Abstract
The purpose of this research was to determine barriers that prevent participation in an employee wellness program, Wellness Wednesdays: "Eat & Meet" About Healthy Living, conducted at East Carolina University (ECU) in Greenville, North Carolina. All ECU ARAMARK employees (n = 481) over the age of 18 were eligible to participate in the wellness program. Weekly 30 minute classes, taught by a Registered Dietitian, on various nutrition- and health-related topics were conducted for 10-weeks. Five question knowledge quizzes were administered to participants at the end of each class to determine the comprehension of material presented. Qualitative interviews (n = 19) were conducted with employees (participants and non-participants) and the program organizer after the completion of the 10-week program to identify barriers to program participation. A total of 50 (10.4% of the total number of potential participants) ECU ARAMARK employees, managers, and leadership team directors attended Wellness Wednesdays at least once during the 10-week program. Employees, on average, scored 71-100% on the weekly knowledge quizzes administered at the end of each class. The most common barriers to participation reported included (most often to least often reported): insufficient incentives, inconvenient locations, time limitations, not interested in topics presented, undefined reasons, schedule, marketing, health beliefs, and not interested in the program. Results showed that employee wellness programs can be effective in increasing knowledge of employees on nutrition- and health-related topics. However, program planning that addresses identified barriers including insufficient incentives, inconvenient locations, and time limitations may facilitate higher participation in future worksite wellness opportunities.
Keywords: Employee wellness, barriers, participation rates
Introduction
The leading causes of death in the United States include heart disease, cancer, and stroke [1]; the incidence of these conditions can be reduced by modifying and/or eliminating associated risk factors [2]. The majority (66.3%) of U.S. adults 20 years and older are overweight or obese and 32.2% are obese [3]. A shift towards more sedentary lifestyles and occupations and increased reliance on and use of labor-saving devices [4] may be associated with the increased prevalence of obesity and chronic disease [5]. Obesity is a major issue for corporate society because of the economic impact, negative effects on work performance, and other potentially serious risks and complications associated with obesity [6].
Most adults may spend more time during the day at work than anywhere else. Therefore, it may be important for worksites to be more conducive to employee health and is an excellent place to promote health and wellness. According to the Wellness Councils of America, more than 81% of businesses with more than 50 employees have some type of health promotion program in place [7]. Employee wellness centers have been shown to provide numerous benefits for employees including: weight reduction, increased physical fitness and stamina [8], and decreased stress [9]. Recent research has also discovered that employers benefit from such programs [10] by experiencing reduced healthcare costs, increased productivity, reduced incidence of sickness and absenteeism [11], improved recruitment [10], decreased turnover rates, and enhanced employee morale [12]. A review of over 70 published research articles on worksite wellness programs found that, on average, employers experience a $3.50-$1.00 savings-to-cost ratio (reduced absenteeism and health care costs compared to program costs) because of wellness programs [7]. On average, research has shown that there is a 28% reduction in sick leave and absenteeism, a 26% reduction in health care costs, and a 30% reduction in worker's compensation claims [11].
Comprehensive worksite wellness programs provide ongoing and integrated programs of health promotion and disease management, with individualized risk reduction for employees as a crucial element [13]. This integrated approach has been found to be much more effective in preventing disease and promoting overall health than addressing each issue separately [14]. Worksites are an ideal setting for health behavior change because they offer access to employees through controlled environmental and communication support systems [15] and a large number of people can be repeatedly reached over an extended period of time [5,16]. By utilizing the built-in social support found in the workplace, recognizing that there are varying levels of influence (intrapersonal, interpersonal, institutional, community), and addressing employee preferences and perceived barriers, the likelihood of achieving and maintaining better health and well-being will be significantly increased [17]. Other factors found to be crucial for successful worksite wellness programs include: long-term commitment, top-level management support, employee involvement, leadership, specified objectives, detailed planning [18], focus on employee needs, resourceful, and a smooth integration into workplace environment [19]. Even if all these factors are present, the true effectiveness of a worksite wellness program is dependent on the characteristics of the target population and the proportion of the population that participates in the intervention [20-22]. If employees are not interested [23], unmotivated, or information is not personally relevant [24], the most well-planned program can fail.
The average participation rate among employees for worksite wellness programs is less than 50% [25,26]. McLellan et al. [26] had an overall participation rate of 23%, ranging widely (10-86%) among different workgroups [26]. Robroek et al. [25] experienced similar rates with an overall median participation rate of 33%, ranging from 10-64% [25]. Research shows that women are generally more likely to participate in worksite wellness programs than men and, overall, married employees have much higher participation rates than their single co-workers [25]. Other determinants of higher participation rates include: white-collar or secured contract employees [27,28], full-time employees [28,29], older age [26], and small company employees [30]; shift workers [31], lower income, and less education [32] displayed much lower participation rates.
Although previous research has indicated what characteristics of employees are most associated with participation in worksite wellness programs, it is still unclear from a qualitative perspective why employees may decide not to participate. Minimal research exists on wellness programs in the university setting, in particular among foodservice employees. The purpose of this research was to determine why employees decided not to participate in an employee wellness program, Wellness Wednesdays: "Eat & Meet" About Healthy Living, conducted for ARAMARK employees at East Carolina University in Greenville, North Carolina.
Subjects and Methods
Wellness Wednesdays: "Eat & Meet" About Healthy Living was conducted at East Carolina University, a public, coeducational university located in Greenville, North Carolina. Total enrollment for the fall 2009 semester was 27,654 students, including both on-campus and distance education students, with an additional 1,782 full-time and part-time faculty members [33]. Currently, the university's Campus Wellness Center provides informational tables and events and offers group presentations on health-related topics such as smoking cessation, nutrition, stress management, alcohol use, and physical activity [34]. To date, there are no known established employee wellness programs at East Carolina University.
Wellness Wednesdays: "Eat & Meet" About Healthy Living was created by the ARAMARK Nutrition Director in order to provide employees with the opportunity to participate in a worksite wellness program, emphasizing various nutrition- and health-related topics. This program has not been implemented for employees at other ARAMARK locations and is unique to East Carolina University. The program was created in order to address employee health characteristics such as high cholesterol, abnormal glucose levels, hypertension, and overweight/obesity. These health needs were discovered at the 2008 ARAMARK employee wellness screening and served as the basis for the class and the selected topics. Topics covered in the program were those that would benefit employees that are overweight or obese, seeking to lose/maintain weight, have hypertension, high cholesterol, and/or diabetes, or are interested in improving their overall health. The number and length of weekly classes were determined based on optimal employee and management schedules. This was critical in planning because organizers had to ensure that employees would be able to take a break from their responsibilities to attend the weekly classes while still keeping food production on schedule. Collaboration with other organization directors and managers was necessary to make the final decision regarding program duration and length/location of classes. Marketing strategies utilized to promote the wellness program and recruit participants included: discussion of program in foodservice facilities' pre-service meetings (all employees in that shift present) and in employee round table meetings, inclusion of an article in the employee newsletter, and distribution of posters/flyers located in all foodservice locations and on employee bulletin boards. Wellness Wednesdays: "Eat & Meet" About Healthy Living was implemented on September 30, 2009 with its first class and an introduction to how the program operates, the timing and location of classes, topics to be discussed each week, and incentives offered.
East Carolina University ARAMARK employees are predominantly service workers (83.7%), with 7.3% administrative support workers, 6.4% officers and manager, and 1.9% other job positions. There are 304 female employees and 177 males. Of these employees, 75.9% are African American, 21.8% are Caucasian, 1.5% are Hispanic, and 0.8% are Asian/Indian. Based on data from the 2008 ARAMARK employee wellness screening, common health characteristics of employees were obtained. Employees were tested for cholesterol, blood pressure, and glucose readings and body measurements were also taken. Of these employees, 27% of participants had moderate (201-239 mg/dL) to high (> 240 mg/dL) total cholesterol; 21% had high fasting (> 100 mg/dL) or non-fasting (> 140 mg/dL) glucose levels; and 68% had moderate (120/80 to 140/90 mmHg) to high (> 140/90 mmHg) blood pressure readings. Additionally, 27% of employees were classified as overweight (BMI: 25.0-29.9 kg/m2) and 51% as obese (BMI: > 30 kg/m2). Overall, a large amount of ARAMARK employees are overweight or obese and have a moderate to high risk for hypertension, with some having a moderate to high risk for high cholesterol and diabetes.
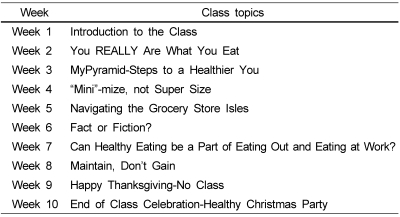
All ARAMARK employees (n = 481) over the age of 18 were eligible to participate. All interested employees (n = 50) obtained clearance/approval from their manager to ensure that schedules permitted participation. Over a 10-week period, 30 minute classes were taught once a week by a Registered Dietitian. Topics (shown in Table 1) included various nutrition- and health-related issues that were intended to increase employees' knowledge and skills on nutrition and healthy eating. The location of the classes alternated between the two dining halls on campus each week to ensure that employees from both ends of campus had the opportunity to attend. The approximate time it took to walk between sites was 15 minutes. Incentives to participate in this program were that employees would receive a $5.00 credit or "wellness bucks" for each class attended. At the end of the 10-week period, the total number of classes attended were tallied by reviewing weekly sign-in sheets and given to the payroll/accounting department so payments could be included in employee paychecks. For example, if an employee attended all 10 classes, he/she would receive an extra $50.00 credit in their paycheck.
Table 1.
Wellness wednesdays weekly class topics
A five question knowledge-check quiz was administered to participants at the end of each class to determine the effectiveness of the information and materials presented and the participants' level of knowledge on the topics. Questions were specific to the topic discussed that week. This method of program evaluation was chosen due to the inconsistency of participant attendance. A pre- and post-program evaluation tool would not have provided accurate and valid results because no employee attended all classes. Therefore, only post-class knowledge quizzes were administered for evaluation to gauge level of participant knowledge and retention of the new material.
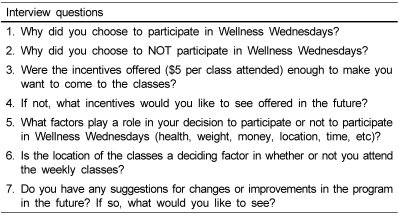
Qualitative interviews were conducted after the completion of the 10-week program. Short, 3-5 minute interviews (n = 19) were randomly obtained from ARAMARK employees (both those who attended, n = 11, and those who did not attend the program, n = 7) and the program organizer (n = 1) with questions aimed at information about attendance, participation, incentives, location, and suggestions. A funnel approach was used in interviews with the broadest questions asked first (to avoid sensitizing interviewees and leading responses) to more specific prompts for further information. Interview questions are listed in Table 2. Interviews were conducted in East Carolina University dining facilities where ARAMARK employees were working. Selection was completely random and there was no inclusion criteria set in order to obtain unbiased, non-influenced responses. By choosing to use a random sampling strategy and conducting short, informal interviews in the work area, feedback from a wide range of employees was able to be obtained (both participants and non-participants) since employees did not have to stop working or feel pressured to answer in a particular way. Interviews were conducted until saturation of themes occurred. All research protocols were approved by East Carolina University Institutional Review Board.
Table 2.
Qualitative interview questions
Results
A total of 50 (10.4%) East Carolina University ARAMARK employees, managers, and leadership team members attended Wellness Wednesdays: "Eat & Meet" About Healthy Living at least once during the 10-week program. Out of the 10 available classes, 50% attended 1 class; 22% attended 2 classes; 14% attended 3 classes; 4% attended 4 classes; and 1% attended 5 classes. No employee attended more than 5 of the 10 classes. It was found that employees from some locations on campus had stronger participation than others. Employees at retail dining facilities located in the middle of campus had the least participation, while the two dining halls (one on each end of campus) and retail facilities on the West End of campus had the highest employee participation rate. Class size varied from week to week and ranged from 4 to 20 people. On average, 11 people attended each class.
After reviewing the weekly five question knowledge quizzes administered at the end of each class, it was found that most people scored well on the knowledge assessments. Average scores ranged from 71-100%.
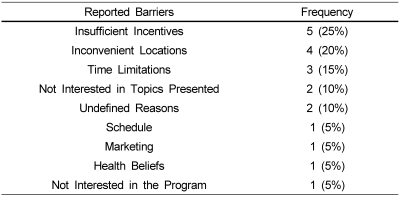
Qualitative interviews of random ARAMARK employees after the completion of the program revealed several themes and barriers for not participating. The top three reported barriers to participation (in order from most often to least often reported) were insufficient incentives, inconvenient locations, and time limitations. A complete list of cited barriers is shown in Table 3. Employees expressed that offering more money as an incentive would make it more likely for them to attend and the extra money was "always good." Location was an issue due to the distance between foodservice facilities. Some employees would only attend classes held at their location and did not attempt to go to the classes held at the opposite end of campus. Timing and scheduling of the weekly classes were reported to be difficult because they were conducted during the work day and it was often hard to find a time that employees would be able to attend without disrupting their shift schedules and responsibilities. Time was an especially important barrier with retail location facilities which did not have time in between meals to leave and classes were held during one of their busiest times. Scheduling the classes on one morning during the week limited the number of employees that could attend. Employees who were off on Wednesdays or who worked the night shifts had to make an extra effort to come in during their time off to attend the classes. Some employees reported that they were not interested in the topics discussed and, therefore, did not attend. Topics that were cited as being of interest that were not included in the program or were not covered in-depth included: hypertension, stress management, heart health, shopping on a budget, exercise, and proper child nutrition. Marketing referred to initiatives for the promotion and publication of the program such as flyers, information from location managers during pre-service meetings with employees, and other media outlets. Employees felt that they were not adequately informed and made aware of the program and the timing and scheduling of the occurrence of the classes. Health beliefs were expressed as comments such as not attending because of perceived sufficient health knowledge and having a healthy family.
Table 3.
Barriers to participation reported by employees (in order from most often to least often reported)
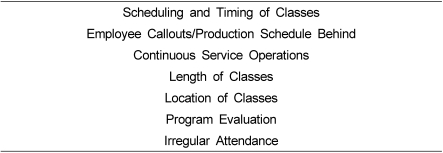
From an organizers perspective, successfully planning and implementing this program was not without its own set of barriers, many of which were similar to those expressed by employees. Scheduling and timing of the weekly classes were reported to be difficult because they were conducted during the work day and it was often hard to find a time that employees would be able to attend without disrupting the shift schedules. Attendance was further hindered when sites were short-handed due to callouts (employee calls to inform managers that he/she will not be at work due to sickness, transportation issues, etc), production schedule being behind target, or by continuous service operations (such as retail outlets versus dining halls that had set meal periods and open/close schedules). To better accommodate the busy schedules of foodservice employees, organizers tried to keep the classes short, 15 to 30 minutes. However, it was reported to be difficult to adequately address all of the information within the short class periods. The location of the weekly classes was another important and sometimes difficult factor for organizers to address. On this college campus, employees were spread out over 14 dining locations. With people in so many different locations, it was nearly impossible to find a location that was convenient for all to attend without having to walk or drive. If employees chose to drive, parking spaces are limited and, therefore, created another problem to factor in with transportation. This issue was addressed by alternating the end of campus that classes were held at, but this still did not capture all dining locations, leaving some employees with a travel time to factor in. Finally, program evaluation on knowledge for Wellness Wednesdays was extremely difficult due to low participation rates and regular attendees. An overall knowledge pre/post-evaluation would not have provided accurate information about the effectiveness of the program because all employees did not attend all 10 classes. With such irregular attendance, it was hard to evaluate how effective the program was in relation to lifestyle factors, weight, and health status as well as preventing maximum knowledge gain due to the inability to build on information from one week to the next. A complete list of barriers cited by the program organizer is shown in Table 4. Table 4 does not show percentages of responses because only one organizer was interviewed.
Table 4.
Program organizer's reported barriers
Discussion
According to previous research, the average participation rate among employees for worksite wellness programs is less than 50% [25,26]. McLellan et al. [26] had an overall participation rate of 23%; Robroek et al. [25] experienced similar rates with an overall median participation rate of 33%. Evaluation of Wellness Wednesdays: "Eat & Meet" About Healthy Eating supported these findings with an overall participation rate of 10.4%. Barriers such as insufficient incentives, inconvenient locations, time limitations, not interested in topics presented, schedule, marketing, health beliefs, and not interested in the program were found and negatively impacted participation rates in this employee wellness program. These barriers also supported previous findings, especially employee disinterest [23] and information presented not being personally relevant [24]. However, the top three barriers reported (incentives, location, and time) had not been previously reported as barriers to worksite wellness program participation. These barriers may be unique to college campus employees and partially related to the physical spread of the work environment.
In order to increase participation rates, creative approaches to meeting employees' needs are required. Previous research shows that by addressing employee preferences and perceived barriers, the likelihood of achieving and maintaining better health and well-being will be significantly increased [17]. This information can be obtained prior to the start of the program by distributing a needs and interest survey to all employees and would ensure that the topics presented were relevant and appropriate for the intended audience.
Evaluation of Wellness Wednesdays: "Eat & Meet" About Healthy Living provides useful information for future program development of employee wellness programs, especially in work environments that are diverse and physically spread out such as college campuses. Results show that employee wellness programs can be implemented on college campuses and are effective in increasing knowledge and skills of employees on nutrition- and health-related topics. However, program planning that addresses identified barriers including insufficient incentives, inconvenient locations, and time limitations may facilitate higher participation in future worksite wellness opportunities.
References
- 1.Heron M, Hoyert DL, Murphy SL, Xu J, Kochanek KD, Tejada-Vera B, Division of. Deaths: final data for 2006. Natl Vital Stat Rep. 2009;57:1–135. [PubMed] [Google Scholar]
- 2.Carnethon M, Whitsel LP, Franklin BA, Kris-Etherton P, Milani R, Pratt CA, Wagner GR. Worksite wellness programs for cardiovascular disease prevention: a policy statement from the American Heart Association. Circulation. 2009;120:1725–1741. doi: 10.1161/CIRCULATIONAHA.109.192653. [DOI] [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 4.Kruger J, Yore MM, Ainsworth BE, Macera CA. Is participation in occupational physical activity associated with lifestyle physical activity levels? J Occup Environ Med. 2006;48:1143–1148. doi: 10.1097/01.jom.0000245919.37147.79. [DOI] [PubMed] [Google Scholar]
- 5.Pronk NP, Kottke TE. Physical activity promotion as a strategic corporate priority to improve worker health and business performance. Prev Med. 2009;49:316–321. doi: 10.1016/j.ypmed.2009.06.025. [DOI] [PubMed] [Google Scholar]
- 6.Pronk NP, Martinson B, Kessler RC, Beck AL, Simon GE, Wang P. The association between work performance and physical activity, cardiorespiratory fitness, and obesity. J Occup Environ Med. 2004;46:19–25. doi: 10.1097/01.jom.0000105910.69449.b7. [DOI] [PubMed] [Google Scholar]
- 7.Aldana SG. Financial impact of health promotion programs: a comprehensive review of the literature. Am J Health Promot. 2001;15:296–320. doi: 10.4278/0890-1171-15.5.296. [DOI] [PubMed] [Google Scholar]
- 8.Aldana SG, Greenlaw RL, Diehl HA, Salberg A, Merrill RM, Ohmine S. The effects of a worksite chronic disease prevention program. J Occup Environ Med. 2005;47:558–564. doi: 10.1097/01.jom.0000165743.18570.66. [DOI] [PubMed] [Google Scholar]
- 9.Van der Klink JJ, Blonk RW, Schene AH, Van Dijk FJ. The benefits of interventions for work-related stress. Am J Public Health. 2001;91:270–276. doi: 10.2105/ajph.91.2.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Racette SB, Deusinger SS, Inman CL, Burlis TL, Highstein GR, Buskirk TD, Steger-May K, Peterson LR. Worksite opportunities for wellness (WOW): Effects on cardiovascular disease risk factors after 1 year. Prev Med. 2009;49:108–114. doi: 10.1016/j.ypmed.2009.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Saving Dollars and Making Sense [Internet] A comprehensive guide to workforce health promotion; [cited 2010 February 10]. Available from: http://www.eatsmartmovemorenc.com/ManagementGuide/Texts/WorksitesMgmtGuide.pdf. [Google Scholar]
- 12.Shepard RJ. Do work-site exercise and health programs work? Phys Sportsmed. 1999;27:48–72. doi: 10.3810/psm.1999.02.667. [DOI] [PubMed] [Google Scholar]
- 13.Pelletier KR. A review and analysis of the clinical and cost-effectiveness studies of comprehensive health promotion and disease management programs at the worksite: Update VII 2004-2008. J Occup Environ Med. 2009;51:822–837. doi: 10.1097/JOM.0b013e3181a7de5a. [DOI] [PubMed] [Google Scholar]
- 14.Sorenson G, Quintilliani L. Effective programs to promote worker health within healthy and safe worksites. In: Pronk NP, editor. ACSM's Worksite Health Handbook. A Guide to Building Healthy and Productive Companies. Second Edition. Champaign, IL: Human Kinetics; 2009. [Google Scholar]
- 15.Henning R, Warren N, Robertson M, Faghri P, Cherniack M CPH-NEW Research Team. Workplace health protection and promotion through participatory ergonomics: An integrated approach. Public Health Rep. 2009;124:26–35. doi: 10.1177/00333549091244S104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Committee Report, 2008. Washington, DC: US Department of Health and Human Services; 2008. [Google Scholar]
- 17.McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15:351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 18.Fielding JE. Health promotion and disease prevention at the worksite. Annu Rev Public Health. 1984;5:237–265. doi: 10.1146/annurev.pu.05.050184.001321. [DOI] [PubMed] [Google Scholar]
- 19.Health Communication Unit. Conditions for successful workplace health promotion initiatives. Toronto: Centre for Health Promotion, University of Toronto; 2002. [Google Scholar]
- 20.Dishman RK, Oldenburg B, O'Neal H, Shepard RJ. Worksite physical activity interventions. Am J Prev Med. 1998;15:344–361. doi: 10.1016/s0749-3797(98)00077-4. [DOI] [PubMed] [Google Scholar]
- 21.Matson-Koffman DM, Brownstein JN, Neiner JA, Greaney ML. A site-specific literature review of policy and environmental interventions that promote physical activity and nutrition for cardiovascular health: What works? Am J Health Promot. 2005;19:167–193. doi: 10.4278/0890-1171-19.3.167. [DOI] [PubMed] [Google Scholar]
- 22.Proper KI, Koning M, Van der Beek AJ, Hildebrandt VH, Bosscher RJ, Van Mechelen W. The effectiveness of worksite physical activity programs on physical activity, physical fitness, and health. Clin J Sport Med. 2003;13:106–117. doi: 10.1097/00042752-200303000-00008. [DOI] [PubMed] [Google Scholar]
- 23.Bull SS, Gillette C, Glasgow RE, Estabrooks P. Work site health promotion research: To what extent can we generalize the results and what is needed to translate research to practice? Health Educ Behav. 2003;30:537–549. doi: 10.1177/1090198103254340. [DOI] [PubMed] [Google Scholar]
- 24.Langille JD, Berry TA, Reade IL, Witcher C, Loitz CC, Rodgers WM. Strength of messaging in changing attitudes in a workplace wellness program. Health Promot Pract. 2009 doi: 10.1177/1524839909336650. Article in press. [DOI] [PubMed] [Google Scholar]
- 25.Robroek SJW, van Lenthe FJ, van Empelen P, Burdorf A. Determinants of participation in worksite health promotion programmes: A systematic review. Int J Behav Nutr Phys Act. 2009;6:26–37. doi: 10.1186/1479-5868-6-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McLellan RK, MacKenzie TA, Tilton PA, Dietrich AJ, Comi RJ, Feng YY. Impact of workplace sociocultural attributes on participation in health assessments. J Occup Environ Med. 2009;51:797–803. doi: 10.1097/JOM.0b013e3181a4b9e8. [DOI] [PubMed] [Google Scholar]
- 27.Sorensen G, Stoddard A, Ockene JK, Hunt MK, Youngstrom R. Worker participation in an integrated health promotion/health protection program: Results from the WellWorks project. Health Educ Q. 1996;23:191–203. doi: 10.1177/109019819602300205. [DOI] [PubMed] [Google Scholar]
- 28.Stein AD, Shakour SK, Zuidema RA. Financial incentives, participation in employer-sponsored health promotion, and changes in employee health and productivity: HealthPlus health quotient program. J Occup Environ Med. 2000;42:1148–1155. doi: 10.1097/00043764-200012000-00005. [DOI] [PubMed] [Google Scholar]
- 29.Hooper JM, Veneziano L. Distinguishing starters from non-starters in an employee physical-activity incentive program. Health Educ Q. 1995;22:49–60. doi: 10.1177/109019819502200106. [DOI] [PubMed] [Google Scholar]
- 30.Blake SM, Caspersen CJ, Finnegan J, Crow RA, Mittlemark MB, Ringhofer KR. The shape up challenge: A community-based worksite exercise competition. Am J Health Promot. 1996;11:23–34. doi: 10.4278/0890-1171-11.1.23. [DOI] [PubMed] [Google Scholar]
- 31.Henritze J, Brammell HL, McGloin J. LIFECHECK: a successful, low touch, low tech, in-plant, cardiovascular disease risk identification and modification program. Am J Health Promot. 1992;7:129–136. doi: 10.4278/0890-1171-7.2.129. [DOI] [PubMed] [Google Scholar]
- 32.Adler NE, Newman K. Socioeconomic disparities in health: Pathways and policies. Health Aff (Millwood) 2002;21:60–76. doi: 10.1377/hlthaff.21.2.60. [DOI] [PubMed] [Google Scholar]
- 33.Fact Book 2009-2010 [Internet] Greenville (NC): East Carolina University; 2010. [updated 2010 March 15; cited 2010 March 23]. Available from: http://www.ecu.edu/cs-admin/ipre/FactBook2010.cfm. [Google Scholar]
- 34.Campus Wellness Programs and Services [Internet] Greenville (NC): East Carolina University; 2010. [updated 2010 January 28; cited 2010 March 23]. Available from: http://www.ecu.edu/csstudentlife/crw/programs/campuswellness/programs_services.cfm. [Google Scholar]