
Results on the effects of distance on receptive sharing of injection equipment are displayed in Table 3. For these models, we used the average distance among all 4 injection-related sites—SEP, home, buy locations, and use locations. We also fit models by using path distances that yielded similar results. We examined the effect of average distance on (1) receptive syringe sharing and (2) using water, cookers, and cotton after someone. Similar to our results for regular source of syringes, we observed significant interaction effects for Latinos, but not for Blacks. Main effects for Blacks indicated that they were the least likely group to use syringes (OR = 0.27; 95% CI = 0.19, 0.38) or other injection equipment (OR = 0.37; 95% CI = 0.27, 0.52) after someone else, an effect not moderated by distance. Latinos' use of injection equipment (syringes, water, cooker, cotton), however, was moderated by distance, showing that their odds of using a syringe or other injection equipment after someone else increased by 21% and 24%, respectively, with each mile increase in average distance among the 4 locations. Results also showed increased odds of receptive syringe sharing after a partner, relative, or friend (OR = 1.94; 95% CI = 1.51, 2.50) compared with other nonkin, nonfriend users (OR = 1.59; 95% CI = 1.10, 2.31). With regard to the sharing of rinse water, cooker, and cotton, individuals were more than twice as likely to use these after a partner, relative, or friend (OR = 2.18; 95% CI = 1.73, 2.73) as they were after “other” users. Regular use of non-SEP sources of syringes increased the odds of receptive syringe sharing by 60%, but had no effect on the use of water, cooker, and cotton after someone.
TABLE 3.
Ordinal Regression Results of Main and Interaction Effects of Average Path Distance in Miles and Race on Receptive Syringe Sharing, Philadelphia, PA, 2002–2006
| Variables | Used Syringe After Someone (n = 1448), OR (95% CI) | Used Water, Cooker, or Cotton After Someone (n = 1450), OR (95% CI) |
| Average distanceshbu | 0.89 (0.83, 0.96) | 0.97 (0.91, 1.03) |
| Race/ethnicity | ||
| White (Ref) | 1.00 | 1.00 |
| Black | 0.27 (0.19, 0.38) | 0.37 (0.27, 0.52) |
| Latino | 0.58 (0.38, 0.88) | 0.55 (0.37, 0.83) |
| Average distanceshbu × race/ethnicity | ||
| Black | 1.11 (0.96, 1.27) | 1.03 (0.92, 1.16) |
| Latino | 1.21 (1.04, 1.40) | 1.24 (1.03, 1.47) |
| Most frequently inject with | ||
| Alone (Ref) | 1.00 | 1.00 |
| Partner, family, or friends | 1.94 (1.51, 2.50) | 2.18 (1.73, 2.73) |
| Other users | 1.59 (1.10, 2.31) | 1.34 (0.95, 1.90) |
| Place of most recent injection | ||
| Private residence (Ref) | 1.00 | 1.00 |
| Shooting gallerya or public venue | 1.63 (1.28, 2.09) | 1.54 (1.23, 1.92) |
| Syringe source | ||
| SEP (Ref) | 1.00 | 1.00 |
| Non-SEP | 1.60 (1.25, 2.04) | 1.05 (0.85, 1.31) |
| Age | 1.00 (0.99, 1.01) | 1.00 (0.99, 1.02) |
| Gender | ||
| Men (Ref) | 1.00 | 1.00 |
| Women | 1.59 (1.21, 2.08) | 1.20 (0.93, 1.54) |
| Education | ||
| No high school diploma or equivalent (Ref) | 1.00 | 1.00 |
| High school diploma or equivalent | 0.86 (0.67, 1.10) | 1.14 (0.90, 1.44) |
| Have a primary sexual partner | ||
| No (Ref) | 1.00 | 1.00 |
| Yes | 0.92 (0.73, 1.16) | 0.86 (0.70, 1.07) |
Note. CI = confidence interval; OR = odds ratio; SEP = syringe exchange program; SHBU = SEP–home–buy–use.
A place, typically an abandoned building, where injectors gather to inject drugs. In some cases, drugs and equipment can be acquired at the shooting gallery.
DISCUSSION
Distances that IDUs traverse in procuring and using drugs are related to injection risk behaviors, but the relationship varies by race. Injection-related behaviors among Blacks tended to be less distance-dependent than among Whites or Latinos. Independent of distance, Blacks were less likely to inject in public places or to inject after someone else than were Whites or Latinos. This is consistent with studies reporting that Blacks engage in less risk behavior than do Whites.10–12
On the other hand, our results also showed that, regardless of distance, Blacks were significantly more likely to access syringes from non-SEP sites, including works sellers, drug dealers, and other users. This is disturbing, but consistent with other findings from Philadelphia and other major US cities.7,8,25 In a study assessing the impact of Operation Safe Streets (a police intervention conducted in Philadelphia from 2002 to 2003 that increased the presence of police officers by stationing them on select street corners in drug-active neighborhoods), researchers found that the intervention had an unintended effect of significantly reducing Blacks' use of SEPs up to 9 months postimplementation.7 Despite the decriminalized (not seeking to increase arrests) approach of the Operation Safe Streets intervention, Blacks' use of SEPs declined at a rate of more than twice that of Whites.7 Our results show that Blacks, who live significantly closer to SEPs than do Whites, were up to 2 times more likely than were Whites to access syringes from non-SEP sites. This suggests that geographic accessibility is not a factor in SEP utilization for Blacks. Other reasons such as racial profiling, mistrust of the police, secondary syringe exchange (getting clean syringes from other SEP participants), and stigma may be more prominent. The finding deserves some public health attention in light of SEPs' established effectiveness in decreasing injection risk, preventing HIV, and serving as a point of entry into other services needed by IDUs, primarily drug treatment.26–32
Despite Blacks and Latinos having similar average distances among the 4 locations, significant interactions with distance were observed for Latinos only. Latinos with greater distances between SEPs and buy and use locations were significantly less likely than were Whites to use SEPs as their regular syringe source. Further, unlike Blacks, compared with Whites, Latinos were more likely to engage in receptive sharing of injection equipment as average distance among the 4 locations increased. This may be attributable to the fact that the Latino community in Philadelphia is much smaller and more concentrated than the Black community. Our data do not address why Latinos appear to be more distance-dependent than are Blacks and Whites. Additional research is warranted to understand the experience of Latino IDUs.
Other results showed that the odds of receptive sharing of injection equipment with partners, relatives, and friends were higher than were the odds of using after other, less well-known users. Whereas not using after near-strangers is a helpful precaution, it is important to not use syringes and other injection equipment after anyone—including family and friends—particularly for Blacks who have high rates of HIV in their social networks and neighborhoods. Refusing to engage in receptive sharing with friends or family may present challenges, as it could raise suspicion of potential infection of or by the person refusing. At the same time, injecting in isolation from others is discouraged because it has been shown to increase the risk of overdose.33,34 Interventions that address issues around stigma, open communication, and supporting each other to protect everyone's health are needed, particularly among users who are socially close such as family and close friends. Additionally, stronger efforts should be taken to ensure that every IDU has consistent and convenient access to his or her own sterile injection equipment, so that the need to use syringes and other injection equipment after others is eliminated. SEPs contribute to this mission, and, although safe injection facilities are currently politically unpopular in the United States, the data also highlight their potential value.35–38
We analyzed novel data by using point locations of where IDUs purchase and inject their drugs to help illuminate geographic predictors of risk that residential address locations cannot do alone. Analyzing distances offers a more nuanced approach to understanding how geography influences HIV risk behaviors, incidence, and prevalence. Because HIV prevalence in our sample was insufficient for analysis, we were limited to examining behavior as an endpoint. It is noteworthy that despite our results indicating less risky injection behavior among Blacks, χ2 results of race by HIV serostatus among study enrollees indicated significantly higher HIV prevalence among Blacks compared with Whites and Latinos. This is consistent with other studies and highlights the limitations of behaviors in explaining racial disparities in HIV; however, behavior remains a necessary factor in transmission.
The data used were nonrandom and cross-sectional; therefore, caution should be taken in making causal interpretations. We did not have complete data for all prescreened injectors, but instead reported on available data. Responses were voluntary and answering survey questions, particularly related to specific address locations of one's residence and illegal activities, may have presented concerns for some respondents. Respondents with missing location information were significantly more likely to inject in public places and shooting galleries and to not use SEPs as their regular source of syringes, but were not more likely to engage in receptive sharing of injection equipment (data not shown). Because the initial sample was not a probability sample, the missingness likely had little effect on generalizability. We feel our results can be generalized to similar diverse populations of injectors who are street-recruited from high-risk areas in urban settings. The consistency of our results with IDU studies in other cities supports this claim.1–4,8,25–27
Notwithstanding the limitations, the use of novel data to report on geobehavioral risk for HIV among a large sample of injectors is a major strength of our study and makes a contribution to our understanding of racial disparities in HIV. Because of the greater HIV prevalence in minority networks and neighborhoods, the least bit of risky behavior could result in transmission. Where people are located in relation to the risks and resources that surround them is an important aspect of understanding effects of the environment on health and behavior, and is also important for the development of interventions. Geographic clustering of HIV in minority urban neighborhoods presents unique opportunities for place-based interventions because, to some degree, the epidemic is geographically contained. Individual preventive measures, such as drug treatment, syringe hygiene, and regular HIV testing and care continue to be important.
Acknowledgments
This work was supported by the National Institutes of Health grants to the Penn HIV Prevention Trials Unit (grant U01 AI048014) and the Penn Center for AIDS Research (grant P30 AI45008).
The authors would also like to thank all study staff and the participants who provided the data.
Human Participant Protection
This study was approved by the Office of Human Research at the University of Pennsylvania School of Medicine and ongoing ethical guidance was provided by the HIV Prevention Trials Network Ethics Working Group.
References
- 1.Latkin C, Mandell W, Vlahov D, Oziemkowska M, Knowlton A, Celentano D. My place, your place, and no place: behavior settings as a risk factor for HIV-related injection practices of drug users in Baltimore, Maryland. Am J Community Psychol 1994;22(3):415–430 [DOI] [PubMed] [Google Scholar]
- 2.Celentano DD, Vlahov D, Cohn S, Anthony JC, Solomon L, Nelson KE. Risk factors for shooting gallery use and cessation among intravenous drug users. Am J Public Health 1991;81(10):1291–1295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Klein H, Levy J. Shooting gallery users and HIV risk. J Drug Issues 2003;33(3):751–767 [Google Scholar]
- 4.Thorpe LE, Ouellet LJ, Levy J, Williams IT, Monterroso ER. Hepatitis C virus infection: prevalence, risk factors and prevention of opportunities among young injection drug users in Chicago, 1997–1999. J Infect Dis 2000;182(6):1588–1594 [DOI] [PubMed] [Google Scholar]
- 5.Buchanan D, Shaw S, Teng W, Hiser P, Singer M. Neighborhood differences in patterns of syringe access, use, and discard among injection drug users: implications for HIV outreach and prevention education. J Urban Health 2003;80(3):438–454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Latkin CA, Williams CT, Wang J, Curry A. Neighborhood social disorder as a determinant of drug injection behaviors: a structural equation modeling approach. Health Psychol 2005;24(1):96–100 [DOI] [PubMed] [Google Scholar]
- 7.Davis CS, Burris S, Kraut-Becher J, Lynch KG, Metzger D. Intensive street-level police intervention on syringe exchange program use in Philadelphia, PA. Am J Public Health 2005;95(2):233–236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cooper H, Moore L, Gruskin S, Krieger N. The impact of a police drug crackdown on drug injectors' ability to practice harm reduction: a qualitative study. Soc Sci Med 2005;61(3):673–684 [DOI] [PubMed] [Google Scholar]
- 9.Rhodes T, Singer M, Bourgois P, Friedman SR, Strathdee SA. The social structural production of HIV risk among injection drug users. Soc Sci Med 2005;61(5):1026–1044 [DOI] [PubMed] [Google Scholar]
- 10.Hallfors DD, Iritani BJ, Miller WC, Bauer DJ. Sexual and drug behavior patterns and HIV and STD racial disparities: the need for new directions. Am J Public Health 2007;97(1):125–132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ellen JM, Aral SO, Madger LS. Do differences in sexual behavior account for the racial/ethnic differences in adolescents' self-reported history of a sexually transmitted disease? Sex Transm Dis 1998;25(3):125–129 [DOI] [PubMed] [Google Scholar]
- 12.Broz D, Ouellet LJ. Racial and ethnic changes in heroin injection in the United States: implications for the HIV/AIDS epidemic. Drug Alcohol Depend 2008;94(1–3):221–233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Laumann EO, Youm Y. Racial/ethnic group differences in the prevalence of sexually transmitted diseases in the United States: a network explanation. Sex Transm Dis 1999;26(5):250–261 [DOI] [PubMed] [Google Scholar]
- 14.Adimora AA, Schoenbach VJ. Social context, sexual networks, and racial disparities in rates of sexually transmitted infections. J Infect Dis 2005;191:S115–S122 [DOI] [PubMed] [Google Scholar]
- 15.Williams CT, Latkin CA. Neighborhood socioeconomic status, personal network attributes, and use of heroin and cocaine. Am J Prev Med 2007;32(suppl 6):S203–S210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Burris S, Blankenship KM, Donoghoe M, et al. Addressing the “risk environment” for injection drug users: the mysterious case of the missing cop. Milbank Q 2004;82(1):125–156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maas B, Fairbairn N, Kerr T, Li K, Montaner JS, Wood E. Neighborhood and HIV infection among IDU: place of residence independently predicts HIV infection among a cohort of injection drug users. Health Place 2007;13(2):432–439 [DOI] [PubMed] [Google Scholar]
- 18.Camara G, Monteiro AM, Fucks SD, Carvalho MS. Spatial analysis and GIS: a primer. Available at: http://www.dpi.inpe.br/gilberto/tutorials/spatial_analysis/spatial_analysis_primer.pdf. Accessed June 12, 2009
- 19.Agnew J. The United States in the World Economy Cambridge, England: Cambridge University Press; 1987 [Google Scholar]
- 20.Kearns RA, Joseph AE. Space in its place: developing the link in medical geography. Soc Sci Med 1993;37(6):711–717 [DOI] [PubMed] [Google Scholar]
- 21.McLafferty S. Placing substance abuse: geographical perspectives on substance use and addiction. : Thomas YF, Richardson D, Cheung I, Geography and Drug Addiction New York, NY: Springer; 2008 [Google Scholar]
- 22.Penchansky R, Thomas JW. The concept of access: definition and relationship to consumer satisfaction. Med Care 1981;19(2):127–140 [DOI] [PubMed] [Google Scholar]
- 23.Perkins WE, Metzger DS. AIDS in Philadelphia: emerging from the shadow of crack. : Bowser BP, Quimby E, Singer M, When Communities Assess Their AIDS Epidemics: Results of Rapid Assessment of HIV/AIDS in Eleven Cities New York, NY: Lexington Books; 2007 [Google Scholar]
- 24.Latkin CA, Donnell D, Metzger D, et al. The efficacy of a network intervention to reduce HIV risk behaviors among drug users and risk partners in Chiang Mai, Thailand, and Philadelphia, USA. Soc Sci Med 2009;68(4):740–748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bluthenthal RN, Kral AH, Lorvick J, Watters JK. Impact of law enforcement on syringe exchange programs: a look at Oakland and San Francisco. Med Anthropol 1997;18(1):61–83 [DOI] [PubMed] [Google Scholar]
- 26.Watters JK, Estilo MJ, Clark GL, Lorvick J. Syringe and needle exchange as HIV/AIDS prevention for injection drug users. JAMA 1994;271(2):115–120 [PubMed] [Google Scholar]
- 27.Vlahov D, Junge B. The role of needle exchange programs in HIV prevention. Public Health Rep 1998;113(suppl 1):75–80 [PMC free article] [PubMed] [Google Scholar]
- 28.Strathdee SA, Celentano DD, Shah N, et al. Needle-exchange attendance and health care utilization promote entry into detoxification. J Urban Health 1999;76(4):448–460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vertefeuille J, Marx MA, Tun W, et al. Decline in self-reported high-risk injection-related behaviors among HIV-seropositive participants in the Baltimore needle exchange program. AIDS Behav 2000;4(4):381–388 [Google Scholar]
- 30.Bluthenthal RN, Kral AH, Gee L, Erringer EA, Edlin BR. The effect of syringe exchange use on high-risk injection drug users: a cohort study. AIDS 2000;14(5):605–611 [DOI] [PubMed] [Google Scholar]
- 31.Latkin CA, Davey MA, Hua W. Needle exchange program utilization and entry into drug user treatment: is there a long-term connection in Baltimore, Maryland. Subst Use Misuse 2006;41(14):1991–2001 [DOI] [PubMed] [Google Scholar]
- 32.Huo D, Ouellet LJ. Needle exchange and injection-related risk behaviors in Chicago: a longitudinal study. J Acquir Immune Defic Syndr 2007;45(1):108–114 [DOI] [PubMed] [Google Scholar]
- 33.Davidson PJ, McLean RL, Kral AH, Gleghorn AA, Edlin BR, Moss AR. Fatal heroin-related overdose in San Francisco, 1997–2000: a case for targeted intervention. J Urban Health 2003;80(2):261–273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tobin KW, Hua W, Costenbader EC, Latkin CA. The association between change in social network characteristics and non-fatal overdose: results from the SHIELD study in Baltimore, MD, USA. Drug Alcohol Depend 2007;87(1):63–68 [DOI] [PubMed] [Google Scholar]
- 35.Wood E, Tyndall MW, Montaner JS, Kerr T. Summary of findings from the evaluation of a pilot medically supervised safer injecting facility. CMAJ 2006;175(11):1399–1404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.van Beek I, Gilmour S. Preference to have used a medically supervised injecting centre among injecting drug users in Kings Cross, Sydney. Aust N Z J Public Health 2000;24(5):540–542 [DOI] [PubMed] [Google Scholar]
- 37.Salmon AM, Thein HH, Kimber J, Kaldor JM, Maher L. Five years on: what are the community perceptions of drug-related public amenity following the establishment of the Sydney Medically Supervised Injecting Centre? Int J Drug Policy 2007;18(1):46–53 [DOI] [PubMed] [Google Scholar]
- 38.Hunt N, Lloyd C, Kimber J, Tompkins C. Public injecting and willingness to use a drug consumption room among needle exchange programme attendees in the UK. Int J Drug Policy 2007;18(1):62–65 [DOI] [PubMed] [Google Scholar]