Abstract
Acetabular component revision in the context of large contained bone defects with less than 50% host bone contact traditionally have been treated with roof reinforcement or antiprotrusio cages. Trabecular Metal™ cups (Zimmer, Inc, Warsaw, IN) may offer a reasonable treatment alternative. We evaluated the clinical and radiographic outcome of this mode of treatment. We prospectively followed 53 hip revision acetabular arthroplasty procedures performed with Trabecular Metal™ cups for contained defects with 50% or less contact with native bone. All patients were clinically and radiographically evaluated for evidence of loosening or failure. Minimum followup was 24 months (average, 45 months; range, 24–71 months). Contact with host bone ranged from 0% to 50% (average, 19%). The mean postoperative Merle d’Aubigne-Postel score was 10.6 (range, 1–12), with a mean improvement of 5.2 (range, −4–10) compared to the preoperative score. Two failed cups (4%) were revised. Two additional cups (4%) had radiographic evidence of probable loosening. Complications included four dislocations and one sciatic nerve palsy. The data suggest treatment of cavitary defects with less than 50% host bone contact using Trabecular Metal™ cups, without structural support by augments or structural bone grafts, is a reasonable option.
Level of Evidence: Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Acetabular bone loss encountered during revision hip arthroplasty can pose a major challenge to reconstruct. Cavitary bone defects are the most commonly encountered major bone deficits [3, 10]. These defects represent a volumetric loss in bony substance of the acetabular cavity (including the medial wall), but the acetabular rim remains intact [4].
It is well accepted that cementless hemispheric cups need initial mechanical stability and biologic conditions favorable for bony ingrowth to have reliable longevity [7]. Thus, acetabular bone defects in which implant contact with greater than 50% host bone can be attained reportedly can be addressed using a conventional uncemented cup, screw fixation, and packing with morselized bone graft, resulting in high hip scores and survivorship [3, 7, 10]. In such cases, a slightly high or medial hip center and the use of large-diameter cups are sometimes necessary to achieve good initial stability of the cup.
In larger contained bone defects, when 50% host contact cannot be achieved, roof reinforcement rings or antiprotrusio cages are often recommended [1, 3, 10, 11]. The recently introduced highly porous Trabecular Metal™ (TM) cups (Zimmer, Inc, Warsaw, IN) facilitate bone ingrowth and primary stability [22]. These cups have demonstrated encouraging revisions rates of 0% to 6% for mechanical loosening for both primary and revision hip arthroplasty at an average of 3 to 5 years [3, 6, 13, 14, 21, 22]. Utilizing these new TM cups, it is quite possible, when reasonable primary stability can be obtained and reinforced by effective screw fixation, the need for more than 50% host bone contact may now be reduced. Contained defects usually allow reaming to a hemispheric cavity at or near the correct hip center and do not require structural support in the form of metal augments or structural bone grafts. Morselized bone packed into the contained defect adds to the primary press fit of the cup and will later remodel and integrate to the highly porous TM to provide long-term support [2]. More extensive contained defects for which no initial stability can be achieved should be protected by a cage [1, 3, 10] or the use of impaction grafting [19]. It is the authors’ practice to use the cup-cage construct for such cases [3, 10]. Adequate management of segmental, uncontained bone defects requires structural support, such as structural bone grafts or metal augments [1, 3].
To assess the viability of TM cups as a treatment option for contained defects for which more than 50% host bone contact could not be made, we assessed (1) the radiographic mechanical failure and loosening rates and (2) the functional outcome and complications of this technique.
Materials and Methods
We performed acetabular revision surgery in 254 patients (272 cups) in our institution between January 2002 and June 2006. We prospectively followed 191 of these patients (203 acetabular revisions) in whom the TM shell was used. This study is part of a larger prospective study following all patients treated with TM cups and for this study, we included only patients with contained bone defects in which more than 50% host could not be achieved. All defects were Type II defects according to the classification of Saleh et al. [17]. These defects involve dilatation and weakening of the acetabulum, while the columns and rim remain intact [17]. We excluded patients who needed structural support in the form of a structural graft or a TM acetabular augment and patients for whom there was no initial stability of the trial component and therefore had the cup protected by an antiprotrusio cage (a cup-cage construct). This left 58 patients (58 arthroplasties) for study. Five patients died or were lost to followup before 2 years of followup were completed. Thus, 53 patients were available for evaluation. The mean age at time of surgery was 63 years (range, 29–86 years). Included were 29 (55%) men and 24 (45%) women. The indication for 48 revisions (91%) was aseptic loosening. Three (5%) of the revisions were for instability and two (4%) for infection (two-stage revisions). The femoral component was also revised in 23 (43%) cases. Cementless modular stems (ZMR®; Zimmer) were used in 16 cases, cementless nonmodular stems were used in three cases, and proximal femoral allografts with long cemented stems were used in four cases. The index operation was a first hip arthroplasty revision for 32 (60%) patients, a second revision for 18 (34%), and a third revision for three (6%) (Table 1). The mean preoperative Merle d’Aubigne-Postel score was 5.3 (range, 1–10) [16]. The minimum followup was 24 months (mean, 45 months; range, 24–71 months). All patients were enrolled and provided consent to participate in the study before the operation.
Table 1.
Patient demographics and preoperative clinical characteristics
| Characteristic | Number of patients (%) |
|---|---|
| Gender | |
| Male | 29 (55%) |
| Female | 24 (45%) |
| Age (years)* | 63 ± 13 (29–86) |
| Indication for revision | |
| Aseptic loosening | 48 (91%) |
| Instability | 3 (5%) |
| Infection | 2 (4%) |
| Femoral component | |
| Revised | 23 (43%) |
| Not revised | 30 (57%) |
| Number of hip revisions | |
| 1 | 32 (60%) |
| 2 | 18 (34%) |
| 3 | 3 (6%) |
* Value expressed as mean ± standard deviation, with range in parentheses.
Our surgical preoperative planning included the radiographic assessment of cup fixation and position, assessment of acetabular bone stock, determination of the hip’s center of rotation, and templating of the cup’s size in the ideal position. This allowed us to be prepared in advance with allograft, cages, equipment for extraction of well-fixed cups, and, when uncontained defects are suspected, TM augments or structural allografts. Erythrocyte sedimentation rate and C-reactive protein levels were obtained for all patients, and, if suggestive of infection, we performed a preoperative hip aspiration.
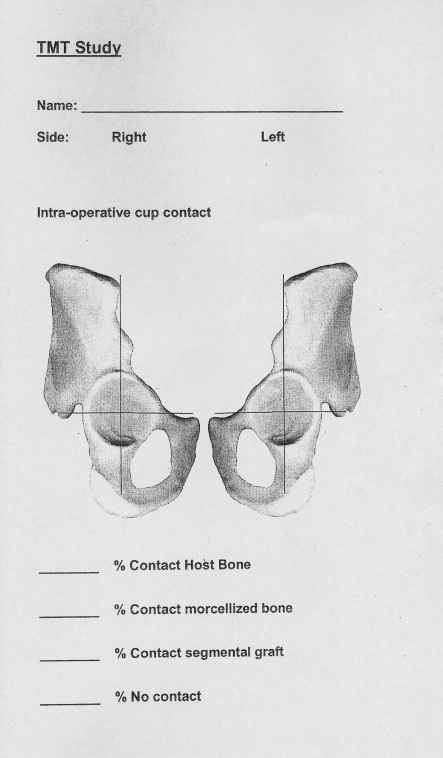
All patients were operated on in the lateral decubitus position. We routinely used a modified trochanteric slide to improve surgical exposure in complex acetabular revisions [8]. If necessary, the slide was extended distally to remove the femoral stem. After excision of the pseudocapsule and removal of the old component, the available bone stock was assessed. We sequentially reamed the acetabulum until a hemispheric cavity was formed with the support of both walls. Cancellous bleeding bone would be more favorable for bone ingrowth, but in the revision situation one must often accept sclerotic and not bleeding bone [15]. We prefer to position the cup slightly more anteverted and horizontal than for primary hip replacement to protect from posterior dislocation. At this point, the bone defect was reassessed. If the defect was mostly contained and did not need structural support, the cavities were packed with morselized bone graft. Since autograft is usually less available in revision surgery, we generally used deep-frozen allografts. If autograft was available, for instance from the femoral reaming, we added it to augment the allograft. Trial components were used to assess coverage, impingement, and stability. We do not rely on screws only to support the load forces of the hip [15]. If we could not achieve stability with the trial, we protected the cup with a cage. One of the two surgeons (AEG or DB) estimated the percentage of host bone contact and allograft contact intraoperatively. With the trial cup in, each quadrant of the acetabular hemisphere was assessed separately for contact with host bone, morselized bone graft, or no contact with bone (uncoverage). Contact with each one of those surfaces was expressed in 20% segments for each quadrant (representing 5% segments for the whole hemisphere). The overall contact was calculated by joining the quadrant scores and was recorded on designated forms (Fig. 1). Contact areas in the different quadrants were also depicted on the diagram. These data were entered into a prospective database.
Fig. 1.
An intraoperative cup contact recording form is shown. The percentage of contact with host bone and morselized bone was recorded and drawn on the acetabular illustration.
For situations where the bone defect was more global, we used the acetabular reamer in reverse mode to better pack and more evenly spread the morselized allograft while creating a hemispheric cavity, which allows for improved press fit of the cup. The cup is completely covered with morselized bone and has no contact with host bone. Such cases were recorded as 100% allograft contact and 0% of host bone contact. The definitive cup was then inserted and reinforced by as many effective screws as possible. At least two good screws were required to provide adequate cup stability. The TM cups can be either a “modular cup” with a locking mechanism for the polyethylene liner or a “revision cup” into which the polyethylene liner is cemented. We use antibiotic-impregnated cement in all revisions. The revision shell liner, sized as recommended by the manufacturer, provides a nominal 2- to 3-mm cement mantle. The revision cup type allows customization of the liner inclination and version relative to the cup. In addition, so-called “revision cups” allow for drilling directly through the metal shell to provide additional screw fixation. Only one cup was modular. Average intraoperative bone contact with the cups was 19% (range, 0%–50%). Five cups had a global defect for which we performed reverse reaming of morselized bone; we considered these to have 0% of host bone contact. The remaining 49 cups had between 20% and 50% of host bone contact (mean, 38%) (Table 2). The overall contact with morselized bone graft was between 10% and 100%. The five sockets that were reverse reamed were all completely covered and were considered to have a 100% of morselized bone contact. The remaining 49 cups had between 10% and 80% (mean, 38%) of morselized bone contact. The mean cup size was 60 (range, 46–72). All cups were reinforced by at least two screws (range, 2–5; mean, 3). All liners but one were cemented into the cup. Two cups were constrained due to prior instability and deficient abductor mechanism.
Table 2.
Percentage contact of cups with host bone and morselized bone graft
| Percentage contact of TM cup with particulate graft | Percentage contact of TM cup with acetabulum | ||
|---|---|---|---|
| 0% | 20%–30% | 35%–50% | |
| 100% | 5 | ||
| 51%–99% | 15 | 8 | |
| 10%–50% | 1 | 24 | |
Followup visits occurred at 6 weeks, 12 weeks, 6 months, and 1 year after the procedure and then annually. Clinical evaluation in each patient included the Merle d’Aubigne-Postel scores preoperatively, at 6 weeks postsurgery, and at annual followup visits.
We obtained routine standard hip radiographs (anteroposterior view of the pelvis and anteroposterior and lateral views of the affected hip) performed preoperatively, at 6 weeks, and annually postoperatively. The initial 6-week postoperative series of radiographs served as the baseline to which all subsequent radiographs were compared. All radiographs were reviewed by one observer (DL) not involved in patient care. Evaluation of fixation of the cup was based on evidence of migration and the occurrence of radiolucent lines at the bone-implant interface. We recorded cup inclination angles, the vertical distance of the hip center of rotation from the interteardrop line, and the horizontal distance of the hip center of rotation from the teardrop. These measurements were used to assess cup migration on the last radiograph compared to the baseline radiograph. The cup was considered loose only if more than 3 mm of migration in the vertical or horizontal directions or more than 3° change of inclination were demonstrated [12, 18]. Radiolucent lines in the three acetabular zones of DeLee and Charnley [5] were recorded. When serial radiographs demonstrated a radiolucent line of more than 1 mm in width in all zones, the cup was considered probably loose [23]. Cups were considered as failed if they were revised for loosening or deemed mechanically unstable based on migration or change of inclination on radiographs.
Results
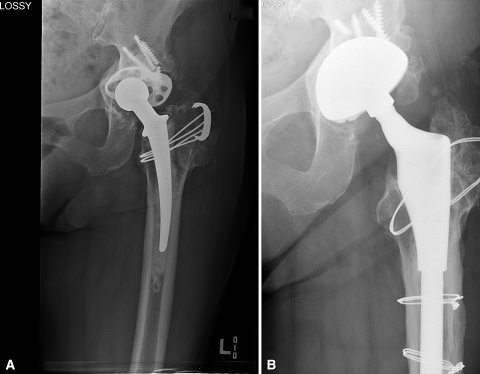
There were two cup failures as defined by component migration and need for revision. One had an initial host bone contact of 30% and was revised 6 months after the first revision (Fig. 2). The second patient had an initial contact of 40%, failed at 9 months postoperatively, but refused further revision. Thus, the mechanical failure rate was 4%. Two cups (4%) had 1-mm radiolucent lines that appeared during followup, both in all three zones. The two cups’ position and alignment did not change. In one patient, it was associated with the onset of minor nonprogressive groin pain 5 years postoperatively. The other patient complained of pain associated with a recent fall 2 years after the revision that was later resolved. These cups were considered as probably loose. All other cups were radiographically well fixed (Fig. 3). Four cups (7%) had 1-mm radiolucent lines in the 6-week postoperative radiograph that did not fill up at last followup: one in Zone I, two in Zone II, and one in Zone III.
Fig. 2A–D.
(A) A 75-year-old patient had a cup revision after failure of an antiprotrusio cage. (B) She had a cavitary bone defect with 30% of host bone contact, and a TM cup was used. (C) Five months later, the cup failed and (D) was revised again using a cage.
Fig. 3A–B.
(A) This 77-year-old patient had a revision of a failed roof ring. (B) Five years later, the TM cup was well fixed and the morselized allograft remodeled.
The mean postoperative Merle d’Aubigne-Postel score was 10.6 (range, 1–12), with a mean improvement of 5.2 (range, −4–10) compared to the preoperative score. There were five (9%) complications: four (8%) dislocations and one (2%) sciatic nerve palsy. Three of the patients who had dislocations had revision to a constrained liner. The cup itself was well fixed in all of them and the new liners were cemented in. We tend to use constrained liners more liberally when only the liner is replaced and the cup is already well fixed. This is even more so when it is a TM cup. There were no deep infections.
Discussion
Acetabular component revision in the face of large contained bone defects with no more than 50% host bone contact has been traditionally treated with roof reinforcement rings or antiprotrusio cages, associated with substantial complication and failure rates [9, 20]. Trabecular Metal™ cups may offer a reasonable treatment alternative. The objective of this study was to evaluate the clinical and radiographic outcome of this mode of treatment.
There were several limitations to our study. First, assessment of bone contact was performed intraoperatively and cannot be reproduced by an unbiased observer. Unfortunately, preoperative objective assessment of bone defect was not practical for the purpose of this study, since bone contact needed be evaluated after removing the old component and reaming the socket. Photography of the defect and later calculation of bone contact would also be impractical because of the difficulty in standardizing the technique. A second limitation of this study is that there was no control group of patients with the same characteristics, treated traditionally with bone graft protected by a cage. We could find no report in the English literature addressing specifically contained acetabular defects with reference to extent of bone loss for the purpose of comparison.
Cementless acetabular cups in revision hip surgery have been used extensively over the past two decades [7]. It is well accepted that a favorable biologic environment to allow bony ingrowth is necessary for these implants to achieve long-term stability and primary mechanical stability. Previous reports stated more than 50% host bone contact, preferably in the dome and posterior column, is necessary to allow initial stabilization of an uncemented cup by screws and subsequent bony ingrowth [7, 9, 11]. More severe cavitary bone defects, where less host bone contact is possible, have been traditionally treated with a large amount of morselized bone graft packed into the defect and protected by an antiprotrusio cage or a reinforcement ring. However, cages are technically challenging and need a wide exposure of the ilium and ischium. The most important problem with cages is that they are not made of a material that allows osteointegration and consequently there is a high incidence of hardware failure due to screw breakage or ischial flange migration [10]. A failure rate as high as 24% at 5 years has been reported (Table 3) [1, 9, 20]. Cages also have a high rate of complications, such as sciatic nerve injuries, flange fractures, and dislocations [9]. The recently introduced tantalum TM cups have had encouraging results in both primary and revision hip arthroplasty [3, 12–14, 21, 22]. TM is 80% porous, has a bonelike microstructure, and has a modulus of elasticity between that of cortical and cancellous bone. It also has a high coefficient of friction [3, 6, 12]. These improved material characteristics provide a favorable environment for bone ingrowth, bone graft remodeling, and better initial stability [2]. We still do not have long term followup of the use of TM cups, and the selection criteria and outcome assessment vary considerably among studies (Table 3). Nevertheless, cages had no advantage over TM cups regarding mechanical failure rates at a mean followup of 4 to 5 years, despite their potential better initial stability [1, 9, 20]. Other studies that evaluated the performance of TM cups for more heterogeneous groups of acetabular defects had failure rates comparable to that of our series [5, 13, 21, 22].
Table 3.
Results of different series of revision acetabular reconstruction in the literature
| Study | Year | Specific selection | Implants used for reconstruction | Number of patients | Mean followup (years)* | Mechanical failure rate | Mean Merle d’Aubigné-Postel score improvement† |
|---|---|---|---|---|---|---|---|
| Berry and Müller [1] | 1992 | Combined contained and segmental defects | Antiprotrusio cages | 42 | 5 (2–11) | 12% | 2.2 |
| Goodman et al. [9] | 2004 | Contained with > 50% loss of acetabulum and segmental defects | Reconstruction rings | 61 | 5 (2–18) | 24% | NA |
| Sembrano and Cheng [20] | 2008 | Contained and segmental defects | Cages | 72 | 5 (1–11) | 19% | NA |
| Flecher et al. [6] | 2008 | Segmental defects | TM cups + augments | 23 | 3 (2–4) | 0% | 3.8 |
| Kim et al. [13] | 2008 | Contained and segmental defects | TM cups | 46 | 3 (2–4) | 2% | NA |
| Siegmeth et al. [21] | 2009 | Contained and segmental defects | TM cups + augments | 34 | 3 (2–5) | 6% | NA |
| Unger et al. [22] | 2005 | Contained and segmental defects | TM cups | 60 | 3.5 (1–6) | 2% | NA |
| Garcia-Cimbrelo [7] | 1999 | Contained and segmental defects | Cementless hemispheric cups | 65 | 8 (6–11) | 11% | 5.9 |
| Lakstein et al. (Currrent study) | 2009 | Contained defects with ≤ 50% host bone contact | TM cups | 53 | 4 (2–6) | 4% | 5.1 |
* Range in parentheses; †combined pain and function Merle d’Aubigné-Postel score; TM = Trabecular Metal™; NA = not available.
Our results demonstrate a 4% failure rate and high Merle d’Aubigne-Postel scores at last followup (average, 45 months; range, 24–71 months). This specific and challenging subset of patients with large cavitary defects and limited contact with host bone can clearly benefit from the use of the described technique. As opposed to other options, such as the antiprotrusio cage or the reinforcement ring, this technique offers better potential for long-term survival based on bone stock renewal and progressive integration with the surrounding bone. In the short term, the theoretical advantage of the reconstruction cage in the provision of better initial stability did not prove itself important, considering the low failure rate of our series. One final although not trivial advantage of the TM cup technique is its relative technical simplicity without the need for extensive exposure of the ischium and ileum.
Our preliminary followup suggests the treatment of massive contained acetabular defects with no more than 50% host bone contact by TM cups is a reasonable option. However, patients should be followed closely to detect cup migration, which can occur before satisfactory bony ingrowth takes place.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Berry DJ, Müller ME. Revision arthroplasty using an anti-protrusio cage for massive acetabular bone deficiency. J Bone Joint Surg Br. 1992;74:711–715. doi: 10.1302/0301-620X.74B5.1527119. [DOI] [PubMed] [Google Scholar]
- 2.Bobyn JD, Stackpool GJ, Hacking SA, Tanzer M, Krygier JJ. Characteristics of bone ingrowth and interface mechanics of a new porous tantalum biomaterial. J Bone Joint Surg Br. 1999;81:907–914. doi: 10.1302/0301-620X.81B5.9283. [DOI] [PubMed] [Google Scholar]
- 3.Boscainos PJ, Kellett CF, Maury AC, Backstein D, Gross AE. Management of periacetabular bone loss in revision hip arthroplasty. Clin Orthop Relat Res. 2007;465:159–165. doi: 10.1097/BLO.0b013e3181560c6c. [DOI] [PubMed] [Google Scholar]
- 4.D’Antonio JA, Capello WN, Borden LS, Bargar WL, Bierbaum BF, Boettcher WG, Steinberg ME, Stulberg SD, Wedge JH. Classification and management of acetabular abnormalities in total hip arthroplasty. Clin Orthop Relat Res. 1989;243:126–137. [PubMed] [Google Scholar]
- 5.Lee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32. [PubMed] [Google Scholar]
- 6.Flecher X, Sporer S, Paprosky W. Management of severe bone loss in acetabular revision using a trabecular metal shell. J Arthroplasty. 2008;23:949–955. doi: 10.1016/j.arth.2007.08.019. [DOI] [PubMed] [Google Scholar]
- 7.Garcia-Cimbrelo E. Porous-coated cementless acetabular cups in revision surgery: a 6- to 11-year follow-up study. J Arthroplasty. 1999;14:397–406. doi: 10.1016/S0883-5403(99)90094-3. [DOI] [PubMed] [Google Scholar]
- 8.Goodman S, Pressman A, Saastamoinen H, Gross A. Modified sliding trochanteric osteotomy in revision total hip arthroplasty. J Arthroplasty. 2004;19:1039–1041. doi: 10.1016/j.arth.2004.03.023. [DOI] [PubMed] [Google Scholar]
- 9.Goodman S, Saastamoinen H, Shasha N, Gross A. Complications of ilioischial reconstruction rings in revision total hip arthroplasty. J Arthroplasty. 2004;19:436–446. doi: 10.1016/j.arth.2003.11.015. [DOI] [PubMed] [Google Scholar]
- 10.Gross AE. Restoration of acetabular bone loss 2005. J Arthroplasty. 2006;21(4 Suppl 1):117–120. doi: 10.1016/j.arth.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 11.Gross AE, Goodman SB. Rebuilding the skeleton: the intraoperative use of trabecular metal in revision total hip arthroplasty. J. Arthroplasty. 2005;20(4 Suppl 2):91–93. doi: 10.1016/j.arth.2005.03.020. [DOI] [PubMed] [Google Scholar]
- 12.Gruen TA, Poggie RA, Lewallen DG, Hanssen AD, Lewis RJ, O’Keefe TJ, Stulberg SD, Sutherland CJ. Radiographic evaluation of a monoblock acetabular component: a multicenter study with 2- to 5-year results. J Arthroplasty. 2005;20:369–378. doi: 10.1016/j.arth.2004.12.049. [DOI] [PubMed] [Google Scholar]
- 13.Kim WY, Greidanus NV, Duncan CP, Masri BA, Garbuz DS. Porous tantalum uncemented acetabular shells in revision total hip replacement: two to four year clinical and radiographic results. Hip Int. 2008;18:17–22. doi: 10.1177/112070000801800104. [DOI] [PubMed] [Google Scholar]
- 14.Malizos KN, Bargiotas K, Papatheodorou L, Hantes M, Karachalios T. Survivorship of monoblock trabecular metal cups in primary THA: midterm results. Clin Orthop Relat Res. 2008;466:159–166. doi: 10.1007/s11999-007-0008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McGann WA, Welch RB, Picetti GD., 3rd Acetabular preparation in cementless revision total hip arthroplasty. Clin Orthop Relat Res. 1988;235:35–46. [PubMed] [Google Scholar]
- 16.Merle D’Aubigné R, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am. 1954;36:451–475. [PubMed] [Google Scholar]
- 17.Saleh KJ, Holtzman J, Gafni A, Saleh L, Davis A, Resig S, Gross AE. Reliability and intraoperative validity of preoperative assessment of standardized plain radiographs in predicting bone loss at revision hip surgery. J Bone Joint Surg Am. 2001;83:1040–1046. doi: 10.2106/00004623-200107000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Schmalzried TP, Harris WH. The Harris-Galante porous-coated acetabular component with screw fixation: radiographic analysis of eighty-three primary hip replacements at a minimum of five years. J Bone Joint Surg Am. 1992;74:1130–1139. [PubMed] [Google Scholar]
- 19.Schreurs BW, Bolder SB, Gardeniers JW, Verdonschot N, Slooff TJ, Veth RP. Acetabular revision with impacted morsellised cancellous bone grafting and a cemented cup: a 15- to 20-year followup. J Bone Joint Surg Br. 2004;86:492–497. [PubMed] [Google Scholar]
- 20.Sembrano JN, Cheng EY. Acetabular cage survival and analysis of factors related to failure. Clin Orthop Relat Res. 2008;466:1657–1665. doi: 10.1007/s11999-008-0183-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Siegmeth A, Duncan CP, Masri BA, Kim WY, Garbuz DS. Modular tantalum augments for acetabular defects in revision hip arthroplasty. Clin Orthop Relat Res. 2009;467:199–205. doi: 10.1007/s11999-008-0549-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Unger AS, Lewis RJ, Gruen T. Evaluation of a porous tantalum uncemented acetabular cup in revision total hip arthroplasty: clinical and radiological results of 60 hips. J Arthroplasty. 2005;20:1002–1009. doi: 10.1016/j.arth.2005.01.023. [DOI] [PubMed] [Google Scholar]
- 23.Zicat B, Engh CA, Gokcen E. Patterns of osteolysis around total hip components inserted with and without cement. J Bone Joint Surg Am. 1995;77:432–439. doi: 10.2106/00004623-199503000-00013. [DOI] [PubMed] [Google Scholar]