Abstract
Background:
Fire suppression activities results in cardiovascular stress, hyperthermia, and hypohydration. Fireground rehabilitation (rehab) is recommended to blunt the deleterious effects of these conditions.
Objective:
We tested the hypothesis that three rehydration fluids provided after exercise in thermal protective clothing (TPC) would produce different heart rate or core temperature responses during a second bout of exercise in TPC.
Methods:
On three occasions, 18 euhydrated firefighters (16 males, 2 females) wearing TPC completed a standardized, 50-minute bout of upper and lower body exercise in a hot room that mimicked the National Fire Protection Association (NFPA) rehabilitation guidelines of “two cylinders before rehab” (20 min work, 10 min recovery, 20 min work). After an initial bout of exercise, subjects were randomly assigned water, sport drink, or an intravenous (IV) infusion of normal saline equal to the amount of body mass lost during exercise. After rehydration, the subject performed a second bout of exercise. Heart rate, core and skin temperature, and exercise duration were compared with a two-way ANOVA.
Results:
Subjects were firefighters aged 28.2±11.3 years with a VO2peak of 37.4±3.4 ml/kg/min. 527±302 mL of fluid were provided during the rehabilitation period. No subject could complete either the pre- or post-rehydration 50-minute bout of exercise. Mean (SD) time to exhaustion (min) was longer (p<0.001) in bout 1 (25.9±12.9 min. water, 28.0±14.1 min. sport drink, 27.4±13.8 min. IV) compared to bout 2 (15.6±9.6 min. water, 14.7±8.6 min. sport drink, 15.7±8.0 min. IV) for all groups but did not differ by intervention. All subjects approached age predicted maximum heart rate at the end of bout 1 (180±11 bpm) and bout 2 (176±13 bpm). Core temperature rose 1.1±0.7°C during bout 1 and 0.5±0.4°C during bout 2. Core temperature, heart rate, and exercise time during bout 2 did not differ between rehydration fluids.
Conclusions:
Performance during a second bout of exercise in TPC did not differ when firefighters were rehydrated with water, sport drink, or IV normal saline when full rehydration is provided. Of concern was the inability of all subjects to complete two consecutive periods of heavy exercise in TPC suggesting the NFPA “two cylinders before rehab” guideline may not be appropriate in continuous heavy work scenarios.
Keywords: Cardiovascular strain, Thermal Stress, Performance, Hydration
Introduction
Mild or moderate heat strain experienced by firefighters is a complex condition consisting of progressive hypohydration coupled both with external heat and continuous endogenous heat production. Heat is produced at a greatly accelerated rate when firefighters perform strenuous activities in hot environments while wearing protective gear that inhibits the body's ability to shed this additional thermal burden.1, 2 This results in an elevated core temperature and cardiovascular strain.
Maintenance of euhydration ensures that the blood plasma volume is sufficient to bring excess body heat to the skin surface thereby facilitating evaporative cooling. Continued sweating without fluid replacement reduces plasma volume, which progressively impairs thermoregulation. Subsequently, the heart rate increases and beats with greater contractile force to compensate for the loss of plasma volume. When fluid losses are not adequately replaced following exertion, the heart will need to work harder in order to compensate for the thermal stress. If this burden is maintained over a prolonged period of time, the cardiovascular strain that is induced may become detrimental.3 In some cases, an uncompensated heat stress may occur, placing the individual in danger of exertional heat illness.
The National Fire Protection Association (NFPA) has produced a standard for on-scene rehabilitation (Fireground Rehab) of firefighters working at an incident or training exercise including recommendations for rehydration.4 The standard recommends formal fireground rehabilitation when the firefighter 1) consumes two 30-minute air cylinders during fire suppression activities, 2) one 45-minute cylinder, or 3) completes 40 minutes of heavy work without self-contained breathing apparatus (SCBA). The standard also requires that emergency medical care be available “as part of the incident scene rehabilitation for the evaluation and treatment of members.”.
The optimal rehydration strategy for firefighters working in thermal protective clothing (TPC) is unknown. This study examined rehydration with water, sport drink, and intravenous (IV) normal saline following exercise in TPC using a protocol designed to mimic the timing of a common work-rest ratio to determine an optimal strategy to enhance the duration of exercise, heart rate response, or temperature response during a subsequent bout of exercise in TPC.
Methods
The University of Pittsburgh Institutional Review Board approved this prospective laboratory trial. Methods presented have been previously described by our group.5, 6
Study Design and Population
Eighteen firefighters (16 males, 2 females) were recruited and provided written informed consent. Prior to entering the protocol, subjects reported to the lab for a physical exam and an exercise stress test. In addition to a physical exam, subjects provided a blood sample for a fasting lipid profile and had body fat percentage measured by three site skinfold analysis.7 Subjects were recruited using a flyer mailed to every fire department listed with the county fire academy. Inclusion criteria were age 18-45 years and NFPA certified firefighter while the exclusion criteria were existing heart or respiratory disease, medications known to alter cardiac response to exercise or thermoregulation, previous abdominal surgery, or renal disease. Subjects were compensated $100 after completing each protocol.
Exercise Stress Test
Subjects performed a modified Storer-Davis protocol graded exercise stress test on a Monark 828E cycle ergometer (Vansbro, Sweden) to determine aerobic capacity and cardiovascular function.8 Female subjects were required to take a urine pregnancy test prior to each testing day and excluded if a positive result was confirmed. Subjects were asked to refrain from caffeine, tobacco, and exercise 12 hours before the stress test. During testing, an open circuit spirometer (MedGraphics Cardiorespiratory Diagnostic System with Breeze Suite Software, St. Paul, MN) calculated breath by breath analysis of oxygen consumption (VO2) carbon dioxide production (VCO2), respiratory exchange ratio (RER), ventilation, and respiratory rate. The electronic analyzers were calibrated prior to each exercise test using standard reference gases. A twelve-lead ECG was obtained every three minutes during the protocol and post exercise. A cardiologist interpreted test results to identify ischemic changes.
Testing Protocol
The testing protocol was designed to mimic an extended period of fire suppression that complied with the NFPA 1584: Standard on the Rehabilitation Process for Members During Operations and Training Exercises which recommends that firefighters use a maximum of two breathing air cylinders before submitting to on-scene rehabilitation (approximately 50 minutes total including the cylinder change) prior to a second work period.4 Other than the group assignment of rehydration fluid (water, sport drink, normal saline) received during rehabilitation, all testing days were identical. The order of the rehydration fluid delivered over three visits was predetermined by random assignment.
Subjects reported to the lab between 0800 and 1100 hours on three separate occasions, each visit separated by at least one week, to perform an exercise protocol in TPC. The lab was heated to 33.0 ± 1.64°C and 13.9 ± 7.0% relative humidity. Subjects were instructed to abstain from any food intake the morning of testing and were asked to refrain from alcohol, nicotine and caffeine for at least 12 hours before testing. Urine specific gravity (USG) was measured via hand-held refractometer (ATAGO Ltd, Bellevue, WA) when the subject reported to the lab. Subjects were required to be well hydrated (USG ≤ 1.025). Subjects were weighed in short pants (women short pants and sport bra). To assure equivalent pre-exercise nutrition, subjects received a standardized diet of 1 g/kg of body weight of carbohydrates of meal replacement bars (Clif Bar, Berkeley CA) and 400-600 ml of water one hour before testing.
Subjects were dressed in standard station wear (cotton-poly long pants, 100% cotton t-shirt) prior to donning the uniform and TPC. Subjects donned standardized thermal protective clothing consisting of turnout pants and coat (Body guard, Lion Apparel, Dayton OH), Nomex® hood (Majestic Fire Apparel, Leighton PA), rubber bunker boots (Servus, Rock Island, IL), polycarbonate helmet (Paul Conway, Dayton, OH), and leather gloves. Subjects wore SCBA (Firehawk®, MSA, Pittsburgh, PA). The SCBA mask was worn during the protocol but left open to room air. After donning TPC and SCBA, subjects stood on the treadmill while baseline measures of heart rate, respiratory rate, core and skin temperature were assessed.
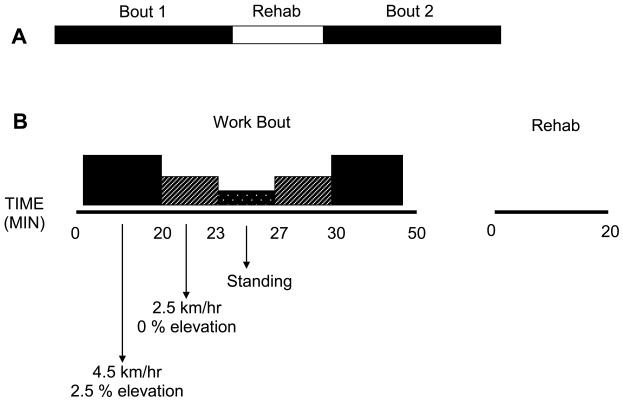
Subjects performed a treadmill exercise protocol adapted from a previous study of firefighter response to cooling devices that was designed to simulate fire suppression (Figure 1).9 Subjects initially walked at 4.5 km/hr on a 2.5% incline to mimic the exertion of fire suppression. Different from the original protocol, subjects were instructed to carry an 8.1 kg bar (6.8 kg for females) above waist height for one minute out of every three minutes to simulate cyclical upper body activity. After 20 minutes the treadmill was lowered to a level position and the speed was decreased to 2.5 km/hr for three minutes to mimic exiting the fire structure followed by a four minute standing period to simulate changing the SCBA cylinder. Following the standing period, the subjects again walked at 2.5 km/hr on a 0% incline for three minutes followed by a 20 minute bout of walking at 4.5 km/hr on a 2.5% incline to simulate returning to the fire structure for a second period of fire suppression. Total protocol length was a 50 minutes (BOUT 1). Subjects ended BOUT 1 when they completed the 50-minute protocol or when one of the following termination criteria were achieved 1) respiratory rate > 60 breaths per min, 2) heart rate exceeded age predicted maximum (220-age) – 10 bpm, 3) core temperature > 39.5°C, 4) unsteady gait making it unsafe to continue treadmill exercise, or 5) subject request for volitional fatigue. Heart rate, respiratory rate, core temperature, and skin temperature (chest, back, triceps, and anterior thigh) were recorded every two minutes during exercise.
Figure 1.
Protocol timeline for subjects performing heavy exercise in thermal protective clothing and self-contained breathing apparatus. A: Total protocol was two 50-minute exercise periods separated by 20-minute rehabilitation period. B: Timeline and representation of work intensity during a single 50-minute bout.
At the end of BOUT 1, subjects exited the heated room and doffed TPC. Subjects were immediately weighed in short pants. They were then instructed to rest in the semi-fowler position for a 20-minute period. Subjects received rehydration volume equal to the mass lost during exercise. For subjects who lost less than 0.2 kg, 200 ml of fluids were provided. Subjects received room temperature water, room temperature sport drink (Gatorade, Chicago, IL) or 37°C, 0.9% saline via peripheral intravenous catheter placed in a superficial arm vein). Subjects were again weighed in shorts, donned the uniform, TPC, and SCBA and returned to the heated room. A second 50-minute period of treadmill exercise was administered (BOUT 2). At the conclusion of the second phase all subjects doffed gear, were weighed a final time in shorts, and monitored until recovered.
Physiological Measures
Subjects were fitted with a heart rate monitor (Polar Electro – USA, NY) placed around the chest. Core temperature was measured with an indigestible pill and radio receiver (HQ Inc, FL). Subjects took the pill eight hours before arrival to minimize the confounding influence of recently consumed food or fluid.10 This device provides a core temperature measurement that is intermediate to rectal and esophageal temperature.11 Skin thermistors (Physitemp, NJ) were applied over the supraspinatis, triceps brachii, the clavicular head of the pectoralis major, and the anterior quadriceps femoris muscles to calculate skin temperature measurements. Mean skin temperature was calculated by using the formula, Tsk = chest (0.25) + back(0.25) + thigh(0.3) + arm (0.2).12
Data analysis
Data were compared with a two-way ANOVA (time × condition). Vital signs and temperature were compared at pre and post BOUT1, pre and post rehab, and pre and post BOUT2. Analyses were performed with SPSS v11 for Mac (Chicago, IL) with significance set at p ≤ 0.05. Based on the previous work with a similar work examining firefighter cooling, an a priori power calculation indicated that 15 subjects would allow us to spot differences during exercise or recovery for core temperature of 1°C ± 0.5 and for heart rate of 20 bpm ± 10.9
Results
All subjects were credentialed as NFPA Firefighter I or Firefighter II. Ten subjects served as volunteers while eight were career firefighters. Subject demographics and morphometrics are shown in Table 1. On average, males were heavier than females. Both female subjects took oral contraceptives and were allowed to schedule protocol visits without regard to menstrual cycle. Peak oxygen consumption from the cycle test indicates that subjects were moderately fit and was consistent with other cohorts of public safety providers studied in our lab.5, 6
Table 1.
Subjects demographics and morphometrics.
| Age (yrs) | Height (cm) | Weight (kg) | Body Fat (%) |
VO2peak (ml/kg/min) |
Total Cholesterol (mg/dL) |
|
|---|---|---|---|---|---|---|
| Males (16) | 30.9 ± 8.6 | 174.6 ± 9.0 | 93.9 ± 10.8* | 20.1 ± 5.3 | 37.9 ± 3.7 | 170.6 ± 31.6 |
| Females (2) | 22.0 ± 4.2 | 161.5 ± 6.4 | 56.5 ± 4.9 | 23.0 5.7 | 36.6 ± 6.0 | 156.5 ± 9.2 |
Data presented as mean ± SD.
= different from female subjects (p < 0.001).
Performance
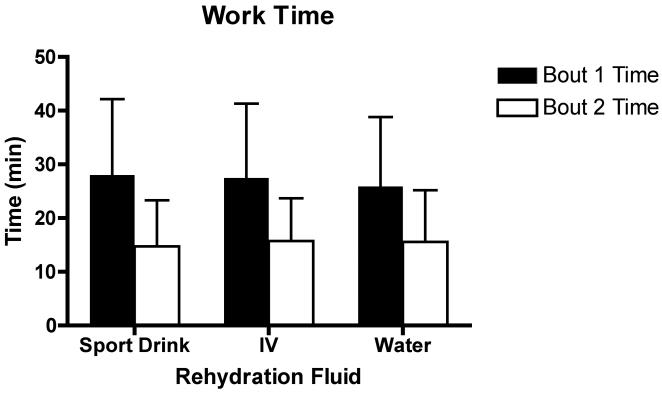
No subject could complete the 50-minute exercise protocol either before or after rehabilitation. On average, exercise duration during BOUT 1 was less than 30 minutes in duration and did not differ among the three visits (Figure 2). Exercise duration during BOUT 2 was shorter than BOUT 1 (p < 0.001) but did not differ by rehydration fluid. For all trials (BOUT 1 and Bout 2 combined) exercise duration was limited by the heart rate criteria (57.4% of trials) or volitional fatigue (39.8%). Three trials were stopped on the core temperature criteria. For BOUT 1, all but four cases of volitional fatigue terminations (20%) were within 10 bpm of reaching the heart rate termination criteria. More subjective fatigue was displayed in BOUT 2 with 13 volitional fatigue terminations (56.5%) ending more than 10 bpm from the heart rate termination criteria. There was no association between cardiorespiratory fitness (VO2peak) and reason for terminating exercise.
Figure 2.
Work time (in minutes) for treadmill exercise in TPC before rest and rehydration (bout 1) and after (bout 2). Bout 1 was significantly longer than bout 2 (p < 0.001). Neither bout differed among rehydration fluids. Data presented as mean ± SD.
Change in body mass
Change in body water was assumed to be approximately equal to change in body mass.13 Following BOUT 1, mass decreased by 0.48 ± 0.32 kg in the sport drink arm, 0.53 ± 0.32 kg in the water arm, and 0.58 ± 0.33 kg in the IV arm. These values did not differ between groups and were used to prescribe the rehydration volume. All subjects consumed the prescribed volume during the 20-minute rehab period.
Vital signs
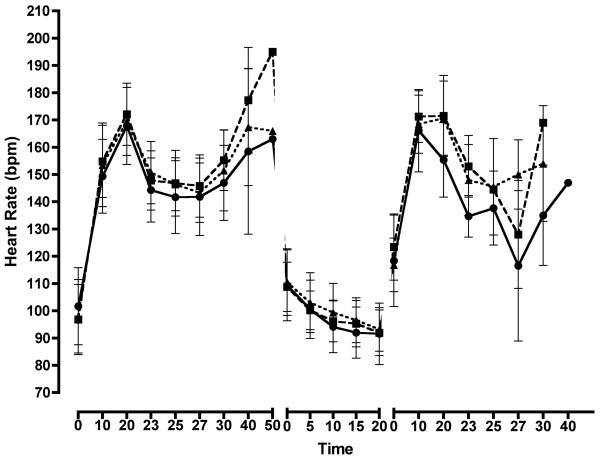
Vital signs during, before, and after exercise and rehabilitation are shown in Table 2. Heart rate rose as the duration of exercise was prolonged (Figure 3). Two peaks are seen in both BOUT 1 and BOUT 2. The first peak corresponds to less fit subjects approaching heart rate maximum immediately before ceasing exercise while the second peak corresponds to more fit subjects approaching heart rate maximum later in the protocol. Heart rate changed over time increasing during exercise and partially recovering during the rehabilitation period (F=662.7, p < 0.001) but did not differ by rehydration fluid (F=0.08, p = 0.27). Respiratory rate increased over time (F=80.7, p < 0.001) but did not differ by condition (F=1.6, p = 0.20).
Table 2.
Vital signs and temperatures before and after exercise in TPC and rehabilitation
| BOUT 1 start |
BOUT 1 stop |
REHAB start |
REHAB stop |
BOUT 2 start |
BOUT 2 stop |
|
|---|---|---|---|---|---|---|
| Heart rate (bpm) | ||||||
| Sport Drink | 97 ± 13 | 179 ± 12 | 109 ± 9 | 92 ± 8 | 123 ± 12 | 178 ± 11 |
| IV | 98 ± 13 | 181 ± 9 | 111 ± 12 | 93 ± 8 | 117 ± 10 | 176 ± 14 |
| Water | 102 ± 14 | 179 ±11 | 109 ± 13 | 92 ± 11 | 118 ± 17 | 174 ± 16 |
| Resp. rate (bpm) | ||||||
| Sport Drink | 18.3 ± 4.9 | 35.3 ± 9.9 | 18.2 ± 4.4 | 16.5 ± 2.8 | 20.8 ± 5.3 | 33.3 ± 6.0 |
| IV | 19.4 ± 5.5 | 33.7 ± 6.2 | 18.3 ± 5.4 | 15.3 ± 4.7 | 21.4 ± 6.5 | 33.0 ± 10.4 |
| Water | 20.1 ± 5.4 | 31.8 ± 5.7 | 18.3 ± 5.5 | 16.9 ± 2.3 | 20.0 ± 5.0 | 32.3 ± 6.1 |
| Tc (°C) | ||||||
| Sport Drink | 37.0 ± 0.5 | 38.1 ± 0.8 | 38.3 ± 0.8 | 37.6 ± 0.5 | 37.6 ± 0.4 | 37.9 ± 0.5 |
| IV | 37.0 ± 0.3 | 38.2 ± 0.6 | 38.5 ± 0.6 | 37.8 ± 0.5 | 37.5 ± 0.4 | 38.1 ± 0.6 |
| Water | 37.1 ± 0.6 | 38.3 ± 0.6 | 38.4 ± 0.6 | 37.6 ± 0.5 | 37.6 ± 0.5 | 38.2 ± 0.5 |
| Tsk (°C) | ||||||
| Sport Drink | 34.6 ± 0.8 | 37.7 ± 1.1 | 36.6 ± 0.8 | 35.9 ± 0.7 | 35.6 ± 0.7 | 37.3 ± 0.7 |
| IV | 35.0 ± 0.8 | 37.9 ± 0.7 | 36.8 ± 0.7 | 36.2 ± 0.6 | 35.6 ± 0.7 | 37.9 ± 0.8 |
| Water | 34.3 ± 0.8 | 37.5 ± 1.0 | 36.4 ± 1.0 | 35.5 ± 0.7 | 35.0 ± 0.8 | 37.0 ± 1.0 |
Data presented as mean ± SD. Tc = Core temperature, Tsk = Mean skin temperature. All variables increased during exercise and partially recovered during rehab. Bout 1 stop and Bout 2 stop did not differ.
Figure 3.
Heart rate response during exercise in TPC before rest and rehydration (left segment), during rest and rehydration (middle segment), and during a bout of work after (right segment). Data present as mean ± SD for sport drink (square), IV (triangle), and water (circle). Heart rate increased during exercise and partially recovered during rehab. Bout 1 stop and Bout 2 stop did not differ. Data did not differ by rehydration fluid.
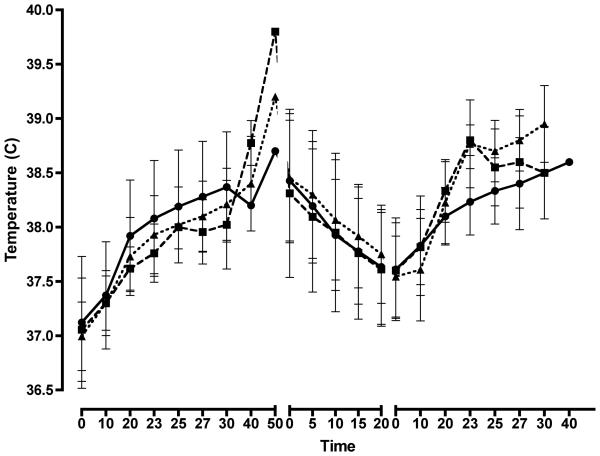
Temperature
Core temperature increased over time (F=50.2, p < 0.001) and partially recovered during the rehabilitation period (Figure 3). Typically, there was approximately 1.0°C rise in core temperature during BOUT 1 and a 0.5°C rise during BOUT2 (Table 2). There were no differences by rehydration fluid (F=0.88, p = 0.11).
Mean skin temperature rose during both bouts and partially recovered during the rehabilitation phase (F=83.3, p < 0.001). Mean skin temperature was lower during the water trial when compared to both the sport drink and IV trial (F=10.3, p < 0.001). However, the magnitude of the differences was typically less than 0.5°C (Table 2).
Discussion
We have shown that generally fit firefighters were unable to complete 50 minutes of heavy treadmill exercise in TPC. Furthermore, we demonstrated that performance during a second bout of treadmill exercise is not altered by the choice of rehydration fluid (water, sport drink, or intravenous fluid) when full rehydration is provided.
A bout of treadmill exercise, followed by a period of rehab, followed by a second bout of treadmill exercise cannot entirely mimic the demands of fire suppression but it is similar to the work-rest ratios commonly employed by the fire service and has been used in other studies of firefighter physiology.9 The inability of firefighters to complete the 50-minute work period seen in this study was not anticipated. The exercise protocol was adapted from a previous study of firefighters performed in Toronto, Ontario.9 In the Toronto study, the mean combined work time ranged from 78.0 to 124.7 minutes with all subjects completing the first 50-minute bout. The Toronto cohort was leaner and possessed a high cardiorespiratory capacity than our subjects. This has been shown to result in longer exercise duration during uncompensable heat stress.14
However, the addition of the upper body exercise to this protocol increased the intensity of the exercise and likely played an important role in limiting exercise duration. In terms of myocardial performance, the relative inefficiency of upper arm exercise is known to contribute to myocardial oxygen supply/demand imbalance and raise heart rate.15 Arm exercise has been shown to precipitate angina pectoris and/or ischemic ECG changes at lower external workloads than those of leg exercise.16 However, as nearly every element of fire suppression (e.g. advancing hose, forcing entry, pulling ceiling) involves significant upper body activity we felt it was important to add upper body exertion to the protocol.17, 18 Additionally, the continuous nature of treadmill exercise made it impossible for our subjects to self pace or regulate their activity as may be done during fire suppression. The protocol in this report typified a heavy exertion scenario that reduced exercise duration. EMS practitioners and fire service personnel should recognize the possibility of continuous heavy exertion during certain fire suppression scenarios (e.g. victim rescue) and be prepared to shorten work times and increase the frequency and/or duration of fireground rehab.19
It has been known since the 1940s that failing to replace fluids during exercise in the heat impairs performance and results in a continuous rise in core body temperature.20 In a previous study of healthy, heat acclimated men performing 50-minutes of work in a hot environment, it was shown that hypohydration of 5% body weight results in a thermal burden even at low workloads and imposes cardiovascular strain that increases with exercise intensity.21 Considering the known thermal burden associated with structural firefighting, it is critically important for firefighters to maintain euhydration during their shift and aggressively replace fluid losses during fireground rehab even if fluid choice is less important. The fluid losses of subjects in the present report were relatively modest following BOUT 1. This is likely the result of the short exercise duration achieved by our cohort of subjects.
To our knowledge, this is the first study comparing rehydration fluid choices in firefighters. A previous study of soldiers performing three hours of intermittent marching found that carbohydrate containing beverages increased blood glucose, prevented hypoglycemia, and prevented central fatigue but did not alter hydration status or physiological function when fluid losses were matched with intake.22 In contrast, other studies have reported both improved endurance time and improved sprint performance following carbohydrate-containing solution when compared to water.23, 24 Although performance benefits were not seen in the present study, it is generally accepted that in athletes, a carbohydrate containing solution should be employed for longer duration events and training.25 There may be physiologic benefits to carbohydrate containing solutions that are not directly addressed by these data.
Comparisons of intravenous versus oral rehydration in athletes have failed to support the theoretical benefit of the intravenous route. Four studies have utilized 0.45% (half-normal) saline for rehydration after endurance exercise.26-29 In these studies, oral rehydration was equivalent or superior to intravenous rehydration with regards to performance. In one study examining rapid rehydration over 20 minutes, lower mean skin and core temperature were reported after oral rehydration when compared to intravenous rehydration.26 However, this may be due to the chilled serving temperature of the oral fluid whereas in the present study, oral fluids were served at room temperature and saline was administered at body temperature to avoid the confounding effects of cooling on performance. While we did not identify a performance benefit with intravenous saline there may be advantages from an operational standpoint in that greater volumes of fluid may be administered in short time intervals. The average fluid loss seen in these data was approximately 0.5 L and can easily be consumed in 20-30 minutes. However, in other studies of first responders completed in our lab we have reported fluid losses of more than one liter, which may be difficult to consume in a typical fireground rehab period.6
Limitations
There are limitations that should be considered when interpreting these data. The physical plant of our laboratory did not allow nude weights to be obtained nor did we weigh the short pants and undergarments separately. Therefore, it is likely that the mass loss was underestimated. Subjects were asked to bring the same clothing to each protocol to limit the variance of this underestimation. Previous work has shown that fluid replacement of at least 81% of fluid lost during exercise is required to offset hypohydration induced changes in heart rate, core temperature, and stroke volume.30 It is unlikely that the underestimation of body mass change due to wearing short pants during the weighing exceeded 20% of the true loss.
Our subjects were typical of firefighters in Western Pennsylvania. All were certified and currently working or volunteering as a firefighter in the community. However, they may not be representative of firefighters across the United States. While this study may be replicated in other laboratories with different cohorts, the difficulty in obtaining high-quality physiological data in the field precludes the possibility of a field trial of rehydration.
We did not limit shift work the evening before a protocol. Regardless of potential responses the night before, subjects had to meet the fasting and USG requirements the morning of a protocol. In spite of this, it is possible that a subject may have been fatigued during a protocol visit. Finally, although typical TPC was worn during exercise, the subjects did not breathe pressurized air in any trial.
Conclusion
Performance during a second bout of exercise in TPC did not differ when firefighters were rehydrated with water, sport drink, or IV normal saline when adequate rehydration is provided. Additionally, no subject was able to complete two, consecutive 50-minute periods of heavy exertion in TPC suggesting the NFPA “two cylinders before rehab” guideline may not be appropriate in all scenarios.
Figure 4.
Core body temperature response during exercise in TPC before rest and rehydration (left segment), during rest and rehydration (middle segment), and during a bout of work after (right segment). Data present as mean ± SD for sport drink (square), IV (triangle), and water (circle). Core temperature increased during exercise and partially recovered during rehab. Bout 1 stop and Bout 2 stop did not differ. Data did not differ by rehydration fluid.
Acknowledgments
This study was funded by the FEMA Assistance to Firefighters Grant Program (EMW-2006-FP-02245). This study was also supported in part by Grant Number UL1 RR024153 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official view of FEMA, NCRR, or NIH. The authors gratefully acknowledge Lion Apparel and Mine Safety Appliance for generous equipment grants to support this study.
References
- 1.Bilzon JL, Scarpello EG, Smith CV, Ravenhill NA, Rayson MP. Characterization of the metabolic demands of simulated shipboard Royal Navy fire-fighting tasks. Ergonomics. 2001;44:766–80. doi: 10.1080/00140130118253. [DOI] [PubMed] [Google Scholar]
- 2.Selkirk GA, McLellan TM. Physical work limits for Toronto firefighters in warm environments. J Occup Environ Hyg. 2004;1:199–212. doi: 10.1080/15459620490432114. [DOI] [PubMed] [Google Scholar]
- 3.Coris EE, Ramirez AM, Van Durme DJ. Heat illness in athletes: the dangerous combination of heat, humidity and exercise. Sports Med. 2004;34:9–16. doi: 10.2165/00007256-200434010-00002. [DOI] [PubMed] [Google Scholar]
- 4.National Fire Protection Association . NFPA 1584: Standard on the Rehabilitation Process for Members During Emergency Operations and Training Exercises. National Fire Protection Association; Quincy, MA: 2007. [Google Scholar]
- 5.Northington WE, Suyama J, Goss FL, Randall C, Gallagher M, Hostler D. Physiological responses during graded treadmill exercise in chemical-resistant personal protective equipment. Prehosp Emerg Care. 2007;11:394–8. doi: 10.1080/10903120701536933. [DOI] [PubMed] [Google Scholar]
- 6.Hostler D, Gallagher M, Jr., Goss FL, et al. The effect of hyperhydration on physiological and perceived strain during treadmill exercise in personal protective equipment. Eur J Appl Physiol. 2009;105:607–13. doi: 10.1007/s00421-008-0940-2. [DOI] [PubMed] [Google Scholar]
- 7.Jackson AS, Pollock ML. Generalized equations for predicting body density of men. Brit J Nutr. 1978;40:497–504. doi: 10.1079/bjn19780152. [DOI] [PubMed] [Google Scholar]
- 8.Storer TW, Davis JA, Caiozzo VJ. Accurate prediction of VO2max in cycle ergometry. Med Sci Sports Exerc. 1990;22:704–12. doi: 10.1249/00005768-199010000-00024. [DOI] [PubMed] [Google Scholar]
- 9.Selkirk GA, McLellan TM, Wong J. Active versus passive cooling during work in warm environments while wearing firefighting protective clothing. J Occup Environ Hyg. 2004;1:521–31. doi: 10.1080/15459620490475216. [DOI] [PubMed] [Google Scholar]
- 10.Wilkinson DM, Carter JM, Richmond VL, Blacker SD, Rayson MP. The effect of cool water ingestion on gastrointestinal pill temperature. Med Sci Sports Exerc. 2008;40:523–8. doi: 10.1249/MSS.0b013e31815cc43e. [DOI] [PubMed] [Google Scholar]
- 11.O'Brien C, Hoyt RW, Buller MJ, Castellani JW, Young AJ. Telemetry pill measurement of core temperature in humans during active heating and cooling. Med Sci Sports Exerc. 1998;30:468–72. doi: 10.1097/00005768-199803000-00020. [DOI] [PubMed] [Google Scholar]
- 12.Ayling JH. Regional rates of sweat evaporation during leg and arm cycling. Br J Sports Med. 1986;20:35–7. doi: 10.1136/bjsm.20.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baker LB, Lang J, Larry Kenney W. Change in body mass accurately and reliably predicts change in body water after endurance exercise. Eur J Appl Physiol. 2009;105:959–67. doi: 10.1007/s00421-009-0982-0. [DOI] [PubMed] [Google Scholar]
- 14.Cheung SS, McLellan TM. Heat acclimation, aerobic fitness, and hydration effects on tolerance during uncompensable heat stress. J Appl Physiol. 1998;84:1731–9. doi: 10.1152/jappl.1998.84.5.1731. [DOI] [PubMed] [Google Scholar]
- 15.Franklin B, Bonzheim K. Snow shoveling: a trigger for acute myocardial infarction and sudden coronary death. Am J Cardiol. 1996;77:855–8. doi: 10.1016/S0002-9149(97)89181-3. al e. [DOI] [PubMed] [Google Scholar]
- 16.Wahren J, Bygdeman S. Onset of angina pectoris in relation to circulatory adaptation during arm and leg exercise. Circulation. 1971;4:432–41. doi: 10.1161/01.cir.44.3.432. [DOI] [PubMed] [Google Scholar]
- 17.Mendenhall D, Moffatt S. Validation of a physical work performance evaluation for incumbant firefighters. Fire Engineering. 2005;12:51–8. al e. [Google Scholar]
- 18.Rhea M, Alvar B. Physical fitness and job performance of firefighters. J Strength Cond Res. 2004;18:348–52. doi: 10.1519/R-12812.1. al e. [DOI] [PubMed] [Google Scholar]
- 19.von Heimburg ED, Rasmussen AK, Medbo JI. Physiological responses of firefighters and performance predictors during a simulated rescue of hospital patients. Ergonomics. 2006;49:111–26. doi: 10.1080/00140130500435793. [DOI] [PubMed] [Google Scholar]
- 20.Pitts G, Johnson R, Consolazio F. Work in heat as affected by intake of water, salt and glucose. Am J Physiol. 1944;142:253–9. [Google Scholar]
- 21.Montain SJ, Latzka WA, Sawka MN. Control of thermoregulatory sweating is altered by hydration level and exercise intensity. J Appl Physiol. 1995;79:1434–9. doi: 10.1152/jappl.1995.79.5.1434. [DOI] [PubMed] [Google Scholar]
- 22.Byrne C, Lim CL, Chew SA, Ming ET. Water versus carbohydrate-electrolyte fluid replacement during loaded marching under heat stress. Mil Med. 2005;170:715–21. doi: 10.7205/milmed.170.8.715. [DOI] [PubMed] [Google Scholar]
- 23.Welsh RS, Davis JM, Burke JR, Williams HG. Carbohydrates and physical/mental performance during intermittent exercise to fatigue. Med Sci Sports Exerc. 2002;34:723–31. doi: 10.1097/00005768-200204000-00025. [DOI] [PubMed] [Google Scholar]
- 24.Gant N, Leiper JB, Williams C. Gastric emptying of fluids during variable-intensity running in the heat. International journal of sport nutrition and exercise metabolism. 2007;17:270–83. doi: 10.1123/ijsnem.17.3.270. [DOI] [PubMed] [Google Scholar]
- 25.von Duvillard SP, Braun WA, Markofski M, Beneke R, Leithauser R. Fluids and hydration in prolonged endurance performance. Nutrition. 2004;20:651–6. doi: 10.1016/j.nut.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 26.Casa DJ, Maresh CM, Armstrong LE, et al. Intravenous versus oral rehydration during a brief period: responses to subsequent exercise in the heat. Med Sci Sports Exerc. 2000;32:124–33. doi: 10.1097/00005768-200001000-00019. [DOI] [PubMed] [Google Scholar]
- 27.Castellani JW, Maresh CM, Armstrong LE, et al. Intravenous vs. oral rehydration: effects on subsequent exercise-heat stress. J Appl Physiol. 1997;82:799–806. doi: 10.1152/jappl.1997.82.3.799. [DOI] [PubMed] [Google Scholar]
- 28.Kenefick RW, O'Moore KM, Mahood NV, Castellani JW. Rapid IV versus oral rehydration: responses to subsequent exercise heat stress. Med Sci Sports Exerc. 2006;38:2125–31. doi: 10.1249/01.mss.0000235358.39555.80. [DOI] [PubMed] [Google Scholar]
- 29.Maresh CM, Herrera-Soto JA, Armstrong LE, et al. Perceptual responses in the heat after brief intravenous versus oral rehydration. Med Sci Sports Exerc. 2001;33:1039–45. doi: 10.1097/00005768-200106000-00025. [DOI] [PubMed] [Google Scholar]
- 30.Coyle EF, Montain SJ. Carbohydrate and fluid ingestion during exercise: are there trade-offs? Med Sci Sports Exerc. 1992;24:671–8. [PubMed] [Google Scholar]