Abstract
Objectives. We quantified the relationship between gonorrheal infection rates in California and a measure of poverty status and investigated how this relationship and the spatial dispersion of cases varied among the 4 dominant racial/ethnic groups in the state.
Methods. We geocoded gonorrhea cases reported in California between 2004 and 2006, and estimated the poverty status of each case by using the percentage of residents living below poverty in the census tract of residence. We calculated infection rates for African American, Asian, Hispanic, and White cases in each of 4 poverty strata. We mapped cases to visualize the patterns of spatial dispersion associated with each race/ethnicity–poverty combination.
Results. There was a strong positive relationship between poverty and infection, but racial/ethnic disparities in infection, driven by a disproportionate level of gonorrhea among African Americans, eclipsed this differential. The degree of spatial aggregation varied substantially among groups and was especially pronounced for African Americans with gonorrhea in the highest poverty category.
Conclusions. Prevention efforts should target low-income neighborhood “hot spots” to reach the largest numbers of cases, particularly among African Americans.
Socioeconomic disparities in health make significant contributions to patterns of morbidity and mortality in the United States.1–4 Socioeconomic status (SES) can directly affect access to health care and is often strongly correlated with behavioral patterns and community attributes that profoundly influence health risks and outcomes. Although the elimination of these inequalities is a fundamental objective of many public health initiatives,5 quantifying and monitoring socioeconomic disparities in health is hampered by the paucity of socioeconomic data in most public health surveillance systems.
The use of area-based socioeconomic measures offers a means to link case-based surveillance data with census-based information on associated populations and communities.6,7 Case residential address data are assigned a latitude and longitude (geocoded), and these coordinates are then used to map geocoded cases and associate them with census tracts and the socioeconomic data collected within them as part of the decennial US Census. Thus, area-based socioeconomic measures provide estimates of the SES of individual geocoded cases, as well as direct measures of socioeconomic attributes of the communities in which they reside.6
Sexually transmitted diseases (STDs) have long been of interest to public health practitioners concerned with socioeconomic disparities in health outcomes,8,9 and they represent an ideal focus for geocoding-based studies of such variation. Relative to other infectious and chronic diseases, the geographic ubiquity and high incidence of STDs should allow socioeconomic disparities in infection rates to be readily quantified and accurately mapped. Analyses of data from Massachusetts, Rhode Island, and Virginia found significant positive relationships between rates of STDs and “percent below poverty,” a census-based measure of SES.10,11 A number of other geocoding-based studies of socioeconomic variation in STDs produced similar findings,12–14 but these were limited in their geographic breadth as they examined data from only large cities.
Pronounced racial/ethnic heterogeneity in STDs has also been documented,15–19 but because it is caused in part by disparities in SES among groups, the relative contributions of race/ethnicity and poverty to STD epidemiology remain unclear. Analyses that consider these relationships simultaneously across broader spatial scales, incorporating more cases with a collectively greater diversity of communities and racial/ethnic–socioeconomic combinations, are needed to more accurately and precisely quantify the influence of SES and race/ethnicity on patterns of STDs.
We undertook a geocoding-based social gradient analysis by using gonorrhea incidence data collected over a 3-year period in California at a time when gonorrhea rates were increasing for the first time in decades.20 The objectives of our study were (1) to quantify the relationship between infection rates and a measure of poverty status, (2) to assess whether and how this relationship varied among the 4 dominant racial/ethnic groups in the state, and (3) to examine variation in patterns of spatial dispersion of gonorrhea cases among racial/ethnic–poverty combinations by mapping geocoded cases, in order to better target gonorrhea prevention efforts.
METHODS
We analyzed gonorrhea case-based surveillance data (age, gender, race/ethnicity, and address) reported to the California Department of Public Health's STD Control Branch between 2004 and 2006.18 Using SAS version 9.1 (SAS Institute Inc, Cary, NC), we assigned each case to 1 of 5 address categories: (1) incomplete (address field blank or containing insufficient information to permit geocoding), (2) nonresidential (address corresponding to location other than the patient's permanent residence [e.g., health clinics, detention facilities]), (3) PO Box, (4) homeless (when explicitly identified as such), and (5) potentially geocodable (address information that appeared sufficient to permit geocoding to a residential address). We then validated and standardized addresses of all potentially geocodable cases according to US Postal Service address data and abbreviations with the software ZP4 (Semaphore Corp, Nipomo, CA).
Once addresses were standardized, we geocoded and associated addresses with census tracts by using the Tables Address Geocoder application created by the California Department of Public Health's Environmental Health Investigations Branch (http://www.ehib.org/geocoding_tool.jsp). We used the Tables Address Geocoder to apply 5 different address locator algorithms, sequentially in the following order, to geocode each address: TeleAtlas Points (2006), TeleAtlas Streets (2006), Navteq Streets (2006), GDT Streets (2005), and Tiger Streets (2005). An address was considered successfully matched when its Tables Address Geocoder–generated match score, analogous to the match score generated by geocoding in ArcGIS version 9.2 (ESRI, Redlands, CA), was at least 80.
Quantifying Socioeconomic Levels of Census Tracts
We used data on census tract population size and the number of people living below poverty, collected as part of the 2000 US Census,21 to estimate the socioeconomic profile of each census tract in California. The area-based socioeconomic measure percent below poverty7 was calculated as the quotient of the number of people in a tract living below the federal poverty line and the population of that tract (summary file 3, table 87).21 Each tract was assigned to 1 of 4 poverty categories on the basis of its percent below poverty values (< 10%, 10% to 19.99%, 20% to 29.99%, and ≥ 30% of residents living below poverty). We chose cut points for these categories on the basis of quartiles of the full data set so that the number of cases in each category was roughly equal. Federal guidelines designate any region where 20% or more of the population is below the US poverty line as a “poverty area.”22 We did not assign a percent below poverty value to census tracts in which poverty information had been collected from fewer than 60% of the residents because these are usually areas where a high percentage of the population is institutionalized (e.g., incarcerated) and therefore not representative of the state's general population.
Calculating Infection Rates
The outcomes of interest were the mean infection rate for each of the 4 racial/ethnic groups, 4 poverty categories, and 16 racial/ethnic–poverty combinations. Geocoded cases assigned to census tracts constituted numerator data for the calculation of infection rates (cases per 100 000 persons). An appreciable number of cases lacked race/ethnicity information and could therefore not be used directly in calculations of race/ethnicity–specific infection rates. To retain these cases in the data set we calculated rates with numerator data weighted for missing race/ethnicity. For each poverty category, we used the percentage of cases for which race/ethnicity was known as a weighting coefficient, and the inverse of this percentage was multiplied by the number of known cases in each of the 4 major racial/ethnic groups (Asians, African Americans, Hispanics, and Whites) to generate a weighted number of cases. Denominator data for rate calculations included the total population and the number of individuals who self-identified as Asian only, Black or African American only, Hispanic or Latino, and White only in each census tract (summary file 1, table 8).21
We used contingency tables analyses to compare men and women, and the 4 racial/ethnic groups in terms of the proportion of potentially geocodable cases relative to the number of cases in the 4 other address categories combined. We calculated confidence intervals (CIs) for rates with the exact Poisson method and we calculated rate ratios with the median-unbiased estimation (midp) method, both implemented in the Epitools package (Center for Infectious Diseases and Emergency Readiness, Berkeley, CA) in R (R Foundation for Statistical Computing, Vienna, Austria). We used ArcGIS version 9.2 to generate maps that showed the distribution of cases by poverty category and race/ethnicity. We quantitatively compared the degree of spatial aggregation among cases associated with each of the 16 racial/ethnic–poverty combinations by using Ripley K-function23 analysis performed in R.
RESULTS
Of the 98 355 cases of gonorrhea reported in California between 2004 and 2006, case counts and the distribution of cases among the 5 address categories were similar among years (Appendix 1, available as a supplement to the online version of this article at http://www.ajph.org). Across years there were more cases among males (53.6%) than among females (46.0%), and the distribution of cases varied among the 4 racial/ethnic groups, with African Americans disproportionately represented (26.1% of cases) followed by Hispanics (20.6%), Whites (17.4%), and Asians (2.4%; Appendix 1).
The majority of cases were classified as having addresses that were potentially geocodable (mean across years = 84.5%) or incomplete (12.2%). None of the remaining 3 address categories accounted for more than 2% of the total cases (homeless = 0.3%; PO Box = 1.4%; nonresidential = 1.7%; Appendix 1). The percentage of cases with potentially geocodable addresses was significantly higher than expected among females (85.9%) compared with males (83.6%; χ21 = 101.7; P < .001), and there were statistically significant differences in this proportion when the 4 largest racial/ethnic groups were compared (χ23 = 266.6; P < .001). The largest deviations were a lower proportion of potentially geocodable cases among Whites (88.8%) and a higher proportion among African Americans (93.3%).
Overall, 80.7% of all cases were successfully geocoded (Appendix 1). The percent of cases geocoded was 79.8% for males, 82.0% for females, 89.5% for African Americans, 86.9% for Asians and Hispanics, and 84.9% for Whites. The proportion of potentially geocodable cases that were successfully geocoded was at least 95% for each year, gender, and racial/ethnic group. Whereas only 0.4% of all cases were missing gender information, 32.5% were missing data on race/ethnicity. Of these, 95.1% were successfully geocoded and their race/ethnicity estimated with the aforementioned weighting procedure.
Of the 7049 census tracts in California, available data on resident poverty were sufficient to classify 6941 (98.5%) into 1 of the 4 poverty categories (Table 1). Forty-seven percent of tracts were assigned to the < 10% of residents living below poverty category, 28.5% were in the 10% to 19.99% category, 14.2% were in the 20% to 29.99% category, and 10.4% were in the ≥ 30% category. Tracts in the highest poverty category were geographically concentrated in urban centers (e.g., San Francisco, Los Angeles, San Diego) and along a north–south transect spanning the San Joaquin Valley, an urbanized corridor in the central part of the state bisected by 2 major highways that connect large metropolitan areas in northern and southern California (Appendix 2, available as a supplement to the online version of this article at http://www.ajph.org).
TABLE 1.
Number of Geocoded Gonorrhea Cases, Total Number of Census Tracts, Number of Census Tracts in Each Poverty Category With Reported Gonorrhea Cases, and Population Counts, by Race and Poverty Category: California, 2004–2006
| < 10% of Residents Living Below Poverty Line | 10%–19.99% of Residents Living Below Poverty Line | 20%–29.99% of Residents Living Below Poverty Line | ≥ 30% of Residents Living Below Poverty Line | Residents Unassigned to Poverty Category | Total | |
| No. of geocoded cases | 19 209 | 23 862 | 16 925 | 19 026 | 331 | 79 353 |
| African Americans | 2 941 | 5 790 | 5 743 | 8 486 | 56 | 23 016 |
| Asians | 836 | 596 | 315 | 277 | 17 | 2 041 |
| Hispanics | 2 986 | 5 433 | 4 426 | 4 699 | 86 | 17 630 |
| Whites | 5 748 | 4 922 | 2 216 | 1 560 | 90 | 14 536 |
| Other known races | 242 | 243 | 134 | 126 | 7 | 752 |
| Unknown | 6 456 | 6 878 | 4 091 | 3 878 | 75 | 21 378 |
| No. of census tracts | 3 259 | 1 975 | 986 | 721 | 108 | 7 049 |
| No. of census tracts with ≥ 1 case of gonorrhea | 2 919 | 1 872 | 953 | 714 | 75 | 6 533 |
| With ≥ 1 African American cases | 1 089 | 1 043 | 594 | 554 | 36 | 3 316 |
| With ≥ 1 Asian case | 559 | 397 | 195 | 183 | 13 | 1 347 |
| With ≥ 1 Hispanic case | 1 379 | 1 407 | 832 | 663 | 34 | 4 315 |
| With ≥ 1 White case | 1 948 | 1 329 | 610 | 434 | 39 | 4 360 |
| With ≥ 1 case among other known races | 217 | 196 | 115 | 93 | 7 | 628 |
| With ≥ 1 case among unknown races | 2 076 | 1 438 | 753 | 591 | 34 | 4 892 |
| Population | 15 240 238 | 9 890 103 | 4 951 416 | 3 305 092 | 484 799 | 33 871 648 |
| African Americans | 550 755 | 647 656 | 472 049 | 431 577 | 79 889 | 2 181 926 |
| Asians | 1 980 594 | 963 921 | 407 511 | 256 582 | 40 252 | 3 648 860 |
| Hispanics | 2 539 241 | 3 595 350 | 2 653 477 | 2 040 548 | 137 940 | 10 966 556 |
| Whites | 9 590 616 | 4 289 747 | 1 249 323 | 477 736 | 209 368 | 15 816 790 |
| Other known races | 135 437 | 121 765 | 54 197 | 35 709 | 7293 | 354 401 |
Notes. Case counts reflect gonorrhea cases reported to the California Department of Public Health STD Control Branch between 2004 and 2006. Census tract and population count data for California were collected as part of the 2000 US Census and obtained from the US Census Bureau.
Poverty, Race/Ethnicity, and Infection Rates
Overall, there was a strong positive relationship between poverty and infection. The infection rate among census tracts in the highest poverty category (191.9 per 100 000 persons) was 4.6 times higher (95% CI = 4.4, 4.7) than was the rate in the lowest poverty category (42.0 per 100 000 persons; Table 2). There was a large disparity between the magnitude of the rate associated with African Americans and those of the other racial/ethnic groups. The overall rate among African Americans (392.7 per 100 000 persons) was 6.4 times higher (95% CI = 6.2, 6.5) than was the rate associated with the next closest group (Hispanics; 61.7 per 100 000 persons) and 10.9 times higher (95% CI = 10.5, 11.3) than was the rate among Whites (36.1 per 100 000 persons), which was the group with the largest population.
TABLE 2.
Weighted Gonorrhea Infection Rates Per 100 000 Population Per Year, by Race and Poverty Category: California, 2004–2006
| % of Residents Living Below Poverty Line | African American, Rate (95% CI) | Asian, Rate (95% CI) | Hispanic, Rate (95% CI) | White, Rate (95% CI) | Total, Rate (95% CI) |
| < 10 | 268.11 (254.43, 281.78) | 21.19 (19.17, 23.22) | 59.04 (56.05, 62.03) | 30.09 (28.99, 31.19) | 42.01 (40.98, 43.04) |
| 10–19.99 | 418.68 (402.92, 434.44) | 28.96 (25.56, 32.35) | 70.77 (68.02, 73.52) | 53.75 (51.54, 55.93) | 80.42 (78.66, 82.19) |
| 20–29.99 | 534.81 (513.94, 555.67) | 33.98 (28.32, 39.64) | 73.32 (70.07, 76.58) | 77.97 (73.08, 82.87) | 113.94 (110.97, 116.91) |
| ≥ 30 | 823.22 (796.15, 850.29) | 45.20 (36.97, 53.42) | 96.41 (92.15, 100.67) | 136.71 (126.23, 147.20) | 191.89 (187.16, 196.61) |
| Total | 392.68 (384.37, 401.00) | 21.45 (19.95, 22.95) | 61.67 (60.20, 63.14) | 36.07 (35.14, 37.01) | 96.79 (95.74, 97.84) |
Note. CI = confidence interval. Gonorrhea rates were calculated using case counts weighted for missing race/ethnicity data. Weighted rates and 95% CIs are calculated within each racial/ethnic group or among the 4 racial/ethnic or poverty category totals by the exact Poisson method. Population count data for California were collected as part of the 2000 US Census and obtained from the US Census Bureau.
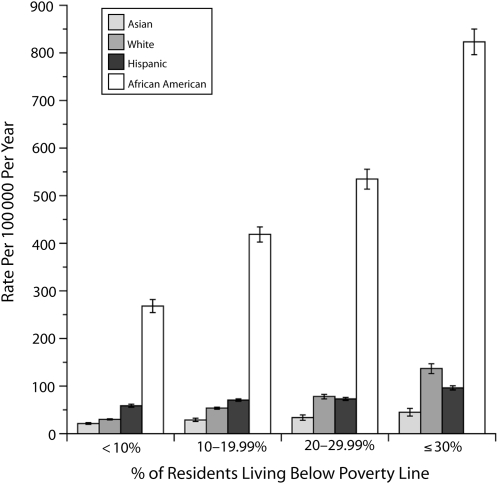
When data were simultaneously stratified by both poverty and race/ethnicity, rates among African Americans were considerably higher than they were among any of the other racial/ethnic groups irrespective of poverty category (Figure 1). For example, the rate among African Americans in the highest poverty category (823.2 per 100 000 persons) was 6.0 times higher (95% CI = 5.5, 6.5) than was the rate among Whites (136.7 per 100 000 persons) in the same poverty category. This racial/ethnic differential eclipsed in magnitude the disparities attributed to poverty. The rate among African Americans in the lowest poverty category (268.1 per 100 000 persons) was 2.0 to 5.9 times higher (95% CI = 1.8, 7.2) than were rates for any of the other 3 racial/ethnic groups in the highest poverty category. We repeated these comparisons with unweighted rates (excluding cases with unknown race/ethnicity), and the results were qualitatively identical to those detailed before.
FIGURE 1.
Gonorrhea infection rates, by race/ethnicity and percentage of census tract residents living below the poverty line: California, 2004–2006.
Note. Gonorrhea rates were calculated using case counts weighted for race/ethnicity. Error bars show 95% confidence intervals calculated with the exact Poisson method. Census tract and population count data for California were collected as part of the 2000 US Census and obtained from the US Census Bureau.
Geographic Distribution and Aggregation of Cases
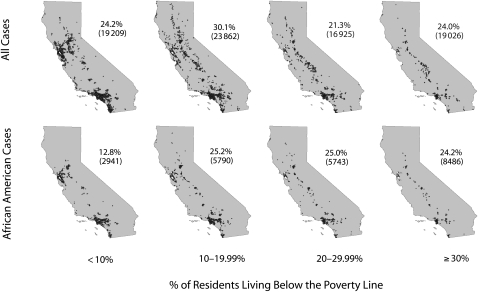
Mapping of geocoded cases illustrated a striking pattern of spatial aggregation of gonorrhea infection across California (Figure 2). This was partially a consequence of the fact that as community poverty increased, fewer census tracts were associated with each poverty stratum. In the lowest poverty category, 19 209 (24.2%) of the total geocoded cases were distributed among 2919 census tracts, which represented 44.7% of the total number of tracts in the state with at least 1 gonorrhea case (Table 1). The mean (±SE) number of cases in the lowest poverty census tracts was 2.9 ± 0.1 per tract per year (among tracts with at least 1 case in a given year). In contrast, a roughly equal number of cases in the highest poverty category (19 026, or 24.0% of all geocoded cases) were concentrated in just 714 census tracts, representing 10.9% of the total number of tracts in the state with at least 1 associated case of gonorrhea in a given year. The mean (±SE) number of cases in these highest poverty tracts was 9.4 ± 0.1 cases per tract per year. These highest poverty tracts and the associated cases were aggregated primarily in or near San Francisco, Los Angeles, San Diego, Sacramento, and the San Joaquin Valley (Figure 2).
FIGURE 2.
Spatial distribution of geocoded gonorrhea cases across census tracts among all California residents and among African Americans, by the percentage of residents living below the poverty line: California, 2004–2006.
Note. The percentage of cases within each poverty level category and raw case counts upon which these values are based (in parentheses) are displayed to the right of each map. Census tract and population count data for California were collected as part of the 2000 US Census and obtained from the US Census Bureau.
This pattern of spatial aggregation was especially pronounced for African Americans, the racial/ethnic group with the highest number of cases and the only group characterized by a strong positive relationship between number of cases and community poverty (Table 1). The number of African American cases in the highest poverty category (n = 8486) was far higher than was the number associated with any other race/ethnicity–poverty combination. These high-poverty African American cases, representing 36.9% of geocoded African American cases and 10.69% of all geocoded cases across the state, were concentrated in just 554 census tracts with at least 1 gonorrhea case reported, or 8.5% of such census tracts (Table 1; Table 3; Figure 2). The mean annual African American case density in these tracts was 6.3 ± 0.2 cases. Results of the Ripley K-function analysis provided quantitative evidence that African American cases associated with the highest poverty category exhibited by far the greatest degree of spatial aggregation relative to cases in the other 15 racial/ethnic–poverty combinations (Appendix 3, available as a supplement to the online version of this article at http://www.ajph.org).
TABLE 3.
Gonorrhea Cases Presented as a Percentage of Total California Gonorrhea Cases and of Total State Population, by Race and Poverty Category: California, 2004–2006
| < 10% of Residents Living Below Poverty Line | 10%–19.99% of Residents Living Below Poverty Line | 20%–29.99% of Residents Living Below Poverty Line | ≥ 30% of Residents Living Below Poverty Line | Total | |
| African American | |||||
| % of cases | 3.71 | 7.30 | 7.24 | 10.69 | 38.81 |
| % of population | 1.63 | 1.91 | 1.39 | 1.27 | 6.44 |
| Asian | |||||
| % of cases | 1.05 | 0.75 | 0.40 | 0.35 | 3.60 |
| % of population | 5.85 | 2.85 | 1.20 | 0.76 | 10.77 |
| Hispanic | |||||
| % of cases | 3.76 | 6.85 | 5.58 | 5.92 | 30.08 |
| % of population | 7.50 | 10.61 | 7.83 | 6.02 | 32.38 |
| White | |||||
| % of cases | 7.24 | 6.20 | 2.79 | 1.97 | 25.78 |
| % of population | 28.31 | 12.66 | 3.69 | 1.41 | 46.70 |
| Total | |||||
| % of cases | 24.21 | 30.07 | 21.33 | 23.98 | |
| % of population | 44.99 | 29.20 | 14.62 | 9.76 | |
Note. Percentages of gonorrhea cases were calculated using case counts weighted for missing race/ethnicity data. Population count data for California were collected as part of the 2000 US Census and obtained from the US Census Bureau.
DISCUSSION
Our analyses documented strong gradients in gonorrhea rates by poverty status and independently by racial/ethnic group, with African Americans having the highest gonorrhea rates at all levels of poverty. Rates of infection were positively related to the percent of census tract residents living below the poverty line, with the average rate in tracts with at least 30% of residents below poverty more than 4.5 times the rate in tracts for which the poverty fraction was less than 10%. Similar relationships have been documented in other states,10,11,24 but our study is by far one of the largest geocoding-based assessments of SES-related trends in the epidemiology of an STD–in terms of geographic area, total population, and number of cases–conducted in the United States to date.
Additionally, we found that high-poverty gonorrhea cases were highly aggregated in a relatively small number of census tracts. This result suggests that targeted prevention efforts in neighborhood “hot spots” could reach large numbers of cases, particularly among African Americans, and that a range of screening programs, prevention outreach, and social marketing activities should be focused in these areas. With the complex relationships among STD rates, race/ethnicity, poverty, and related socioeconomic-related factors (e.g., access to medical care, education, unemployment, incarceration, racism), results of our analyses support control efforts that are collaborative and involve partners operating in a number of domains rather than efforts that are focused on the biomedical prevention “silo” alone.
We also found evidence for striking racial/ethnic disparities in gonorrhea infection rates that eclipsed in magnitude the disparities attributable to poverty. The overall rate among African Americans was between 6.4 and 18.3 times higher than were rates for the other 3 racial/ethnic groups examined, and rates among African Americans in the lowest poverty stratum were double the highest rate among the other 3 racial/ethnic groups in the highest poverty stratum. When the overall rate among African Americans was compared with that among Whites, the rate ratio of 10.9 is close to the value of 11.8 calculated for gonorrhea cases in western states of the United States in 2005 as part of a nationwide study of STD disparities in African American communities.15 Race/ethnicity and socioeconomic status are highly correlated, with African Americans and Hispanics often associated with lower socioeconomic positions relative to Asians and Whites. Similar to a number of other studies that have attempted to decouple the influence of these 2 factors on patterns of STDs, our analyses show that racial/ethnic differences in gonorrhea rates persisted after we stratified or controlled for indicators of poverty.12–14,25,26 Because of the disproportionate burden of cases among African Americans, studies and intervention strategies that focus on disease dynamics in this group are critical to reducing both the overall number of cases and the magnitude of racial/ethnic disparities in disease levels.15,27
Although differences in individual behaviors related to exposure, transmission, and treatment seem likely contributors to racial/ethnic variation in infection rates, findings that show the persistence of racial/ethnic disparities after individual behavior is controlled for13,25,26,28 indicate the influence of other factors. The context dependence of individuals within larger sexual networks,29 especially involving partner choice and assortative mating, have been shown to increase infection rates among African Americans by linking peripheral populations with areas of high infection.30 Lower levels of access to or quality of care in these areas are also probably important factors.31 Provider behavior could further contribute if clinics used by particular racial/ethnic groups are more likely to perform diagnostic tests and report infection statistics.32 Regardless of the mechanisms by which gonorrhea incidence became higher among African Americans than it did in other racial/ethnic groups, the higher incidence has resulted in disproportionately higher prevalence33 so that, even if all risk factors equalize, the higher prevalence alone would sustain ongoing higher incidence unless aggressive control measures intervene.
Although the observation of gonorrhea concentration within areas of high poverty and large African American and Hispanic populations was somewhat expected, we were surprised by the degree to which aggregation varied with race/ethnicity and socioeconomic status. This general pattern is consistent with the concept of spatially discrete “core” areas of infection34–38 and evidences the context dependence of individual behaviors that is central to sexual network theory39–41 and models of within-group mixing, assortative partner selection, and internetwork bridging30,42–44 that are often invoked to explain large-scale patterns of sexually transmitted infection.
By design, the highest and lowest poverty strata considered in our analyses each accounted for about one fourth of the total number of geocoded cases. Despite this parity, the lowest-poverty cases were distributed among 41% of the state's census tracts, whereas high-poverty cases were aggregated within just 10% of the tracts. This phenomenon was especially pronounced among African Americans. Low-poverty cases, representing 13% of the African American cases and 4% of all cases in the state, occurred within 15% of the state's tracts, whereas high-poverty cases, accounting for 37% of African American cases and 11% of all cases statewide, were concentrated in just 8% of all tracts. The high mean annual African American case density in these tracts suggests that the pattern of spatial aggregation among high-poverty cases was driven largely by infection in this racial/ethnic group. These areas of high gonorrhea incidence would seem to be ideal locations for targeted intervention strategies and for studies of disease transmission within sexual networks.45,46
Our analytical approach was not without problems that limit or suggest caution in interpretation of our results. First, more than 15% of cases could not be geocoded and were excluded from our analyses. Among geocoded cases, a higher proportion were female than were male, and there were fewer White and more African American cases geocoded, relative to the proportion for Hispanics and Asians. Although biases could be introduced into our findings as a result, the absolute differences seem too small for their influence to conceivably affect our interpretation of the analyses, particularly the overall relationship between poverty and infection rates.
Second, the use of area-based socioeconomic measures to approximate the socioeconomic status of individual cases may not be precise if variance in regard to the mean socioeconomic status within a spatial area of inference (here, census tract) is large. However, because case-specific data on socioeconomic characteristics are almost never collected as part of public health surveillance, few alternatives are available for studies of the relationship between health outcomes and socioeconomic status. Use of area-based socioeconomic measures should provide a reasonable approximation of such information, but because socioeconomic status is inherently an aggregate measure affected by a multitude of different factors (e.g., income, education, employment, home ownership), identifying a simple but accurate metric with which to quantify it can be difficult. Studies of socioeconomic disparities in a wide array of health conditions (including 3 STDs) found that, relative to a number of other measures of community poverty, the percent below poverty metric appears to be particularly robust in its ability to detect socioeconomic gradients in health outcomes.11 In addition to estimating an individual's level of poverty, such measures should accurately represent the socioeconomic features of the neighborhoods and communities in which the individual resides.6 The influence of such environmental characteristics on individual health outcomes, and on STDs in particular, has been documented empirically.47
Finally, because of our use of year 2000 census data to estimate population sizes for infection rate calculations and the steady rates of population growth in California, it seems probable that our methods slightly overestimated actual rates and may have introduced some small biases between racial/ethnic and poverty groups because of differential growth among populations (e.g., relatively high growth rates among Hispanics). In addition, our method of weighting data to retain cases with unreported race/ethnicity may also have reduced the precision, and perhaps accuracy, of our race-specific rate estimates. There was a slight positive relationship between the proportion of cases of known race/ethnicity and poverty. Although we do not have data to quantify the nature or magnitude of the bias that this may have introduced, it seems likely that it would result in more cases (and a higher weighted rate than expected) at lower poverty levels, making the poverty–infection relationship identified with weighted rates a conservative estimate. The magnitude of the differences we observed among racial/ethnic groups and poverty categories, and the fact that we obtained qualitatively identical results when unweighted rates were compared, suggest that such influences would not have distorted the overall trends sufficiently to alter our conclusions.
Our findings provide strong evidence for pronounced racial/ethnic and socioeconomic variation in rates of sexually transmitted infection in California and highlight the value of spatially explicit analyses for characterizing this heterogeneity and formulating effectively targeted public health interventions.
Acknowledgments
We acknowledge the support from the Centers for Disease Control and Prevention's Outcome Assessment Through Systems of Integrated Surveillance Project (grant H25/CCH922328-02) and the Centers for Disease Control and Prevention's Comprehensive STD Prevention Systems (grant 5H25/PS904362-17).
We thank Denise Gilson, Matt Beyers, Dan Wohlfeiler, Kai-Jen Cheng, Robert Kohn, Peter Kerndt, and Jeff Klauser for their assistance with the collection and processing of the data, and Craig Wolff for access to the Tables Address Geocoding application. Zev Ross graciously provided consultation on methods to quantify spatial aggregation and the R code to perform the Ripley's K-function analyses.
Human Participant Protection
Because these analyses involved only the use of routine surveillance data and publicly available census data, institutional review board approval was not required and was not sought.
References
- 1.Adler NE, Boyce T, Chesney MA, et al. Socioeconomic status and health. The challenge of the gradient. Am Psychol 1994;49(1):15–24 [DOI] [PubMed] [Google Scholar]
- 2.Anderson NB, Armstead CA. Toward understanding the association of socioeconomic status and health: a new challenge for the biopsychosocial approach. Psychosom Med 1995;57(3):213–225 [DOI] [PubMed] [Google Scholar]
- 3.Feinstein JS. The relationship between socioeconomic status and health: a review of the literature. Milbank Q 1993;71(2):279–322 [PubMed] [Google Scholar]
- 4.Davey Smith G, Egger M. Socioeconomic differentials in wealth and health. BMJ 1993;307(6912):1085–1086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Healthy People 2010: Understanding and Improving Health. Vol. 2 2nd ed Washington, DC: US Dept of Health and Human Services; 2000 [Google Scholar]
- 6.Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Painting a truer picture of US socioeconomic and racial/ethnic health inequalities: the Public Health Disparities Geocoding Project. Am J Public Health 2005;95(2):312–323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Race/ethnicity, gender, and monitoring socioeconomic gradients in health: a comparison of area-based socioeconomic measures—the Public Health Disparities Geocoding Project. Am J Public Health 2003;93(10):1655–1671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Darrow WW. Social stratification, sexual behavior, and the sexually transmitted diseases. Sex Transm Dis 1979;6(3):228–230 [DOI] [PubMed] [Google Scholar]
- 9.Morton WE, Horton HB, Baker HW. Effects of socioeconomic status on incidences of three sexually transmitted diseases. Sex Transm Dis 1979;6(3):206–210 [DOI] [PubMed] [Google Scholar]
- 10.Dolan C, Delcher C. Monitoring health inequities and planning in Virginia: poverty, human immunodeficiency virus, and sexually transmitted infections. Sex Transm Dis 2008;35(12):981–984 [DOI] [PubMed] [Google Scholar]
- 11.Krieger N, Waterman PD, Chen JT, Soobader MJ, Subramanian SV. Monitoring socioeconomic inequalities in sexually transmitted infections, tuberculosis, and violence: geocoding and choice of area-based socioeconomic measures—the Public Health Disparities Geocoding Project (US). Public Health Rep 2003;118(3):240–260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ellen JM, Kohn RP, Bolan GA, Shiboski S, Krieger N. Socioeconomic differences in sexually transmitted disease rates among Black and White adolescents, San Francisco, 1990 to 1992. Am J Public Health 1995;85(11):1546–1548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rice RJ, Roberts PL, Handsfield HH, Holmes KK. Sociodemographic distribution of gonorrhea incidence: implications for prevention and behavioral research. Am J Public Health 1991;81(10):1252–1258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lacey CJ, Merrick DW, Bensley DC, Fairley I. Analysis of the sociodemography of gonorrhea in Leeds, 1989–1993. BMJ 1997;314(7096):1715–1718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Newman LM, Berman SM. Epidemiology of STD disparities in African American communities. Sex Transm Dis 2008;35(suppl 12):S4–S12 [DOI] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention Racial disparities in nationally notifiable diseases—United States, 2002. MMWR Morb Mortal Wkly Rep 2005;54(1):9–11 [PubMed] [Google Scholar]
- 17.Sexually Transmitted Disease Surveillance, 2006 Atlanta, GA: Centers for Disease Control and Prevention, US Dept of Health and Human Services; 2007 [Google Scholar]
- 18.California Department of Public Health STD Control Branch. Sexually Transmitted Diseases in California, 2006 Sacramento, CA: California Department of Public Health; 2007 [Google Scholar]
- 19.Miller WC, Ford CA, Morris M, et al. Prevalence of chlamydial and gonococcal infections among young adults in the United States. JAMA 2004;291(18):2229–2236 [DOI] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention Increases in gonorrhea—eight western states, 2000–2005. MMWR Morb Mortal Wkly Rep 2007;56(10):222–225 [PubMed] [Google Scholar]
- 21.US Census Bureau Census 2000 [American FactFinder]. Available at: http://factfinder.census.gov. Accessed May 15, 2009
- 22.US Census Bureau Poverty areas. Available at: http://www.census.gov/hhes/www/poverty/definitions.html. Accessed February 11, 2008
- 23.Ripley BD. The second-order analysis of stationary processes. J Appl Probab 1976;13:255–266 [Google Scholar]
- 24.Du P, McNutt LA, O'Campo P, Coles FB. Changes in community socioeconomic status and racial distribution associated with gonorrhea rates: an analysis at the community level. Sex Transm Dis 2009;36(7):430–438 [DOI] [PubMed] [Google Scholar]
- 25.Ellen JM, Aral SO, Madger LS. Do differences in sexual behaviors account for the racial/ethnic differences in adolescents' self-reported history of a sexually transmitted disease? Sex Transm Dis 1998;25(3):125–129 [DOI] [PubMed] [Google Scholar]
- 26.Hallfors DD, Iritani BJ, Miller WC, Bauer DJ. Sexual and drug behavior patterns and HIV and STD racial disparities: the need for new directions. Am J Public Health 2007;97(1):125–132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Barrow RY, Berkel C, Brooks LC, Groseclose SL, Johnson DB, Valentine JA. Traditional sexually transmitted disease prevention and control strategies: tailoring for African American communities. Sex Transm Dis 2008;35(suppl 12):S30–S39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moran JS, Aral SO, Jenkins WC, Peterman TA, Alexander ER. The impact of sexually transmitted diseases on minority populations. Public Health Rep 1989;104(6):560–565 [PMC free article] [PubMed] [Google Scholar]
- 29.Aral SO, Adimora AA, Fenton KA. Understanding and responding to disparities in HIV and other sexually transmitted infections in African Americans. Lancet 2008;372(9635):337–340 [DOI] [PubMed] [Google Scholar]
- 30.Laumann EO, Youm Y. Racial/ethnic group differences in the prevalence of sexually transmitted diseases in the United States: a network explanation. Sex Transm Dis 1999;26(5):250–261 [DOI] [PubMed] [Google Scholar]
- 31.Chandra A, Skinner JS. Geography and racial health disparities. Available at: http://papers.ssrn.com/sol3/papers.cfm?abstract_id=382444. Published 2003. Accessed November 23, 2008. NBER working paper W9513
- 32.Zenilman JM. Gonorrhea, chlamydia and the sexual network: pushing the envelope. Sex Transm Dis 2000;27(4):224–225 [DOI] [PubMed] [Google Scholar]
- 33.Datta SD, Sternberg M, Johnson RE, et al. Gonorrhea and chlamydia in the United States among persons 14 to 39 years of age, 1999 to 2002. Ann Intern Med 2007;147(2):89–96 [DOI] [PubMed] [Google Scholar]
- 34.Becker KM, Glass GE, Brathwaite W, Zenilman JM. Geographic epidemiology of gonorrhea in Baltimore, Maryland, using a geographic information system. Am J Epidemiol 1998;147(7):709–716 [DOI] [PubMed] [Google Scholar]
- 35.Bernstein KT, Curriero FC, Jennings JM, Olthoff G, Erbelding EJ, Zenilman J. Defining core gonorrhea transmission utilizing spatial data. Am J Epidemiol 2004;160(1):51–58 [DOI] [PubMed] [Google Scholar]
- 36.Potterat JJ, Rothenberg RB, Woodhouse DE, Muth JB, Pratts CI, Fogle JS., II Gonorrhea as a social disease. Sex Transm Dis 1985;12(1):25–32 [DOI] [PubMed] [Google Scholar]
- 37.Rothenberg RB. The geography of gonorrhea. Empirical demonstration of core group transmission. Am J Epidemiol 1983;117(6):688–694 [DOI] [PubMed] [Google Scholar]
- 38.Jennings JM, Curriero FC, Celentano D, Ellen JM. Geographic identification of high gonorrhea transmission areas in Baltimore, Maryland. Am J Epidemiol 2005;161(1):73–80 [DOI] [PubMed] [Google Scholar]
- 39.Aral SO, Fenton KA, Holmes KK. Sexually transmitted diseases in the USA: temporal trends. Sex Transm Infect 2007;83(4):257–266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ghani AC, Ison CA, Ward H, et al. Sexual partner networks in the transmission of sexually transmitted diseases. An analysis of gonorrhea cases in Sheffield, UK. Sex Transm Dis 1996;23(6):498–503 [DOI] [PubMed] [Google Scholar]
- 41.Kottiri BJ, Friedman SR, Neaigus A, Curtis R, Des Jarlais DC. Risk networks and racial/ethnic differences in the prevalence of HIV infection among injection drug users. J Acquir Immune Defic Syndr 2002;30(1):95–104 [DOI] [PubMed] [Google Scholar]
- 42.Aral SO, Hughes JP, Stoner B, et al. Sexual mixing patterns in the spread of gonococcal and chlamydial infections. Am J Public Health 1999;89(6):825–833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ford K, Sohn W, Lepkowski J. American adolescents: sexual mixing patterns, bridge partners, and concurrency. Sex Transm Dis 2002;29(1):13–19 [DOI] [PubMed] [Google Scholar]
- 44.Aral SO. Behavioral aspects of sexually transmitted diseases: core groups and bridge populations. Sex Transm Dis 2000;27(6):327–328 [DOI] [PubMed] [Google Scholar]
- 45.Han Y, Coles FB, Muse A, Hipp S. Assessment of a geographically targeted field intervention on gonorrhea incidence in two New York State counties. Sex Transm Dis 1999;26(5):296–302 [DOI] [PubMed] [Google Scholar]
- 46.Rothenberg RB, Potterat JJ. Temporal and social aspects of gonorrhea transmission: the force of infectivity. Sex Transm Dis 1988;15(2):88–92 [DOI] [PubMed] [Google Scholar]
- 47.Cohen D, Spear S, Scribner R, Kissinger P, Mason K, Wildgen J. “Broken windows” and the risk of gonorrhea. Am J Public Health 2000;90(2):230–236 [DOI] [PMC free article] [PubMed] [Google Scholar]