Abstract
Purpose
The purpose of the study was to assess the validity of surgical interference with elastic nailing in treating pediatric femur fractures in comparison with the traditional treatment method—hip spica casting.
Methods
Sixteen consecutive femur fractures in children 5–15 years of age were recruited prospectively over 13 months. An equal number of age-matched children treated by spica casting were recruited retrospectively. Subtrochanteric, supracondylar femur fractures were excluded.
Results
Fracture union occurred earlier in the surgical group (6 weeks) than in the spica group (8 weeks) (P = 0.001). Spica casting caused higher coronal plane angulation (P = 0.001), higher rotational malalignment (P < 0.001), higher limb length discrepancy at 1-year follow-up (P < 0.001), longer duration of immobilization (P < 0.001), later full weight-bearing (P < 0.001), and greater absence from school (P < 0.001). Flynn outcome scores were better with titanium elastic nailing than with hip spica casting.
Conclusion
Titanium elastic nailing led to better outcomes compared to hip spica casting in terms of earlier union, lower rates of malunion, shorter rehabilitation milestones, and better functional outcome scores.
Keywords: Titanium elastic nailing, Pediatric femur fracture, Hip spica casting
Introduction
Femoral shaft fractures are among the most common major pediatric injuries treated by orthopedic surgeons [1] and result in high direct and indirect medical costs [2]. The treatment of such fractures has ranged from closed reduction with hip spica casting with or without traction to surgical stabilization with intramedullary devices, plates and screws, and external fixators [3–6].
While spica casting is effective for most children less than 6 years of age and the skeletally mature teenager is best managed with an antegrade interlocked intramedullary nail, the best treatment for children between 6 and 16 years of age is a matter of much debate [3–6].
Traditionally, this age group had been managed by spica casting after a period of traction. However, this method of treatment is fraught with many complications and, in addition, causes psychological, social, educational, and economic difficulties [7].
Over the past two decades, the advantages of fixation and early mobilization have been increasingly recognized [5, 8]. These surgical methods included external fixation, plating, and solid intramedullary nailing. Though the long-term results of the majority of children treated by these methods have been excellent, the risk of certain significant complications remain. A search for a solution to these intricacies led to the development of the elastic stable intramedullary nail in Nancy, France, by Metaizeau, Prévot, Ligier, and others in the 1980s. Thereafter, these elastic stable intramedullary nails (ESINs) have been refined in many ways.
The present study attempts to validate the use of one of the recent advances in the treatment of pediatric femur fractures, i.e., titanium elastic nailing (TEN). Though there are recent studies describing the outcome of treatment with TEN and complications associated with the treatment, there are few studies comparing the flexible intramedullary nailing with the common treatment modality, i.e., hip spica casting. Also, the usefulness of such a change of trend to operative treatment of pediatric femoral fractures in developing countries like India is not known. The purpose of this study is to compare the outcome of fractures treated by this relatively new method, i.e., TEN, with the conservative treatment method, i.e., hip spica casting.
Patients and methods
The study was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki and was approved by the Ethics Committee of our institution. Sixteen consecutive children of ages 5 to 15 years with closed or Gustilo Anderson type I compound fractures of the femoral shaft presenting to the Emergency Department of our institute between January 2008 and February 2009 were recruited for elastic nailing. They underwent retrograde elastic nailing with a pair of equal-sized titanium nails. An equal number of age-matched (within 2 years) children with similar inclusion criteria treated with hip spica casting were randomly selected retrospectively from hospital records and the patients were reviewed (Spica group). Segmental, Winquist type III and IV comminuted and pathological fractures were excluded from both groups. The standard method for retrograde elastic nailing of the femur [8] was used. The distal ends of the nails were not bent and were allowed to lie flush with the metaphyseal flare (Fig. 1). Stable fracture fixations underwent external support with plaster-of-Paris thigh corset, while fixations with doubtful stability were put on a walking long-leg cast until 1 month postoperatively. Quadriceps strengthening exercises and non-weight-bearing with axillary crutches were started immediate postoperatively when tolerated. Partial weight-bearing was started at around 4 weeks and progressed to full weight-bearing after 2 weeks.
Fig. 1.
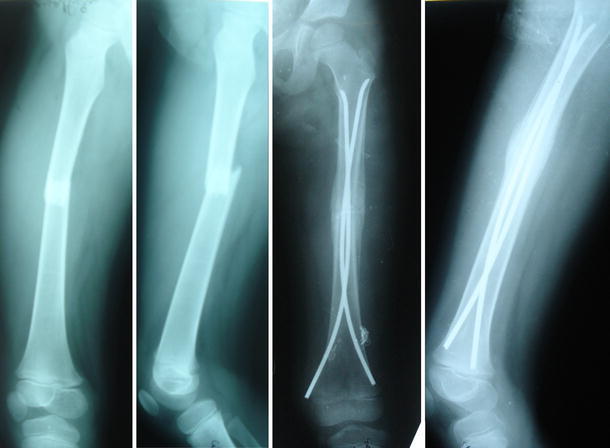
Preoperative and 2 months postoperative radiographs of a 6-year-old child showing good union
In the retrospective group, one-and-half hip spica was applied under general anesthesia, with the hips at 20 to 30° of flexion and the limb in 10°–15° external rotation under fluoroscopy. Spica was continued until union. Full weight-bearing was started 1–2 weeks following spica removal.
Data collected included details of the patient (age, gender), description of the fracture (type, location, pattern), surgery (open/closed), presence of fracture angulation or rotational malalignment, details of fracture union and rehabilitation milestones (non-weight-bearing, partial and full weight-bearing, return to school), and the presence of complications.
Measurements of angulation in the sagittal and coronal planes were done on anteroposterior and lateral radiographs immediately following surgery and during subsequent visits. Rotational malalignment was assessed by comparison of the available rotations of the hip with the normal side. Fracture union was defined as the ability to fully bear weight on the limb without pain in the presence of bridging callus in at least three cortices. Major complications were defined as those leading to unscheduled operative treatment or malunion, delayed union, or nonunion. Delayed union was defined as the persistence of bone pain and tenderness 3 months after the fracture without complete radiological union. Nonunion was defined as the absence of osseous union more than 6 months after the injury. Angular malalignment was defined as an angulation of >10° in the coronal plane or >15° in the sagittal plane [9]. Rotational malalignment was termed ‘excessive’ if it was more than 10°. Minor complications were defined as those that did not require operative treatment and would not cause future disability. The details of minor complications were not available for the retrospective hip spica group. Limb length was measured clinically by the tape method. Final outcome was graded excellent, satisfactory, or poor based on criteria described by Flynn et al. [5].
Nonparametric unpaired Student’s t test and test of proportions were used for comparison. A P value < 0.05 was considered as significant.
Results
Among the 16 patients managed with titanium elastic nails, there were 12 boys and 4 girls. The mean age was 10 years and the median body weight was 25.5 kg (range 15–47 kg) (Table 1).
Table 1.
Clinical and radiological details of patients treated with titanium elastic nailing (TEN)
| Subject no. | Age/sex | Site of fracture | Pattern of fracture | Coronal angulation | Sagittal angulation | Malrotation | LLD | Flynn score | Complication |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 8/M | Middle 1/3 | Short oblique | 2° varus | 0° | 0° | 0.0 | Poor | Postoperative fall , fracture angulation, and implant exposure |
| 2 | 12/F | Prox-mid jn | Transverse | 10° varus | 10° anterior | 10° ER | 0.0 | Satisfactory | Asymptomatic nail migration |
| 3 | 14/M | Middle 1/3 | Transverse | 0° | 4° anterior | 0° | 0.0 | Excellent | Nil |
| 4 | 8/M | Middle 1/3 | Transverse | 5° varus | 0° | 0° | 1.0 | Excellent | Nil |
| 5 | 13/M | Mid-dist jn | Winquist II | 4° valgus | 5° anterior | 10° ER | 0.0 | Excellent | Nil |
| 6 | 6/F | Middle 1/3 | Transverse | 0° | 2° anterior | 0° | 0.5 | Excellent | Nil |
| 7 | 6/M | Middle 1/3 | Spiral | 0° | 5° anterior | 10° IR | 0.5 | Excellent | Nil |
| 8 | 10/M | Middle 1/3 | Short oblique | 10° varus | 24° anterior | 10° ER | −1.0 | Poor | Fracture angulation following delayed fixation |
| 9 | 8/M | Middle 1/3 | Short oblique | 5° varus | 0° | 10° ER | 1.0 | Excellent | Nil |
| 10 | 5/M | Mid-dist jn | Short oblique | 0° | 5° anterior | 10° ER | 1.0 | Excellent | Nil |
| 11 | 15/M | Middle 1/3 | Winquist II | 0° | 5° anterior | 10° ER | 0.5 | Excellent | Nil |
| 12 | 12/M | Prox-mid jn | Long oblique | 0° | 4° anterior | 0° | 1.0 | Excellent | Nil |
| 13 | 8/F | Middle 1/3 | Short oblique | 4° varus | 5° anterior | 0° | 1.0 | Excellent | Nil |
| 14 | 15/M | Prox-mid jn | Short oblique | 2° varus | 4° posterior | 10° ER | 0.5 | Excellent | Nil |
| 15 | 12/M | Middle 1/3 | Short oblique | 4° varus | 15° anterior | 0° | 0.0 | Poor | Subclinical 15° anterior angulation |
| 16 | 10/F | Prox-mid jn | Long oblique | 5° varus | 4° anterior | 10° ER | 1.0 | Excellent | Nil |
ER external rotation; IR internal rotation; LLD limb length discrepancy in cm
Of the sixteen patients in the spica group, there were 13 boys and three girls, with a mean age of 9.25 years. The distribution of gender, site of fracture, type of fracture (open/closed), mode of injury, and pattern of fracture were not significantly different between the groups as tested by test of proportions. In the surgical group, follow-up ranged from 12 to 18 months. All patients in the spica group had a follow-up of more than 1 year.
There was no significant difference in the delay of definitive treatment between the nailing group (range 4–16 days; mean 8.25 days) and the spica group (range 1–20 days; mean 6.62 days) (P = 0.295).
The duration of hospital stay was significantly higher in the elastic nailing group (range 12–41 days; mean 21.19 days) than in the spica group (range 5–36 days; mean 11.62 days) (P = 0.002).
In the nailing group, angulation in the coronal plane ranged from 10° varus to 4° valgus, while that in the sagittal plane ranged from 24° anterior (major complication; Fig. 2) to 4° posterior angulation. Angulation in the coronal plane (varus or valgus) was significantly higher in the spica group (mean 9.6°) than in the nailing group (mean 3.2°) (P = 0.001). However, such a difference was not noted with sagittal plane angulation (Table 2). The lack of difference is likely to be due to an extreme value (24° anterior angulation) in one patient in the surgical group.
Fig. 2.
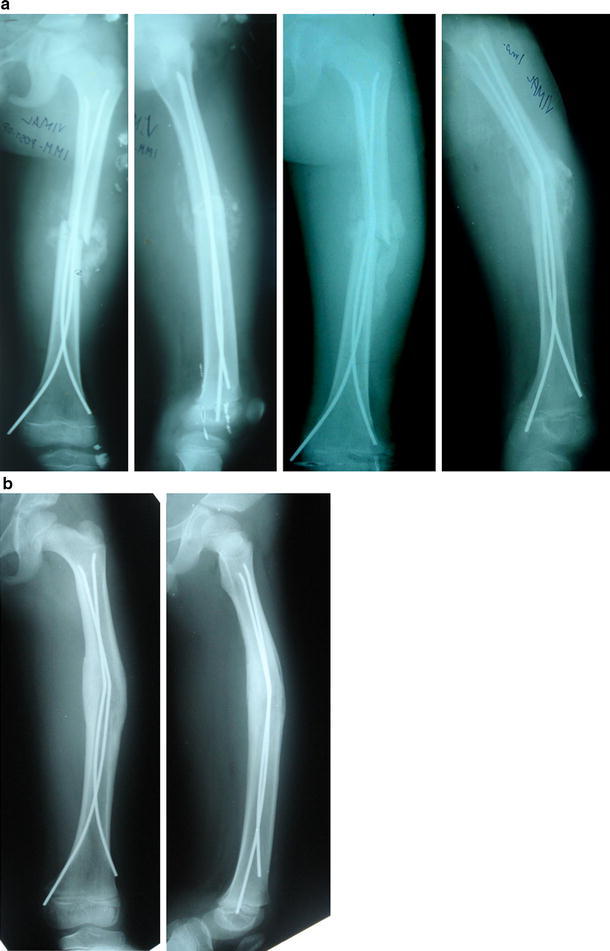
a Immediate postoperative and 4 weeks postoperative radiographs of a 10-year-old child who underwent closed elastic nailing at 16 days post-trauma. The child developed angulation of the fracture due to the deforming force of the strong callus towards the preoperative shortened position. b One year follow-up radiograph
Table 2.
Comparison of the outcomes of TEN and spica casting
| Parameter | Group | Range | Mean | Standard deviation | Significance (P value, two-tailed) |
|---|---|---|---|---|---|
| Coronal plane angulation (°) | TEN | 10° varus to 4° valgus | 3.19 | 3.351 | 0.001 |
| Spica | 22° varus to 8° valgus | 9.57 | 5.612 | ||
| Sagittal plane angulation (°) | TEN | 24° anterior to 4° posterior | 5.75 | 6.137 | 0.349 |
| Spica | 20° anterior to 8° posterior | 7.79 | 5.466 | ||
| Rotational malalignment (°) | TEN | 10° IR to 10° ER | 5.62 | 5.123 | 0.000 |
| Spica | 25° IR to 20° ER | 14.69 | 5.907 | ||
| LLD at 1 year follow-up (cm) | TEN | −1 cm to +1 cm | 0.56 | 0.443 | 0.000 |
| Spica | −0.5 cm to −2 cm | 1.25 | 0.408 | ||
| Union (weeks) | TEN | 5–8 weeks | 6.47 | 0.990 | 0.001 |
| Spica | 6–12 weeks | 8.25 | 1.483 | ||
| Non-weight-bearing (weeks) | TEN | 4–8 weeks | 5.33 | 1.447 | 0.000 |
| Spica | 6–9 weeks | 7.38 | 1.025 | ||
| Full weight-bearing (weeks) | TEN | 5–8 weeks | 6.87 | 1.125 | 0.000 |
| Spica | 8–12 weeks | 10.00 | 1.155 | ||
| Schooling lost (weeks) | TEN | 5–12 weeks | 7.13 | 1.767 | 0.000 |
| Spica | 8–14 weeks | 11.44 | 1.632 |
Rotational malalignment ranged from 10° internal rotation to 10° external rotation in the surgical group and from 25° internal rotation to 20° external rotation in the spica group. The presence of rotational malalignment (internal or external rotation) was significantly higher in the spica group (mean 14.69°) than in the nailing group (mean 5.62°) (P < 0.001) (Table 2). Parents complained of in-toe gait in 7 of 16 children (43.75%) in the spica group, while none of the children had in-toeing in the surgical group.
At 1 year follow-up, the limb length discrepancy (LLD) in the surgical group ranged from 1 cm shortening (in the child with angulation) to 1 cm lengthening. In the spica group, LLD at 1 year ranged from 0.5 cm shortening to 2 cm shortening. Length inequality (lengthening or shortening) at 1 year was significantly higher in the spica group (median = 1.25 cm) than in the surgical group (median = 0.56 cm) (P < 0.001) (Table 2). Parents noticed length inequality in 8 of 16 children (50%) in the spica group and in none of the children in the nailing group.
Union occurred at a median of 6.47 weeks (range 5–8 weeks) in the nailing group and at a median of 8.25 weeks (range 6–12 weeks) in the spica group. It was significantly earlier in the nailing group (P = 0.001) (Table 2).
The duration of non-weight-bearing (P < 0.001), postoperative duration at full weight-bearing (P < 0.001), and the duration of schooling lost (P < 0.001) were all significantly higher in the spica group in comparison with the TEN group (Table 2).
Two patients (12.5%) had major complications. The first patient of the series who had corkscrewing of the nails sustained a fall postoperatively and angulated the fracture. He underwent closed reduction and spica casting with nails in situ. The other major complication occurred in a 10-year-old child, who had an oblique fracture of the midshaft femur and underwent closed elastic nailing at 16 days post-trauma in the presence of fracture callus. Follow-up radiographs revealed fracture angulation (Fig. 2). The deforming force of the strong callus towards the preoperative shortened position in an oblique fracture had resulted in fracture angulation.
There were no cases of skin ‘irritation’ due to nails. There was no incidence of infection, either superficial or deep. In the spica group, 12 children (75%) had major complications (‘excessive’ rotational malalignment in 11 and redo closed reduction for unacceptable angulation in one). The proportion of patients with major complications was significantly higher in the spica group (P < 0.001).
In the surgical group, the Flynn score was ‘excellent’ in 12 (75%), ‘satisfactory’ in 1 (6.2%), and ‘poor’ in 3 (18.8%), while the scores for the spica group were ‘excellent’ in 1 (6.2%), ‘satisfactory’ in 2 (12.5%), and ‘poor’ in 13 (81.3%).
Discussion
Femoral fractures in children have been traditionally treated with either early spica casting or traction followed by spica casting. Though this is an accepted standard of care in younger children, such treatment in older children has commonly resulted in complications like malunion, joint stiffness, and delay in functional recovery [10–14]. The psychological, social, educational, and economic difficulties resulting from such treatment has also been of much concern recently [5, 7, 15].
An ideal device for treating pediatric femur fractures would be a simple load-sharing internal splint, allowing the mobilization and maintenance of alignment until bridging callus forms. The device would exploit the rapid healing and ability to remodel without risking the physes or blood supply to the femoral head [5]. TEN fulfills these qualities.
The duration of hospital stay in the present study was significantly higher in the surgical group than in the control group. This is in contrast to other reports [4, 16–18], most of which have reported shorter hospital stay with TEN. This difference was because the surgical patients were discharged only after suture removal in order to have a closer follow-up for the presence of early postoperative complications, if any. The spica patients were usually discharged a day or two following spica casting after observation for the presence of plaster-of-Paris-related complications. The longer hospital stay in the surgical group was, however, not related to the development of any postoperative complications.
The present study demonstrates higher coronal angulation and rotational malalignment in patients treated with spica casts. High incidence of loss of reduction and malunion in children treated with spica casting has been reported earlier [4, 11, 19]. However, no literature exists comparing the rotational alignment of fractures treated by the two modalities.
Angulation following titanium elastic nails have been reported by other authors and followed the use of mismatched nail diameters or comminution at the fracture site [6, 8]. Both cases of fracture angulation in the present study occurred early in the series and could be avoided by strictly adhering to the principles of the procedure.
Children in the spica casting group had a significantly higher limb length inequality than those treated with elastic nailing at 1 year postoperatively.
High risk of shortening with spica casting has also been reported by other authors [10, 19, 20]. Flynn et al. [4] reported a higher incidence of shortening and unacceptable angulation with spica casting than with elastic nailing.
Earlier union and return to weight-bearing and school was observed in the surgical group compared to the spica casting group. This could be a result of greater contact of the fracture surfaces and anatomical reduction in the operated patients. Earlier fracture union and earlier mobilization in turn led to earlier return to the normal routine in these patients. Such earlier recovery milestones have also been shown by Greisberg et al. [17] and Flynn et al. [4].
The Flynn scores were better in the surgical group than in the spica group. The most common cause of poor score in the control group was ‘excessive’ rotational malalignment. Such comparison of the final outcome score has not been done in other studies.
The study has certain limitations. As this was a single-center study, the results should be generalized with caution. Other surgeons may find different results or complication rates with the two treatment methods. We did not attempt to estimate the cost of treatment in the two groups and, hence, the difference in the cost of treatment. As with any other new procedure, TEN has a steep learning curve and a small sample size in such a situation could lead to erroneously high complication rates. The study attempts to assess the short-term outcome of the treatment methods. We did not attempt to determine the long-term results of treatment.
In conclusion, the present study supports the treatment of femoral shaft fractures in children aged 5–15 years with TEN, as it hastens fracture union, reduces the rate of malunion and amount of shortening, and allows earlier rehabilitation and return to school.
References
- 1.Flynn JM, Skaggs D, Sponseller PD, Ganley TJ, Kay RM, Leitch K. The operative management of pediatric fractures of the lower extremity. J Bone Joint Surg Am. 2002;84:2288–2300. doi: 10.1302/0301-620X.84B1.11972. [DOI] [Google Scholar]
- 2.Hinton RY, Lincoln A, Crockett MM, Sponseller P, Smith G. Fractures of the femoral shaft in children. Incidence, mechanisms, and sociodemographic risk factors. J Bone Joint Surg Am. 1999;81(4):500–509. doi: 10.2106/00004623-199904000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Khazzam M, Tassone C, Liu XC, Lyon R, Freeto B, Schwab J, Thometz J. Use of flexible intramedullary nail fixation in treating femur fractures in children. Am J Orthop. 2009;38(3):E49–E55. [PubMed] [Google Scholar]
- 4.Flynn JM, Luedtke LM, Ganley TJ, Dawson J, Davidson RS, Dormans JP, Ecker ML, Gregg JR, Horn BD, Drummond DS. Comparison of titanium elastic nails with traction and a spica cast to treat femoral fractures in children. J Bone Joint Surg Am. 2004;86:770–777. doi: 10.2106/00004623-200404000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Flynn JM, Hresko T, Reynolds RA, Blasier RD, Davidson R, Kasser J. Titanium elastic nails for pediatric femur fractures: a multicenter study of early results with analysis of complications. J Pediatr Orthop. 2001;21:4–8. doi: 10.1097/01241398-200101000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Saikia KC, Bhuyan SK, Bhattacharya TD, Saikia SP. Titanium elastic nailing in femoral diaphyseal fractures of children in 6–16 years of age. Indian J Orthop. 2007;41:381–385. doi: 10.4103/0019-5413.33876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hedin H. Surgical treatment of femoral fractures in children. Comparison between external fixation and elastic intramedullary nails: a review. Acta Orthop Scand. 2004;75:231–240. doi: 10.1080/00016470410001132. [DOI] [PubMed] [Google Scholar]
- 8.Narayanan UG, Hyman JE, Wainwright AM, Rang M, Alman BA. Complications of elastic stable intramedullary nail fixation of pediatric femoral fractures, and how to avoid them. J Pediatr Orthop. 2004;24:363–369. doi: 10.1097/01241398-200407000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Wall EJ, Jain V, Vora V, Mehlman CT, Crawford AH. Complications of titanium and stainless steel elastic nail fixation of pediatric femoral fractures. J Bone Joint Surg Am. 2008;90(6):1305–1313. doi: 10.2106/JBJS.G.00328. [DOI] [PubMed] [Google Scholar]
- 10.Martinez AG, Carroll NC, Sarwark JF, Dias LS, Kelikian AS, Sisson GA., Jr Femoral shaft fractures in children treated with early spica cast. J Pediatr Orthop. 1991;11:712–716. doi: 10.1097/01241398-199111000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Thompson JD, Buehler KC, Sponseller PD, Gray DW, Black BE, Buckley SL, Griffin PP. Shortening in femoral shaft fractures in children treated with spica cast. Clin Orthop Relat Res. 1997;338:74–78. doi: 10.1097/00003086-199705000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Singh R, Sharma SC, Magu NK, Singla A. Titanium elastic nailing in pediatric femoral diaphyseal fractures. Indian J Orthop. 2006;40:29–34. doi: 10.4103/0019-5413.34071. [DOI] [Google Scholar]
- 13.Ligier JN, Metaizeau JP, Prévot J, Lascombes P. Elastic stable intramedullary nailing of femoral shaft fractures in children. J Bone Joint Surg Br. 1988;70:74–77. doi: 10.1302/0301-620X.70B1.3339064. [DOI] [PubMed] [Google Scholar]
- 14.Galpin RD, Willis RB, Sabano N. Intramedullary nailing of pediatric femoral fractures. J Pediatr Orthop. 1994;14:184–189. doi: 10.1097/01241398-199403000-00010. [DOI] [PubMed] [Google Scholar]
- 15.Kirby RM, Winquist RA, Hansen ST., Jr Femoral shaft fractures in adolescents: a comparison between traction plus cast treatment and closed intramedullary nailing. J Pediatr Orthop. 1981;1:193–197. doi: 10.1097/01241398-198110000-00010. [DOI] [PubMed] [Google Scholar]
- 16.Reeves RB, Ballard RI, Hughes JL. Internal fixation versus traction and casting of adolescent femoral shaft fractures. J Pediatr Orthop. 1990;10:592–595. doi: 10.1097/01241398-199009000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Greisberg J, Bliss MJ, Eberson CP, Solga P, d’Amato C. Social and economic benefits of flexible intramedullary nails in the treatment of pediatric femoral shaft fractures. Orthopedics. 2002;25:1067–1070. doi: 10.3928/0147-7447-20021001-18. [DOI] [PubMed] [Google Scholar]
- 18.Herndon WA, Mahnken RF, Yngve DA, Sullivan JA. Management of femoral shaft fractures in the adolescent. J Pediatr Orthop. 1989;9:29–32. doi: 10.1097/01241398-198901000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Pollak AN, Cooperman DR, Thompson GH. Spica cast treatment of femoral shaft fractures in children—the prognostic value of the mechanism of injury. J Trauma. 1994;37:223–229. doi: 10.1097/00005373-199408000-00013. [DOI] [PubMed] [Google Scholar]
- 20.Lee SS, Mahar AT, Newton PO. Ender nail fixation of pediatric femur fractures: a biomechanical analysis. J Pediatr Orthop. 2001;21:442–445. [PubMed] [Google Scholar]


