Abstract
Study Design
Case report
Background
Clinical practice guidelines regarding the conservative management of degenerative hip conditions in older adults routinely incorporate therapeutic exercise and manual therapy. However, the application of these recommendations to young, active adults is less clear. The purpose of this case report is to describe the management of a young adult with advanced hip arthrosis using a multi-faceted rehabilitation program.
Case Description
A 28-year old female with severe left hip degeneration per diagnostic imaging was referred to physical therapy. Reduced hip range of motion and strength, sacroiliac joint asymmetries, and a modified Harris Hip Score of 76 were observed. She was seen for 12 visits over a 3-month period and treated with an individualized program including manual therapy, therapeutic exercise, and neuromuscular re-education.
Outcome
Substantial improvements were noted in pain, hip range of motion and strength and function (modified Harris Hip Score of 97). In addition, she discontinued the use of anti-inflammatory medications and returned to her prior level of activity. Improvements were maintained at a 3 month follow up, with symptom recurrence managed using a self mobilization technique to the left hip and massage to the left iliopsoas.
Discussion
Degenerative hip conditions are common among older adults but are relatively rare in the younger population. Although it is likely that this patient will experience a return of her symptoms and functional limitations as her hip disease progresses, the immediate improvements may delay the need for eventual surgical management. These outcomes suggest that physical therapy management should be considered in those with an early onset of degenerative hip disease and are consistent with results previously reported in the older population.
Level of Evidence
Therapy, Level 4
Keywords: Manual therapy, OA, Osteoarthritis, Therapeutic exercise
Osteoarthritis (OA) and other arthritic conditions are estimated to incur an annual cost between $80 and $123 billion in the United States comprised of medical expenses and lost wages.33,45 Degenerative joint disease is becoming more prevalent in our aging population attributed, in part, to an increased life expectancy, reduced physical activity, and the growing obesity epidemic.12 Degenerative conditions of the hip have a prevalence estimated to vary from 0.7 to 4.45% of the population.12,24 Of greater concern, individuals with advanced hip arthrosis display a substantial reduction in health-related quality of life, including severe mobility restrictions secondary to pain and poor general health.1,3,14
Hip arthrosis is diagnosed based on the combination of patient complaints, diagnostic imaging, and physical examination findings. Individuals with degenerative hip conditions are frequently over 40-years old, overweight, and report aching and stiffness in the groin and/or buttock/hip.7,21,25,39 Hip degeneration is uncommon in younger patients in the absence of prior trauma or systemic illness.21 Common clinical findings include limitation into hip internal rotation and flexion range of motion (ROM), pain and/or crepitus with hip ROM testing, and weakness of periarticular hip musculature.21,39 It is not uncommon for pain to be referred to the anterior aspect of the distal thigh.7,25 The presence of joint space narrowing, osteophytes, and changes to subchondral bone on radiographic evaluation provide further indication of degenerative hip conditions.21
Current clinical practice guidelines for the conservative management of hip OA promote a combination of pharmacologic and non-pharmacologic interventions.10,21,28,47 Considering the adverse effects linked with chronic non-steroidal anti-inflammatory drug use such as gastrointestinal bleeding and cardiovascular disease,21,26,35 non-pharmacological management options are often emphasized. However, utilization of commonly recommended self-management strategies such as exercise, weight loss, use of an assistive device, and orthotic prescriptions have demonstrated questionable compliance among patients and clinicians alike.21 35,47
Physical therapy has been recommended to slow the progression of OA with a focus on addressing the individual's impairments and faulty movement patterns.10,21,47 Therapeutic exercise has been found to have a small effect on the management of this condition when used alone.18,32 Common manual interventions including clinician-administered stretching of hip musculature and variations of a long axis distraction manipulation have shown positive effects on pain, ROM, and various outcome measures including the SF-36 and Harris Hip Score.19 By combining these 2 treatment approaches (i.e., therapeutic exercise and manual therapy), optimal clinical outcomes have been demonstrated.10,12,26 Despite this evidence and inclusion of exercise and manual therapy in most clinical practice guidelines, physical therapy management is recommended to only 28-48% of patients with hip OA presenting in physician offices.10,35 Further, while the benefit of physical therapy has been demonstrated in those over 50 years old,10,18,32 evidence supporting the use of this approach in young adults is limited. While similar benefits may be expected, it is uncertain as to whether young adults would achieve sufficient gains to return to the high level of activity common to their age group. However, given the limited surgical options available for this younger population, physical therapy management may play a more critical role.
The goal of this case report is to describe the conservative management of a young adult female diagnosed with advanced hip arthrosis. Through this report, we hope to provide insights into the benefits that an individualized treatment program combining therapeutic exercise and manual therapy techniques can have on reducing pain and improving function in individuals with hip arthrosis.
CASE DESCRIPTION
Patient History
The patient was a 28 year-old female (height, 167.6 cm; mass, 77 kg) that worked as a part-time aerobics instructor while completing her graduate studies. She reported a 4-month history of pain in her left buttock, groin, and distal quadriceps. She attributed her buttock pain to a recent “deep hip stretching” routine that she self-initiated and described it as burning or tightness that worsened while performing aerobics, lunges, or squats and can reach 4/10 (0, no pain; 10, worse pain imaginable) in intensity on a numeric pain rating (NPR) scale. The patient believed that the pain in her left groin and distal quadriceps resulted from altered mechanics following a severe ankle sprain that occurred 4 years ago. This pain would reach 9/10 in intensity on a NPR scale, was described as a deep ache, and was aggravated with prolonged weight bearing, particularly on consecutive days. Rest and use of naproxen decreased her pain in each location. At the time of the evaluation, she had discontinued her work as an aerobics instructor secondary to her pain.
The patient was initially referred to a different physical therapist by her primary care physician and underwent treatment for the diagnoses of iliotibial band syndrome, hip pain, and subluxing patella. Treatment consisted of activity modification, soft tissue massage using a foam roller, and passive stretching into hip internal and external rotation, resulting in minimal improvement.
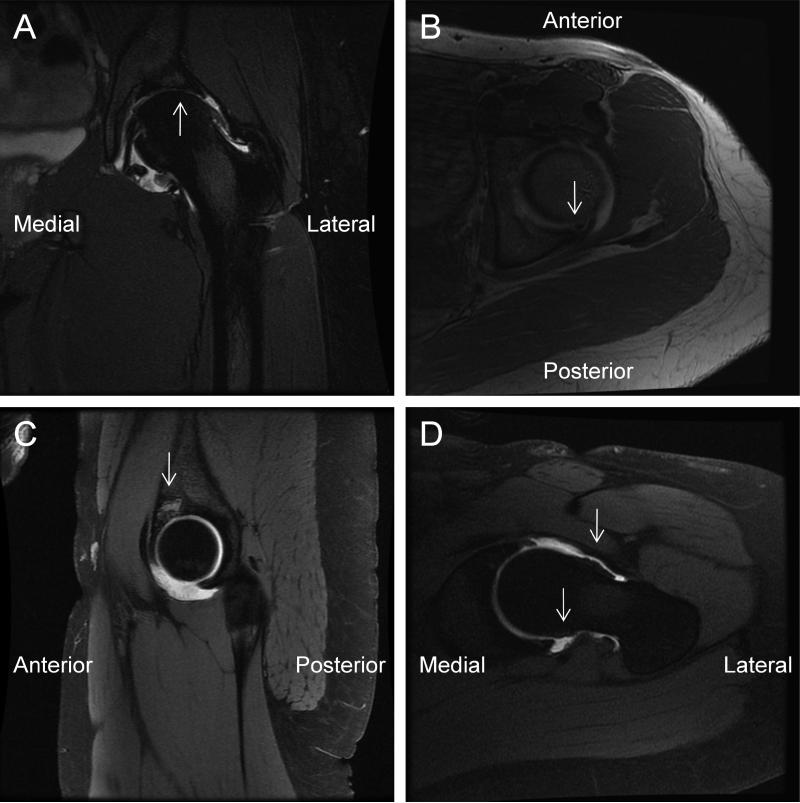
The patient sought further evaluation by an orthopedic surgeon who ordered a thorough diagnostic imaging work up for her left hip. Radiographs and contrast magnetic resonance imaging (MRI) indicated the presence of cam type lesion on the femoral head-neck junction, severe chondrosis with areas of full thickness cartilage loss, and an osteochondral loose body (FIGURES 1 and 2). The surgeon believed that she would not benefit from an arthroscopic osteotomy to address the cam lesion because the chondrosis was the likely pain generator.
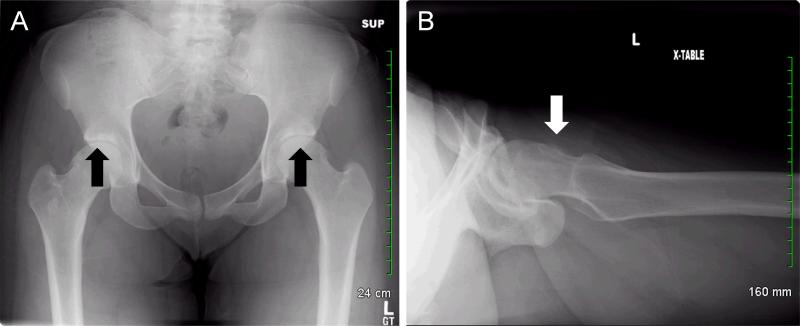
Figure 1.
Radiographic imaging of the pelvis and proximal femur indicating (A) mild hip joint space narrowing and subchondral sclerosis bilaterally (anteroposterior view) and (B) cam lesion of the left hip (cross-table lateral view).
Figure 2.
Contrast magnetic resonance image of the left hip region indicating (A) the presence of severe chondrosis with broad areas of full thickness cartilage loss (T2 coronal view), (B) an associated subchondral cyst (T1 axial view), (C) a 12mm loose osteochondral body (proton dense sagittal view) and (D) large rim osteophytes on the femoral head/neck junction (T1 oblique view).
Once the original physical therapist was made aware of the imaging findings, treatment was discontinued as he believed he had little more to offer. The patient was then seen by 2 additional orthopedic surgeons specializing in joint replacements, as well as a rheumatologist with recommendations to reduce activity and to contact their office when she was ready for a total hip arthroplasty (THA). She requested further physical therapy consultation to be instructed on strategies to slow the degenerative process in hopes of prolonging the time before a possible eventual THA.
Examination
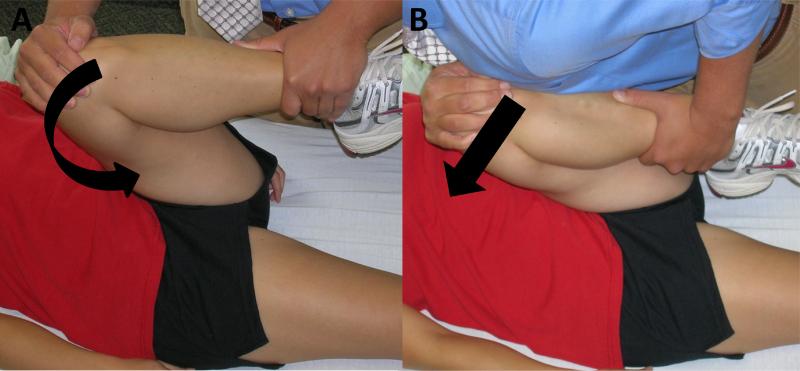
The patient demonstrated hip ROM restrictions bilaterally with less internal rotation and reproduction of her groin pain with testing of the left side (TABLE 1). The Scour test 2,7,39 was provocative for her groin pain but did not produce a palpable “click”, therefore a more aggressive impingement test,5,27,44 was not performed (FIGURE 3). Reproduction of her pain with these maneuvers suggested an intra-articular source of her groin pain.
Table 1.
Objective measures from initial evaluation.
| Passive Range of Motion (°) |
Right |
Left |
|---|---|---|
| Hip flexion | 110 | 110* |
| Hip external rotation | 60 | 60 |
| Hip internal rotation | 30 | 20* |
| Knee flexion | Full | Full |
| Knee extension | Full | Full |
| Active Lumbar Movement |
|---|
| Full in all planes |
| Muscle Length Tests‡ |
Right |
Left |
|---|---|---|
| 90/90 Hamstring | None | None |
| Ely's test | 30° | 30° |
| Supine piriformis test | Moderate | Mild |
| Thomas test | 10° | 10° |
| Strength Testing |
Right |
Left |
|---|---|---|
| Hip flexion | 4+/5 | 4+/5 |
| Hip abduction | 4/5 | 3+/5 |
| Hip extension | 4-/5 | 4-/5 |
| Knee extension | 5/5 | 5/5 |
| Knee flexion | 5/5 | 5/5 |
| Ankle (PF and DF) | 5/5 | 5/5 |
| Standing Posture |
|---|
| • Increased lumbar lordosis |
| • Mild bilateral femoral internal rotation and adduction |
| • Mild bilateral pes planus and hallux valgus |
| Joint Play Assessment |
Spinal Level |
|---|---|
| Hypomobile | L5 |
| Hypermobile | T8-10, L1-2 |
| Normal Mobility | T11-12, L3-4 |
| Neurologic Screen (Bilateral) | |
|---|---|
| Dermatome (light touch) | Normal L2 thru S2 |
| DTR (patellar/Achilles) | 1+ /2+ |
| Special Tests |
|
|---|---|
| Hip Scour* | Limited on left |
| Hip FABER† | Limited on left |
| Patellar compression test | Negative |
| Standing forward bending test‡ | Positive on right |
| Supine to long sitting test§ | Right leg shifts from long to short |
| Motion testing in sitting§ | FRS-L at L5-S1 Right unilateral extension sacral lesion |
| Palpation |
|---|
| • Superior right iliac crest, posterior right sacral base, superior right ASIS in comparison to left |
| • Quadriceps and buttock were non-tender with firm palpation |
reproduced groin pain
reproduced buttock pain
expressed in restriction from normal length
testing performed as described in Greenman15.
PF, plantarflexion; DF, dorsiflexion; ASIS, anterior superios iliac spine; L, lumbar; T thoracic; DTR, deep tendon reflex;; FABER, flexion-abduction-external rotation; FRS-L, flexion rotation sidebend left
Figure 3.
The Scour and Impingement tests are similar, however (A) the Scour test consists of passively positioning the involved hip into flexion and adduction, applying an axial load through the femur, and moving the femur through 2 arcs of motion in the superomedial quadrant while the2,7 (B) impingement test consists of loading until end-range flexion-adduction-internally rotation is achieved.5,27,44
Considerable weakness was detected with strength testing of the patient's hip extensors and abductors in neutral. Symptoms were not produced with resistance testing of the knee and hip, reducing the likelihood of a contractile source of symptoms. Standing posture showed increased lumbar lordosis and the lower extremities were in an adducted and internally rotated position suggesting weakness of the abdominal and gluteal musculature.
Considerable sacroiliac joint (SIJ) asymmetries suggestive of a right ilial up-slip, right anteriorly rotated innominate, and a right unilateral sacral extension lesion were perceived with palpation and special testing (ie, standing forward bending test, supine to long sitting test, lumbosacral motion testing in sitting).15,17 While the reliability of palpatory findings in this region has been questioned,11,23 these tests are commonly used to positively guide treatment of SIJ dysfunction in patients with hip and/or knee complaints.8,42
Diagnosis and Prognosis
The physical examination and imaging findings suggested that this 28 year-old female had bilateral hip degeneration with the left hip being symptomatic. Impairments identified that were likely contributing to this condition were reduced hip and abdominal strength, limited hip motion, and SIJ dysfunction. The patient's complaints of groin and knee pain were attributed to the hip pathology while the buttock pain was thought to be originating from the SIJ. This assessment is supported in that groin and thigh pain are accepted symptoms of hip OA, 7,21,25,39 groin pain was provoked with hip ROM testing and knee pain was not reproduced with direct testing of the knee joint. Furthermore, buttock pain is a common referral pattern associated with SIJ dysfunction.36 Finally, the patient reported the groin/thigh pain and buttock pain were aggravated by different activities and believed the pain locations had different causes. The short term prognosis for this patient was fair to good secondary to the multitude of impairments deemed treatable, as well as evidence to support use of manual therapy and exercise for this condition.10,12,18,26 The long term prognosis for this patient was more guarded secondary to the degenerative nature of this condition and tendency for home exercise program compliance to wane over time.32
Intervention
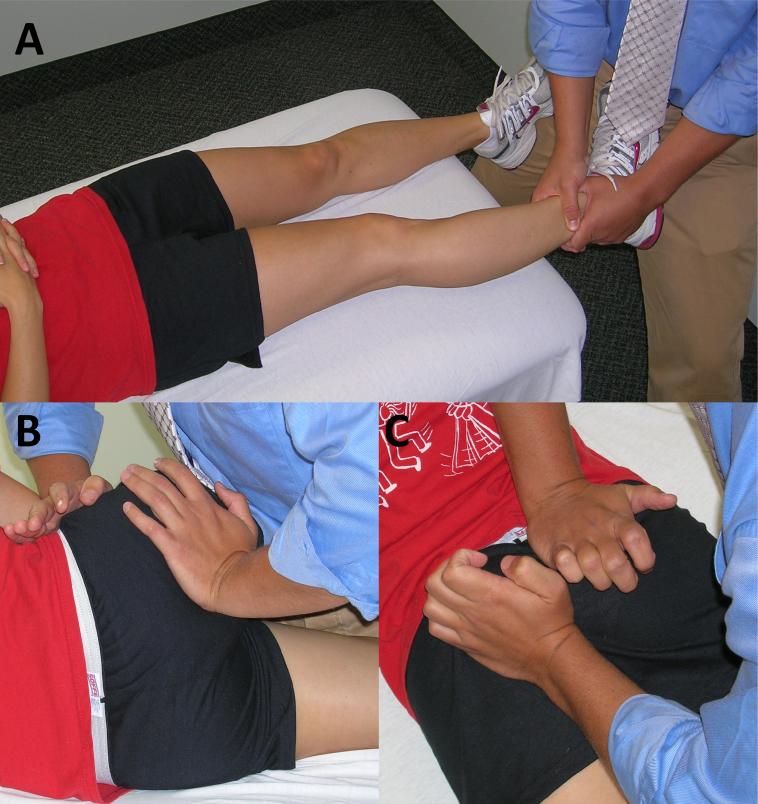
Session 1 (Day 1)
Treatment on the day of the initial evaluation was performed to assess the response of her buttock pain to treatment of the SIJ. Manual therapy techniques were performed for the SIJ dysfunctions perceived during the evaluation and performed sequentially as directed by Greenman15 (FIGURE 4). Treatment of the SIJ in subsequent appointments was determined based on motion testing and perceived boney asymmetries present on that day. The patient was instructed in a piriformis stretch exercise because of the flexibility limitation detected during testing and its believed relationship to SIJ dysfunction.
Figure 4.
Manual therapy techniques to the sacroiliac joint were performed as part of the comprehensive treatment plan. (A) A post-isometric relaxation technique to treat the right ilial up-slip consisted of long axis hip distraction at end range hip internal rotation. (B) A second post-isometric relaxation technique for the right anteriorly rotated innominate which includes isometric hip extension with anterior to posterior pressure to the anterior superior iliac spine and PA pressure on the ischial tuberosity. (C) A direct mobilization using oscillations in a posterior to anterior (PA) direction on the right sacral base and cranially on the left sacral inferior lateral angle to address the right unilateral extension lesion. 15
Session 2 (Day 3)
A positive response to the interventions aimed at the SIJ was determined as the patient reported experiencing minimal buttock pain, however the groin and knee pain was essentially unchanged. However, the buttock pain returned after attending an aerobics class the previous evening (TABLE 2). During this session, manual therapy techniques aimed at the SIJ were performed (ie, post-isometric relaxation techniques for a flexed, rotated and sidebent left L5-S1 segment, right on left sacral torsional lesion and right anteriorly rotated innominate), and a hip lateral distraction mobilization29 was initiated. The lateral hip distraction was performed in the flexed-adducted-internally rotated (FADIR) position (FIGURE 5) short of symptom provocation resulting in improved tolerance to passive hip movement into internal rotation and flexion. This intervention was performed with the intention of reducing the individual's groin pain. A posterior pelvic tilting exercise was initiated in hook-lying as a means to retrain the transverse abdominis.41
Table 2.
Summary of patient's symptoms and objective findings throughout the course of treatment.
| Visit (Days post initial examination) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 (0) | 2 (3) | 3 (18) | 4 (24) | 5 (31) | 6 (38) | 7 (45) | 8 (52) | 9 (59) | 10 (66) | 11 (73) | 12 (80) | |
| Pain (average)* | 4 | 2 | 1 | 0 | 4 | 3 | 0 | 0 | 0 | 0 | 1 | 2 |
| Pain (worst)* | 9 | 5 | 8 | 4 | 4 | 5 | 5 | 5 | 2 | 5 | 4 | 4 |
| Hip pain location | Groin & buttock | Groin & buttock | Groin | Buttock | Groin | Buttock | Groin | Groin | Groin | Groin | Groin | Groin |
| Naproxen use | Often | Often | None | None | None | Often | Rare | None | None | None | None | Rare |
| Hip flexion (°)† | 110 | 110 | 110 | 120 | 120 | 120 | 125 | 110 | 125 | 120 | 125 | 121 |
| Hip IR (°)† | 20 | 20 | 20 | 30 | 30 | 30 | 30 | 30 | 30 | 30 | 30 | 33 |
assessed verbally on a Numeric Pain Rating Scale (0, no pain; 10, worse pain imaginable)
maximal passive range of motion
IR, internal rotation
Figure 5.
Lateral hip distraction was initiated during the third treatment session to help alleviate the patient's groin pain and improve her tolerance to passive hip movement into internal rotation and flexion. Lateral translation of the pelvis is minimized with use of a belt placed inferior to the anterior superior iliac spines and wrapped around the table. This hip mobilization technique was performed with the hip in a flexed-adducted-internally rotated position short of symptom provocation with oscillations performed with the clinician's hips via a second belt.
Session 3 (Day 18)
Improvement of the groin symptoms was reported following the previous appointment, however these symptoms gradually returned to previous levels. The patient noted minimal buttock pain despite not using naproxen over the majority of the previous 2 weeks; however symptoms returned when she performed squats and lunges as part of her exercise program the previous evening. She acknowledged that running and performing step aerobics may reduce her potential to recover. This initiated a conversation regarding the severity of degeneration found in each of her hips and that avoiding impact activities may potentially be important to delay further progression of the degenerative process. The patient was instructed in a self mobilization technique (FIGURE 7) with an intention of mimicking the mobilization performed at the last session. After performing this activity, her passive hip internal rotation improved from 20 degrees to 30 degrees. The posterior pelvic tilting exercise was progressed to include knee lifts with a focus on pelvic stability. The patient scored 76 on the modified Harris Hip Score.30
Figure 7.
Self mobilization technique used as independent management technique. The patient was instructed to position her hip into a pain free flexed-adducted-internally rotated position and place a belt on the proximal femur. Oscillations were performed by pushing away from the wall, resulting in lateral distraction of the femur, at a rate of 1 Hz for 30 s, followed by a 30 s hold.
Sessions 4-6 (Days 24-38)
Over the subsequent 3 visits, the patient experienced a continued reduction of her groin, knee, and buttock pain, and was often asymptomatic. The patient had increased her activity level to include 1-2 hr bicycle rides, yoga, and kickboxing. Kickboxing resulted in a return of her buttock pain and SIJ asymmetries, both of which were subsequently resolved when manual therapy techniques were applied to that region. After performing yoga, the patient experienced significant burning and tightness in her left anterior hip. This was alleviated by a therapist-performed massage technique utilizing sustained compression over the iliopsoas muscle belly followed by self treatment using a hip flexor stretch and a modified Yamuna Body Rolling™ 46 technique (FIGURE 6). Yamuna Body Rolling™ is a form of self massage where an individual repeatedly rolls on a 6 or 10 inch partially-inflated ball over a targeted muscle with the aim of reducing muscle tone.46 Prone and side-lying plank exercises were initiated to improve abdominal41 and hip strength. The abnormal mechanics associated with lower extremity pathology were discussed further with the patient and the need to avoid hip adduction/internal rotation during activities was stressed. This was a point of emphasis as there is evidence that functioning in a more neutral position immediately reduced the pain reported in an individual with intraarticular hip pathology.2 A step down exercise was introduced to the patient to begin a functional strengthening progression and to educate the patient on more optimal movement patterns.
Figure 6.
A modified form of Yamuna Bodyrolling™ was performed to the left iliopsoas to reduce muscle tone and improve flexibility. This technique involves (A) lying prone over the ball and (B) rolling perpendicular to the muscle belly 5 times each above, medial to, and inferior to the anterior superior iliac spine followed by 5 repetitions of rolling parallel to the muscle belly.46
Sessions 7-11 (Days 45-70)
During this time, the patient self-initiated a 6-week total body exercise regimen.43 A significant amount of clinic time was spent cueing the patient to perform each exercise with proper mechanics or suggestions of avoiding exercises that included impact. Complaints of tightness in the hip adductors and quadriceps were addressed with anterior and medial hip joint mobilizations without a significant change. The patient also requested an evaluation of her right ankle as she believes this had a relationship to the onset of her hip and knee pain. The anterior drawer test indicated 2+ laxity and the patient was shown a series of exercises aimed at improving her ankle proprioception.9,16 In addition to her home exercise program, she was regularly cycling and performing yoga and a whole-body strengthening program.
OUTCOMES
Discharge (Day 80)
At discharge, the patient demonstrated substantial improvements from baseline including increased hip ROM and strength, decreased pain and naproxen usage, and improved modified Hip Harris score (TABLE 3). Despite these improvements, the patient demonstrated a positive impingement test. The impingement test is defined inconsistently in the literature5,27,44 and was performed by loading the hip in a flexed-adducted-internally rotated (FADIR) position until end-range is achieved in this case. More importantly, the patient had returned to all previous activities with the exception of running and was able to resume teaching step aerobics every 2 wks without increased hip symptoms. The patient continued to perform the self-management strategies, hip flexor and piriformis, stretches and plank exercises.
Table 3.
Key findings at the initiation of treatment, discharge and a 3-month follow-up.
| Initial Evaluation | Discharge (12 wks) | 3 Month Follow-up | |
|---|---|---|---|
| Pain (average / maximum)* | 4/ 9 | 2 / 4 | 2 / 4 |
| Naproxen use | Frequent | Infrequent | None |
| Hip motion (flexion/internal rotation) | 110° / 20° | 121° / 33° | 123° / 32° |
| Hip strength (extension/ abduction) | 4- / 3+ | 4+ / 5 | 5 / 5 |
| Impingement test | Positive† | Positive | Negative |
| Modified Harris Hip score | 76‡ | 97 | 95 |
assessed verbally on a Numeric Pain Rating Scale (0, no pain; 10, worse pain imaginable)
pain provoked during the scour test was considered positive for the purpose of this table
administered on the 3rd appointment
3 Month Follow-up (180 days)
Objective improvements were maintained 3 months following discharge (TABLE 3). The patient stated that she was very pleased to be active without consistently irritating her hip. She continued to limit impact activities while still comfortably performing Pilates, yoga, a whole body strengthening routine, and step aerobics.
DISCUSSION
This case report describes the short-term successful management of a young female with hip arthrosis using an individualized therapeutic exercise program combined with manual therapy techniques. Despite the presence of significant intra-articular pathology based on diagnostic imaging and limited success with previous conservative care, this patient was able to improve her hip and abdominal strength, hip ROM and level of function and activity while reducing her level of pain.
This case was unique in several aspects. First, despite being only 28 years old, severe degeneration of the hip was already present. Second, the use of a self mobilization technique involving lateral distraction to the hip was effective in allowing the patient to self-manage her anterior hip pan. Finally, this patient was able to improve despite flare-ups on a near weekly basis related to activities such as aerobics, yoga, and kickboxing. However, her eagerness to exercise allowed the aggressive prescription of exercises as a part of her treatment program without concern for lack of compliance.
Despite the recommendation of exercise in clinical practice guidelines for adults with osteoarthritis, this patient reported being told by several health care providers that physical therapy management would not prove beneficial. However, this case report provides further support that an individualized and comprehensive physical therapy program can significantly improve the symptoms and function associated with advanced hip degeneration, including in younger adults. The combination of manual therapy and a targeted home exercise program improved this patient's short term quality of life and likely delayed the eventual possible need for THA.
Surgical options for individuals with degenerative hip conditions consist of osteotomy and THA. Cam lesions have been associated with early degenerative changes in young hips and surgical removal has shown promising results. However, an osteotomy in this scenario would not be indicated because poor results are associated with those displaying advanced chondral changes.31,38 Delaying the need for a total hip replacement for this young woman is of paramount importance. Although the technology of THA implants continues to evolve, the life expectancy of the implant material is typically limited to 25 yrs and is often less with active individuals secondary to osteolysis around the prosthesis, loosening of the prosthesis and dislocation.6,34,37 The success of revision THA is more variable with 10 yr longevity of the device varying from 35-100% with a higher rate of failure in the younger population.37
An interesting part of this individual's presentation was the lack of symptoms present in or adjacent to her right hip despite the degeneration identified in the radiographs (FIGURE 1). While no definite conclusions can be made, the absence of right hip symptoms may be due, in part, to the bilateral differences in joint ROM and muscle strength (TABLE 1). That is, the increased ROM and strength of the right hip may have enabled it to better manage loads encountered during activity. In addition, it is not known whether a cam lesion was present in the right hip similar to the left hip (FIGURE 1), as the necessary imaging techniques to establish this were only conducted on the symptomatic hip. If indeed, a cam lesion was limited to the left hip, then this might further explain the lack of right hip symptoms. While not specifically addressed, it is likely that the right hip did benefit from the strengthening and improved movement patterns that came as a part of the rehabilitation program.
One of the primary goals of the initial 3 treatment sessions was to provide some clarity to the role of the hip degeneration and perceived SIJ dysfunction. The initial treatment session addressed the perceived SIJ dysfunction and a piriformis stretch. Her buttock symptoms were nearly eliminated (at least for the 36 hours prior to her participation in an aerobics class) with no accompanying improvement in groin or thigh pain, supporting the initial assessment that the buttock pain was related to the SIJ.
The second treatment began with a re-administration of manual interventions to the SIJ and was supported with a low level abdominal strengthening exercise. An attempt to address the hip pathology through a hip joint mobilization technique was initiated. Lateral hip distraction in the FADIR position was chosen because it was the most provocative position during the initial evaluation. It was theorized that this would increase the posterolateral translation of the femoral head and reduce abnormal contact between the femoral head and the anterior acetabular rim, comparable to the goal of joint mobilizations that are commonly used to treat primary and internal shoulder impingements.4 Following these interventions, she reported a reduction in her buttock pain that lasted the 15 days between treatment sessions but had only a short term effect on the groin symptoms.
Through the initial 2 treatments and the remainder of the course of treatment, complaints of buttock pain seemed to correlate with asymmetries found in the SIJ boney landmarks. While buttock pain has been associated with hip pathology,25 this individual's buttock pain demonstrated immediate improvement with treatment aimed at the SIJ. The use of SIJ manual therapy techniques have been shown to have a positive influence on conditions affecting the hip and knee.7,20,22,42
The short-term reduction in groin pain experienced after the second treatment was attributed to the lateral hip distraction performed during that session. This is supported by a change in groin pain shortly after the initiation of this treatment technique and immediate improvements in the tolerance to hip internal rotation and flexion. Therefore, more frequent hip mobilization was thought to be beneficial and the self mobilization technique was initiated. At that time, the patient's knee pain quickly resolved and she was able to self-manage her groin pain throughout the treatment period and after discharge.
The exercise program was focused on improving the patient's flexibility and strength in the pelvis and hip region. The initial program focused on transverse abdominis recruitment and was quickly progressed. Despite her level of prior physical activity, the patient demonstrated notable weakness of the hip extensors and abductors. This was addressed initially by the plank exercises. The step down exercises and squats were added to increase strength, as well as improve postural lower extremity control during weight bearing activities by avoiding excessive hip adduction and internal rotation. Contact between an abnormally shaped femoral head-neck junction and acetabular rim is currently accepted as the mechanics behind cam type femoral acetabular impingement (FAI).13,31,38,40 Focusing on functioning with the hip in a neutral position was intended to reduce the contact between those surfaces and the resultant stress to the hip joint. A similar approach using a brace to assist in reducing hip adduction and internal rotation provided immediate relief to an individual with FAI and a labral tear.2 Once the patient began an exercise regimen in week 9, technique errors were discussed with the patient and she was able to modify her form appropriately.
Significant improvements in strength, ROM, and activity tolerance were made throughout the treatment course and maintained for 3 months following the completion of her physical therapy. Further, these improvements were made despite discontinuing the use of naproxen. While the intra-articular pathology was likely not improved through this course of care, a negative impingement test was observed at the 3 month follow-up. The impingement test was thought to be more appropriate than the scour test to assess the irritability of the joint at discharge as the loading into the restricted ROM was considered to be more provocative than moving through the FADIR position. We theorized that this finding was a result of reduced intra-articular inflammation secondary to improved load distribution within the hip joint subsequent to the increases in strength and ROM.
CONCLUSION
This case describes the management of an individual presenting with advanced degenerative changes in the hip. The treatment program included manual therapy and exercise aimed at improving strength, ROM, and flexibility deficits. Degenerative conditions of the hip are increasing in prevalence and providing optimal conservative treatment can be integral to the successful management of these conditions.
Footnotes
This patient was seen at Meriter Health Services, Department of Rehabilitation, Middleton Clinic, Physical Therapy Department, Madison, WI during Kyle Cook's Orthopedic Residency. The opinions or assertions and the private views of the authors do not reflect the views of the University of Wisconsin Hospital/Clinics or Meriter Health Services.
REFERENCES
- 1.Aroski MH, Haara M, Helminen HJ, Arokoski JP. Physical function in men with and without hip osteoarthritis. Archives of Physical Medicine and Rehabilitation. 2004;85:574–81. doi: 10.1016/j.apmr.2003.07.011. [DOI] [PubMed] [Google Scholar]
- 2.Austin A, Souza R, Meyer J, Powers C. Identification of abnormal hip motion associated with acetabular labral pathology. Journal of Orthopedic & Sports Physical Therapy. 2008:38;558–65. doi: 10.2519/jospt.2008.2790. [DOI] [PubMed] [Google Scholar]
- 3.Bachmeier CJ, March LM, Cross MJ, et al. Arthritis cost and outcome project group. A comparison of outcomes in osteoarthritis in patients undergoing total hip and knee replacement surgery. Osteoarthritis Cartilage. 2001;9:137–46. doi: 10.1053/joca.2000.0369. [DOI] [PubMed] [Google Scholar]
- 4.Bang MD, Deyle GD. Comparison of supervised exercise with and without manual physical therapy for patients with shoulder impingement syndrome. Journal of Orthopedic & Sports Physical Therapy. 2000;30(3):126–37. doi: 10.2519/jospt.2000.30.3.126. [DOI] [PubMed] [Google Scholar]
- 5.Byrd J. Evaluation of the hip: history and physical examination. North American Journal of Sports Physical Therapy. 2007;2:231–40. [PMC free article] [PubMed] [Google Scholar]
- 6.Chang JD, Yoo JH, Hur M, Lee SS, Chung YK, Lee CJ. Revision total hip arthroplasty for pelvic osteolysis with well-fixed cementless cup. The Journal of Arthroplasty. 2007;22(7):987–92. doi: 10.1016/j.arth.2007.05.049. [DOI] [PubMed] [Google Scholar]
- 7.Cibulka MT, White DM, Woehrle J, et al. Hip pain and mobility deficits- hip osteoarthritis: clinical practice guidelines linked to the International Classification of Functioning, Disability, and Health from the Orthopedic Section of the American Physical Therapy Association. Journal of Orthopedic & Sports Physical Therapy. 2009;39(4):A1–25. doi: 10.2519/jospt.2009.0301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cibulka MT, Delitto A. A comparison of two different methods to treat hip pain in runners. Journal of Orthopedic & Sports Physical Therapy. 1993;17(4):172–176. doi: 10.2519/jospt.1993.17.4.172. [DOI] [PubMed] [Google Scholar]
- 9.Clark VM, Burden AM. A 4-week wobble board exercise programme improved muscle onset latency and perceived stability in individuals with a functionally unstable ankle. Physical Therapy in Sport. 2005;6:181–7. [Google Scholar]
- 10.Delarue Y, de Branche B, Anract P, Revel M, Rannou F. Supervised or unsupervised exercise for the treatment of hip and knee osteoarthritis. Clinical practice recommendations. Annales de réadaptation et de médecine physique. 2007;50(9):759–68. 747. doi: 10.1016/j.annrmp.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 11.Freberger J, Riddle D. Using published evidence to guide the examination of the sacroiliac joint region. Physical Therapy. 2001;81(5):1135–43. [PubMed] [Google Scholar]
- 12.French HP, Cusack T, Brennan A, et al. Exercise and manual physiotherapy arthritis research trial (EMPART)- a multicentre randomized controlled trial. BMC Musculoskeletal Disorders. 2009;10(9) doi: 10.1186/1471-2474-10-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock K. Femoroacetabular impingement: a cause of osteoarthritis of the hip. Clinical Orthopaedics and Related Research. 2003;417:112–20. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 14.Glazebrook M, Daniels T, Younger A, et al. Comparison of health-related quality of life between patients with end-stage ankle and hip arthrosis. The Journal of Bone and Joint Surgery. 2008;90:499–505. doi: 10.2106/JBJS.F.01299. [DOI] [PubMed] [Google Scholar]
- 15.Greenman PE. Principles of Manual Medicine. 3rd ed. Lippincott Williams &Wilkins; Philadelphia, PA: 2003. [Google Scholar]
- 16.Han K, Ricard MD, Fellingham GW. Effects of a 4-week exercise program on balancing using elastic tubing as a perturbation force for individuals with a history of ankle sprains. Journal of Orthopedic & Sports Physical Therapy. 2009;39(4):246–255. doi: 10.2519/jospt.2009.2958. [DOI] [PubMed] [Google Scholar]
- 17.Hansen H, McKenzie-Brown A, Cohen S, Swicegood J, Colson J, Manchikanti L. Sacroiliac joint interventions: a systematic review. Pain Physician. 2007;10:165–84. [PubMed] [Google Scholar]
- 18.Hernández-Molina G, Reichenbach S, Zhang B, Lavalley M, Felson DT. Effect of therapeutic exercise for hip osteoarthritis pain: results of a meta-analysis. Arthritis & Rheumatism. 2008;59(9):1221–1228. doi: 10.1002/art.24010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hoeksma HL, Dekker J, Ronday HK, et al. Comparison of manual therapy and exercise in osteoarthritis of the hip: a randomized clinical trial. Arthritis & Rheumatism. 2004;51(5):722–729. doi: 10.1002/art.20685. [DOI] [PubMed] [Google Scholar]
- 20.Horton SJ, Franz A. Mechanical diagnosis and therapy approach to assessment and treatment of derangement of the sacro-iliac joint. Manual Therapy. 2007;12:126–132. doi: 10.1016/j.math.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 21.Hunter DJ, Lo GH. The management of osteoarthritis: an overview and call to appropriate conservative treatment. Rheumatic Disease Clinics of North America. 2008;4:689–712. doi: 10.1016/j.rdc.2008.05.008. [DOI] [PubMed] [Google Scholar]
- 22.Iverson CA, Sutlive TG, Crowell MS, et al. Lumbopelvic manipulation for the treatment of patients with patellofemoral syndrome: development of a clinical prediction rule. Journal of Orthopedic & Sports Physical Therapy. 2008;38(6):297–309. doi: 10.2519/jospt.2008.2669. [DOI] [PubMed] [Google Scholar]
- 23.Laslett M, Williams M. The reliability of selected pain provocation tests for sacroiliac joint pathology. Spine. 1996;19(11):1243–9. doi: 10.1097/00007632-199405310-00009. [DOI] [PubMed] [Google Scholar]
- 24.Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis & Rheumatism. 2008;58(1):26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lesher JM, Dreyfuss P, Hager N, Kaplin M, Furman M. Hip joint pain referral patterns: a descriptive study. Pain Medicine. 2008;9(1):22–25. doi: 10.1111/j.1526-4637.2006.00153.x. [DOI] [PubMed] [Google Scholar]
- 26.MacDonald CW, Whitman JM, Cleland JA, Smith M, Hoeksma HL. Clinical outcomes following manual physical therapy and exercise for hip osteoarthritis: a case series. Journal of Orthopedic & Sports Physical Therapy. 2006;36(8):588–99. doi: 10.2519/jospt.2006.2233. [DOI] [PubMed] [Google Scholar]
- 27.Martin RL, Sekiya JK. The interrater reliability of 4 clinical tests used to assess individuals with musculoskeletal hip pain. Journal of Orthopedic & Sports Physical Therapy. 2008;38(2):71–6. doi: 10.2519/jospt.2008.2677. [DOI] [PubMed] [Google Scholar]
- 28.Misso ML, Pitt VJ, Jones KM, Barnes HN, Piterman L, Green SE. Quality and consistency of clinical practice guidelines for diagnosis and management of osteoarthritis of the hip and knee: a descriptive overview of published guidelines. Medical Journal of Australia. 2008;189(7):394–399. doi: 10.5694/j.1326-5377.2008.tb02086.x. [DOI] [PubMed] [Google Scholar]
- 29.Mulligan BG. Mobilisations with movement (MWMS) for the hip joint to restore internal rotation and flexion. The Journal of Manual & Manipulative Therapy. 1996;4(1):5–8. [Google Scholar]
- 30.Over S, Sandvik L, Madsen J, Roise O. Modification of the harris hip score in acetabular fracture treatment. Injury. International Journal of the Care of the Injured. 2007;38:344–9. doi: 10.1016/j.injury.2006.04.129. [DOI] [PubMed] [Google Scholar]
- 31.Philippon M, Briggs K, Yen Y, Kuppersmith D. Outcomes following hip arthroscopy for Femoroacetabular impingement with associated chondrolabral dysfunction: minimum two-year follow-up. The Journal of Bone and Joint Surgery. 2009;91:16–23. doi: 10.1302/0301-620X.91B1.21329. [DOI] [PubMed] [Google Scholar]
- 32.Pisters MF, Veenhof C, van Meeteren NLU, et al. Long-term effectiveness of exercise therapy in patients with osteoarthritis of the hip or knee: a systematic review. Arthritis & Rheumatism. 2007;57(7):1245–53. doi: 10.1002/art.23009. [DOI] [PubMed] [Google Scholar]
- 33.Pop T, Szczygielska D, Drubicki M. Epidemiology and cost of conservative treatment of patients with degenerative joint disease of the knee and hip. Ortopedia Traumatologia Rehabilitacja. 2007;9(4):405–12. [PubMed] [Google Scholar]
- 34.Santauida PL, Hawker GA, Hudak PL, et al. Patient characteristics affecting the prognosis of total hip and knee joint arthroplasty: a systematic review. Canadian Journal of Surgery. 2008;51(6):428–46. [PMC free article] [PubMed] [Google Scholar]
- 35.Shrier I, Feldman DE, Gaudet MC, et al. Conservative non-pharmacological treatment options are not frequently used in the management of hip osteoarthritis. Journal of Science and Medicine in Sport. 2006;9:81–86. doi: 10.1016/j.jsams.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 36.Slipman CW, Jackson HB, Lipetz JS, et al. Sacroiliac joint pain referral zones. Achives of Physical Medicine and Rehabilitation. 2000;81:334–8. doi: 10.1016/s0003-9993(00)90080-7. [DOI] [PubMed] [Google Scholar]
- 37.Springer BD, Fehring TK, Griffin WL, Odum SM, Masonis JL. Why revision total hip arthroplasty fails. Clinical Orthopaedics and Related Research. 2009;467:166–173. doi: 10.1007/s11999-008-0566-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Standaert C, Manner P, Herring S. Expert opinion and controversies in musculoskeletal sports medicine: femoroacetabular impingement. Archives of Physical Medicine and Rehabilitation. 2008;89:890–3. doi: 10.1016/j.apmr.2008.02.013. [DOI] [PubMed] [Google Scholar]
- 39.Sutlive TG, Lopez HP, Schnitker DE, et al. Development of a clinical prediction rule for diagnosing hip osteoarthritis in individuals with unilateral hip pain. Journal of Orthopedic & Sports Physical Therapy. 2008;38(9):542–550. doi: 10.2519/jospt.2008.2753. [DOI] [PubMed] [Google Scholar]
- 40.Tannast M, Goricki D, Beck M, Murphy S, Siebenrock K. Hip damage occurs at the zone of femoroacetabular impingement. Clinical Orthopaedics and Related Research. 2008;466:273–80. doi: 10.1007/s11999-007-0061-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Teyhen DS, Rieger JL, Westrick RB, Miller AC, Molloy JM, Childs JD. Changes in deep abdominal muscle thickness during common trunk-strengthening exercise using ultrasound imaging. Journal of Orthopedic & Sports Physical Therapy. 2008;38(10):596–605. doi: 10.2519/jospt.2008.2897. [DOI] [PubMed] [Google Scholar]
- 42.Vaughn DW. Isolated knee pain: a case report highlighting regional interdependence. Journal of Orthopedic & Sports Physical Therapy. 2008;38(10):616–23. doi: 10.2519/jospt.2008.2759. [DOI] [PubMed] [Google Scholar]
- 43. [6/1/2009];Valerie Waters Red Carpet Ready: 6 week total body transformation system. Available at: http://www.redcarpetready.com.
- 44.Weir A, de Vos RJ, Moen M, Hölmich P, Tol JL. Prevelance of radiologic signs of femoroacetabular impingment in patients presenting with long standing adductor related groin pain. British Journal of Sports Medicine. 2009 July 20;:50. doi: 10.1136/bjsm.2009.060434. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 45.Yelin E, Murphy L, Cisternas M, Foreman A, Pasta D, Helmick C. Medical expenditures and earnings losses of persons with arthritis and other rheumatic conditions in 200 with comparisons to 1997. Arthritis & Rheumatism. 2007;56(5):1397–1407. doi: 10.1002/art.22565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zake Yamuna, Golden Stephanie. The Ultimate Body Rolling Workout: The Revolutionary Way to Tone, Lengthen, and Realign Your Body. Broadway Books; New York, NY: 2003. [Google Scholar]
- 47.Zhang W, Moskowitz RW, Nuki G, et al. OARSI recommendations for the management of hip and knee osteoarthritis, part II: critical appraisal of existing treatment guidelines and systematic review of current research evidence. Osteoarthritis and Cartilage. 2008;16:137–162. doi: 10.1016/j.joca.2007.06.014. [DOI] [PubMed] [Google Scholar]