Abstract
Stigma and discrimination toward obese persons are pervasive and pose numerous consequences for their psychological and physical health. Despite decades of science documenting weight stigma, its public health implications are widely ignored. Instead, obese persons are blamed for their weight, with common perceptions that weight stigmatization is justifiable and may motivate individuals to adopt healthier behaviors. We examine evidence to address these assumptions and discuss their public health implications. On the basis of current findings, we propose that weight stigma is not a beneficial public health tool for reducing obesity. Rather, stigmatization of obese individuals threatens health, generates health disparities, and interferes with effective obesity intervention efforts. These findings highlight weight stigma as both a social justice issue and a priority for public health.
Negative attitudes toward obese persons are pervasive in North American society. Numerous studies have documented harmful weight-based stereotypes that overweight and obese individuals are lazy, weak-willed, unsuccessful, unintelligent, lack self-discipline, have poor willpower, and are noncompliant with weight-loss treatment.1–3 These stereotypes give way to stigma, prejudice, and discrimination against obese persons in multiple domains of living, including the workplace, health care facilities, educational institutions, the mass media, and even in close interpersonal relationships.1–3 Perhaps because weight stigma remains a socially acceptable form of bias, negative attitudes and stereotypes toward obese persons have been frequently reported by employers, coworkers, teachers, physicians, nurses, medical students, dietitians, psychologists, peers, friends, family members,1–4 and even among children aged as young as 3 years.5
Recent estimates suggest that the prevalence of weight discrimination has increased by 66% over the past decade,6 and is now comparable to prevalence rates of racial discrimination in America.7 Despite several decades of literature documenting weight stigma as a compelling social problem,1,2,8,9 this form of stigma is rarely challenged in North American society and its public health implications have been primarily ignored. Instead, prevailing societal attributions place blame on obese individuals for their excess weight, with common perceptions that weight stigmatization is justifiable (and perhaps necessary) because obese individuals are personally responsible for their weight,10 and that stigma might even serve as a useful tool to motivate obese persons to adopt healthier lifestyle behaviors.11–13
We have examined existing evidence to address these assumptions about weight stigma and discuss their public health implications. Documentation of the stigma of obesity has been extensively reviewed elsewhere,1,2,4 thus, our aim was to highlight relevant evidence from this body of work to examine public health implications of weight stigma, an issue that has received little attention in the obesity field.
We obtained articles cited in this paper through comprehensive literature searches in computerized medical and social science databases, including PubMed, PsycINFO, and SCOPUS. Search terms were limited to various keyword combinations pertaining specifically to body weight and stigma descriptors to identify studies examining the relationship between weight stigma and public health, and emotional and physical health consequences of obesity stigma. (For examples of descriptor search terms, please refer to Puhl and Heuer.2) We also conducted manual searches for specific authors and journals that have published relevant research on these topics. In addition, we retrieved references from a recent comprehensive systematic review of peer-reviewed research studies documenting bias and stigma toward obese individuals that we recently published.2 The vast majority (87%) of studies we included were published in the past decade, with the exception of several studies published earlier that are cited when relevant to the historical context of the discussion or to provide 7 examples of landmark studies.
On the basis of the current evidence, we conclude that weight stigma is not a beneficial public health tool for reducing obesity or improving health. Rather, stigmatization of obese individuals poses serious risks to their psychological and physical health, generates health disparities, and interferes with implementation of effective obesity prevention efforts. This evidence highlights the importance of addressing weight stigma as both a social justice issue and a priority in public health interventions to address obesity.
DISEASE STIGMA AND PUBLIC HEALTH
In the field of public health, stigma is a known enemy. Throughout history, stigma has imposed suffering on groups vulnerable to disease and impaired efforts to thwart the progression of those diseases. Disease stigma occurs when groups are blamed for their illnesses because they are viewed as immoral, unclean, or lazy.14 For example, in 19th century America, Irish immigrants were commonly believed to be responsible for epidemic diseases because they were “filthy and unmindful of public hygiene.”14(p4) As large numbers of Irish-born immigrants died of cholera and other diseases, many viewed their deaths as acts of retribution upon the “sinful and spiritually unworthy.”14(p36) When African Americans were dying from tuberculosis at the beginning of the 20th century, rather than investing in prevention or treatment of tuberculosis, many cities’ authorities issued warnings to its White citizens against commingling with or hiring African Americans.15 Even the stigmatization of injection drug users and individuals with gonorrhea has been denounced as a barrier to testing and treatment.16,17 These examples have resulted in a broad understanding of the implications of stigma for public health. According to Herek et al.,
Historical examples abound of stigma interfering with collective responses to diseases ranging from cholera to syphilis. In all of these cases, the social construction of illness incorporated moral judgments about the circumstances in which it was contracted as well as preexisting hostility toward the groups perceived to be most affected by it.18(p538)
In the case of HIV/AIDS, the detrimental role of stigma has become so clear that national and international health agendas explicitly identify stigma and discrimination as major barriers to effectively addressing the epidemic. As early as the mid-1980s, just a few years after the disease was initially identified, discrimination against those at risk for HIV/AIDS was identified as counterproductive,19 and early public health policies included protections for patients’ privacy and confidentiality.20 As it became more evident that stigma and discrimination were among the root causes of vulnerability to HIV/AIDS, the United Nations General Assembly Special Session on HIV/AIDS adopted the Declaration of Commitment in 2001, which pledged signatory states to “develop strategies to combat stigma and social exclusion connected with the epidemic.”21(p9) Subsequently, stigma and discrimination were chosen as the theme for the 2002–2003 World AIDS Campaign.22 In 2007, the Joint United Nations Programme on HIV/AIDS issued the report, Reducing HIV Stigma and Discrimination: A Critical Part of National AIDS Programmes, which provides strategies for centralizing the reduction of stigma and discrimination within national responses to the disease. Recommendations from the report include providing funding and programming activities for multifaceted national approaches to the reduction of HIV stigma and discrimination.23
Thus, within current public health ideology there is clear recognition of the critical obstacles created by disease stigma. Bayer notes:
In the closing decades of the 20th century, a broadly shared view took hold that the stigmatization of those who were already vulnerable provided the context within which diseases spread, exacerbating morbidity and mortality… . In this view, it was the responsibility of public health officials to counteract stigma if they were to fulfill their mission to protect the communal health.24(p252)
In sharp contrast, the stigma of obesity has not been addressed as a legitimate concern that requires the attention of those working to combat obesity, and is rarely discussed in the context of public health.25,26 In fact, weight stigma has been suggested by some as a method for obesity control.11–13 The lack of attention to weight stigma has persisted despite nearly 5 decades of scientific research documenting weight stigma and its consequences for obese individuals.1,2 Its absence was noted in the 1960s when stigma research was first emerging. In 1968, Cahnman published the article entitled “The Stigma of Obesity,” in which he wrote:
Obesity is hardly ever mentioned in the writings of sociologists, and not at all in the literature on social deviance. This omission is amazing… . Clearly, in our kind of society, with its stress on affluence and upward mobility, being overweight is considered to be detrimental to health, a blemish to appearance, and a social disgrace.27(p283)
This omission remains almost 50 years later. Even as obesity rates have risen dramatically, weight stigma is rarely, if ever, afforded the same recognition or intervention as other disease stigmas.
Although there is significant consensus that stigma undermines public health, this principle has not been applied to the obesity epidemic. Common societal assumptions about obesity, including the notion that obese individuals are to blame for their weight, contribute to the disregard of weight stigma and its impact on emotional and physical health. An examination of these assumptions in light of current scientific evidence reveals that obesity stigma creates significant barriers in efforts to address obesity and deserves recognition in the public health agenda.
COUNTERING ASSUMPTIONS THAT PERPETUATE WEIGHT STIGMA
Social constructions of body weight are ingrained in the way that our society perceives and reacts to obesity.10,28 According to Herek, the social meaning of disease involves assigning responsibility and blame, so that those afflicted with disease become regarded as either victims or perpetrators.18 Society regularly regards obese persons not as innocent victims, but as architects of their own ill health, personally responsible for their weight problems because of laziness and overeating.29–31 These common assumptions provide the foundation for weight stigma, a prejudice that is often dismissed as acceptable and necessary. Not only is weight stigma viewed as a beneficial incentive for weight loss, but it is also assumed that the condition of obesity is under personal control,10,28,32,33 implying that the social influence of weight stigma will be sufficient to produce change.
Although these assumptions about obesity and weight stigma are prevalent in our national mindset, considerable scientific evidence has emerged to challenge them. To optimize obesity prevention and intervention efforts, these assumptions must be addressed within the sphere of public health, with recognition of the harmful impact of weight stigma on quality of life and the need to eliminate stigma from current and future public health approaches to the obesity epidemic. We present scientific evidence relevant to these societal assumptions.
Weighty Misperceptions
Societal attributions about the causes of obesity contribute significantly to expressions of weight stigma. Experimental research in psychology consistently demonstrates that obese persons are stigmatized because their weight is perceived to be caused by factors within personal control (e.g., overeating and lack of exercise).9,34–37 More than 2 decades ago Weiner et al. first assessed the relationship between perceptions of personal responsibility and stigmatizing conditions, and found that conditions rated low on personal responsibility (such as Alzheimer's disease) were rated high on liking and elicited pity and intentions to help from others.28 However, individuals with stigmatizing conditions rated high on personal responsibility (e.g., obesity and drug addiction) were disliked, evoked little pity and high anger, and received low ratings of helping tendencies.28
Research findings since that time have followed suit. In a study examining attitudes toward 66 different diseases and health conditions (including obesity), the attributed degree of personal responsibility for the disease predicted social distance and rejection by participants.38 Experimental research additionally shows that providing individuals with information emphasizing personal responsibility for obesity increases negative stereotypes toward obese persons, whereas information highlighting the complex etiology of obesity (such as biological and genetic contributors) improves attitudes and reduces stereotypes.39
The view that obesity is a matter of personal responsibility is the prevailing message in the media.29–31,40,41 News coverage of the personal causes and solutions to obesity significantly outnumber other societal attributions of responsibility.29 Entertainment media also communicate anti-fat messages and reinforce perceptions that body weight is within personal control.42–44 The current societal message is that both the cause and the solution for obesity reside within the individual. Thus, the pervasiveness of the “personal responsibility” message plays a key role in stigmatization, and serves to justify stigma as an acceptable societal response.45–47
However, this prevailing message does not accurately reflect the science. Many significant contributors to obesity are beyond the control of individuals. In addition to the important role of genetic and biological factors regulating body weight,48–50 multiple social and economic influences have significantly altered the environment to promote and reinforce obesity.51 As Seng Lee notes,
We have created a biology–environment mismatch, as the human weight regulation is unable to evolve fast enough to keep pace with the environmental change.50(p45)
Advancements in workplace technology and reduction of manual labor have resulted in decreased energy expenditure. The built environment has decreased opportunities for healthy lifestyle behaviors through factors such as urban design, land use, public transportation availability,52,53density and location of food stores and restaurants,54 and neighborhood barriers such as safety and walkability.53,55,56
Significant changes have taken place in the food environment with increased accessibility of inexpensive foods. Prices of calorie-dense foods and beverages have decreased considerably in contrast to increasing prices of fresh fruits, vegetables, fish, and dairy items,51 contributing to increased consumption of unhealthy foods, especially as the portion sizes of these items have grown considerably larger.57 Significant marketing and advertising of unhealthy, energy-dense foods by the food industry contribute to excessive food consumption in important ways,58,59 especially for children, who are heavily targeted.60,61
These complex societal and environmental conditions that have created obesity necessitate that we move beyond the narrow focus that targets the individual as both the culprit and the solution for obesity. Public health efforts must address the multiple forces contributing to the development and maintenance of obesity and recognize that individual behaviors are powerfully shaped by the obesogenic environment. As Cohen concludes, “a more accurate conceptualization of the obesity epidemic is that people are responding to the forces in their environment, rather than lacking in willpower and self-control.”62(pS141) There is increasing consensus that environmental change is essential to the solution of obesity.62–64
There is also considerable scientific consensus about the challenge of significant long-term weight loss.65 A systematic review of 80 randomized clinical trials of weight-loss interventions with at least 1 year of follow-up (including interventions of diet, diet and exercise, exercise, meal replacements, very-low-calorie diets, and weight-loss medications) found the mean weight loss across studies to be 5% to 9% at 6 months, with a subsequent plateau across most interventions.66 These findings parallel a recent meta-analysis of 46 randomized controlled trials that revealed a maximum net treatment effect of approximately 6% of body weight lost at 1-year follow-up.67 Many other recent scientific reviews of multiple weight-loss trials and programs produced, on average, no more than 10% weight loss at 1- or 2-year follow-up.68–71
As a result of these and other consistent findings demonstrating modest results of most weight-loss interventions, there is recognition in the scientific community that existing dietary programs and medications can produce no more than an average of 10% weight loss.72 This evidence has prompted agreement among a number of expert panels and scientific groups (including the Institute of Medicine, World Health Organization, Preventive Task Force, Canadian Task Force of Preventive Health Care, and National Heart, Lung, and Blood Institute) that health care providers should counsel patients to set a goal of 10% reduction in total body weight rather than struggle to attain ideal body weight.73 For obese individuals who want to lose substantial body weight to improve their health (as opposed to individuals who want to obtain modest weight loss for aesthetic reasons), a 10% weight loss means that many obese persons will remain obese and continue to be vulnerable to weight stigma.
The high rate of weight regain following weight loss is equally concerning. Most weight losses are not maintained and individuals regain weight after completing treatment.67,70 Patients who have lost weight through lifestyle modification typically regain 30% to 35% of their lost weight during the year following treatment, and regain most (if not all) of their lost weight within 5 years.65,68,74–76 The consistent findings in this area indicate that preventing weight regain is extremely challenging.77 As a result, experts in the obesity field have concluded that weight regain occurs in practically all dietary and behavioral interventions,65 and other researchers have asserted that
Dieters who manage to sustain a weight loss are the rare exception, rather than the rule. Dieters who gain back more weight than they lost may very well be the norm, rather than an unlucky minority.70(p230)
Despite weight regain, individuals can experience important improvements in health with modest weight loss of approximately 10%,75,78 including reductions in obesity-related health complications such as type 2 diabetes and hypertension68 and improvements in cardiovascular risk.77 However, even if modest weight loss improves some health indices, it is unlikely to significantly alter appearance or translate to a nonobese body mass index (BMI; weight in kilograms divided by height in meters squared) for most people, and is doubtful to be sufficient to reduce weight stigma and discrimination.
It is also important to note increasing research documenting a considerable percentage of overweight and obese persons who are metabolically healthy and nonoverweight individuals who exhibit metabolic and cardiovascular risk factors.79 Although excess weight can incur significant implications for disease risk, variation in health indices observed in people with similar body mass indicates caution in generalizations made about body size and health behaviors, which can further contribute to stigma and misleading stereotypes. For those individuals without metabolic risk factors, losing weight may not be important for improving health. The recognition that there are obese individuals who are metabolically healthy and nonoverweight individuals who are metabolically obese challenges weight-based stereotypes and reinforces the heterogeneous nature of obesity.80,81
Because weight-based stereotypes and prejudice so often emerge from attributions that obesity is caused and maintained by personal characteristics such as laziness or lack of willpower,10,47 there is a clear need for increased public awareness and education about the complex etiology of obesity and the significant obstacles present in efforts to achieve sustainable weight loss. The prevailing societal and media messages that reinforce blame on obese persons need to be replaced with messages that obesity is a chronic disease with a complex etiology, and a lifelong condition for most obese persons.73
An Unlikely Motivator for Weight Loss
In his recent writings about the counterproductive nature of stigma on health, Burris asks “Where is the evidence that inculcating a sense of spoiled identity is a good way to get people to adopt healthier behaviors?” 82(p475) Indeed, despite the shame and prejudice induced by weight stigma, there is a perception that stigmatizing obese individuals may instill motivation to engage in healthier eating and exercise behaviors. The idea that stigma may be a useful tool of social control to discourage unhealthy behaviors and improve the health of stigmatized individuals has been debated, with some theorizing that individuals will act to change their behaviors to avoid being out of step with social norms and the resulting stigmatization.83
However, several lines of evidence fail to demonstrate this relationship with obesity. First, if weight stigma promoted healthier lifestyle behaviors and weight loss, then the documentation of increased weight stigmatization over the past several decades84 should be accompanied by a reduction in obesity rates, rather than the alarming increase.85 A recent study examining a nationally representative sample of more than 2000 Americans found that as obesity rates have continued to climb, weight discrimination has also increased by 66% over the past 10 years, even after control for a range of variables including BMI.6 Not only are there more obese people, but there are more obese people reporting discrimination on the basis of their weight.
Second, a number of studies have consistently demonstrated that experiencing weight stigma increases the likelihood of engaging in unhealthy eating behaviors and lower levels of physical activity, both of which exacerbate obesity and weight gain. Among youths, several studies have demonstrated that overweight children who experience weight-based teasing are more likely to engage in binge-eating and unhealthy weight control behaviors compared with overweight peers who are not teased, even after control for variables such as BMI and socioeconomic status.86,87 Prospective studies demonstrate that weight-based teasing in youths predicts binge eating and extreme weight-control practices 5 years later, after control for variables including age, race, and socioeconomic status.88 Other research has consistently documented a positive association between weight-based victimization and eating disorder symptoms and bulimia.89–92 Weight-based victimization among overweight youths has been linked to lower levels of physical activity, negative attitudes about sports, and lower participation in physical activity among overweight students.93–95
Among overweight and obese adults, similar findings have emerged. In both clinical and nonclinical samples, adults who experience weight-based stigmatization engage in more frequent binge eating,96–99 are at increased risk for maladaptive eating patterns and eating disorder symptoms,90,100,101 and are more likely to have a diagnosis of binge eating disorder.99 Some research has found that psychological distress may mediate the association between stigma and binge eating, where experiences of stigma increase vulnerability to poor psychological functioning, which in turn increases risk of binge eating behaviors.97
Coping responses in reaction to weight stigma may also lead to unhealthy eating behaviors. In a study of more than 2400 overweight and obese women who belonged to a weight loss support organization, 79% reported coping with weight stigma on multiple occasions by eating more food, and 75% reported coping by refusing to diet.102 Similar research demonstrated that overweight and obese women who internalized negative weight stigma reported more frequent binge eating and refusal to diet compared with overweight or obese adults who did not internalize stigma.103 Research also shows that adults who experience weight stigma are more likely to avoid exercise, even after control for BMI and body dissatisfaction.104
Few studies have addressed the relationship between stigmatizing experiences and actual weight loss. In a study of more than 1000 overweight and obese women participating in a weight-loss support organization, it was found that stigma and internalization of weight-based stereotypes did not predict adoption of weight-loss strategies.103 Another study demonstrated that weight stigmatization was associated with greater caloric intake, higher program attrition, lower energy expenditure, less exercise, and less weight loss in a sample of treatment-seeking overweight and obese adults who participated in a behavioral weight loss program.105 In contrast, one study found that higher initial BMI, more stigmatizing experiences, lower body dissatisfaction, and greater fear of fat were associated with weight loss among adults participating in the Trevose Behavior Modification Program.106 However, the authors cautioned against interpretation and generalizability of these results, as the obesity treatment model in this study required participants to lose a prescribed amount of weight each month or face dismissal from the program. The atypical sample and concurrent assessment of variables raise uncertainty about these findings.
Rather than using stigma as an incentive to lose weight, it may be that supporting individuals with adaptive ways to cope with weight stigma can facilitate weight loss outcomes. A recent randomized treatment study found that, compared with wait-list controls, a brief 1-day intervention that taught patients acceptance-based strategies to cope with obesity-related stigma resulted in greater improvements in body mass, quality of life, perceived weight-related stigma, and psychological distress at 3-month follow-up.107 Thus, a model that can reduce the distress associated with stigma while simultaneously empowering weight control efforts provides a new treatment approach that seems worthwhile to pursue.
Although more work is needed to examine the impact of weight stigma on weight loss outcomes, the available evidence challenges the assumption that weight stigma is a useful tool for changing health behaviors. Instead, research shows that weight stigmatization reinforces unhealthy lifestyle behaviors that contribute to obesity, and is an unlikely method of inducing successful weight loss.
A Threat to Psychological and Physical Health
In addition to reinforcing unhealthy behaviors, weight stigma poses a significant threat to psychological and physical health. An accumulation of evidence demonstrates that weight stigma invokes psychological stress and emerging research suggests that this stress leads to poor physical health outcomes for obese individuals. Among both clinical and nonclinical samples of obese adults, weight stigmatization has been documented as a significant risk factor for depression,90,99,108–111 low self-esteem,96,112 and body dissatisfaction.113–115 These findings persist despite control for variables including age, gender, obesity onset, and BMI,108,110 indicating that, rather that being associated with excess body weight in itself, negative psychological outcomes are linked with experiences of weight-based stigmatization. In addition, a recent study examining a nationally representative sample of more than 9000 obese adults found that perceived weight discrimination was significantly associated with a current diagnosis of mood and anxiety disorders and mental health services use after control for sociodemographic characteristics and perceived stress.116
Meunnig117 argued that the high degree of psychological stress experienced by obese persons as a result of weight stigma contributes to the pathophysiology associated with obesity, and that many of the adverse biochemical changes that are associated with adiposity can also be caused by the psychological stress that accompanies the experience of frequent weight-based discrimination. Social disadvantages may specifically affect obesity through chronic stress, anxiety, and negative mood, which are associated with abdominal obesity, and may increase risk for obesity by activating particular physiological mechanisms that can increase appetite and blunt the satiety system, increasing fat retention and food intake.118
The belief that stigma-induced stress both exacerbates and triggers disease is frequently discussed in literature on the health effects of racial prejudice and discrimination. Research has demonstrated that African Americans who perceive racial discrimination or mistreatment have an increased risk of coronary events,119 breast cancer,120 coronary artery calcification,121 vascular reactivity, and elevated blood pressure,122–124 and higher substance use.125 These outcomes persist even when possible confounding variables—including sociodemographics, typical cardiovascular risk factors, and BMI—are controlled.121,124 Similar findings have emerged among Asian Americans and Chinese Americans, demonstrating that racial discrimination is associated with numerous chronic conditions such as heart disease, pain, and respiratory illness, even after related sociodemographic factors are controlled.126,127 These findings have led researchers to conclude that racism may act as a psychosocial stressor that elevates cardiovascular responses and in turn impairs health.122
Some evidence points directly to links between perceived racial discrimination and obesity-related outcomes, including weight gain and metabolic abnormalities.118,128 Hunte and Williams found that perceived chronic discrimination was related to excess body fat accumulation. Irish, Jewish, Polish, and Italian Whites who perceived chronic discrimination were 2 to 6 times more likely to have a high-risk waist circumference than White individuals of the same ethnic descent who did not perceive chronic discrimination.129 Other research has found that individuals who internalize stigma may be especially vulnerable to abdominal obesity and glucose intolerance.128
There are distinctions between prejudices based on race and weight (see Puhl and Latner for discussion4), but these findings have important implications for the impact of weight stigma on health outcomes for obese individuals. Current evidence suggests that weight-based stigma and discrimination increase vulnerability to psychological distress that may contribute to poor physical health. Given the increased risk of adverse outcomes already present with obesity, the additional negative impact of weight stigmatization on health is concerning. As Link and Phelan concluded:
[T]he stress associated with stigma can be particularly difficult for those with disease-associated stigma. Not only are they at risk to develop other stress-related illnesses, but the clinical course of the stigmatized illness itself may be worsened and other outcomes affected, such as the ability to work or lead a normal social life.130(p529)
Continued research in this area will help to clarify the relationship between weight stigma–induced stress and health.
A Threat to Quality Health Care
An accumulation of research has found that health care settings are a significant source of weight stigma,2 which undermines obese patients’ opportunity to receive effective medical care. Both self-report and experimental research demonstrate negative stereotypes and attitudes toward obese patients by a range of health care providers and fitness professionals, including views that obese patients are lazy, lacking in self-discipline, dishonest, unintelligent, annoying, and noncompliant with treatment.1,2 There is also research indicating that providers spend less time in appointments and provide less health education with obese patients compared with thinner patients.131,132 In response, obese individuals frequently report experiences of weight bias in health care.102,133,134 Obese patients also indicate that they feel disrespected by providers, perceive that they will not be taken seriously because of their weight, report that their weight is blamed for all of their medical problems, and are reluctant to address their weight concerns with providers.133–135 All of these findings point to substandard health care experiences for obese individuals.
Health care utilization is also compromised by weight stigma. A number of studies demonstrate that obese persons are less likely to undergo age-appropriate preventive cancer screenings.136–139 Lower rates of preventive health care exist even after control for factors typically associated with reduced health care use, such as less education, lower income, lack of health insurance, and greater illness burden.140 Recent research indicates that weight stigma may be a specific contributor to these findings.2 Amy et al. surveyed 498 overweight and obese women (with health insurance and high access to health care) about their perceived barriers to routine gynecological cancer screenings.135 For women at the highest levels of obesity, 68% reported that they delayed seeking health care because of their weight, and 83% reported that their weight was a barrier to getting appropriate health care. When asked about specific reasons for delay of care, women reported disrespectful treatment and negative attitudes from providers, embarrassment about being weighed, receiving unsolicited advice to lose weight, and also reported that gowns, examination tables, and other medical equipment were too small to be functional for their body size. The percentage of women reporting these barriers increased with BMI.135
As obese individuals are at a high risk for weight-related comorbidities, quality health care is essential. Acknowledging the detrimental effects of weight stigma in health care is essential for a better understanding of the cumulative impacts of weight stigma on public health.
Impaired Obesity Intervention Efforts
The stigmatized nature of a disease greatly influences public health efforts to prevent or treat that disease, which is widely evidenced by the social history of HIV/AIDS and other stigmatized illnesses.24 Although the social constructions of obesity are far less recognized, they play a central role in defining policy responses to the epidemic. Governments historically fail to respond appropriately to diseases that primarily afflict socially undesirable groups.15 Obesity is dismissed as a personal failing; thus, it is not addressed “on par” with nonstigmatized medical conditions. Rather than working on a comprehensive plan to address the obesity epidemic, policymakers have mainly focused efforts on education of those afflicted.15 Pomeranz writes:
Discrimination manifests in illness and disease that society and governments do not adequately address due to the very discrimination causing the harm. On the contrary, society and the government tend to blame the victims and enact and interpret legislation based on the theory that the people are not taking appropriate responsibility for their own health. Obese individuals internally suffer from weight bias but also suffer because society blames them for their illness and thus relinquishes responsibility of addressing the underlying causes of their obesity.15(pS93)
The emphasis on nutrition education in the US approach to obesity reflects assumptions that rates of obesity have risen because Americans lack sufficient knowledge of the personal behaviors that lead to weight gain. For example, the US Department of Health and Human Services launched its “Small Steps” campaign in 2004, funded at $1.5 million annually, with the primary objective to increase awareness among “unhealthy” Americans.141 The campaign consists of a series of radio and television public service messages that “use humor to inspire overweight adults to incorporate ‘Small Steps’ into their hectic lives.” The campaign's Web site also features a “Health Tip of the Day,” such as Small Step #92: “Walk instead of sitting around.” Critics have complained that the Small Steps campaign is ineffective and sidesteps the real causes of obesity.142
The stigmatization of obesity is also apparent when federal institutions’ actions and policies regarding obesity are compared with those of other diseases.143 For example, the National Institutes of Health projected 2009 budgets for cancer, HIV/AIDS, and digestive diseases are $5.6 billion, $2.9 billion, and $1.2 billion, respectively. At the same time, the budget for obesity, which poses numerous health risks and affects significantly more Americans, pales at $658 million.144 Downey notes that, historically, government responses to public health challenges (such as tuberculosis, influenza, polio, smoking, and HIV/AIDS) have included large-scale coordinated efforts that contain strategies to combat stigma and discrimination. The federal government's response to obesity, however, has failed to meet this historical standard for addressing diseases that threaten the health and lives of a major proportion of Americans across every age, gender, racial, and socioeconomic group.143
It is also significant to note that federal and state legislative initiatives related to obesity have largely avoided addressing the societal and environmental causes of the disease. Governments have spent significant time considering legislation to protect the food and restaurant industry from potential civil injury claims compared with time spent developing obesity prevention policies.143 In arguing in favor of the “Personal Responsibility in Food Consumption Act,” one Congressman stated, “This bill is about self-responsibility. If you eat too much, you get fat. It is your fault. Don't try to blame somebody else.”15,145 In 2008, a Mississippi State House Bill was proposed to prohibit restaurants from serving food to any person who is obese.15 Such a deliberate attempt at overt discrimination underscores the prevalence of weight stigma, even among key decision makers.
Optimistically, recent efforts have attempted to address the environmental and structural contributors to obesity (e.g., through policies aimed at improving school food, enacting menu labeling legislation, taxing sodas, and improving healthy food access). However, larger-scale efforts are needed. To address obesity commensurate to its impact, a coordinated and well-funded response is critical.
CRITICAL IMPLICATIONS FOR PUBLIC HEALTH
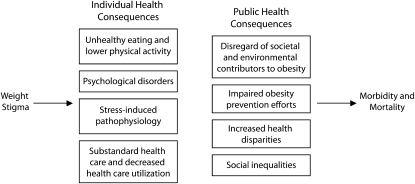
With the current body of evidence, it is apparent that, as with other stigmas, weight stigma has negative implications for public health. Weight stigma threatens the psychological and physical health of obese individuals, impedes the implementation of effective efforts to prevent obesity, and exacerbates health disparities. Figure 1 summarizes individual and public health consequences of weight stigma that may ultimately worsen life outcomes for obese persons.
FIGURE 1.
Individual and public health consequences of weight stigma.
By limiting the national response for obesity to education about individual choices regarding nutrition and physical activity, important societal and environmental causes of obesity are overlooked, the economic and social disparities that contribute to obesity are ignored, and weight stigma and discrimination are equally disregarded. Indeed, public health policy can either protect those afflicted with a disease from discrimination, or can promote unfair treatment and disparities. Unfortunately, the US government has not addressed weight stigma and discrimination in formal legislation, leaving millions of obese people to suffer unfair treatment because of their weight. These social consequences may intensify the health disparities already faced by obese Americans. Because obesity is especially prevalent among poor or minority groups who live in disadvantaged areas,146 obese individuals often already belong to marginalized groups and experience multiple stigmatized statuses. Consequently, the stigmatization of obese individuals is inextricably linked to social inequalities.
For the public health community to address the widespread health and social disparities faced by obese people, we must move past the victim-blaming approach and instead advocate a comprehensive obesity prevention strategy that includes efforts to reduce weight-based stigma and discrimination. We offer 3 recommendations to achieve this goal.
First, it is essential for weight stigma to be addressed in obesity interventions, and for anti-stigma messages to be incorporated into obesity prevention campaigns. For example, interventions should focus on health as both the primary motivator and desired outcome for behavior change, rather than messages that emphasize achieving an ideal weight, which may perpetuate obesity stereotypes and chastise obese individuals. Unhealthy eating behaviors, such as fast food and soda consumption, can be discouraged for all people, regardless of their body size. It may be especially important to incorporate anti-stigma messages in interventions for youths, because of the vulnerability of obese children to the negative emotional and physical health consequences of weight-based victimization.4 A 2005 report issued by the Institute of Medicine acknowledged the importance of considering weight-based stigmatization in obesity interventions for youths and recommended shifting the focus of prevention efforts to emphasize behaviors that promote health rather than appearance.147 Similarly, the Society for Nutrition Education also recommends that school-based obesity prevention programs include promotion of weight tolerance and school policies prohibit weight-based teasing and victimization.148 MacLean et al. asserted a range of stigma-specific recommendations for public health interventions for obesity, including evaluation of the social impact of existing interventions on stigma, providing stigma-reduction training for health care professionals, screening public health communication messages for stigmatizing content, seeking perspectives from obese persons in efforts to identify solutions to stigmatizing programs, and ensuring consistent implementation of nonstigmatizing messages.25
Second, obesity prevention efforts need to expand beyond educational campaigns focused on individual behaviors toward larger-scale, coordinated policies that initiate social changes to help reverse the societal and environmental conditions that create obesity in the first place. Adler and Stewart proposed a “behavioral justice” approach to address obesity, which highlights the need to provide sufficient resources in the environment that enable individuals to engage in health-promoting behaviors.26 They posited that individuals should only be held responsible for engaging in healthy behaviors if they have full access to conditions that enable those behaviors. That is, unless people have adequate resources (e.g., access to affordable, healthy foods) to resist the obesogenic environment, it is too difficult (and unjust) to expect individual actions to be successful. Thus, although this approach does not ignore personal responsibility, the emphasis is shifted from personal blame to an issue of social justice. Efforts to create environmental changes that support responsible behaviors will serve to improve health and reduce health disparities for all Americans, regardless of their weight. Acknowledging the complex etiology of obesity will also help reduce weight stigma and its negative consequences. As more local and national resources are allocated toward obesity prevention, it is important to ensure that resources are used productively and that weight stigma does not undermine new efforts.
Third, efforts to improve the health of obese individuals will be facilitated by legislation to prohibit weight-based discrimination. Currently, no federal legislation exists to protect obese individuals from discrimination on the basis of weight. Michigan is the only state that prohibits employment discrimination on the basis of weight, and the District of Columbia and the California cities of San Francisco and Santa Cruz are the only other areas to include body size in human rights ordinances.2 Thus, as weight discrimination increases, overweight and obese individuals have no means to seek legal redress for wrongful discrimination. This lack of protection for obese individuals allows discrimination in employment, education, and health care to persist, contributing to health disparities, morbidity, and mortality. Meaningful legal remedies are clearly needed to protect against weight discrimination, both at a state and federal level. The accumulation of science documenting the negative consequences of weight stigma and discrimination provides ample justification for legal action. Public health professionals can play an important role in supporting necessary protections for obese individuals.
The stigmatization of obesity is pervasive, damaging, and threatens core public health values. Rates of overweight and obesity are as high as 76% for some groups in the United States.149 By ignoring weight stigma, the public health community ignores substantial suffering of many Americans. To effectively address the obesity epidemic and improve public health, it is essential to challenge common societal assumptions that perpetuate weight stigma, and prioritize discussions of weight stigma in the national discourse on obesity.
Acknowledgments
This research was funded by the Rudd Center for Food Policy and Obesity at Yale University.
Human Participant Protection
No protocol approval was needed for this research.
References
- 1.Puhl R, Brownell KD. Bias, discrimination, and obesity. Obes Res 2001;9(12):788–805 [DOI] [PubMed] [Google Scholar]
- 2.Puhl RM, Heuer CA. Weight bias: a review and update. Obesity (Silver Spring) 2009;17(5):941–964 [DOI] [PubMed] [Google Scholar]
- 3.Brownell KD, Puhl RM, Schwartz MB, Rudd L, Weight Bias: Nature, Consequences, and Remedies New York, NY: The Guilford Press; 2005 [Google Scholar]
- 4.Puhl RM, Latner JD. Stigma, obesity, and the health of the nation's children. Psychol Bull 2007;133(4):557–580 [DOI] [PubMed] [Google Scholar]
- 5.Cramer P, Steinwert T. Thin is good, fat is bad: how early does it begin? J Appl Dev Psychol 1998;19:429–451 [Google Scholar]
- 6.Andreyeva T, Puhl RM, Brownell KD. Changes in perceived weight discrimination among Americans: 1995–1996 through 2004–2006. Obesity (Silver Spring) 2008;16(5):1129–1134 [DOI] [PubMed] [Google Scholar]
- 7.Puhl RM, Andreyeva T, Brownell KD. Perceptions of weight discrimination: prevalence and comparison to race and gender discrimination in America. Int J Obes (Lond) 2008;32(6):992–1000 [DOI] [PubMed] [Google Scholar]
- 8.Richardson SA, Goodman N, Hastorf AH, Dornbusch SM. Cultural uniformity in reaction to physical disabilities. Am Sociol Rev 1961;26:241–247 [Google Scholar]
- 9.DeJong W. The stigma of obesity: the consequences of naive assumptions concerning the causes of physical deviance. J Health Soc Behav 1980;21(1):75–87 [PubMed] [Google Scholar]
- 10.Puhl R, Brownell KD. Ways of coping with obesity stigma: conceptual review and analysis. Eat Behav 2003;4(1):53–78 [DOI] [PubMed] [Google Scholar]
- 11.Crister G. Fat Land: How Americans Became the Fattest People in the World New York, NY: Houghton Mifflin; 2004 [Google Scholar]
- 12.Averett S, Korenman S. Black-white differences in social and economic consequences of obesity. Int J Obes Relat Metab Disord 1999;23(2):166–173 [DOI] [PubMed] [Google Scholar]
- 13.Hebl MR, Heatherton TF. The stigma of obesity in women: the difference is black and white. Pers Soc Psychol Bull 1998;24(4):417–426 [Google Scholar]
- 14.Kraut AM. Silent Travelers: Germs, Genes, and the “Immigrant Menace.” Baltimore, MD: The Johns Hopkins University Press; 1994 [Google Scholar]
- 15.Pomeranz JL. A historical analysis of public health, the law, and stigmatized social groups: the need for both obesity and weight bias legislation. Obesity (Silver Spring) 2008;16:S93–S102 [DOI] [PubMed] [Google Scholar]
- 16.Luoma JB, Twohig MP, Waltz T, et al. An investigation of stigma in individuals receiving treatment for substance abuse. Addict Behav 2007;32(7):1331–1346 [DOI] [PubMed] [Google Scholar]
- 17.Fortenberry JD, McFarlane M, Bleakley A, et al. Relationships of stigma and shame to gonorrhea and HIV screening. Am J Public Health 2002;92(3):378–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Herek GM, Capitanio JP, Widaman KF. Stigma, social risk, and health policy: public attitudes toward HIV surveillance policies and the social construction of illness. Health Psychol 2003;22(5):533–540 [DOI] [PubMed] [Google Scholar]
- 19.Mann J, Tarantola D. Responding to HIV/AIDS: a historical perspective. Health Hum Rights 1998;2(4):5–8 [Google Scholar]
- 20.Bayer R. Public health policy and the AIDS epidemic: an end to HIV exceptionalism? N Engl J Med 1991;324(21):1500–1504 [DOI] [PubMed] [Google Scholar]
- 21.United Nations General Assembly. Declaration of Commitment on HIV/AIDS. Twenty-sixth special session; August 2, 2001. Available at: http://www.un.org/ga/aids/docs/aress262.pdf. Accessed November 30, 2009.
- 22.Parker R, Aggleton P. HIV and AIDS-related stigma and discrimination: a conceptual framework and implications for action. Soc Sci Med 2003;57(1):13–24 [DOI] [PubMed] [Google Scholar]
- 23.Reducing HIV Stigma and Discrimination: A Critical Part of National AIDS Programmes Geneva, Switzerland: Joint United Nations Programme on HIV/AIDS; 2007 [Google Scholar]
- 24.Bayer R. Stigma and the ethics of public health: not can we but should we. Soc Sci Med 2008;67(3):463–472 [DOI] [PubMed] [Google Scholar]
- 25.MacLean L, Edwards N, Garrad M, Sims-Jones N, Clinton K, Ashley L. Obesity, stigma, and public health planning. Health Promot Int 2009;24(1):88–93 [DOI] [PubMed] [Google Scholar]
- 26.Adler NE, Stewart J. Reducing obesity: motivating action while not blaming the victim. Milbank Q 2009;87(1):49–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cahnman WJ. The stigma of obesity. Sociol Q 1968;9:283–299 [Google Scholar]
- 28.Weiner B, Perry RP, Magnusson J. An attributional analysis of reactions to stigmas. J Pers Soc Psychol 1988;55(5):738–748 [DOI] [PubMed] [Google Scholar]
- 29.Kim S-H, Willis LA. Talking about obesity: news framing of who is responsible for causing and fixing the problem. J Health Commun 2007;12(4):359–376 [DOI] [PubMed] [Google Scholar]
- 30.Lawrence RG. Framing obesity: the evolution of news discourse on a public health issue. Int J Press Politics 2004;9(3):56–75 [Google Scholar]
- 31.Rich E, Evans J. ‘Fat ethics’––the obesity discourse and body politics. Soc Theory Health 2005;3(4):341–358 [Google Scholar]
- 32.Crandall CS, Biernat M. The ideology of anti-fat attitudes. J Appl Soc Psychol 1990;20:227–243 [Google Scholar]
- 33.Balko R. Are you responsible for your own weight? Absolutely, government has no business interfering with what you eat. Time June 7, 2004. Available at: http://www.time.com/time/subscriber/covers/1101040607/article/are_you_responsible_for01a.html. Accessed November 30, 2009
- 34.DeJong W. Obesity as a characterological stigma: the issue of responsibility and judgments of task performance. Psychol Rep 1993;73(3 Pt 1):963–970 [DOI] [PubMed] [Google Scholar]
- 35.Musher-Eizenman DR, Holub SC, Miller AB, Goldstein SE, Edwards-Leeper L. Body size stigmatization in preschool children: the role of control attributions. J Pediatr Psychol 2004;29(8):613–620 [DOI] [PubMed] [Google Scholar]
- 36.Bell SK, Morgan SN. Children's attitudes and behavioral intentions toward a peer presented as obese: does a medical explanation for the obesity make a difference? J Pediatr Psychol 2000;25(3):137–145 [DOI] [PubMed] [Google Scholar]
- 37.Crandall CS. Prejudice against fat people: ideology and self-interest. J Pers Soc Psychol 1994;66(5):882–894 [DOI] [PubMed] [Google Scholar]
- 38.Crandall CS, Moriarty D. Physical illness stigma and social rejection. Br J Soc Psychol 1995;34(Pt 1):67–83 [DOI] [PubMed] [Google Scholar]
- 39.Puhl RM, Schwartz MB, Brownell KD. Impact of perceived consensus on stereotypes about obese people: a new approach for reducing bias. Health Psychol 2005;24(5):517–525 [DOI] [PubMed] [Google Scholar]
- 40.Bonfiglioli CM, Smith BJ, King LA, Chapman SF, Holding SJ. Choice and voice: obesity debates in television news. Med J Aust 2007;187(8):442–445 [DOI] [PubMed] [Google Scholar]
- 41.Boero N. All the news that's fat to print: the American "obesity epidemic" and the media. Qual Sociol 2007;30:41–60 [Google Scholar]
- 42.Himes SM, Thompson JK. Fat stigmatization in television shows and movies: a content analysis. Obesity (Silver Spring) 2007;15(3):712–718 [DOI] [PubMed] [Google Scholar]
- 43.Greenberg BS, Eastin M, Hofshire L, Lachlan K, Brownell KD. The portrayal of overweight and obese persons in commercial television. Am J Public Health 2003;93(8):1342–1348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Geier AB, Schwartz MB, Brownell KD. "Before and after" diet advertisements escalate weight stigma. Eat Weight Disord 2003;8(4):282–288 [DOI] [PubMed] [Google Scholar]
- 45.Puhl RM, Schwartz MB. If you are good you can have a cookie: how memories of childhood food rules link to adult eating behaviors. Eat Behav 2003;4(3):283–293 [DOI] [PubMed] [Google Scholar]
- 46.Crandall CS, Schiffhauer KL. Anti-fat prejudice: beliefs, values, and American culture. Obes Res 1998;6(6):458–460 [DOI] [PubMed] [Google Scholar]
- 47.Crandall CS, D'Anello S, Sakalli N, Lazarus E, Nejtardt GW, Feather NT. An attribution-value model of prejudice: anti-fat attitudes in six nations. Pers Soc Psychol Bull 2001;27(1):30–37 [Google Scholar]
- 48.Perusse L, Bouchard C. Gene-diet interactions in obesity. Am J Clin Nutr 2000;72(5 suppl):1285S–1290S [DOI] [PubMed] [Google Scholar]
- 49.Frayling TM, Timpson NJ, Weedon MN, Zeggini E, Freathy RM, Lindgren CM. A common variant in the FTO gene is associated with body mass index and predisposes to childhood and adult obesity. Science 2007;316(5826):889–894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lee YS. The role of genes in the current obesity epidemic. Ann Acad Med Singapore 2009;38(1):45–47 [PubMed] [Google Scholar]
- 51.Finkelstein EA, Ruhm CJ, Kosa KM. Economic causes and consequences of obesity. Annu Rev Public Health 2005;26:239–257 [DOI] [PubMed] [Google Scholar]
- 52.Dannenberg AL, Jackson RJ, Frumkin H, et al. The impact of community design and land-use choices on public health: a scientific research agenda. Am J Public Health 2003;93(9):1500–1508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Booth KM, Pinkston MM, Poston WS. Obesity and the built environment. J Am Diet Assoc 2005;105(5 suppl 1):S110–S117 [DOI] [PubMed] [Google Scholar]
- 54.Andreyeva T, Blumenthal DM, Schwartz MB, Long MW, Brownell KD. Availability and prices of foods across stores and neighborhoods: the case of New Haven, Connecticut. Health Aff (Millwood) 2008;27(5):1381–1388 [DOI] [PubMed] [Google Scholar]
- 55.Sallis JF, Saelens BE, Frank LD, et al. Neighborhood built environment and income: examining multiple health outcomes. Soc Sci Med 2009;68(7):1285–1293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Li F, Harmer P, Cardinal BJ, et al. Built environment and 1-year change in weight and waist circumference in middle-aged older adults: Portland Neighborhood Environment and Health Study. Am J Epidemiol 2009;169(4):401–408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nielsen SJ, Popkin BM. Patterns and trends in food portion sizes, 1977–1998. JAMA 2003;289(4):450–453 [DOI] [PubMed] [Google Scholar]
- 58.Brownell KD, Horgen KB. Food Fight: The Inside Story of the Food Industry, America's Obesity Crisis, and What We Can Do About It New York, NY: McGraw-Hill; 2004 [Google Scholar]
- 59.Brownell KD, Warner KE. The perils of ignoring history: Big Tobacco played dirty and millions died. How similar is Big Food? Milbank Q 2009;87(1):259–294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Harris JL, Pomeranz JL, Lobstein T, Brownell KD. A crisis in the marketplace: how food marketing contributes to childhood obesity and what can be done. Ann Rev Public Health 2009;30:211–225 [DOI] [PubMed] [Google Scholar]
- 61.Schwartz MB, Vartanian LR, Wharton CM, Brownell KD. Examining the nutritional quality of breakfast cereals marketed to children. J Am Diet Assoc 2008;108(4):702–705 [DOI] [PubMed] [Google Scholar]
- 62.Cohen DA. Obesity and the built environment: changes in environmental cues cause energy imbalances. Int J Obes (Lond) 2008;32(suppl 7):S137–S142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Schwartz MB, Brownell KD. Actions necessary to prevent childhood obesity: creating the climate for change. J Law Med Ethics 2007;35(1):78–89 [DOI] [PubMed] [Google Scholar]
- 64.Sallis JF, Glanz K. Physical activity and food environments: solutions to the obesity epidemic. Milbank Q 2009;87(1):123–154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wadden TA, Brownell KD, Foster GD. Obesity: responding to the global epidemic. J Consult Clin Psychol 2002;70(3):510–525 [DOI] [PubMed] [Google Scholar]
- 66.Franz MJ, VanWormer JJ, Crain AL, et al. Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J Am Diet Assoc 2007;107(10):1755–1767 [DOI] [PubMed] [Google Scholar]
- 67.Dansinger ML, Tatsioni A, Wong JB, Chung M, Balk EM. Meta-analysis: the effect of dietary counseling for weight loss. Ann Intern Med 2007;147(1):41–50 [DOI] [PubMed] [Google Scholar]
- 68.Wadden TA, Butryn ML, Wilson C. Lifestyle modification for the management of obesity. Gastroenterology 2007;132(6):2226–2238 [DOI] [PubMed] [Google Scholar]
- 69.Powell LH, Calvin JE, 3rd, Calvin JE., Jr Effective obesity treatments. Am Psychol 2007;62(3):234–246 [DOI] [PubMed] [Google Scholar]
- 70.Mann T, Tomiyama AJ, Westling E, Lew A-M, Samuels B, Chatman J. Medicare's search for effective obesity treatments. Am Psychol 2007;62(3):220–233 [DOI] [PubMed] [Google Scholar]
- 71.Tsai AG, Wadden TA. Systematic review: an evaluation of major commercial weight loss programs in the United States. Ann Intern Med 2005;142(1):56–66 [DOI] [PubMed] [Google Scholar]
- 72.Waseem T, Mogensen KM, Lautz DB, Robinson MK. Pathophysiology of obesity. Obes Surg 2007;17(10):1389–1398 [DOI] [PubMed] [Google Scholar]
- 73.Orzano AJ, Scott JG. Diagnosis and treatment of obesity in adults: an applied evidence-based review. J Am Board Fam Pract 2004;17(5):359–369 [DOI] [PubMed] [Google Scholar]
- 74.Anderson JW, Konz EC, Frederich RC, Wood CL. Long-term weight-loss maintenance: a meta-analysis of U.S. studies. Am J Clin Nutr 2001;74(5):579–584 [DOI] [PubMed] [Google Scholar]
- 75.Wadden TA, Butryn ML, Byrne KJ. Efficacy of lifestyle modification for long-term weight control. Obes Res 2004;12(suppl):151S–162S [DOI] [PubMed] [Google Scholar]
- 76.Wadden TA, Sternberg JA, Letizia KA, Stunkard AJ, Foster GD. Treatment of obesity by very-low-calorie diet, behavior therapy, and their combination: a five-year perspective. Int J Obes 1989;13(suppl 2):39–46 [PubMed] [Google Scholar]
- 77.Svetkey LP, Stevens VJ, Brantley PJ, et al. Comparison of strategies for sustaining weight loss: the weight loss maintenance randomized controlled trial. JAMA 2008;299(10):1139–1148 [DOI] [PubMed] [Google Scholar]
- 78.Wing RR, Phelan S. Long-term weight loss maintenance. Am J Clin Nutr 2005;82(1 suppl):222S–225S [DOI] [PubMed] [Google Scholar]
- 79.Wildman RP, Muntner P, Reynolds K, et al. The obese without cardiometabolic risk factor clustering and the normal weight with cardiometabolic risk factor clustering: prevalence and correlates of 2 phenotypes among the US population (NHANES 1999-2004). Arch Intern Med 2008;168(15):1617–1624 [DOI] [PubMed] [Google Scholar]
- 80.Karelis AD, St-Pierre DH, Conus F, Rabasa-Lhoret R, Poelhman ET. Metabolic and body composition factors in subgroups of obesity: what do we know? J Clin Endocrinol Metab 2004;89(6):2569–2575 [DOI] [PubMed] [Google Scholar]
- 81.Ruderman N, Chisholm D, Pi-Sunyer X, Schneider S. The metabolically obese, normal weight individual revisited. Diabetes 1998;47(5):699–713 [DOI] [PubMed] [Google Scholar]
- 82.Burris S. Stigma ethics, and policy: a commentary on Bayer's "Stigma and the ethics of public health: not can we but should we." Soc Sci Med 2008;67(3):473–475, discussion 476–477 [DOI] [PubMed] [Google Scholar]
- 83.Stuber J, Meyer I, Link B. Stigma, prejudice, discrimination and health. Soc Sci Med 2008;67(3):351–357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Latner JD, Stunkard AJ. Getting worse: the stigmatization of obese children. Obes Res 2003;11(3):452–456 [DOI] [PubMed] [Google Scholar]
- 85.National Center for Health Statistics. Prevalence of overweight and obesity among adults: United States, 2003–2004. 2006. Available at: http://www.cdc.gov/nchs/fastats/overwt.htm. Accessed November 30, 2009.
- 86.Neumark-Sztainer D, Falkner N, Story M, Perry C, Hannan PJ, Mulert S. Weight-teasing among adolescents: correlations with weight status and disordered eating behaviors. Int J Obes 2002;26(1):123–131 [DOI] [PubMed] [Google Scholar]
- 87.Libbey HP, Story MT, Neumark-Sztainer DR, Boutelle KN. Teasing, disordered eating behaviors, and psychological morbidities among overweight adolescents. Obesity (Silver Spring) 2008;16(suppl 2):S24–S29 [DOI] [PubMed] [Google Scholar]
- 88.Haines J, Neumark-Sztainer D, Eisenberg ME, Hannan PJ. Weight teasing and disordered eating behaviors in adolescents: longitudinal findings from Project EAT (Eating Among Teens). Pediatrics 2006;117(2):209e–215e [DOI] [PubMed] [Google Scholar]
- 89.Kaltiala-Heino R, Rissanen A, Rimpela M, Rantanen P. Bulimia and bulimic behavior in middle adolescence: more common than thought? Acta Psychiatr Scand 1999;100(1):33–39 [DOI] [PubMed] [Google Scholar]
- 90.Jackson TD, Grilo CM, Masheb RM. Teasing history, onset of obesity, current eating disorder psychopathology, body dissatisfaction, and psychological functioning in binge eating disorder. Obes Res 2000;8(6):451–458 [DOI] [PubMed] [Google Scholar]
- 91.Striegel-Moore RH, Dohm FA, Pike KM, Wilfley DE, Fairburn CG. Abuse, bullying, and discrimination as risk factors for binge eating disorder. Am J Psychiatry 2002;159(11):1902–1907 [DOI] [PubMed] [Google Scholar]
- 92.Fairburn CG, Welch SL, Doll HA, Davies BA, O'Connor ME. Risk factors for bulimia nervosa. A community-based case-control study. Arch Gen Psychiatry 1997;54(6):509–517 [DOI] [PubMed] [Google Scholar]
- 93.Storch EA, Milsom VA, DeBraganza N, Lewin AB, Geffken GR, Silverstein JH. Peer victimization, psychosocial adjustment, and physical activity in overweight and at-risk-for-overweight youth. J Pediatr Psychol 2007;32(1):80–89 [DOI] [PubMed] [Google Scholar]
- 94.Faith MS, Leone MA, Ayers TS, Heo M, Pietrobelli A. Weight criticism during physical activity, coping skills, and reported physical activity in children. Pediatrics 2002;110(2 pt 1):e23. [DOI] [PubMed] [Google Scholar]
- 95.Bauer KW, Yang YW, Austin SB. “How can we stay healthy when you're throwing all this in front of us?” Findings from focus groups and interviews in middle schools on environmental influences on nutrition and physical activity. Health Educ Behav 2004;31(1):34–36 [DOI] [PubMed] [Google Scholar]
- 96.Annis NM, Cash TF, Hrabosky JI. Body image and psychosocial differences among stable average weight, currently overweight, and formerly overweight women: the role of stigmatizing experiences. Body Image 2004;1(2):155–167 [DOI] [PubMed] [Google Scholar]
- 97.Ashmore JA, Friedman KE, Reichmann SK, Musante GJ. Weight-based stigmatization, psychological distress, and binge eating behavior among obese treatment-seeking adults. Eat Behav 2008;9(2):203–209 [DOI] [PubMed] [Google Scholar]
- 98.Womble LG, Williamson DA, Martin CK, et al. Psychosocial variables associated with binge eating in obese males and females. Int J Eat Disord 2001;30(2):217–221 [DOI] [PubMed] [Google Scholar]
- 99.Friedman KE, Ashmore JA, Applegate KL. Recent experiences of weight-based stigmatization in a weight loss surgery population: psychological and behavioral correlates. Obesity (Silver Spring) 2008;16(suppl 2):S69–S74 [DOI] [PubMed] [Google Scholar]
- 100.Benas JS, Gibb BE. Weight-related teasing, dysfunctional cognitions, and symptoms of depression and eating disturbances. Cognit Ther Res 2008;32(2):143–160 [Google Scholar]
- 101.Mora-Giral M, Raich-Escursell RM, Segues CV, Torras-Claraso J, Huon G. Bulimia symptoms and risk factors in university students. Eat Weight Disord 2004;9(3):163–169 [DOI] [PubMed] [Google Scholar]
- 102.Puhl RM, Brownell KD. Confronting and coping with weight stigma: an investigation of overweight and obese adults. Obesity (Silver Spring) 2006;14(10):1802–1815 [DOI] [PubMed] [Google Scholar]
- 103.Puhl RM, Moss-Racusin CA, Schwartz MB. Internalization of weight bias: implications for binge eating and emotional well-being. Obesity (Silver Spring) 2007;15(1):19–23 [DOI] [PubMed] [Google Scholar]
- 104.Vartanian LR, Shaprow JG. Effects of weight stigma on exercise motivation and behavior: a preliminary investigation among college-aged females. J Health Psychol 2008;13(1):131–138 [DOI] [PubMed] [Google Scholar]
- 105.Carels RA, Young KM, Wott CB, et al. Weight bias and weight loss treatment outcomes in treatment-seeking adults. Ann Behav Med 2009;37(3):350–355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Latner JD, Wilson GT, Jackson ML, Stunkard AJ. Greater history of weight-related stigmatizing experience is associated with greater weight loss in obesity treatment. J Health Psychol 2009;24(2):190–199 [DOI] [PubMed] [Google Scholar]
- 107.Lillis J, Hayes SC, Bunting K, Masuda A. Teaching acceptance and mindfulness to improve the lives of the obese: a preliminary test of a theoretical model. Ann Behav Med 2009;37(1):58–69 [DOI] [PubMed] [Google Scholar]
- 108.Friedman KE, Reichmann SK, Costanzo PR, Zelli A, Ashmore JA, Musante GJ. Weight stigmatization and ideological beliefs: relation to psychological functioning in obese adults. Obes Res 2005;13(5):907–916 [DOI] [PubMed] [Google Scholar]
- 109.Chen EY. Depressed mood in class III obesity predicted by weight-related stigma. Obes Surg 2007;17(5):669–671 [DOI] [PubMed] [Google Scholar]
- 110.Rosenberger PH, Henderson KE, Bell RL, Grilo CM. Associations of weight-based teasing history and current eating disorder features and psychological functioning in bariatric surgery patients. Obes Surg 2007;17(4):470–477 [DOI] [PubMed] [Google Scholar]
- 111.Myers A, Rosen JC. Obesity stigmatization and coping: relation to mental health symptoms, body image, and self-esteem. Int J Obes Relat Metab Disord 1999;23(3):221–230 [DOI] [PubMed] [Google Scholar]
- 112.Carr D, Friedman MA. Is obesity stigmatizing? Body weight, perceived discrimination, and psychological well-being in the United States. J Health Soc Behav 2005;46(3):244–259 [DOI] [PubMed] [Google Scholar]
- 113.Rosenberger PH, Henderson KE, Grilo CM. Correlates of body image dissatisfaction in extremely obese female bariatric surgery candidates. Obes Surg 2006;16(10):1331–1336 [DOI] [PubMed] [Google Scholar]
- 114.Matz PE, Foster GD, Faith MS, Wadden TA. Correlates of body image dissatisfaction among overweight women seeking weight loss. J Consult Clin Psychol 2002;70(4):1040–1044 [PubMed] [Google Scholar]
- 115.Wardle J, Waller J, Fox E. Age of onset and body dissatisfaction in obesity. Addict Behav 2002;27(4):561–573 [DOI] [PubMed] [Google Scholar]
- 116.Hatzenbuehler ML, Keyes KM, Hasin DS. Associations between perceived weight discrimination and the prevalence of psychiatric disorders in the general population. Obesity 2009;17(11)2033–2039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Muennig P. The body politic: the relationship between stigma and obesity-associated disease. BMC Public Health 2008;8:128–138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Gee GC, Ro A, Gavin A, Takeuchi DT. Disentangling the effects of racial and weight discrimination on body mass index and obesity among Asian Americans. Am J Public Health 2008;98(3):493–500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.De Vogli R, Ferrie JE, Chandola T, Kivimaki M, Marmot MG. Unfairness and health: evidence from the Whitehall II study. J Epidemiol Community Health 2007;61(6):513–518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Taylor TR, Williams CD, Makambi KH, et al. Racial discrimination and breast cancer incidence in U.S. black women. Am J Epidemiol 2007;166(1):46–54 [DOI] [PubMed] [Google Scholar]
- 121.Lewis TT, Everson-Rose SA, Powell LH, et al. Chronic exposure to everyday discrimination and coronary artery calcification in African-American women: the SWAN heart study. Psychosom Med 2006;68(3):362–368 [DOI] [PubMed] [Google Scholar]
- 122.Merritt MM, Bennett GG, Williams RB, Edwards CL, Sollers JJ. Perceived racism and cardiovascular reactivity and recovery to personally relevant stress. Health Psychol 2006;25(3):364–369 [DOI] [PubMed] [Google Scholar]
- 123.Din-Dzietham R, Nembhard WN, Collins R, Davis SK. Perceived stress following race-based discrimination at work is associated with hypertension in African Americans. The metro Atlanta heart disease study, 1999-2001. Soc Sci Med 2004;58(3):449–461 [DOI] [PubMed] [Google Scholar]
- 124.Clark R. Peceived racism and vascular reactivity in black college women: moderating effects of seeking social support. Health Psychol 2006;25(1):20–25 [DOI] [PubMed] [Google Scholar]
- 125.Borrell LN, Jacobs DR, Williams DR, Pletcher MJ, Houston TK, Kiefe CI. Self-reported racial discrimination and substance use in the coronary artery risk development in adults study. Am J Epidemiol 2007;166(9):1068–1079 [DOI] [PubMed] [Google Scholar]
- 126.Gee GC. A multilevel analysis of the relationship between institutional and individual racial discrimination and health status. Am J Public Health 2002;92(4):615–623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Gee GC, Spencer MS, Chen J, Takeuchi DT. A nationwide study of discrimination and chronic health conditions among Asian Americans. Am J Public Health 2007;97(7):1275–1282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Tull ES, Sheu YT, Butler C, Cornelious K. Relationships between perceived stress, coping behavior and cortisol secretion in women with high and low levels of internalized racism. J Natl Med Assoc 2005;97(2):206–212 [PMC free article] [PubMed] [Google Scholar]
- 129.Hunte HE, Williams DR. The association between perceived discrimination and obesity in a population-based multiracial and multiethnic adult sample. Am J Public Health 2009;99(7):1285–1292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Link BG, Phelan JC. Stigma and its public health implications. Lancet 2006;367(9509):528–529 [DOI] [PubMed] [Google Scholar]
- 131.Hebl MR, Xu J. Weighing the care: physicians’ reactions to the size of a patient. Int J Obes Relat Metab Disord 2001;25(8):1246–1252 [DOI] [PubMed] [Google Scholar]
- 132.Bertakis KD, Azari R. The impact of obesity on primary care visits. Obes Res 2005;13(9):1615–1622 [DOI] [PubMed] [Google Scholar]
- 133.Anderson DA, Wadden TA. Bariatric surgery patients’ views of their physicians; weight-related attitudes and practices. Obes Res 2004;12(10):1587–1595 [DOI] [PubMed] [Google Scholar]
- 134.Brown I, Thompson J, Tod A, Jones G. Primary care support for tackling obesity: a qualitative study of the perceptions of obese patients. Br J Gen Pract 2006;56(530):666–672 [PMC free article] [PubMed] [Google Scholar]
- 135.Amy NK, Aalborg A, Lyons P, Keranen L. Barriers to routine gynecological cancer screening for White and African-American obese women. Int J Obes (Lond) 2006;30(1):147–155 [DOI] [PubMed] [Google Scholar]
- 136.Ferrante JM, Ohman-Strickland P, Hudson SV, Hahn KA, Scott JG, Crabtree BF. Colorectal cancer screening among obese versus non-obese patients in primary care practices. Cancer Detect Prev 2006;30(5):459–465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Ostbye T, Taylor DH, Jr, Yancy WS, Jr, Krause KM. Associations between obesity and receipt of screening mammography, Papanicolaou tests, and influenza vaccination: results from the Health and Retirement Study (HRS) and the Asset and Health Dynamics Among the Oldest Old (AHEAD) Study. Am J Public Health 2005;95(9):1623–1630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Wee CC, McCarthy EP, Davis RB, Phillips RS. Screening for cervical and breast cancer: is obesity an unrecognized barrier to preventive care? Ann Intern Med 2000;132(9):697–704 [DOI] [PubMed] [Google Scholar]
- 139.Mitchell RS, Padwal RS, Chuck AW, Klarenbach SW. Cancer screening among the overweight and obese in Canada. Am J Prev Med 2008;35(2):127–132 [DOI] [PubMed] [Google Scholar]
- 140.Wee CC, Phillips RS, McCarthy EP. BMI and cervical cancer screening among White, African American, and Hispanic women in the United States. Obes Res 2005;13(7):1275–1280 [DOI] [PubMed] [Google Scholar]
- 141.US Department of Health and Human Services, The Advertising Council. Healthy Lifestyles and Disease Prevention Media Campaign: Take a Small Step to Get Healthy. [white paper]. 2004. Available at: http://www.smallstep.gov/pdf/obesity_whitepaperfinal_71205.pdf. Accessed November 30, 2009.
- 142.Stein K. Obesity PSAs: are they working as a public service? J Am Diet Assoc 2008;108(1)25–28 [DOI] [PubMed] [Google Scholar]
- 143.Downey M. Expression of bias against obesity in public policy and its remedies. : Brownell KD, Puhl RM, Schwartz MB, Rudd L, Weight Bias: Nature, Consequences, and Remedies New York, NY: The Guilford Press; 2005 [Google Scholar]
- 144.National Institutes of Health Estimates of funding for various diseases, conditions, research areas. 2008. Available at: http://www.nih.gov/news/fundingresearchareas.htm. Accessed February 22, 2008
- 145.151 Cong Rec H8927 (2005) (statement of Rep Chabot) [Google Scholar]
- 146.Zhang Q, Wang Y. Socioeconomic inequality of obesity in the United States: do gender, age, and ethnicity matter? Soc Sci Med 2004;58(6):1171–1180 [DOI] [PubMed] [Google Scholar]
- 147.Institute of Medicine Preventing Childhood Obesity Washington, DC: The National Academies Press; 2005 [Google Scholar]
- 148.Berg F, Buechner J, Parham E, Weight Realities Division of the Society for Nutrition Education Guidelines for childhood obesity prevention programs: promoting healthy weight in children. J Nutr Educ Behav 2003;35(1):1–4 [DOI] [PubMed] [Google Scholar]
- 149.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA 2006;295(13):1549–1555 [DOI] [PubMed] [Google Scholar]