Abstract
Objective
Insufficient sleep in children is associated with adverse health effects. We examined the associations of early life risk factors with infant sleep duration.
Methods
We studied 1676 mother-infant pairs in a pre-birth cohort study. Main outcomes were mothers’ report of their infants’ average 24-hour sleep duration at 6 months, 1 year, and 2 years of age.
Results
Infants slept mean (SD) durations of 12.2 (2.0) hours/day at 6 months, 12.8 (1.6) hours/day at 1 year, and 11.9 (1.3) hours/day at 2 years. In multivariable regression models, maternal antenatal depression, introduction of solids < 4 months, and infant TV/video viewing were associated with shorter sleep durations at both 1 and 2 years of age. Estimates were 0.36 fewer hours/day of sleep for maternal antenatal depression, 0.39 fewer hours/day of sleep if infant was introduced to solids < 4 months, and 0.11 fewer hours/day of sleep for each 1-hour of TV viewed per week. Attendance at child care outside the home was associated with 0.18 fewer hours/day of sleep at age 2 years. At 2 years of age, black, Hispanic, and Asian infants slept 0.40, 0.82, and 0.95 fewer hours per day, respectively, than white infants.
Conclusions
Maternal depression during pregnancy, early introduction of solid foods, infant TV viewing, and attendance of child care were associated with shorter infant sleep duration. Racial/ethnic minority children slept fewer hours in the first two years of life than white children. Our results suggest that various risk factors, some potentially modifiable, are worthy of clinical consideration when addressing infant sleep duration.
INTRODUCTION
Sleep is an essential physiological component of health and well being in both children and adults. In infancy, recommendations from the National Sleep Foundation for sleep range from 10.5 to 18 hours/day among newborns to 12–14 hours/day among 1–3 year olds. Insufficient sleep in older children appears to have negative effects on cognitive development, mood regulation, and overall health.1 Among infants, short sleep duration and poor sleep quality have been associated with later obesity 2 and behavioral problems.3 Recent studies suggest that children are getting insufficient sleep, that the quality of their sleep is too often compromised, 4 and that pediatric sleep disturbances often become chronic, with few children outgrowing the problem.5, 6
Few studies have examined correlates of infant sleep duration in the first two years of life which is when sleep behaviors and patterns are being established.7, 8 It is possible that such factors could be possible foci of interventions to prevent both short- and long-term sleep problems. Some factors that have been identified as negatively impacting infant sleep have included TV viewing 9 and past history of maternal depression.10 These studies, however, have been limited by an inability to adjust for a wide range of potential confounders including child health status and infant feeding practices. Studies of maternal alcohol consumption during pregnancy 8, small body size at birth, 8 and exposure to cigarette smoke 11 have shown associations with short infant sleep duration, but these studies have been limited by small sample sizes.
The purpose of this study was to examine early life risk factors for short infant sleep duration at ages 6 months and 1 and 2 years (herein referred to as “infancy”) independent of sociodemographic characteristics.
METHODS
Subjects/Study Design
Study subjects were participants in Project Viva, a prospective observational cohort study of gestational diet, pregnancy outcomes, and offspring health.12 We recruited women who were attending their initial prenatal visit at 8 urban and suburban obstetrical offices of a large, multi-specialty group practice in eastern Massachusetts. Eligibility criteria included fluency in English, gestational age less than 22 weeks at initial prenatal clinical appointment, and singleton pregnancy. Further details of the recruitment and retention procedures are available elsewhere.12
Of the 2128 women who delivered a live singleton infant, 1802 had sleep data for at least one of the three time points we analyzed during infancy: 6 months, 1 year, and 2 years of age. Since sleep duration at each time point was our main outcome, we included all mother-infant pairs with sleep data at each respective time point and excluded those with missing data on the covariates included in our model. Thus, our sample size was 1676 for the 6 month time point, 1228 for the 1 year time point, and 1365 for the 2 year time point. Comparison of the 1676 participants included in the 6-month analysis with the 452 excluded participants showed that the subjects in this analysis had higher percentage of white (68 v. 47%) and educated (70 v. 45% ≥ college graduate) participants, and had higher household incomes (87 v. 71% ≥ $40,000/yr), but did not differ on mean birth weight. These estimates were similar among the sample with 1-year and 2-year data.
After obtaining informed consent, we performed in-person study visits with the mother during pregnancy (1st and 2nd trimesters) and both mother and child immediately after delivery and at 6 months postpartum. Mothers completed mailed questionnaires at 1 and 2 years postpartum, on which they reported child sleep duration. All procedures were in accordance with the ethical standards for human experimentation established by the Declaration of Helsinki.
Measurements
Parental and Infant Risk Factors
Based on a review of published literature, we identified several potential parental and infancy risk factors that could be associated with shorter sleep duration. Parental risk factors included maternal depression during the 2nd trimester of pregnancy and smoking during pregnancy; maternal depression at 6 months and 1 year postpartum (but not at 2 years); and at each time point, maternal smoking status, and number of smoking household members. We measured maternal depression using the Edinburgh Postnatal Depression Scale; a validated 10-question screening tool (maximum score of 30 with ≥ 13 indicating possible depression).13
Infant-specific risk factors included gestational age at delivery, birth weight for gestational age z-score (a measure of fetal growth),14 feeding type at age 6 months, timing of introduction of solid foods, and at each time point, general health, child TV/video viewing, and whether or not the infant attended any child care outside the home.
Outcome Measures
The primary outcomes were mothers’ report of their infants’ average 24-hour sleep duration at 6 months, 1 year, and 2 years of age. Secondary outcomes included average daytime nap and nighttime sleep durations, which were available only at age 6 months. At 6 months postpartum, we asked mothers 3 questions about their child’s sleep: 1) “In the past month, on average, for how long does your baby nap during the morning”, 2) “In the past month, on average, for how long does your baby nap during the afternoon”, and 3) “In the past month, on average, how many hours does your baby sleep during the night”. At 1 year postpartum, we asked, “In the past month, on average, for how long does your child sleep in a usual 24-hour period? Please include morning naps, afternoon naps, and nighttime sleep”. At 2 years, we asked parents to report the number of hours their child slept in a usual 24-hour period on an average weekday and weekend day in the past month. Response categories included, “< 9 hours, 9 hours a day, 10 hours a day, 11 hours a day, 12 hours a day, 13 hours a day, and 14 or more hours a day”. In a previous study of this cohort, we validated these questions by demonstrating their association with childhood obesity.2
Covariates/Confounders
At enrollment, mothers also reported their age in years, their pre-pregnancy weight and their height, from which we calculated pre-pregnancy body mass index (BMI), parity, marital status, educational attainment, foreign born status, and annual household income. After delivery, mothers reported their infants’ gender and race/ethnicity and the total number of household members.
Statistical Analysis
We first examined unadjusted estimates (in hours/day) of infant sleep duration at 6 months, 1 year, and 2 years by parental and infant risk factors and by sociodemographic characteristics. We then used multivariable linear regression to assess the independent, main effects of parental and infant risk factors on sleep duration at each time point. Each preliminary multivariable model included one of the risk factors of interest (main effects) and all potential confounders. We assessed for potential confounding by examining effect estimates before and after individually adding covariates to the models. We removed from the models variables that did not change the effect estimates by more than 10% and that were not themselves associated with sleep duration. We assessed for co-linearity by examining standard errors when adding variables to the models. We kept in our final model covariates that independently predicted the outcome or acted as confounders. We present effect estimates (β) in units of hours/day and 95% confidence intervals (CI’s).
In secondary analyses, we examined two additional outcomes available only at 6 months of age: average daytime nap and average nighttime sleep durations. We conducted all analyses using SAS, version 9.1 (Cary, North Carolina).
RESULTS
Table 1 and Table 2 summarize parental, household, and infant characteristics of the study sample. Approximately 30% of infants were of non-white race/ethnicity and the majority of infants lived in households with an annual income greater than $40,000/year. Infants slept mean (SD) durations of 12.2 (2.0) h/d at age 6 months, 12.8 (1.6) h/d at age 1 year, and 11.9 (1.3) h/d at age 2 years. At 6 months, the mean (SD) daytime nap duration was 2.9 (1.2) h/d and mean (SD) nighttime sleep duration was 9.3 (1.8) h/d.
Table 1.
Parental and Household Characteristics of Participants at Ages 6 Months, 1 Year, and 2 Years. Data from 1676 Participants in Project Viva.
| Characteristic | Mean (SD) or N (%) |
|---|---|
| Parental and Household Characteristics | |
| Maternal age (years) at enrollment | 32.3 (5.0) |
| Maternal pre-pregnancy BMI (kg/m2) | 24.8 (5.3) |
| Parity at enrollment | |
| ≥ 1 | 862 (51.4) |
| 0 | 814 (48.6) |
| Mother born outside the U.S. | |
| No | 1330 (80.8) |
| Yes | 316 (19.2) |
| Marital status | |
| Married or cohabitating | 1352 (95.8) |
| Other | 59 (4.2) |
| Maternal Education | |
| ≥ College graduate | 1165 (69.8) |
| < College graduate | 503 (30.2) |
| Household Income | |
| ≥ $40,000/year | 1334 (79.6) |
| < $40,000/year | 191 (11.4) |
| Don’t know/missing | 151 (9.0) |
| Maternal depression | |
| Antenatal depression | 128 (9.2) |
| Depression at 6 months postpartum | 118 (8.4) |
| Depression at 1 year postpartum | 77 (6.4) |
| Maternal smoking status (% yes) | |
| Smoked during pregnancy | 179 (11.2) |
| Smoked at 6 months postpartum | 76 (5.4) |
| Smoked at 1 year postpartum | 64 (5.3) |
| Smoked at 2 years postpartum | 68 (5.0) |
| Number of household members who smoked | |
| 0 | 1478 (88.3) |
| 1 | 157 (9.4) |
| ≥ 2 | 38 (2.3) |
| Total number of household members | 3.9 (1.2) |
Table 2.
Infant Characteristics and Sleep Patterns at Ages 6 Months, 1 Year, and 2 Years. Data from 1676 Participants in Project Viva.
| Characteristic | Mean (SD) or N (%) |
|---|---|
| Infant Characteristics | |
| Gestational age at delivery (wks) | 39.5 (1.8) |
| Birth weight for gestational age z-score | 0.20 (0.97) |
| Male gender | 851 (50.8) |
| Race / ethnicity | |
| White | 1137 (68.0) |
| Black | 235 (14.1) |
| Hispanic | 85 (5.1) |
| Asian | 64 (3.8) |
| Other | 150 (9.0) |
| Excellent / Very Good General health | |
| at 6 months | 1342 (94.4) |
| at 1 year | 1121 (91.5) |
| at 2 years | 1247 (91.4) |
| Feeding type at age 6 months | |
| Breast only | 361 (21.5) |
| Mixed breast and formula | 401 (23.9) |
| Weaned | 728 (43.4) |
| Formula only | 186 (11.1) |
| Introduction of solid foods | |
| < 4 months | 249 (17.4) |
| ≥ 4 months | 1182 (82.6) |
| Child TV / Video viewing (hrs/wk) | |
| at 6 months | 0.89 (1.21) |
| at 1 year | 1.20 (1.46) |
| at 2 years | 1.44 (1.22) |
| Any child care outside the home | |
| at 6 months | 719 (42.9) |
| at 1 year | 604 (49.2) |
| at 2 years | 733 (53.9) |
| Infant Sleep Duration (hrs/day) | |
| at 6 months | 12.2 (2.0) |
| at 1 year | 12.8 (1.6) |
| at 2 years | 11.9 (1.3) |
In bivariate analyses, infants whose parents were single or divorced or who lived in homes with lower household incomes and lower maternal educational attainment slept less at each of the 3 time points (Table 3). In addition, black, Hispanic, and other race/ethnicity children slept fewer hours in a 24-hour period (Table 3). Maternal antenatal depression and total number of household members were associated with shorter sleep duration at all three time points (Table 3).
Table 3.
Bivariate Associations of Parent, Household, and Infant Characteristics with Infant Daily Sleep Duration at 6 Months, 1 Year, and 2 Years of Age. Data from 1676 Participants in Project Viva.
| Characteristic | 6 Months | 1 Year | 2 Years |
|---|---|---|---|
| Parental and Household Characteristics | Estimate in Hours/Day (95% Confidence Intervals) | ||
| Maternal age (per 5 years) | 0.02 (−0.08 to 0.12) | 0.00 (−0.09 to 0.09) | 0.04 (−0.03 to 0.11) |
| Maternal pre-pregnancy BMI (kg/m2) | −0.03 (−0.05 to −0.01) | −0.03 (−0.04 to −0.01) | −0.03 (−0.04 to −0.02) |
| Parity | |||
| 0 v. ≥ 1 | −0.15 (−0.34 to 0.04) | −0.08 (−0.26 to 0.10) | 0.22 (0.09 to 0.35) |
| Mother born outside the U.S. | |||
| Yes v. No | −0.05 (−0.29 to 0.20) | −0.20 (−0.44 to 0.04) | −0.34 (−0.51 to −0.17) |
| Marital status | |||
| Not married v. Married or cohabitating | −0.59 (−1.10 to −0.08) | 0.57 (−0.97 to −0.17) | −0.64 (−0.92 to −0.36) |
| Maternal Education | |||
| < College graduate v. ≥ College graduate | −0.46 (−0.67 to −0.25) | 0.25 (−0.45 to −0.04) | −0.49 (−0.63 to −0.34) |
| Household Income | |||
| < $40,000/year v. ≥ $40,000/year | −0.72 (−1.02 to −0.41) | 0.55 (−0.84 to −0.26) | −0.60 (−0.81 to −0.40) |
| Maternal depression | |||
| Antenatal depression | |||
| Yes v. No | −0.61 (−0.96 to −0.26) | 0.39 (−0.72 to −0.06) | −0.70 (−0.94 to −0.45) |
| Depressed at respective time point | |||
| Yes v. No | −0.38 (−0.75 to −0.01) | −0.09 (−0.47 to 0.28) | NA |
| Smoked during pregnancy | |||
| Yes v. No | −0.27 (−0.58 to 0.04) | −0.09 (−0.40 to 0.21) | −0.39 (−0.62 to −0.16) |
| Smoking status at respective time point | |||
| Yes v. No | −0.02 (−0.48 to 0.43) | −0.18 (−0.58 to 0.23) | −0.40 (−0.70 to −0.09) |
| Number of household members who smoked |
|||
| 1 v. 0 | −0.21 (−0.54 to 0.12) | −0.01 (−0.34 to 0.31) | −0.28 (−0.50 to −0.06) |
| ≥ 2 v. 0 | −0.44 (−1.09 to 0.20) | −0.22 (−0.76 to 0.32) | −0.85 (−1.33 to −0.36) |
| Total number of household members | −0.09 (−0.17 to −0.01) | 0.12 (−0.21 to −0.04) | −0.10 (−0.16 to −0.04) |
| Infant Characteristics | |||
| Gestational age at delivery (wks) | 0.02 (−0.03 to 0.07) | 0.03 (−0.02 to 0.08) | 0.02 (−0.01 to 0.06) |
| Birth weight for gestational age z-score | 0.18 (0.09 to 0.28) | 0.07 (−0.03 to 0.16) | 0.06 (−0.01 to 0.13) |
| Gender | |||
| Male v. Female | −0.08 (−0.28 to 0.11) | −0.06 (−0.24 to 0.12) | −0.11 (−0.24 to 0.03) |
| Race / ethnicity | |||
| Black v. White | −0.93 (−1.21 to −0.66) | 0.91 (−1.19 to −0.63) | −0.86 (−1.05 to −0.67) |
| Hispanic v. White | −0.55 (−0.99 to −0.12) | 0.59 (−1.05 to −0.13) | −1.06 (−1.39 to −0.72) |
| Asian v. White | −0.70 (−1.19 to −0.20) | 0.53 (−1.05 to −0.02) | −0.74 (−1.10 to −0.37) |
| Other v. White | −0.32 (−0.66 to 0.01) | 0.50 (−0.79 to −0.21) | −0.50 (−0.71 to −0.29) |
| General health | |||
| Good / Fair v. Excellent / Very Good | −0.67 (−1.11 to −0.22) | −0.50 (−0.82 to −0.18) | −0.43 (−0.67 to −0.19) |
| Feeding type at 6-months of age | |||
| Any breastfeeding v. No breastfeeding | 0.05 (−0.14 to 0.24) | 0.02 (−0.17 to 0.20) | 0.20 (0.07 to 0.33) |
| Introduction of solid foods | |||
| < 4 months v. ≥ 4 months | −0.20 (−0.47 to 0.07) | −0.38 (−0.64 to −0.12) | −0.41 (−0.60 to −0.22) |
| Child TV / Video viewing (hrs/wk) | −0.06 (−0.14 to 0.02) | −0.12 (−0.19 to −0.06) | −0.13 (−0.19 to −0.08) |
| Any child care outside the home | |||
| Yes vs. No | −0.12 (−0.32 to 0.07) | −0.30 (−0.48 to −0.12) | −0.22 (−0.35 to −0.08) |
NA = data not available
In multivariable analyses adjusted for maternal age, parity, and education; household income; and infant gender and race/ethnicity, we found that maternal antenatal depression, introduction of solids < 4 months, and infant TV/video viewing were associated with shorter sleep duration at both 1 and 2 years of age (Table 4). Infants whose mothers were depressed during pregnancy slept 0.36 fewer hours/day at 1 year and 0.38 fewer hours/day at 2 years, compared to children whose mothers were not depressed during pregnancy. Confidence limits were narrow suggesting that our study had sufficient power to detect an association. Furthermore, the confidence limits suggest that the range of infant sleep duration was between 0.02 to 0.71 fewer hours/day if mothers were antenatally depressed. Infants who were introduced to solid foods < 4 months slept 0.39 fewer hours/day at 1 year and 0.22 fewer hours/day at 2 years. Finally, for every 1-hour/week of TV/video viewed at ages 1 and 2 years, infants slept 0.11 fewer hours/day and 0.09 fewer hours/day at 1 and 2 years, respectively (Table 4). Attendance at child care outside the home was also associated with shorter sleep duration at age 2 years. After multivariable adjustment, neither number of household members who smoked nor breastfeeding status at 6 months of age was associated with sleep duration at any time in the first 2 years of life (Table 4).
Table 4.
Multivariable Linear Regression Models* for Daily Sleep Duration Outcomes at 6 Months, 1 Year, and 2 Years of Age. Data from 1676 Participants in Project Viva.
| Characteristic | 6 Months | 1 Year | 2 Years |
|---|---|---|---|
| Parental Risk Factors | Estimate in Hours/Day (95% Confidence Intervals) | ||
| Maternal Antenatal Depression | |||
| Yes v. No | −0.23 (−0.61 to 0.15) | −0.36 (−0.71 to −0.02) | −0.38 (−0.63 to −0.12) |
| Number of household members who smoked |
−0.09 (−0.38 to 0.20) | 0.06 (−0.19 to 0.31) | −0.16 (−0.36 to 0.04) |
| Infant Risk Factors | |||
| General health | |||
| Good / Fair v. Excellent / Very Good | −0.73 (−1.20 to −0.26) | −0.32 (−0.69 to 0.04) | −0.11 (−0.38 to 0.16) |
| Feeding type at 6-months of age | |||
| Any breastfeeding v. No breastfeeding | −0.15 (−0.37 to 0.07) | −0.17 (−0.37 to 0.03) | −0.02 (−0.17 to 0.13) |
| Introduction of solid foods | |||
| < 4 months v. ≥ 4 months | −0.05 (−0.35 to 0.24) | −0.39 (−0.67 to −0.11) | −0.22 (−0.42 to −0.01) |
| Child TV / Video viewing (hrs/wk) | −0.07 (−0.16 to 0.02) | −0.11 (−0.18 to −0.04) | −0.09 (−0.15 to −0.02) |
| Any child care outside the home | |||
| Yes v. No | −0.04 (−0.26 to 0.18) | −0.18 (−0.37 to 0.02) | −0.18 (−0.32 to −0.04) |
Adjusted for maternal age, parity, and education; household income; and infant gender and race/ethnicity.
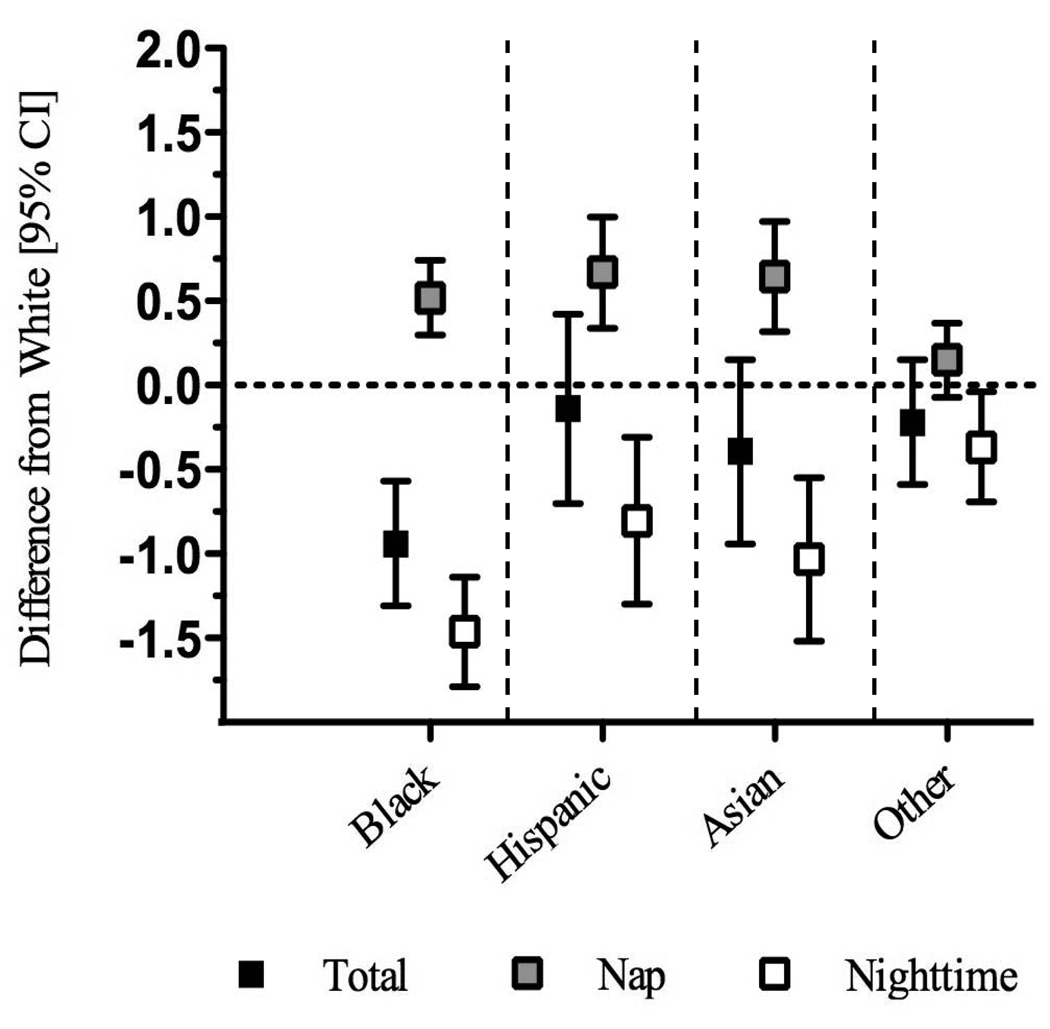
Independent of other risk factors of interest, we found that at age 2, black, Hispanic, and Asian infants slept 0.40 (Confidence Interval [CI]: −0.66 to −0.13), 0.82 (CI: −1.28 to −0.37), and 0.95 (CI:−1.35 to −0.54) fewer hours per day, respectively, than white infants. Black infants also slept fewer hours at age 6 months (0.94 fewer hours/day) than white children, whereas Hispanic and Asian infants slept less than white infants at older ages. In secondary analyses we found that black, Hispanic, and Asian infants slept more hours during daytime naps (0.52 more hours/day for blacks, 0.67 for Hispanics, and 0.64 for Asians) but fewer hours at night (1.46 fewer hours/day for blacks, −0.81 for Hispanics, and −1.03 for Asians) than white infants (Figure).
Figure.
Racial/Ethnic Differences in Infant Sleep Duration (Hours/Day) at Age 6 Months. Data from 1676 Project Viva Participants.
DISCUSSION
Our study identified several potential risk factors during the prenatal, infancy, and early childhood periods that are associated with infant sleep duration independent of sociodemographic characteristics. Shorter sleep duration was associated with maternal depression during pregnancy, introduction of solid foods prior to 4 months of age, infant TV/video viewing, and attendance at child care outside the home. Racial/ethnic minority children slept substantially less than their white counterparts in the first two years of life. At age 6 months, we also observed racial/ethnic differences in daytime nap and nighttime sleep duration. Whenever possible we examined longitudinal risk factors for sleep duration, but several of our infant risk factors were cross-sectional and therefore hold the potential for reverse causality (e.g., mothers whose infants are not sleeping well may be inclined to introduce solids earlier, and/or increase exposure to TV/video viewing). Our results, however, suggest that various risk factors, some potentially modifiable, are worthy of clinical consideration when addressing infant sleep duration.
Our finding that maternal antenatal depression is associated with shorter infant sleep duration is consistent with prior studies of maternal depression during pregnancy and infant sleep.15, 16 In the existing literature, as well in our analyses, maternal antenatal (rather than postpartum) depression has been found to be associated with negative impacts on infant sleep. In addition, this relationship to infant sleep supports the clinical relevance of monitoring perinatal maternal mood states. Although the mechanisms relating maternal prenatal mood disturbance and infant sleep have yet to be fully understood, it has been suggested that prenatal maternal anxiety and depression may lead to increased prenatal stress leading to elevated glucocorticoid secretion. In animal studies, elevated prenatal exposure to glucocorticoids has been shown to disrupt the circadian activity of the fetus' hypothalamic pituitary adrenal axis. Thus, it is possible that exposure to elevated prenatal exposure to glucocorticoids could disrupt infants’ sleep patterns.16 It is also possible that maternal depression can influence maternal behavior, which in turn can impact infant sleep patterns.
In the early infancy period, we found that introduction of solid foods prior to 4 months of age was associated with shorter sleep duration at ages 1 and 2 years. Although the American Academy of Pediatrics (AAP) recommends that solid foods be introduced to healthy children no earlier than 4 to 6 months of age, previous studies have found that parents believe solids help children sleep better at night, and it is one reason why they introduce solids before 4 months of age.17 To our knowledge, there are no published studies of timing of introduction of solids and infant sleep duration. Although previous studies have found that breastfeeding is associated with frequent night waking and shorter sleep duration during infancy, 18–21 we did not find an association between breastfeeding and infant sleep duration.
Consistent with previous studies of older children,9, 22, 23 we found that TV/video viewing was associated with shorter sleep duration at 1 and 2 years of age. Although the effect estimates of these associations are small, if the relationship between TV viewing and sleep loss track throughout childhood, the observed small magnitudes of effect could be additive throughout the child’s lifecourse. In this context of potential chronic sleep loss, even risk factors during infancy may be clinically relevant and merit awareness by clinicians. Numerous mechanisms have been proposed by which TV/video viewing may disturb children’s sleep including disruption of regular sleep schedules 9 and our findings support the AAP guidelines 24 of no TV viewing in infancy. We also observed a trend of shorter sleep duration among infants who attended child care outside of their home in the first two years of life. Child care outside of the home may present new challenges for infants, such as longer periods of parent-child separation that may influence their daily routine and sleep-wake schedules. It is also possible that parents might not be aware of the duration of naps during the day while at child care and could report fewer hours of total sleep duration. Infants might also have long naps while in child care which could shorten their nighttime sleep. Finally, we can not rule out the possibility of reverse causation, i.e. perhaps child care schedules required infants to be woken up earlier. To our knowledge, no previous studies have examined the relationship between child care attendance and infant sleep duration.
In unadjusted analyses, exposure to cigarette smoke, i.e. maternal smoking during pregnancy and at each time point measured in infancy, and total number of smoking household members, was associated with shorter sleep duration in infancy. However, in multivariable models adjusted for sociodemographic characteristics, the relationship between cigarette smoke exposure and sleep duration was attenuated. Previous studies have found an association of maternal prenatal smoking and smoking in early infancy with shorter sleep duration among infants. 11, 25 Our findings suggest that the observed association between smoking and sleep duration may be, in part, explained by parental sociodemographic characteristics.
We found substantial racial/ethnic differences in sleep duration in the first two years of life. Already by 6 months of age, black infants were sleeping almost 1 hour less than white children with significant differences in daytime nap and nighttime sleep durations. By age 2 years, sleep duration was shorter among black, Hispanic, and Asian children than among their white counterparts. Our findings persisted even after adjusting for potential confounders including sociodemographic characteristics. Our findings of racial/ethnic differences in daytime nap duration are consistent with those of older children.26, 27 In a study of 2- to 8-year-old children, Crosby et al.26 found that black children took daytime naps on more days per week and had shorter nighttime sleep duration than non-Hispanic white children. However, total weekly sleep duration was similar for the 2 racial groups. Among 2- to 5-year-old children, Lavigne et al. 27 found that racial/ethnic minority children napped longer and more often and spent less time sleeping at night than non-Hispanic white children, but also with comparable total sleep durations. The findings of our study differ in that less nighttime sleep among black children at 6 months of age was not balanced by longer daytime naps.
Viewed collectively with prior studies; our results suggest that racial/ethnic differences in sleep duration may extend to infancy. It is possible that the observed differences may reflect culturally distinct parental beliefs and practices regarding sleep. Previous studies have shown racial/ethnic differences in children’s bedtime routines, sleep location, and mothers’ level of concern about their child’s sleep.28 In addition, a study of 2- to 7-year-old children found African-Americans to have later bedtimes than whites with similar wake times, resulting in shorter sleep duration, independent of socioeconomic status. 29 Given the number of adverse health outcomes related to short sleep duration, including obesity and cardiovascular disease which are more prevalent in racial/ethnic minorities, our findings indicate a need to better understand the mechanisms relating race/ethnicity to sleep duration.
Our study had several strengths including the ability to examine a broad range of potential predictors and possible confounders in a large, pre-birth cohort of mother-infant pairs. Our study also had limitations. First, we measured sleep duration by mother’s report on the questionnaires as opposed to using an objective measure of sleep such as actigraphs or diaries. Although parental report has its limitations, a previous validation study among infants found that parental report of total sleep duration was significantly associated with infants having severe sleep problems, and was found to be a clinically useful measure to determine if a child needs subspecialty referral for sleep evaluation.30 In addition, potential bias exists for the reporting of sleep duration in our study. For example, antenatal depression could lead to postnatal depression and result in a systematic misreporting of infant sleep (~30% of our women who were depressed during pregnancy also reported being depressed at age 6 months and 1 year). Second, we did not measure infant sleep quality measures or other key sleep-related data, e.g. number of nighttime awakenings, sleep location/environment, bedtime routines, co-sleeping, crowding, or parental perceptions of sleep, all of which may be related to sleep duration. Third, although mothers in the study had diverse racial/ethnic backgrounds, their education and income levels were relatively high. Our results may not be generalizable to more socioeconomically disadvantaged populations. Finally, in any observational study it is possible that statistically significant associations may be surrogates for other risk factors and/or residual confounding may be present.
CONCLUSIONS
Our findings regarding maternal antenatal depression, early introduction of solid foods, TV/video viewing, and child care attendance are likely to be of importance to pediatricians and public health researchers interested in potential targets for intervention to improve infant sleep duration. Our study also suggests the need to better understand the factors leading to racial/ethnic differences in sleep duration and their impact on health outcomes.
Acknowledgments
This study was supported in part by grants from the U.S. National Institutes of Health (HD 34568, HL 64925, HL 68041). E.M. Taveras is supported in part by the Physician Faculty Scholars Program of the Robert Wood Johnson Foundation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
An abstract version of this manuscript was published as part of the proceedings of the 22nd Annual Meeting of the Associated Professional Sleep Societies on June 9, 2008 in Baltimore, MD.
The authors have no conflicts of interest to declare.
REFERENCES
- 1.Meltzer LJ, Mindell JA. Sleep and sleep disorders in children and adolescents. Psychiatr Clin North Am. 2006;29(4):1059–1076. doi: 10.1016/j.psc.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 2.Taveras EM, Rifas-Shiman SL, Oken E, Gunderson EP, Gillman MW. Short sleep duration in infancy and risk of childhood overweight. Arch Pediatr Adolesc Med. 2008;162(4):305–311. doi: 10.1001/archpedi.162.4.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zuckerman B, Stevenson J, Bailey V. Sleep problems in early childhood: continuities, predictive factors, and behavioral correlates. Pediatrics. 1987;80(5):664–671. [PubMed] [Google Scholar]
- 4.National Sleep Foundation. [Accessed May 11, 2009];Sleep in America Poll. http://www.sleepfoundation.org/site/c.huIXKjM0IxF/b.2417353/k.6764/Sleep_in_America_Polls.htm.
- 5.Kataria S, Swanson MS, Trevathan GE. Persistence of sleep disturbances in preschool children. J Pediatr. 1987;110(4):642–646. doi: 10.1016/s0022-3476(87)80571-1. [DOI] [PubMed] [Google Scholar]
- 6.Pollock JI. Night-waking at five years of age: predictors and prognosis. J Child Psychol Psychiatry. 1994;35(4):699–708. doi: 10.1111/j.1469-7610.1994.tb01215.x. [DOI] [PubMed] [Google Scholar]
- 7.Baird J, Hill CM, Kendrick T, Inskip HM. Infant sleep disturbance is associated with preconceptional psychological distress: findings from the Southampton Women's Survey. Sleep. 2009;32(4):566–568. doi: 10.1093/sleep/32.4.566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pesonen AK, Raikkonen K, Matthews K, et al. Prenatal origins of poor sleep in children. Sleep. 2009;32(8):1086–1092. doi: 10.1093/sleep/32.8.1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thompson DA, Christakis DA. The association between television viewing and irregular sleep schedules among children less than 3 years of age. Pediatrics. 2005;116(4):851–856. doi: 10.1542/peds.2004-2788. [DOI] [PubMed] [Google Scholar]
- 10.Bayer JK, Hiscock H, Hampton A, Wake M. Sleep problems in young infants and maternal mental and physical health. J Paediatr Child Health. 2007;43(1–2):66–73. doi: 10.1111/j.1440-1754.2007.01005.x. [DOI] [PubMed] [Google Scholar]
- 11.Mennella JA, Yourshaw LM, Morgan LK. Breastfeeding and smoking: short-term effects on infant feeding and sleep. Pediatrics. 2007;120(3):497–502. doi: 10.1542/peds.2007-0488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gillman MW, Rich-Edwards JW, Rifas-Shiman SL, Lieberman ES, Kleinman KP, Lipshultz SE. Maternal age and other predictors of newborn blood pressure. J Pediatr. 2004;144(2):240–245. doi: 10.1016/j.jpeds.2003.10.064. [DOI] [PubMed] [Google Scholar]
- 13.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. The British Journal of Psychiatry. 1987;150(6):782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 14.Oken E, Kleinman KP, Rich-Edwards JW, Gillman MW. A nearly continuous measure of birth weight for gestational age using a United States national reference. BMC Pediatr. 2003;3:6. doi: 10.1186/1471-2431-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Field T, Diego M, Hernandez-Reif M, Figueiredo B, Schanberg S, Kuhn C. Sleep disturbances in depressed pregnant women and their newborns. Infant Behav Dev. 2007;30(1):127–133. doi: 10.1016/j.infbeh.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 16.O'Connor TG, Caprariello P, Blackmore ER, Gregory AM, Glover V, Fleming P. Prenatal mood disturbance predicts sleep problems in infancy and toddlerhood. Early Hum Dev. 2007;83(7):451–458. doi: 10.1016/j.earlhumdev.2006.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Crocetti M, Dudas R, Krugman S. Parental beliefs and practices regarding early introduction of solid foods to their children. Clin Pediatr (Phila) 2004;43(6):541–547. doi: 10.1177/000992280404300606. [DOI] [PubMed] [Google Scholar]
- 18.DeLeon CW, Karraker KH. Intrinsic and extrinsic factors associated with night waking in 9-month-old infants. Infant Behav Dev. 2007;30(4):596–605. doi: 10.1016/j.infbeh.2007.03.009. [DOI] [PubMed] [Google Scholar]
- 19.Anuntaseree W, Mo-suwan L, Vasiknanonte P, Kuasirikul S, Ma-a-lee A, Choprapawan C. Night waking in Thai infants at 3 months of age: association between parental practices and infant sleep. Sleep Med. 2008;9(5):564–571. doi: 10.1016/j.sleep.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 20.Burnham MM, Goodlin-Jones BL, Gaylor EE, Anders TF. Nighttime sleep-wake patterns and self-soothing from birth to one year of age: a longitudinal intervention study. J Child Psychol Psychiatry. 2002;43(6):713–725. doi: 10.1111/1469-7610.00076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ball HL. Breastfeeding, bed-sharing, and infant sleep. Birth. 2003;30(3):181–188. doi: 10.1046/j.1523-536x.2003.00243.x. [DOI] [PubMed] [Google Scholar]
- 22.E. Juulia P, Marjo P, Mira R, Satu V, Anja Riitta L. TV exposure associated with sleep disturbances in 5- to 6-year-old children. Journal of Sleep Research. 2006;15(2):154–161. doi: 10.1111/j.1365-2869.2006.00525.x. [DOI] [PubMed] [Google Scholar]
- 23.Owens J, Maxim R, McGuinn M, Nobile C, Msall M, Alario A. Television-viewing habits and sleep disturbance in school children. Pediatrics. 1999;104(3):e27. doi: 10.1542/peds.104.3.e27. [DOI] [PubMed] [Google Scholar]
- 24.American Academy of Pediatrics, Committee on Public Education. Children, adolescents, and television. Pediatrics. 2001;107(2):423–426. doi: 10.1542/peds.107.2.423. [DOI] [PubMed] [Google Scholar]
- 25.Stephan-Blanchard E, Telliez F, Leke A, et al. The influence of in utero exposure to smoking on sleep patterns in preterm neonates. Sleep. 2008;31(12):1683–1689. doi: 10.1093/sleep/31.12.1683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Crosby B, LeBourgeois MK, Harsh J. Racial differences in reported napping and nocturnal sleep in 2- to 8-year-old children. Pediatrics. 2005;115(1 Suppl):225–232. doi: 10.1542/peds.2004-0815D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lavigne JV, Arend R, Rosenbaum D, et al. Sleep and behavior problems among preschoolers. J Dev Behav Pediatr. 1999;20(3):164–169. doi: 10.1097/00004703-199906000-00005. [DOI] [PubMed] [Google Scholar]
- 28.Milan S, Snow S, Belay S. The context of preschool children's sleep: racial/ethnic ifferences in sleep locations, routines, and concerns. J Fam Psychol. 2007;21(1):20–28. doi: 10.1037/0893-3200.21.1.20. [DOI] [PubMed] [Google Scholar]
- 29.McLaughlin Crabtree V, Beal Korhonen J, Montgomery-Downs HE, Faye Jones V, O'Brien LM, Gozal D. Cultural influences on the bedtime behaviors of young children. Sleep Med. 2005;6(4):319–324. doi: 10.1016/j.sleep.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 30.Sadeh A. A brief screening questionnaire for infant sleep problems: validation and findings for an Internet sample. Pediatrics. 2004;113(6):e570–e577. doi: 10.1542/peds.113.6.e570. [DOI] [PubMed] [Google Scholar]