Abstract
We recognized a trend of positive cultures taken from presumably uninfected shoulders during revision arthroplasty. Owing to the indolent nature of common shoulder pathogens such as Propionibacterium acnes, these cultures often become positive several days, even weeks, after surgery. Having concern regarding the potential importance of these positive cultures, we reviewed our revision arthroplasty population to determine the rate of positive intraoperative cultures in patients presumed to be aseptic, to characterize the isolated organisms, and to determine the subsequent development of infection. We retrospectively reviewed 27 patients (28 revisions) presumed to be uninfected between April 2005 and October 2007. Intraoperative cultures were positive in eight (29%) of the 28 revisions. Propionibacterium acnes was isolated in six. Methicillin-resistant Staphylococcus aureus was isolated in one patient and coagulase-negative Staphylococcus aureus was isolated in one patient. One-year followup was available on 24 of the 28 revisions. Two of the eight culture-positive revisions had a subsequent infection develop. Cultures taken at revision surgery for failed shoulder arthroplasty are often positive, and our findings document the importance of these positive cultures. Our data confirm previous reports isolating Propionibacterium acnes as a primary pathogen in revision shoulder arthroplasty.
Level of Evidence: Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Failure of shoulder arthroplasty can result from malpositioned components, instability, rotator cuff tear, periprosthetic fracture, and infection [12]. Of these causes of failure, infection is widely regarded as the most devastating, and poor results can be expected when compared with other causes of failure [4]. The incidence of infection is reportedly as much as 4% in primary unconstrained arthroplasty and 15% in revision arthroplasty [2]. Reimplantation after a previously infected arthroplasty can be accomplished once the infection has been eradicated; however, severe bone and soft tissue deficits make this a major challenge; therefore, prompt detection and appropriate treatment of infection in shoulder arthroplasty are of paramount importance [3, 6, 8].
Intraoperative cultures taken at revision surgery for presumed aseptic loosening are positive in as much as 11% of THAs [11]. Therefore, during revision shoulder arthroplasty, we routinely take multiple cultures, even if an infection is not suspected by preoperative studies or obvious by inspection at the time of surgery. We have seen a trend of positive intraoperative cultures in our revision shoulder arthroplasties presumed to be uninfected.
The purpose of this review therefore was to: (1) determine the rate of positive intraoperative cultures in the presumed uninfected revision shoulder arthroplasty, (2) characterize the isolated pathogens, and (3) determine if subsequent periprosthetic infection developed in patients with positive intraoperative cultures at 1-year followup.
Materials and Methods
All 38 patients undergoing 39 revision surgeries by one surgeon (JDK) for a failed shoulder arthroplasty (including failure caused by infection) between April 2005 and October 2007 were identified via a computerized database (Table 1). We retrospectively reviewed the charts for these 38 patients. No patient was seen in followup specifically for this study. The mean age of the group at the time of revision was 62 years (range, 43–81 years). There were 15 men and 23 women. The mean time to revision was 44.8 months (range, 3–198 months). We obtained prior Institutional Review Board approval.
Table 1.
Summary of procedures for all revisions (n = 39)
| Index procedure | Index diagnosis | Number | Reason for revision | Number |
|---|---|---|---|---|
| Hemiarthroplasty | 23 | 23 | ||
| Fracture | 15 | Obvious infection | 5 | |
| Primary osteoarthritis | 8 | Rotator cuff insufficiency | 12 | |
| Inflammatory arthritis | 1 | Glenoid arthrosis | 2 | |
| Periprosthetic fracture | 2 | |||
| Humeral loosening | 2 | |||
| Total shoulder arthroplasty | 14 | 14 | ||
| Primary osteoarthritis | 9 | Obvious infection | 4 | |
| Capsulorrhaphy arthropathy | 4 | Glenoid loosening | 5 | |
| Posttraumatic arthritis | 1 | Rotator cuff insufficiency | 4 | |
| Reverse shoulder arthroplasty | 2 | 2 | ||
| Rotator cuff arthropathy | 2 | Obvious infection | 1 | |
| Component instability | 1 |
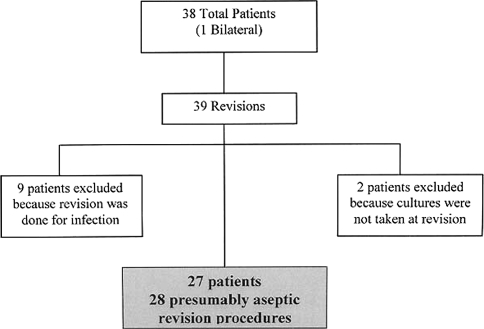
We defined a patient with a periprosthetic infection as one with an arthroplasty and any associated skin erythema, wound drainage, or obvious purulence or tissue synovitis at the time of surgery. Any patient with a clinical aspiration yielding a positive Gram stain or culture was considered infected. Also, any patient with a positive intraoperative Gram stain or frozen section showing more than five polymorphonuclear leukocytes per high-powered field was considered infected. Therefore, we excluded nine patients (five hemiarthroplasties, four total shoulder arthroplasties) infected based on these defined criteria. Two patients with hemiarthroplasties had revision surgery owing to painful rotator cuff insufficiency; however, no intraoperative cultures were taken. These two patients were excluded for this reason. With these exclusions, our cohort included 28 revision procedures in 27 patients (one patient had bilateral revisions) (Fig. 1). There were nine men and 18 women with an average age of 62 years. Two patients were lost to followup and could not be reached. Two patients refused to return for followup. Therefore, a minimum of 1-year followup (average, 22 months; range, 12–37 months) was obtained for 23 patients (24 shoulders).
Fig. 1.
A flowchart illustrates the method of obtaining the study cohort (28 presumed aseptic shoulder arthroplasty revisions).
Of the 28 revisions performed in 27 patients without clinical or intraoperative evidence of infection, 22 shoulders were revised to a reverse total shoulder arthroplasty (13 hemiarthroplasties, nine total shoulder arthroplasties); three hemiarthroplasties were revised to total shoulder arthroplasties owing to painful glenoid erosion; one reverse total shoulder arthroplasty was revised to a second reverse shoulder arthroplasty owing to instability; one painful resection arthroplasty was revised to a reverse total shoulder arthroplasty; and one total shoulder arthroplasty was revised to a hemiarthroplasty owing to glenoid component loosening.
Preoperative laboratory data, physical examination, and operative notes were reviewed. The preoperative laboratory studies reviewed were the complete blood count with differential, C-reactive protein, erythrocyte sedimentation rate, and aspiration. The leukocyte count was considered positive when it was greater than 11.0 × 109/L. The number of polymorphonuclear cells was considered positive when greater than 80% of the total leukocyte count consisted of granulocytes. The C-reactive protein was considered positive if greater than 1 dL/L, and the erythrocyte sedimentation rate was considered positive if greater than 22 mm/hour. Aspirations were considered positive if either the Gram stain or cultures were positive for organisms. The physical examination findings recorded included skin erythema, warmth, induration, and any obvious wound drainage. Operative notes were reviewed for documentation of frank purulence or worrisome synovitis at the time of the revision operation. Unless there was preoperative concern of periprosthetic infection, a preoperative dose of prophylactic intravenous antibiotic (vancomycin, 1 g) was routinely given [9]. One gram vancomycin per 40-g bag of cement was routinely mixed for fixation of the revision humeral component. Culture results were reviewed and recorded, as were the number of days lapsed before the positive cultures revealed an organism.
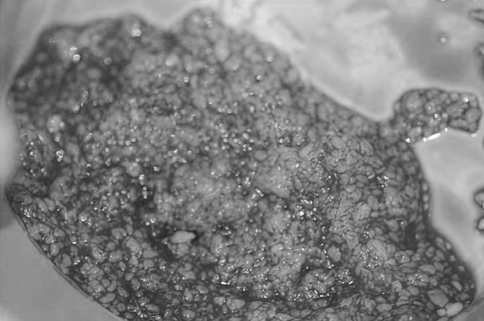
Our protocol of specimen collection for culture was as follows: any fluid encountered on entering the joint space was collected in a sterile syringe and sent for Gram stain and culture. We also routinely collected specimens from three sites: the humeral canal after stem removal, the synovial lining, and the glenoid. These specimens were sent for Gram stain and culture. Cultures are held for 14 days at our institution’s laboratory owing to the slow-growing characteristics of Propionibacterium acnes [5]. If careful inspection of the joint suggested the possibility of infection, or if tissue or bone appeared inflamed or necrotic, then each specimen was divided and ½ sent for Gram stain and culture whereas the other ½ was sent to pathology for frozen section. Any positive Gram stain or frozen section with more than five polymorphonuclear cells per high-powered field confirmed infection based on the criteria of Mirra et al. [7]. A thorough débridement was performed with placement of an antibiotic cement spacer. Frozen-section analysis was used with increasing frequency during the time for this study, but not reliably enough to report results. Regardless of Gram stain or frozen-section results, patients with suspicious findings at the time of surgery underwent two-stage reimplantation. Such findings included purulent fluid, and more subtle findings such as skin erythema, synovitis, or unidentified debris that appeared more infectious than prosthesis-derived particulate matter (Fig. 2).
Fig. 2.
Unidentified debris may appear more infectious than prosthesis-derived particulate matter, requiring histologic evaluation and culture.
Results
Eight of the 28 (29%) revision procedures yielded positive cultures. None of the 27 patients (28 revisions) had a wound problem such as warmth, erythema, or drainage. Twenty-six patients had a preoperative leukocyte count recorded in their records, and only one value was elevated. Only one of 27 patients had elevation in the number of polymorphonuclear cells. Twelve patients had a C-reactive protein level recorded, and five of the 12 were elevated. Sixteen patients had a preoperative erythrocyte sedimentation rate level recorded, and four of the 16 were elevated. Only two patients underwent aspiration, both of which were negative (Table 2).
Table 2.
Preoperative physical examination and laboratory analysis in presumed aseptic revisions
| Parameter | Number |
|---|---|
| Wound problem | 0/28 (0%) |
| Leukocyte count | 1/28 (4%) |
| Polymorphonuclear cells | 1/28 (4%) |
| Erythrocyte sedimentation rate | 4/16 (25%) |
| C-reactive protein | 5/12 (42%) |
| Positive aspiration | 0/2 (0%) |
| Purulence/synovitis | 0/28 (0%) |
Propionibacterium acnes was isolated in six of the eight. Methicillin-resistant Staphylococcus aureus was isolated in one revision and coagulase-negative Staphylococcus aureus was isolated in one revision. The number of cultures taken averaged three per revision procedure (range, 2–6 cultures) (Table 3). An average of 7 days (range, 4–10 days) was required for the cultures to show growth of an organism. Only one of the eight patients was treated with antibiotics postoperatively. This patient was given 4 weeks of oral doxycycline; however, the antibiotics were given secondary to a superficial wound infection at the iliac crest harvest site, not because of the positive intraoperative cultures. The other seven patients with positive cultures were not treated with antibiotics. At a minimum of 1-year followup, two of the eight revisions with positive intraoperative cultures had a late clinical infection (Table 3, Patients 3 and 7). Both late infections had positive cultures for Propionibacterium acnes. All four cultures grew Propionibacterium for Patient 7; however, Patient 3 had only one of four cultures positive for the organism and this was isolated in broth.
Table 3.
Positive intraoperative cultures
| Patient | Number of cultures taken | Number of positive cultures | Organism | Number of days to positive culture | Subsequent infection? (followup [months]) |
|---|---|---|---|---|---|
| 1 | 3 | 3 | Coagulase-negative Staphylococcus aureus | 2 | No (14) |
| 2 | 2 | 2 | Propionibacterium | 4 | No (24) |
| 3 | 4 | 1 | Propionibacterium | 7 | Yes (12) |
| 4 | 2 | 2 | Propionibacterium | 4 | No (25) |
| 5 | 3 | 2 | Propionibacterium | 4 | No (12) |
| 6 | 3 | 1 | Methicillin-resistant Staphylococcus aureus | 3 | No (12) |
| 7 | 4 | 4 | Propionibacterium | 4 | Yes (14) |
| 8 | 6 | 1 | Propionibacterium | 4 | No (13) |
Two patients had subsequent infections develop. Patient 7 presented with obvious clinical infection 14 months after the revision surgery, and Patient 3 presented with obvious clinical infection 12 months postrevision. Both patients initially had revision surgery for glenoid component loosening, and both subsequent infections required resection and placement of an antibiotic cement spacer.
Discussion
We recognized a trend of positive cultures taken from presumably uninfected shoulders during revision arthroplasty. Owing to the indolent nature of common shoulder pathogens such as Propionibacterium acnes, these cultures often become positive several days, even weeks, after surgery. Having concern regarding the importance of these positive cultures, we reviewed our revision arthroplasty population to (1) determine the rate of positive intraoperative cultures in patients presumed to be aseptic, (2) characterize the isolated organisms, and (3) determine the outcome of the patients with positive cultures to determine if subsequent periprosthetic infection developed at 1-year followup.
Our review has several limitations. We recognize this is a retrospective review with short followup of 1 year. There were no absolute criteria used to define a shoulder as aseptic, nor was the preoperative workup standardized for all revisions. Also, all revisions were performed by one surgeon with all cultures being interpreted in one laboratory. However, our results are similar to those reported in another study, which provides validity to our results [10].
Topolski et al. [10] reported a series of 439 revisions of which 75 (17%) had positive cultures. Propionibacterium was isolated in 45 (60%). Among our series of 28 presumably aseptic shoulder revisions, we had an even higher rate of positive cultures, 29% (eight of 28) (Table 4). Six of eight positive cultures in our series were attributable to Propionibacterium acnes. In the series of Topolski et al. [10], 10 of the 75 (13%) patients with positive cultures required rerevisions for subsequent periprosthetic infections, which were caused by Propionibacterium acnes in five of the 10 patients. At a minimum of 1-year followup, two of eight of our patients with positive cultures have required resection and antibiotic spacer for infection caused by Propionibacterium.
Table 4.
Culture-positive comparative literature
| Study | Number of positive cultures | Number of Propionibacterium acnes positive cultures | Number of subsequent infections | Number of subsequent infections Propionibacterium acnes positive |
|---|---|---|---|---|
| Topolski et al. [10] | 75/439 (17%) | 45/75 (60%) | 10/75 (13%) | 5/10 (50%) |
| Current study | 8/28 (29%) | 6/8 (75%) | 2/8 (25%) | 2/2 (100%) |
The interpretation of positive cultures in presumably aseptic revisions is problematic for several reasons. The positive cultures may be false-positive contaminants or true positives. Also, the negative results may not necessarily be true negatives, as Propionibacterium characteristically is slow to grow, averaging 11.4 days in one study [5]. Furthermore, patients without clinical infection receive antibiotics preoperatively to prevent an operatively induced infection, and this may reduce the yield of tissue cultures. Also, if the culture is a true positive, the pathogen may have been partially or wholly eradicated by the débridement and antibiotics administered during the perioperative period. However, given the incidence of Propionibacterium among shoulder infections, we tend to believe these positive cultures are more likely to be true positives. Patient 3 (Table 3) provides support for this belief, as a subsequent infection developed secondary to Propionibacterium when only one of four cultures was positive, and this was isolated in broth subculture. For Patient 7 (Table 3), all four intraoperative cultures grew Propionibacterium acnes and a subsequent infection developed 14 months later.
As the interpretation of the culture result is uncertain, the choice of treatment among patients with positive intraoperative cultures having revision surgery becomes the question. The practical options are the use of antibiotics or observation. We chose to observe our eight patients with positive cultures for two reasons. First, no signs of infection or abnormal laboratory values were present. Second, the patients had been discharged from the hospital by the time the cultures became positive and were already off antibiotics. Therefore, we chose observation unless there was some other reason to use antibiotics (one patient was treated with oral doxycycline for 3 weeks for cellulitis overlying the skin incision for iliac crest bone graft). The alternative would be to use antibiotics until the cultures are found to be negative, which would be 14 days at our institution. We ask our laboratory to maintain these cultures for this length of time because Propionibacterium takes an average of 11.4 days to grow [5]. The rationale behind using antibiotics after revision operations is that Propionibacterium may be converted from its biofilm state to a planktonic form during the operation and therefore may be susceptible to antibiotics [1]. Then patients with positive cultures could have the antibiotics continued without an interruption. Furthermore, patients could be stratified according to the number of positive cultures. Zeller et al. [13] used a criterion of two or more intraoperative cultures to diagnose a true-positive Propionibacterium infection. For example, Patient 7 (Table 3), who had all four cultures positive for Propionibacterium, might be a patient to receive intravenous antibiotics, perhaps even followed by oral suppression. Tsukayama et al. [11] treated their aseptic patients having total hip revisions with more than two positive intraoperative cultures for 6 weeks with antibiotics. They reported a 90% success rate with this intervention. Although we have not instituted such a protocol, it is being considered given that our data suggest a failure rate of two in eight for observation alone. However, such a protocol would leave patients with one positive culture untreated, such as Patient 3 (Table 3) who also had a periprosthetic infection develop.
Whether these positive cultures are true positives or false-positive contaminants is difficult to determine. However, given the fact that 25% of our cohort with positive cultures had a subsequent infection, we believe surgeons treating these patients must maintain a high index of suspicion. We are considering postoperative antibiotic treatment of all patients having revision surgery until cultures are proven negative. Patients with any number of positive cultures then would receive 6 weeks of intravenous antibiotic therapy. As these patients are followed over time, the optimal treatment for asymptomatic patients with positive cultures may become better defined.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his institution has approved the reporting of these cases, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participating in the study was obtained.
Contributor Information
James D. Kelly, II, Email: jimkelly@sfshoulder.com.
E. Rhett Hobgood, Email: rhetthobgood@msmoc.com.
References
- 1.Bayston R, Ashraf W, Barker-Davies R, Tucker E, Clement R, Clayton J, Freeman BJ, Nuradeen B. Biofilm formation by Propionibacterium acnes on biomaterials in vitro and in vivo: impact on diagnosis and treatment. J Biomed Mater Res A. 2007;81:705–709. doi: 10.1002/jbm.a.31145. [DOI] [PubMed] [Google Scholar]
- 2.Cofield RH, Edgerton BC. Total shoulder arthroplasty: complications and revision surgery. Instr Course Lect. 1990;39:449–462. [PubMed] [Google Scholar]
- 3.Crosby L. Infected total shoulder arthroplasty: two stage revision. In: Zuckerman JD, editor. Advanced Reconstruction: Shoulder. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2007. pp. 605–611. [Google Scholar]
- 4.Dines JS, Fealy S, Strauss EJ, Allen A, Craig EV, Warren RF, Dines DM. Outcomes analysis of revision total shoulder replacement. J Bone Joint Surg Am. 2006;88:1494–1500. doi: 10.2106/JBJS.D.02946. [DOI] [PubMed] [Google Scholar]
- 5.Lutz MF, Berthelot P, Fresard A, Cazorla C, Carricajo A, Vautrin AC, Fessy MH, Lucht F. Arthroplastic and osteosynthetic infections due to Propionibacterium acnes: a retrospective study of 52 cases, 1995–2002. Eur J Clin Microbiol Infect Dis. 2005;24:739–744. doi: 10.1007/s10096-005-0040-8. [DOI] [PubMed] [Google Scholar]
- 6.Mileti J, Sperling JW, Cofield RH. Reimplantation of a shoulder arthroplasty after a previous infected arthroplasty. J Shoulder Elbow Surg. 2004;13:528–531. doi: 10.1016/j.jse.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 7.Mirra JM, Amstutz HC, Matos M, Gold R. The pathology of the joint tissues and its clinical relevance in prosthesis failure. Clin Orthop Relat Res. 1976;117:221–240. [PubMed] [Google Scholar]
- 8.Norris TR, Kelly JD, Humphrey CS. Management of glenoid bone defects in revision shoulder arthroplasty: a new application of the reverse total shoulder prosthesis. Tech Shoulder Elbow Surg. 2007;8:528–531. doi: 10.1097/BTE.0b013e318030d3b7. [DOI] [Google Scholar]
- 9.Oprica C, Nord CE. European surveillance study on the antibiotic susceptibility of Propionibacterium acnes. Clin Microbiol Infect. 2005;11:204–213. doi: 10.1111/j.1469-0691.2004.01055.x. [DOI] [PubMed] [Google Scholar]
- 10.Topolski MS, Chin PY, Sperling JW, Cofield RH. Revision shoulder arthroplasty with positive intraoperative cultures: the value of preoperative studies and intraoperative histology. J Shoulder Elbow Surg. 2006;15:402–406. doi: 10.1016/j.jse.2005.10.001. [DOI] [PubMed] [Google Scholar]
- 11.Tsukayama DT, Estrada R, Gustilo RB. Infection after total hip arthroplasty: a study of the treatment of one hundred and six infections. J Bone Joint Surg Am. 1996;78:512–523. doi: 10.2106/00004623-199604000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Wirth MA, Rockwood CA., Jr Complications of total shoulder-replacement arthroplasty. J Bone Joint Surg Am. 1996;78:603–616. doi: 10.2106/00004623-199604000-00018. [DOI] [PubMed] [Google Scholar]
- 13.Zeller V, Ghorbani A, Strady C, Leonard P, Mamoudy P, Desplaces N. Propionibacterium acnes: an agent of prosthetic joint infection and colonization. J Infect. 2007;55:119–124. doi: 10.1016/j.jinf.2007.02.006. [DOI] [PubMed] [Google Scholar]