Abstract
High survival rates have been reported for the uncemented CLS® Spotorno® stem up to 10 years. To confirm survival at longer followup we report the minimum 15-year (mean, 17 years; range, 15–20 years) for 257 hips using this stem. We retrospectively evaluated the clinical and radiographic results of all 326 patients (354 THAs) operated between 1985 and 1989. The patients had a mean age of 57 years using an uncemented grit-blasted, tapered titanium femoral stem. Eighty-six patients (89 hips) died and eight patients (eight hips) were lost to followup, leaving 240 patients (257 hips) for evaluation. The femoral component was revised in 35 hips: eight for infection, nine for periprosthetic fracture, one for traumatic loosening, and 17 for aseptic loosening. Survival of the stem was 88% at 17 years (95% confidence interval, 84%–92%), and survival with femoral revision for aseptic loosening as an end point was 94% (95% confidence interval, 91%–97%). The median Harris hip score at followup was 80 points. No thigh pain was reported. Small osteolytic lesions (< 1 cm2) were found in the proximal Gruen zones (1 or/and 7) in 28 hips (15%). No distal femoral osteolysis was found. The long-term survival with this type of femoral component remains high in the second decade.
Level of Evidence: Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
The early and midterm results of uncemented femoral components are frequently reported. Aseptic failures of contemporary uncemented stem designs within the first 10 years are uncommon, ranging from 0% to 8% [1, 15, 17, 35, 36, 50, 51]. Most revisions within the first decade are due to cup failure (migration, wear, and osteolysis) [1, 44, 47], dislocation, and infection. Equally encouraging are reports of stem performance in the second decade for both cemented and uncemented designs [9, 25, 38, 40, 41]. However, there are relatively few reports with more than 15 years of followup. A number of these reports, however, demonstrate high long-term survival rates ranging from 87% to 99% [13, 17, 18, 20, 27, 29, 31, 34–38, 40, 46, 49, 53].
Many of these studies [13, 17, 29, 37, 53] reviewed the long-term results with cobalt-chromium femoral components. Because proximal femoral resorption has been identified as one of the modes of mechanical failure after THA [6, 23], titanium alloy femoral components have been used in an attempt to enhance the transfer of stress to the proximal part of the femur, thereby potentially prolonging the life of the implant. The midterm survival of titanium femoral implants suggested high survival [1, 18, 20, 27, 31, 34] and severe stress shielding with osteolysis was found less frequently as compared to cobalt chrome stems [2, 4, 40, 49].
The purpose of this study was to determine (1) the survival of an uncemented titanium stem in primary THA; (2) the number of long-term revisions and the reasons; (3) the long-term Harris hip scores; and (4) the radiographic signs of loosening.
Materials and Methods
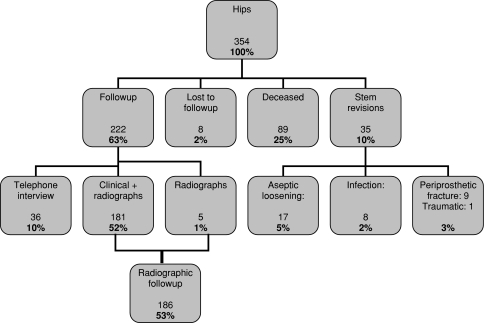
We retrospectively reviewed all 326 patients (354 hips) who had a THA with an uncemented, straight, collarless tapered titanium stem (CLS® Spotorno® stem, Zimmer Inc, Warsaw, IN)) (Fig. 1) performed between January 1985 and December 1989 [1]. Indications for this device were absence of severe femoral canal deformity and adequate bone stock for uncemented fixation using the index of Singh et al. [45] as described by Spotorno et al. [48]. The mean age of the patients was 57 years at the time of surgery (range, 13–81 years.) The minimum followup was 15 years (mean, 17 years; range, 15–20 years). During the followup period, 86 patients (89 hips) died and eight patients (eight hips) were lost to followup, leaving 257 of the 354 hips (72%) available for review (Fig. 2). Of those, 222 hips had clinical followup at a minimum of 15 years and 35 hips were revised (stem revision). At a minimum of 15 years’ followup, we had radiographs for 186 of the 354 hips (53%). In the 86 patients who died, the femoral prosthesis was in situ at the time of death. Patient demographics show a typical distribution of diagnoses leading to hip arthroplasty (Table 1). All 257 patients were seen in followup specifically for this study. All patients gave informed consent to participate in the study and the study was approved by our institutional university review board.
Fig. 1.

The photograph shows the uncemented straight titanium CLS® Spotorno® femoral component (Zimmer Inc) with proximal fins and a grit-blasted surface finish.
Fig. 2.
A flowchart illustrates the patient status at the latest visit 15 to 20 years postoperatively.
Table 1.
Patient demographics and diagnoses
| Demographics | All | Male | Female |
|---|---|---|---|
| Age (years)* | 57 (18–81) | 57 (13–81) | 57 (23–76) |
| Body mass index (kg/m2)* | 27 (19–40) | 27 (19–38) | 27 (20–40) |
| Number of hips | 354 (100%) | 178 (51%) | 176 (49%) |
| Diagnosis | |||
| Osteoarthrosis | 188 (53%) | ||
| Congenital dislocation of the hip | 85 (24%) | ||
| Avascular necrosis | 39 (11%) | ||
| Posttraumatic osteoarthritis | 21 (6%) | ||
| Rheumatoid arthritis | 6 (2%) | ||
| Neck fracture | 6 (2%) | ||
| Other | 10 (3%) | ||
| Previous osteotomies | 57 (16%) | ||
| Side | |||
| Right | 179 (51%) | ||
| Left | 175 (49%) | ||
* Values are expressed as medians, with ranges in parentheses.
The stem had a neck-shaft angle of 145° and was implanted using the press-fit technique described by Spotorno et al. [48]. This rectangular stem was wedge-shaped and tapered in all three planes with proximal, anterior, and posterior located ribs/flutes (Fig. 1). Secondary osseointegration is presumably achieved by osseous ongrowth to the grit-blasted implant surface. The implant was made of Ti6Al7Nb alloy (Protasul® 64; Zimmer Inc) with a microporous surface treatment (Ra = 4.4 μm). Of the 354 hips, 348 (99%) underwent acetabular reconstruction using smooth, uncemented, threaded cups: 222 hips (63%) received threaded, spherical, uncemented Mecron cups (Mecron GmbH, Berlin, Germany) and 126 hips (36%) received a threaded, conical, uncemented Weill ring (Zimmer Inc) [44]. Six hips (1%) received cemented cups (B. Braun Aesculap, Tuttlingen, Germany). In all hips, polyethylene bearing surfaces and 32-mm Biolox® ceramic heads (CeramTec, Plochingen, Germany) were used.
The procedures were performed by 23 surgeons at one center. We used either a modified Watson-Jones or the transgluteal lateral approach of Bauer et al. [5] with the patient in the supine position. The femoral canal was prepared using a series of chipped-tooth broaches of increasing size. No attempt was made to achieve cortical fixation; surgeons did not consider achieving cortical contact to be necessary to achieve stability with this implant; the surgeon relied on the feel of rotational and axial stability to determine fit. We regarded fixation as satisfactory when a series of moderate hammer blows did not change the final position of the femoral implant.
Postoperative partial weightbearing was encouraged for 6 weeks and then weightbearing as tolerated thereafter. No regular prophylaxis (irradiation or NSAIDs) for prevention of heterotopic ossification was given.
Patients were followed in regular intervals at 3 months, 6 months, 1 year and yearly thereafter. As this was a retrospective cohort study, preoperative Harris hip scores (HHS) were not available. Data were retrieved from a permanent continuous electronic database. Patients were contacted and invited for a followup visit at our center. At final followup, two of us (AWJ, PRA, neither a treating surgeon) determined the HHS for each patient/hip. Clinical assessment included limp, range of motion, and pain. Patients assessed the pain in the operated hip at the time of final followup using a visual analog scale (0–10). In addition, the pain component of the HHS was recorded [21].
The first postoperative and subsequent serial low centered pelvic radiographs and anteroposterior and lateral radiographs of the hip were examined by two independent experienced orthopaedic surgeons (HC, FUN) to determine stem alignment, subsidence, radiolucent lines, bone hypertrophy, osteolysis, stress shielding, pedestal formation at the stem tip, heterotopic ossifications, and femoral and acetabular loosening. The radiographic landmarks used for measuring subsidence were the greater trochanter and the shoulder of the prosthesis [16]. The threshold for subsidence was defined as > 2 mm. Varus or valgus stem malalignment was defined as deviation from the longitudinal femoral axis of more than 2°. Radiolucent lines were defined as radiopaque lines of > 1 mm adjacent to the implant and areas of osteolysis were defined as localized bone resorption and described according to Gruen et al. [19]. Bone hypertrophy was defined as thickening of the distal periprosthetic diaphyseal bone of more than 2 mm on anteroposterior radiographs compared to postoperative radiographs [39]. Osteolysis was defined as areas of localized bone resorption or endosteal erosion [52]. Stress shielding was defined according to the criteria of Engh et al. [12]. We considered only second-, third-, and fourth-degree stress shielding with resorption of cortical bone medially, anteriorly, or laterally as stress shielding; we defined rounding of the medial femoral neck as “calcar rounding.” Pedestal formation was defined as a shelf of endosteal new bone at the stem tip partially or completely bridging the intramedullary canal [32]. A femoral stem was regarded as loose if radiolucent lines of over 2 mm were present around the entire implant. Acetabular loosening was defined as continuous migration of greater than 5 mm or tilting of greater than 5° compared with baseline radiographs on anteroposterior views.
We used Kaplan-Meier survival analyses for all patients using revision of the stem for aseptic loosening and revision of the stem for any cause as end points. We used SAS® Version 8 for Windows® (SAS Institute Inc; Cary, NC) for data analysis.
Results
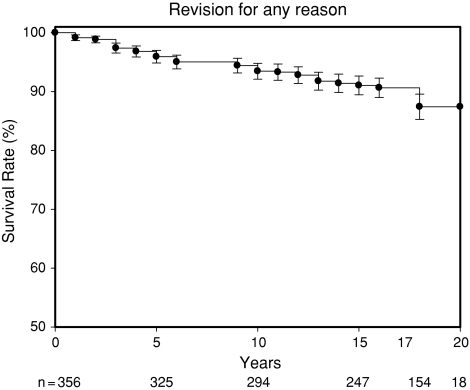
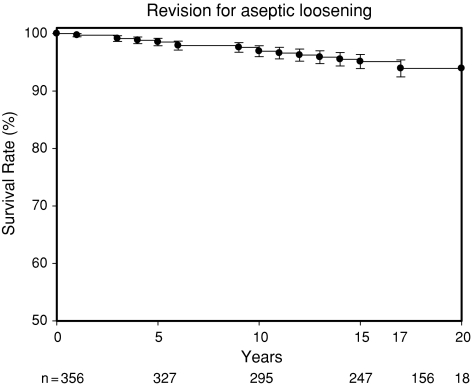
We found a survival of 88% (95% confidence interval [CI], 84%–92%) for all 354 hips after 17 years based on revision for any reason as end point (Fig. 3). Survival with femoral revision for aseptic loosening as end point was 94% (95% CI, 91%–97%) at 17 years (Fig. 4). The survival rate remained unchanged until Year 20. At the time of followup, no patient was awaiting stem revision. The Kaplan-Meier analysis of the acetabular components showed a survival for Mecron components of 49% (95% CI, 41%–57%) at 17 years. For Weill components, the survival rate was 75% (95% CI, 69%–87%) at 17 years.
Fig. 3.
The survival rate with all revisions of the femoral component as an end point is shown. Survival rates were at 96% at 5 years, 94% at 10 years, 91% at 15 years, and 88% at 17 years. n = number at risk.
Fig. 4.
The survival rate with revision for aseptic loosening of the femoral component as an end point is shown. Survival rates were at 99% at 5 years, 97% at 10 years, 95% at 15 years, and 94% at 17 years. n = number at risk.
Thirty-five stems (10%) were revised. Eight hips were revised for deep infection; nine stems were revised after trauma resulting in periprosthetic fracture and stem loosening. Until the time of trauma, there were no signs of stem loosening in these hips. Seventeen stems were revised for other causes. Twelve stems were revised for late aseptic loosening with progressive subsidence. In these hips, the stem was stable in the first decade without change in position and then suddenly subsided with onset of pain. In all 12 hips, the stem had been undersized at the time of surgery. In one additional hip, an intraoperative fracture of the proximal femur occurred and was not stabilized; the stem progressively subsided and was revised after 3 years. In three hips, the femoral component was revised at the time of cup revision in a different institution. The reason for femoral revision is unknown in these cases. One hip was revised for traumatic loosening with subsidence. One hundred twenty-one acetabular cups (33%; 91 Mecron and 30 Weill) had been revised before the most recent followup. The majority of the revisions were due to migration and aseptic loosening of the smooth-surface threaded components [3, 45].
At final followup, the median HHS of 222 hips with clinical followup was 80 points (range, 17–100 points (Table 2). The median Harris pain score was 42 of a possible 44 points for all hips. Only one hip had a Harris pain score of 10 or less. This patient was evaluated after a revision arthroplasty for cup loosening and suffered from other diseases not related to the operated hip. No patient reported thigh pain (Table 2).
Table 2.
Clinical results
| Clinical result | Value |
|---|---|
| Harris hip score (points)* | |
| All hips | 80 (17–100) |
| Stable cup | 79 (17–100) |
| Revised cup | 81 (28–100) |
| Charnley A (43/20%) | 92 (85–100) |
| Charnley B (91/43%) | 79 (17–100) |
| Charnley C (79/37%) | 75 (38–100) |
| VAS pain (number of hips) | |
| No pain | 143 (70%) |
| Slight pain | 28 (14%) |
| Mild pain | 21 (10%) |
| Moderate pain | 8 (4%) |
| Severe pain | 3 (1%) |
| Thigh pain | 0 (0%) |
* Values are expressed as medians, with ranges in parentheses; VAS = visual analog scale.
In the 186 hips evaluated radiographically at a minimum of 15 years, there was no evidence of (femoral) radiographic loosening at the time of followup in any case. The stem position was in a neutral position in 173 hips (94%), in a varus position in nine hips (5%), and in a valgus position in four hips (2%). The mean varus stem position was 3° (range, 2°–5°), and the mean valgus stem position was 3° (range, 2°–6°). Forty-four hips had heterotopic ossification (51%); only eight hips (4%) had Grade 3 heterotopic ossification and one (0.5%) had Grade 4. Four hips had reduced range of motion or pain (three Grade 3 and one Grade 4). We observed small osteolytic lesions (< 1 cm2, scoop lesions) in the proximal Gruen zones (1 or/and 7) in 28 hips (15%). Larger osteolysis (> 1 cm2) was seen in two hips (1%) extending into Gruen Zones 2 and/or 6. Early subsidence was seen in one stem (1%), which stabilized at 12 months without further clinical or radiographic signs of stem loosening at followup. We found mild rounding of the calcar in 165 hips. No instance of distal cortical hypertrophy was seen. We saw no obvious stress shielding (2°–4°) with atrophy of the proximal femur. Pedestal formation at the tip of the prosthesis was seen in 31 hips (17%) (Table 3).
Table 3.
Radiographic results
| Radiographic result | Number of hips |
|---|---|
| Stem alignment | |
| Neutral | 173 (94%) |
| Varus | 9 (5%) |
| Valgus | 4 (2%) |
| Osteolysis | |
| Zone 1 | 14 (8%) |
| Zone 2 | 1 (1%) |
| Zone 3 | 0 (0%) |
| Zone 4 | 0 (0%) |
| Zone 5 | 0 (0%) |
| Zone 6 | 2 (1%) |
| Zone 7 | 28 (15%) |
Discussion
The early and midterm results of uncemented femoral components have been frequently reported, with some reports with more than 15 years of followup demonstrating long-term survival rates over 95% [13, 17, 18, 20, 27, 29, 31, 34–38, 40, 46, 49, 53]. We report the minimum 15-year (mean, 17 years; range, 15–20 years) results of the CLS® Spotorno® stem in primary THA in terms of the long-term survival and revisions, the long-term clinical outcome, and the radiographic findings.
The main limitation of this study is related to the lack of preoperative Harris hip scores. We studied all patients treated with a CLS® Spotorno® stem in a given time frame of 5 years (1985–1989) and an electronic filing system assured all patients were included. During a minimum 15-year followup time, a considerable number of patients died (26%); therefore, the study cohort was reduced. However, with only eight patients (2%) lost to followup, a high clinical followup rate was achieved in our cohort [8] and 63% (n = 222) of the hips were followed for a minimum of 15 years. Thus, the results are reliable.
High survival rates have been reported in primary THA with the use of the CLS® Spotorno® uncemented femoral component [1, 4, 42, 43]. In all of these reports, this stem was associated with low rates of aseptic loosening. In our study, 17 stems have been revised for aseptic loosening; in most cases for late subsidence. In these hips, the stem was undersized during the primary surgery. The survival rate with revision for aseptic loosening/late subsidence as an end point was still 94% (range, 91%–97%) at 17 and 20 years. Only recently have long-term results exceeding 15 years become available for uncemented hip stems (Table 4), and high survival rates over 90% at 15 years [6, 11, 15, 17, 18, 22, 26, 27, 29, 31, 34, 35, 37, 38, 40, 46, 49, 53] have been reported. In some of these series, the implant is no longer in use or has undergone design changes over the years [17, 37, 38, 40, 50, 53]. The CLS® Spotorno® implant used in our study is still the same as in 1985 when we started the study and we have used it ever since for primary THA in younger patients. There are several hypotheses for the good long-term fixation of this stem. One of the most likely ones is the combination of a triple taper with a grit-blasted surface treatment allowing osseous integration of the titanium alloy [48].
Table 4.
Studies on uncemented hip stems with a mean followup of at least 15 years
| Implant* | Study | Year | Followup (years)† | Patient age (years)† | Number of hips | Loss to followup | Mean HHS (points) | Revisions | Revisions aseptic loosening | Survival rate (%) (all revisions/ aseptic loosening) |
|---|---|---|---|---|---|---|---|---|---|---|
| CLS Spotorno | Ihle et al. [22] | 2008 | 19 (17–21) | 52 (28–81) | 93 | 0 | 88 | 8 | —/96 | |
| Zweymüller | Reigstad et al. [40] | 2008 | 16 (15–18) | 52 (24–68) | 75 | 1 | 89 | 3 | 2 | 95/— |
| Grübl et al. [18] | 2006 | 15.5 (15–17) | 61 (22–84) | 208 | 11 | 89 | 3 | 0 | 98/100 | |
| Suckel et al. [49] | 2008 | 15 (15–17) | 67 (29–99) | 320 | 6 | 88 | 3 | 2 | 98/99 | |
| AML | Belmont et al. [6] | 2008 | 22 (20–25) | 55 (16–87) | 223 | 12 | 4 | 3 | 97.8/98.3 | |
| Taperloc | McLaughlin and Lee [31] | 2008 | 20 (18–23) | 50 (20–75) | 145 | 0 | 85 | 13 | 1 | 87/99 |
| McLaughlin and Lee [30] | 2006 | 15 | 54 (20–77) | 100 | 0 | 89 | 5 | 0 | 94/– | |
| 15 | 57 (20–82) | 109 | 0 | 89 | 6 | 1 | 95/– | |||
| Trilock | Teloken et al. [50] | 2002 | 15 (14.5–17) | 50 (25–72) | 67 | 3 | 92 | 9 | 0 | |
| Furlong | Rajaratnam et al. [38] | 2008 | 17.5 (15– 21) | 71 (31–90) | 331 | 2 | 6 | 0 | 97/– | |
| Bicontact | Ochs et al. [33] | 2007 | 18 (16–20) | 56 (22–84) | 250 | 17 | 82 | 10 | 5 | 96/– |
| Harris-Galante | Parvizi et al. [37] | 2004 | 15 (12–18) | 58 (23–80) | 90 | 0 | 89 | 9 | 7 | 87 |
| Lord | Grant and Nordsletten [17] | 2004 | 17 (15–20) | 62 (32–77) | 116 | 1 | 85 | 8 | 1 | 92/– |
| Martinez de Aragón and Keisu [28] | 2007 | 21 | 60 (38–86) | 114 | 1 | 11 | 0 | 83‡ | ||
| PCA | Kim [24] | 2005 | 19 (18–20) | 48 (19–69) | 131 | 4 | 85 | 10 | 8 | 91/– |
| Bojescul et al. [7] | 2003 | 16 (15–17) | 58 (22–81) | 91 | 0 | 81 | 7 | 4 | 93/– |
* Implants still in clinical use include: CLS® Spotorno® (Zimmer Inc, Warsaw, IN), Zweymüller® (Zimmer Inc), AML® (DePuy Orthopaedics, Inc, Warsaw, IN), Taperloc® (Biomet Inc, Warsaw, IN), Tri-lock® (DePuy Orthopaedics, Inc), Furlong® (JRI Ltd, London, UK), Bicontact (B. Braun Aesculap, Tüttlingen, Germany); implants not still in clinical use include: Harris-Galante® (Zimmer Inc), Lord (Howmedica, Rutherford, NJ), PCA® (Howmedica); †values expressed as means, with ranges in parentheses; ‡infection excluded; HHS = Harris hip score.
Despite excellent survival of the stem, the clinical results represented by a median HHS of 80 points were moderate, although only 5% of patients complained of moderate to severe pain. These relatively low HHS at final followup can be attributed partially to the relatively high number of patients with low Charnley classes (B/C) (Table 2) [10], the fact that more than 40% of hips had undergone acetabular revision for the failed acetabular constructs [44], in most cases with major reconstruction (cages), and the natural decline in hip scores with age. Clinical long-term results of other uncemented implants showed variable results ranging from a mean HHS of 81 [7] to 92 [50] (Table 4).
Thigh pain occurs in association with distal canal reaming [12], cobalt-chromium implants [6, 53], and tight fit [12]. Interestingly, in our series, no case of thigh pain has been found. We suggest this is due to the more flexible titanium alloy, the lack of tight distal canal fill, and the more proximal metadiaphyseal loading of the CLS® Spotorno® stem [2].
In all longer-term reports, the CLS® Spotorno® stem was associated with low rates of osteolysis [1, 4, 42, 43]. In our study, we found small (< 1 cm2) proximal osteolytic lesions in 15% of the hips. This is in contrast to other mainly cobalt-chrome alloy uncemented implants, ranging up to 37% osteolysis larger than 1.5 cm2 [6]. However, osteolysis is mainly dependent on polyethylene wear [52] and therefore independent of the stem used. The wedge-shaped design with a fluted tip might have led to the absence of severe stress shielding and distal cortical hypertrophy on radiographic examination. This finding is in contrast to the results of other successful uncemented implants with tight distal fit, where high rates of cortical hypertrophy have been reported due to more distal fixation [6, 13, 14, 17, 18, 40, 49, 53]. Even trochanteric fractures related to stress shielding and osteolysis have been reported in up to 22% [6] of cases using the anatomic medullary locking uncemented components.
The scarcity of long-term results (> 15 years) for uncemented femoral implants makes it difficult to predict long-term outcome. After 17 years with 156 stems still at risk, we found a low revision rate due to aseptic loosening of the stem, no distal femoral osteolysis, and survival similar to the best cemented and uncemented series in younger patient groups [9, 25, 31, 38]. In our opinion, the insertion of this uncemented femoral stem is less demanding than a well-cemented THA. Even in a multisurgeon series, the long-term results were very consistent. Our data demonstrate high rates of stable implants in the long term for this grit-blasted uncemented tapered stem.
Acknowledgments
We thank Dr. Patric Raiss, Research Fellow, and Dr. Jörn Seeger, Research Fellow, for their support in manuscript editing. We acknowledge the work of all 23 surgeons who contributed patients to this study. Among those, we would like to specifically thank Professor Dr. Horst Cotta and Professor Dr. Fritz-Uwe Niethard, who contributed most of the patients for this study.
Footnotes
The institution of one or more of the authors (VE) has received funding from Zimmer GmbH, Winterthur, Switzerland.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Stiftung Orthopädische Universitätsklinik.
References
- 1.Aldinger PR, Breusch SJ, Lukoschek M, Mau H, Ewerbeck V, Thomsen M. A ten- to 15-year follow-up of the cementless Spotorno stem. J Bone Joint Surg Br. 2003;85:209–214. doi: 10.1302/0301-620X.85B2.13216. [DOI] [PubMed] [Google Scholar]
- 2.Aldinger PR, Sabo D, Pritsch M, Thomsen M, Mau H, Ewerbeck V, Breusch SJ. Pattern of periprosthetic bone remodeling around stable uncemented tapered hip stems: a prospective 84-month follow-up study and a median 156-month cross-sectional study with DXA. Calcif Tissue Int. 2003;73:115–121. doi: 10.1007/s00223-002-2036-z. [DOI] [PubMed] [Google Scholar]
- 3.Aldinger PR, Thomsen M, Lukoschek M, Mau H, Ewerbeck V, Breusch SJ. Long-term fate of uncemented, threaded acetabular components with smooth surface treatment: minimum 10-year follow-up of two different designs. Arch Orthop Trauma Surg. 2004;124:469–475. doi: 10.1007/s00402-004-0709-y. [DOI] [PubMed] [Google Scholar]
- 4.Aldinger PR, Thomsen M, Mau H, Ewerbeck V, Breusch SJ. Cementless Spotorno tapered titanium stems: excellent 10–15-year survival in 141 young patients. Acta Orthop Scand. 2003;74:253–258. doi: 10.1080/00016470310014157. [DOI] [PubMed] [Google Scholar]
- 5.Bauer R, Kerschbaumer F, Poisel S, Oberthaler W. The transgluteal approach to the hip joint. Arch Orthop Trauma Surg. 1979;95:47–49. doi: 10.1007/BF00379169. [DOI] [PubMed] [Google Scholar]
- 6.Belmont PJ, Jr, Powers CC, Beykirch SE, Hopper RH, Jr, Engh CA, Jr, Engh CA. Results of the anatomic medullary locking total hip arthroplasty at a minimum of twenty years: a concise follow-up of previous reports. J Bone Joint Surg Am. 2008;90:1524–1530. doi: 10.2106/JBJS.G.01142. [DOI] [PubMed] [Google Scholar]
- 7.Bojescul JA, Xenos JS, Callaghan JJ, Savory CG. Results of porous-coated anatomic total hip arthroplasty without cement at fifteen years: a concise follow-up of a previous report. J Bone Joint Surg Am. 2003;85:1079–1083. doi: 10.2106/00004623-200306000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Britton A, Murray D, Bulstrode C, McPherson K, Denham R. Loss to follow-up: does it matter? Lancet. 1995;345:1511–1512. doi: 10.1016/S0140-6736(95)91071-9. [DOI] [PubMed] [Google Scholar]
- 9.Callaghan JJ, Liu SS, Firestone DE, Yehyawi TM, Goetz DD, Sullivan J, Vittetoe DA, O’Rourke MR, Johnston RC. Total hip arthroplasty with cement and use of a collared matte-finish femoral component: nineteen to twenty-year follow-up. J Bone Joint Surg Am. 2008;90:299–306. doi: 10.2106/JBJS.G.00095. [DOI] [PubMed] [Google Scholar]
- 10.Charnley J. The long-term results of low-friction arthroplasty of the hip performed as a primary intervention. J Bone Joint Surg Br. 1972;54:61–76. [PubMed] [Google Scholar]
- 11.Ellison B, Berend KR, Lombardi AV, Jr, Mallory TH. Tapered titanium porous plasma-sprayed femoral component in patients aged 40 years and younger. J Arthroplasty. 2006;21:32–37. doi: 10.1016/j.arth.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 12.Engh CA, Bobyn JD, Glassman AH. Porous-coated hip replacement: the factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg Br. 1987;69:45–55. doi: 10.1302/0301-620X.69B1.3818732. [DOI] [PubMed] [Google Scholar]
- 13.Engh CA, Jr, Claus AM, Hopper RH, Jr, Engh CA. Long-term results using the anatomic medullary locking hip prosthesis. Clin Orthop Relat Res. 2001;393:137–146. doi: 10.1097/00003086-200112000-00016. [DOI] [PubMed] [Google Scholar]
- 14.Engh CA, Jr, Culpepper WJ, 2nd, Engh CA. Long-term results of use of the anatomic medullary locking prosthesis in total hip arthroplasty. J Bone Joint Surg Am. 1997;79:177–184. doi: 10.1302/0301-620X.79B2.7640. [DOI] [PubMed] [Google Scholar]
- 15.Eskelinen A, Remes V, Helenius I, Pulkkinen P, Nevalainen J, Paavolainen P. Uncemented total hip arthroplasty for primary osteoarthritis in young patients: a mid-to long-term follow-up study from the Finnish Arthroplasty Register. Acta Orthop. 2006;77:57–70. doi: 10.1080/17453670610045704. [DOI] [PubMed] [Google Scholar]
- 16.Fowler JL, Gie GA, Lee AJ, Ling RS. Experience with the Exeter total hip replacement since 1970. Orthop Clin North Am. 1988;19:477–489. [PubMed] [Google Scholar]
- 17.Grant P, Nordsletten L. Total hip arthroplasty with the Lord prosthesis: a long-term follow-up study. J Bone Joint Surg Am. 2004;86:2636–2641. doi: 10.2106/00004623-200412000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Grubl A, Chiari C, Giurea A, Gruber M, Kaider A, Marker M, Zehetgruber H, Gottsauner-Wolf F. Cementless total hip arthroplasty with the rectangular titanium Zweymuller stem: a concise follow-up, at a minimum of fifteen years, of a previous report. J Bone Joint Surg Am. 2006;88:2210–2215. doi: 10.2106/JBJS.E.00810. [DOI] [PubMed] [Google Scholar]
- 19.Gruen TA, McNeice GM, Amstutz HC. “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979;141:17–27. [PubMed] [Google Scholar]
- 20.Hallan G, Lie SA, Furnes O, Engesaeter LB, Vollset SE, Havelin LI. Medium- and long-term performance of 11, 516 uncemented primary femoral stems from the Norwegian arthroplasty register. J Bone Joint Surg Br. 2007;89:1574–1580. doi: 10.1302/0301-620X.89B12.18969. [DOI] [PubMed] [Google Scholar]
- 21.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 22.Ihle M, Mai S, Pfluger D, Siebert W. The results of the titanium-coated RM acetabular component at 20 years: a long-term follow-up of an uncemented primary total hip replacement. J Bone Joint Surg Br. 2008;90:1284–1290. doi: 10.1302/0301-620X.90B10.20274. [DOI] [PubMed] [Google Scholar]
- 23.Kelley SS, Fitzgerald RH, Jr, Rand JA, Ilstrup DM. A prospective randomized study of a collar versus a collarless femoral prosthesis. Clin Orthop Relat Res. 1993;294:114–122. [PubMed] [Google Scholar]
- 24.Kim YH. Long-term results of the cementless porous-coated anatomic total hip prosthesis. J Bone Joint Surg Br. 2005;87:623–627. doi: 10.1302/0301-620X.87B5.15554. [DOI] [PubMed] [Google Scholar]
- 25.Lewthwaite SC, Squires B, Gie GA, Timperley AJ, Ling RS. The Exeter Universal hip in patients 50 years or younger at 10–17 years’ followup. Clin Orthop Relat Res. 2008;466:324–331. doi: 10.1007/s11999-007-0049-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lombardi AV, Jr, Berend KR, Mallory TH. Hydroxyapatite-coated titanium porous plasma spray tapered stem: experience at 15 to 18 years. Clin Orthop Relat Res. 2006;453:81–85. doi: 10.1097/01.blo.0000238872.01767.09. [DOI] [PubMed] [Google Scholar]
- 27.Lombardi AV, Jr, Berend KR, Mallory TH, Skeels MD, Adams JB. Survivorship of 2000 tapered titanium porous plasma-sprayed femoral components. Clin Orthop Relat Res. 2009;467:146–154. doi: 10.1007/s11999-008-0568-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Martinez de Aragon JS, Keisu KS. 21-year results of the uncemented fully textured lord hip prosthesis. Clin Orthop Relat Res. 2007;454:133–138. doi: 10.1097/01.blo.0000238782.13854.50. [DOI] [PubMed] [Google Scholar]
- 29.McAuley JP, Szuszczewicz ES, Young A, Engh CA., Sr Total hip arthroplasty in patients 50 years and younger. Clin Orthop Relat Res. 2004;418:119–125. doi: 10.1097/00003086-200401000-00019. [DOI] [PubMed] [Google Scholar]
- 30.McLaughlin JR, Lee KR. The outcome of total hip replacement in obese and non-obese patients at 10- to 18-years. J Bone Joint Surg Br. 2006;88:1286–1292. doi: 10.1302/0301-620X.88B10.17660. [DOI] [PubMed] [Google Scholar]
- 31.McLaughlin JR, Lee KR. Total hip arthroplasty with an uncemented tapered femoral component. J Bone Joint Surg Am. 2008;90:1290–1296. doi: 10.2106/JBJS.G.00771. [DOI] [PubMed] [Google Scholar]
- 32.Meding JB, Ritter MA, Keating EM, Faris PM. Clinical and radiographic evaluation of long-stem femoral components following revision total hip arthroplasty. J Arthroplasty. 1994;9:399–408. doi: 10.1016/0883-5403(94)90051-5. [DOI] [PubMed] [Google Scholar]
- 33.Ochs U, Eingartner C, Volkmann R, Ochs BG, Huber C, Weller S, Weise K. Prospective long-term follow-up of the cementless bicontact hip stem with plasmapore coating. Z Orthop Unfall. 2007;145(Suppl 1):S3–S8. doi: 10.1055/s-2007-965652. [DOI] [PubMed] [Google Scholar]
- 34.Parsch D, Jung AW, Thomsen M, Ewerbeck V, Aldinger PR. Good survival of uncemented tapered stems for failed intertrochanteric osteotomy: a mean 16 year follow-up study in 45 patients. Arch Orthop Trauma Surg. 2008;128:1081–1085. doi: 10.1007/s00402-007-0444-2. [DOI] [PubMed] [Google Scholar]
- 35.Parvizi J, Keisu KS, Hozack WJ, Sharkey PF, Rothman RH. Primary total hip arthroplasty with an uncemented femoral component: a long-term study of the Taperloc stem. J Arthroplasty. 2004;19:151–156. doi: 10.1016/j.arth.2003.10.003. [DOI] [PubMed] [Google Scholar]
- 36.Parvizi J, Sharkey PF, Hozack WJ, Orzoco F, Bissett GA, Rothman RH. Prospective matched-pair analysis of hydroxyapatite-coated and uncoated femoral stems in total hip arthroplasty: a concise follow-up of a previous report. J Bone Joint Surg Am. 2004;86:783–786. doi: 10.1302/0301-620X.86B6.15356. [DOI] [PubMed] [Google Scholar]
- 37.Parvizi J, Sullivan T, Duffy G, Cabanela ME. Fifteen-year clinical survivorship of Harris-Galante total hip arthroplasty. J Arthroplasty. 2004;19:672–677. doi: 10.1016/j.arth.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 38.Rajaratnam SS, Jack C, Tavakkolizadeh A, George MD, Fletcher RJ, Hankins M, Shepperd JA. Long-term results of a hydroxyapatite-coated femoral component in total hip replacement: a 15- to 21-year follow-up study. J Bone Joint Surg Br. 2008;90:27–30. doi: 10.1302/0301-620X.90B1.19731. [DOI] [PubMed] [Google Scholar]
- 39.Reigstad A, Rokkum M, Bye K, Brandt M. Femoral remodeling after arthroplasty of the hip: prospective randomized 5-year comparison of 120 cemented/uncemented cases of arthrosis. Acta Orthop Scand. 1993;64:411–416. doi: 10.3109/17453679308993656. [DOI] [PubMed] [Google Scholar]
- 40.Reigstad O, Siewers P, Rokkum M, Espehaug B. Excellent long-term survival of an uncemented press-fit stem and screw cup in young patients: follow-up of 75 hips for 15–18 years. Acta Orthop. 2008;79:194–202. doi: 10.1080/17453670710014978. [DOI] [PubMed] [Google Scholar]
- 41.Sathappan SS, Ginat D, Patel V, Walsh M, Jaffe WL, Di Cesare PE. Effect of anesthesia type on limb length discrepancy after total hip arthroplasty. J Arthroplasty. 2008;23:203–209. doi: 10.1016/j.arth.2007.01.022. [DOI] [PubMed] [Google Scholar]
- 42.Schramm M, Keck F, Hohmann D, Pitto RP. Total hip arthroplasty using an uncemented femoral component with taper design: outcome at 10-year follow-up. Arch Orthop Trauma Surg. 2000;120:407–412. doi: 10.1007/PL00013771. [DOI] [PubMed] [Google Scholar]
- 43.Siebold R, Scheller G, Schreiner U, Jani L. Long-term results with the cement-free Spotorno CLS shaft [in German] Orthopade. 2001;30:317–322. doi: 10.1007/s001320050614. [DOI] [PubMed] [Google Scholar]
- 44.Simank HG, Brocai DR, Reiser D, Thomsen M, Sabo D, Lukoschek M. Middle-term results of threaded acetabular cups: high failure rates five years after surgery. J Bone Joint Surg Br. 1997;79:366–370. doi: 10.1302/0301-620X.79B3.7273. [DOI] [PubMed] [Google Scholar]
- 45.Singh M, Nagrath AR, Maini PS. Changes in trabecular pattern of the upper end of the femur as an index of osteoporosis. J Bone Joint Surg Am. 1970;52:457–467. [PubMed] [Google Scholar]
- 46.Slack R, Tindall A, Shetty AA, James KD, Rand C. 15-year follow-up results of the hydroxyapatite ceramic-coated femoral stem. J Orthop Surg (Hong Kong) 2006;14:151–154. doi: 10.1177/230949900601400209. [DOI] [PubMed] [Google Scholar]
- 47.Smith SE, Estok DM, 2nd, Harris WH. 20-year experience with cemented primary and conversion total hip arthroplasty using so-called second-generation cementing techniques in patients aged 50 years or younger. J Arthroplasty. 2000;15:263–273. doi: 10.1016/S0883-5403(00)90463-7. [DOI] [PubMed] [Google Scholar]
- 48.Spotorno L, Romagnoli S, Ivaldo N, Grappiolo G, Bibbiani E, Blaha DJ, Guen TA. The CLS system: theoretical concept and results. Acta Orthop Belg. 1993;59(Suppl 1):144–148. [PubMed] [Google Scholar]
- 49.Suckel A, Geiger F, Kinzl L, Wulker N, Garbrecht M. Long-term results for the uncemented Zweymuller/Alloclassic hip endoprosthesis: a 15-year minimum follow-up of 320 hip operations. J Arthroplasty. 2008 Sep 11. [Epub ahead of print]. [DOI] [PubMed]
- 50.Teloken MA, Bissett G, Hozack WJ, Sharkey PF, Rothman RH. Ten to fifteen-year follow-up after total hip arthroplasty with a tapered cobalt-chromium femoral component (tri-lock) inserted without cement. J Bone Joint Surg Am. 2002;84:2140–2144. doi: 10.2106/00004623-200212000-00003. [DOI] [PubMed] [Google Scholar]
- 51.Vervest TM, Anderson PG, Hout F, Wapstra FH, Louwerse RT, Koetsier JW. Ten to twelve-year results with the Zweymuller cementless total hip prosthesis. J Arthroplasty. 2005;20:362–368. doi: 10.1016/j.arth.2004.11.017. [DOI] [PubMed] [Google Scholar]
- 52.Willert HG, Bertram H, Buchhorn GH. Osteolysis in alloarthroplasty of the hip: the role of ultra-high molecular weight polyethylene wear particles. Clin Orthop Relat Res. 1990;258:95–107. [PubMed] [Google Scholar]
- 53.Yoon TR, Rowe SM, Kim MS, Cho SG, Seon JK. Fifteen- to 20-year results of uncemented tapered fully porous-coated cobalt-chrome stems. Int Orthop. 2008;32:317–323. doi: 10.1007/s00264-007-0337-6. [DOI] [PMC free article] [PubMed] [Google Scholar]