Abstract
This study assessed a 26-week voucher-based intervention to reinforce abstinence and participation in treatment-related activities among substance-abusing offenders court referred to outpatient treatment under drug diversion legislation (California's Substance Abuse and Crime Prevention Act). Standard treatment consisted of criminal justice supervision and an evidence-based model for treating stimulant abuse. Participants were randomly assigned to four groups, standard treatment (ST) only, ST plus vouchers for testing negative, ST plus vouchers for performing treatment plan activities, and ST plus vouchers for testing negative and/or performing treatment plan activities. Results indicate that voucher-based reinforcement of negative urines and of treatment plan tasks (using a flat reinforcement schedule) showed no statistically significant effects on measures of retention or drug use relative to the standard treatment protocol. It is likely that criminal justice contingencies had a stronger impact on participants' treatment retention and drug use than the relatively low-value vouchers awarded as part of the treatment protocol.
Keywords: drug diversion treatment, Substance Abuse and Crime Prevention Act, California, contingency management, voucher-based reinforcement therapy, experimental design
Extensive research on contingency management interventions among drug abusers has resulted in a substantial literature documenting the effectiveness of this approach. An important next step is to test its effectiveness in the context of the criminal justice system because a high proportion of drug abusers find themselves enmeshed in the criminal justice system resulting in high costs to society.
Contingency Management for Substance Abusers
Contingency management (CM) has been extensively investigated and shown to be a highly effective treatment for drug abuse disorders, particularly in its ability to reinforce continuous abstinence during treatment (Higgins & Silverman, 1999; Lussier, Heil, Mongeon, Badger, & Higgins, 2006; Prendergast, Podus, Finney, Greenwell, & Roll, 2006; Silverman, 2004). Voucher-Based Reinforcement Therapy (VBRT) is a commonly used type of CM that has been shown to be effective in many studies (Higgins, Alessi, & Dantona, 2002; Higgins, Budney, Bickel, Hughes, Foerg & Badger, 1993; Higgins, Budney, Bickel, Foerg, Donham & Badger, 1994; Higgins, Roll, Wong, Tidey, & Dantona, 1999; Kidorf & Stitzer, 1999; Lussier, Heil, Mongeon, Badger, & Higgins, 2006; Silverman, Preston, Stitzer, & Schuster, 1999). In this approach, participants receive “vouchers” as reinforcement for providing biological samples (urine or breath) that indicate no recent drug use. In addition, vouchers are withheld when the biological sample indicates recent drug use.
Although it is well-established that CM assists drug treatment participants by reinforcing continuous abstinence during treatment, several studies have found that the CM effect is of limited duration. When CM is discontinued, there is usually a return to drug use, although not necessarily to baseline levels (Silverman, Chutuape, Bigelow, & Stitzer, 1996; Stitzer, Bigelow, & Leibson, 1980; Stitzer, Bigelow, Leibson, & Hawthorne, 1982). In order to increase the duration of the CM effect through exposure to naturally available rewards, researchers created a procedure in which contingent reinforcement is applied to the development of new, prosocial alternative behaviors that are (in principle) incompatible with illicit drug use (Morral, Iguchi, & Belding, 1999). An extensive body of experimental research has demonstrated that reinforcing an alternative, competing behavior can be a powerful strategy in reducing the frequency of a target behavior (Leitenberg, Rawson, & Bath, 1970; Rawson & Leitenberg, 1973; Petry, Tedford, & Martin, 2001). One method for systematically implementing this strategy with illicit drug users is to specify behaviors (e.g., family activities, new hobbies, employment) that are incompatible with illicit drug use and to use CM procedures to increase the frequency of these “competing” behaviors. The rationale is that using vouchers to reinforce prosocial, nondrug-related behaviors will initiate new behaviors and that the naturally occurring reinforcing consequences of these behaviors will help to sustain abstinence when the CM procedure is discontinued.
The use of voucher-based contingent reinforcement of activities consistent with treatment goals has been evaluated within an opioid detoxification program (Bickel, Amass, Higgins, Badger, & Esch, 1997), a methadone maintenance program (Iguchi, Belding, Morral, Lamb, & Husband, 1997), and a community drug treatment program (Petry, et al., 2006). Treatment plan activities consisted of achievable, incremental behavioral tasks that were incompatible with continued illicit drug use (e.g., employment interview, attending a parenting class, attending school, joining an exercise group) and that could be documented as has having occurred. Bickel et al. (1997) found that the total number of activities completed correlated with length of abstinence and retention. Iguchi (Iguchi, et al., 1997) found that the reduction in positive urine samples was significantly superior to the no-voucher group and the drug-contingent-voucher group. In addition, the treatment plan condition produced a reduction in illicit drug use that was sustained following discontinuation of the CM procedure, whereas drug-contingent vouchers did not. Other evidence of sustained treatment benefits from treatment plan contingencies is reported in Morral et al. (1999); however, Petry et al. (2006) were not able to replicate these findings.
CM researchers have encouraged the integration of CM procedures into real world treatment programs, including programs designed for individuals involved in the criminal justice system. In a manual published by the National Institute on Drug Abuse (Budney & Higgins, 1998), use of CM with a wide range of illicit drug user populations was suggested as part of a community reinforcement approach. Similarly, Crowley (1999) and, more recently, the National Institute on Drug Abuse (2006) encouraged the use of CM with criminal justice populations. Despite these recommendations, there is limited information on the effectiveness of CM with the substance-abusing offenders. This population is already subject through the criminal justice system to various contingencies, including punishment, intended to change behavior, and may respond to voucher reinforcement differently from other types of treatment participants.
Contingency Management in Offender Populations
Contingency management and its earlier manifestation, behavior modification, have been used among juvenile and adult offenders since the 1960s. In most cases, research has been undertaken with juvenile offenders or with adults in institutional settings (Remington & Remington, 1987; Rutherford, 2006). CM research with adult offenders in community settings is extremely limited. Polakow and Doctor (1974) found that CM in the form of probation sentence reductions significantly increased attendance and employment and decreased probation violations and arrests. Funderburk, Mackenzie, DeHaven, and Stefan (1993) reported on a quasi-experimental CM study of violent offenders in alcoholism treatment that reinforced program attendance and participation. Those actively participating in CM showed improvements in several areas, including fewer violent crimes and improved employment and social adjustment. The effects of CM on retention could not be reported because this post-hoc study selected groups based on attendance (active vs. intermittent). Recently, we (Prendergast, Hall, Roll, & Warda, 2008) reported on a CM study with a community population of criminal justice clients enrolled in drug court. We found that low-cost incentives failed to achieve statistically significant improvements in attendance or drug use, most likely due to the greater influence of the judge and the sanctions he could impose. Carroll et al. (2006) conducted a study with young adults in the criminal justice system. They found that therapies with CM added to reinforce attendance and drug abstinence were more effective in increasing retention than the therapies alone. Marlowe and Wong (2008) suggest that structured behavioral interventions such as CM are ideally suited for high-risk offenders and may be ineffective for low-risk offenders. This is because low-risk offenders are thought to be more likely to adjust course on their own, while high-risk offenders are “likely to require intensive interventions to dislodge their entrenched behavioral patterns” (Marlowe & Wong, 2008, p. 346). Clearly, additional research with offender populations needs to be undertaken.
California's Substance Abuse Crime and Prevention Act
In November 2000, 61% of the voters in California approved Proposition 36, which was enacted into law as the Substance Abuse and Crime Prevention Act (SACPA) (California Penal Code, Section 1210). SACPA provides that adults who are convicted of nonviolent drug offenses and who are otherwise eligible for SACPA must be offered probation with drug treatment instead of probation without treatment or incarceration. Offenders on probation or parole who commit nonviolent drug offenses or who violate drug-related conditions of their release are also eligible for SACPA treatment instead of incarceration. SACPA participants who commit non-drug-related violations of probation or parole or who are arrested for new non-drug-related crimes may face termination from SACPA. The consequences of drug violations depend on the severity and the number of such violations. Generally, offenders can have three non-violent drug-related arrests or violations before they are terminated from SACPA. Although judges may respond to drug-related arrests or violations with increased treatment requirements, the legislation prohibits the use of jail sanctions for the first two arrests or violations. While reporting on participant status varies by county, in most cases, treatment programs issue participant progress reports to probation/parole departments quarterly or if participants cease to attend treatment. After successful completion of treatment and fulfillment of other SACPA conditions, offenders on probation can petition for their conviction to be set aside.
SACPA began implementation in July 2001 and operated until June 2006; new legislation passed in July 2006 reauthorized the SACPA program (Chapter 63, Statutes of 2006, SB 1137). Evaluations have been conducted of various aspects of SACPA, including policy (Klein, Miller, Noble, & Speiglman, 2004; Percival, 2004) and program outcomes (Farabee, Hser, Anglin, & Huang, 2004; Hser, et al., 2003; Longshore, et al., 2004; Longshore, et al., 2005;Urada et al., 2007).
The goal of this study was to determine the effectiveness of the use of vouchers to reinforce abstinence and positive behaviors among offenders participating in a SACPA treatment program. The study was intended to partially replicate the study by Iguchi et al. (1997), but with three main differences. The present study (1) took place in a drug-free outpatient program (rather than in a methadone program) with (2) participants who were participating in a diversion drug treatment program and whose (3) drug of choice was primarily methamphetamine (rather than heroin). It should be noted that this study was not a direct evaluation of the effectiveness of SACPA, but rather an evaluation of a specific approach (voucher-based contingency management) designed to enhance the outcomes of offenders participating in a SACPA treatment program.
Methods
Procedures
The intervention took place in a San Bernardino County (California) SACPA treatment program that has been operated by Matrix Institute since July 2001. Participants were recruited from January 2003 through April 2004 and participated in the intervention during their initial 26 weeks (6 months) of participation. Although the judge allowed SACPA participants to enroll in the study, he was not directly involved in the study and was not informed of which study participant was in which condition. At the time of this study, the Rancho Cucamonga court was implementing SACPA using a drug court model, however, statutory limitations prevented full adherence to the drug court model (in particular, brief incarcerations for program violations are prohibited under SACPA). Nevertheless, at monthly status hearings, the judge employed other sanctions for program violations, such as community service, additional self-help group attendance, and restarting (lengthening) SACPA program involvement. The judge rewarded clients' treatment progress through decreased court appearances, treatment attendance, and drug testing.
The UCLA Institutional Review Board and the Friends Research Institute Institutional Review Board approved the study procedures.1 All study participants were volunteers and were informed that they could withdraw from the study at any time and that refusal to participate or withdrawal from the study would not affect their receipt of treatment. They were also informed that their decision to participate or not would have no effect on their status within the treatment program or on their relationship with any criminal justice, treatment, or other public agency that they might be involved with. In San Bernardino, SACPA participants pay nothing to the Matrix Institute, however, they pay a $520 fee to the county.
All SACPA participants who were admitted to the Matrix treatment program were eligible to participate in the study. Those who agreed to participate in the study were randomly assigned to one of four groups shortly after admission to the Matrix program. The two conditions being evaluated were contingent vouchers for drug-free urine samples (drug testing variable) and contingent vouchers for completion of assigned treatment plan tasks (treatment-plan variable). The resulting four conditions were:
Standard Treatment Condition
Participants assigned to the Standard Treatment group received usual Matrix treatment and no additional services or intervention. The Matrix model is a manualized cognitive-behavioral treatment program that includes group sessions on relapse prevention, drug education, and social support; individual counseling; and urine and breath testing. Several evaluations of the model have supported its efficacy with cocaine and methamphetamine users (Obert, et al., 2000). All clients attended three sessions per week for 17 weeks; then, one session per week for 11 weeks; then, voluntary aftercare. The standard treatment condition served as the “platform” for all of the groups.
In the other three conditions, participants received vouchers for demonstrating certain behaviors. In all conditions, each voucher was worth $10.00. Vouchers could only be exchanged for those goods or services that were in line with developing a drug-free lifestyle, including payment of drug court treatment fees (see, Roll, Prendergast, Sorensen, Prakash, & Chudzynski, 2005 for more detail on types of exchanges). With assistance from their counselors and research staff, participants decided on the voucher exchange items. Once a request was made, a staff member made the transaction for the participant within approximately one working day.
Drug Testing Condition
Participants in the Drug Testing group received a voucher for each urine specimen that tested negative for unauthorized drugs (opiates, cocaine, methamphetamine, benzodiazepines, marijuana, and alcohol via breathalyzer test). Participants were randomly tested two times per week during the intervention, for a maximum total of $20 per week. (This drug testing schedule paralleled that done for SACPA so as not to overly inconvenience clients with additional tests.)
Treatment Plan Condition
Participants in the Treatment Plan group received up to two vouchers each week (maximum total of $20 per week) for completing treatment plan tasks that were clearly defined and verifiable. When practical, shaping of participants' behavior took place (i.e., moving from resume creation to job search to job interview to employment), but some activities were single events (i.e., assisting a relative to move). Clients were required to document treatment plan activities through receipts, appointment slips, ticket stubs, photocopies of job applications, timesheets from work, church bulletins, and other similar paper documentation. When necessary, research staff made phone calls to verify activities. Participants met with research staff twice a week to turn in documentation of their activities and plan for upcoming activities.
Combined Condition
Participants in the Combined group could earn vouchers for submitting negative drug specimens (two per week) and for completing two specific treatment plan tasks per week (maximum total of $40 per week). Both target behaviors—abstinence and treatment plan tasks—were reinforced through vouchers, but the two behaviors were reinforced independently. That is, Combined group participants could earn vouchers for completing treatment plan tasks even if they tested positive; similarly, vouchers for negative drug tests could be earned despite failure to complete a treatment plan task.
The maximum amount SACPA participants could earn in vouchers over the course of the study was determined by their assigned group. The Standard Group received no vouchers ($0); the Drug Testing Group could earn up to $520 ($20/week for 26 weeks); the Treatment Plan group could earn up to $520; and the Combined Group could earn up to $1,040 ($40/week for 26 weeks).
The most common activities that Treatment Plan and Combined group members undertook were related to employment (e.g., putting together a resume, submitting job applications, getting job-related documentation) and family (e.g., taking children on outings, taking spouse to a sober event, helping elderly or disabled family members). These findings are similar to those reported in Prendergast et al. (2008).
On the basis of previous research on contingency management, the expectation was that each of the three voucher conditions would be more effective than the Standard condition and that among the voucher conditions, the Combined condition would be more effective than the Treatment Plan condition, which would, in turn, be more effective than the Drug Testing condition.
Participants
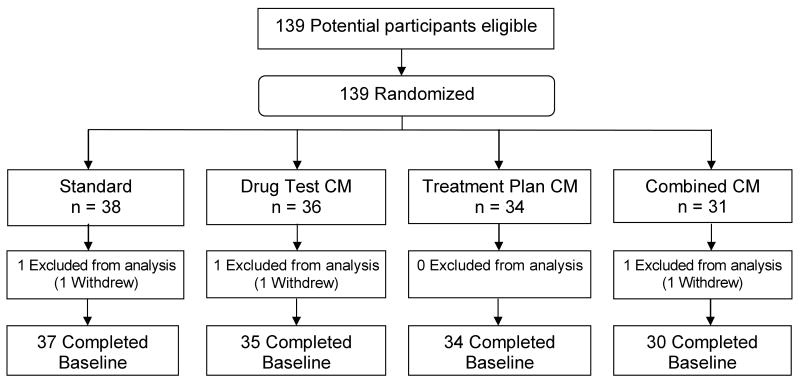
A total of 139 participants were enrolled into the study between January 2003 and March 2004 and were randomized into one of the four conditions described above. There were no study refusers. Three participants withdrew from the study, leaving a total of 136 participants for analysis. (See Figure 1 for the flow of participants through the study.)
Figure 1. Study Design.
Table 1 shows selected background characteristics of the study participants in each of the four conditions. In general, the randomization procedure resulted in similarity in background characteristics across the four study groups. At baseline, there were significant or near-significant differences among the groups in BSI Global Score and mean months of prior incarceration. We controlled for these group differences in all multivariate analyses. Participants were typically methamphetamine-using males in their early thirties and were primarily white and Latino. About half had never been married. The average participant had not completed high school. Few had been working in the past 30 days. Most were living with parents, relatives, or friends. Illicit drug use typically began about age 12. Participants reported having been arrested a mean of 6 to 7 times, and length of time incarcerated ranged from 8 to nearly 25 months across the groups.
Table 1. Background Variables of Participants in Each of the Study Conditions.
| Variable | Study Condition | p* | |||
|---|---|---|---|---|---|
| Standard n=37 | Drug Testing n=35 | Treatment Plan n=34 | Combined n=30 | ||
| Gender, % women | 16.2 | 20.0 | 32.4 | 10.0 | 0.14 |
| Ethnicity, % | 0.72 | ||||
| White | 46.0 | 57.1 | 61.8 | 56.8 | |
| Hispanic | 51.4 | 37.1 | 32.4 | 40.0 | |
| African American | 2.7 | 5.7 | 2.9 | 3.3 | |
| Other | 0.0 | 0.0 | 2.9 | 0.0 | |
| Marital status, % never married | 51.4 | 62.9 | 47.1 | 56.7 | 0.58 |
| Living situation, % with parents, relatives, or friends | 63.2 | 66.7 | 64.7 | 58.1 | 0.90 |
| Primary drug, % methamphetamine | 76.3 | 80.6 | 88.2 | 83.9 | 0.71 |
| Injection of drugs in past 30 days, % Yes | 2.6 | 0.0 | 2.9 | 0.0 | 0.59 |
| Age, mean years (SD) | 31.7 (8.0) | 32.6 (8.6) | 31.8 (8.6) | 33.0 (9.9) | 0.91 |
| Education, mean years (SD) | 11.8 (1.1) | 12.2 (1.0) | 11.8 (1.9) | 12.1 (1.5) | 0.70 |
| Employed in past 30 days, mean days (SD) | 9.6 (10.3) | 8.4 (9.9) | 8.9 (9.6) | 10.8 (10.5) | 0.79 |
| BSI Global Severity Index, mean (SD) | 0.3 (0.4) | 0.5 (0.8) | 0.2 (0.4) | 0.2 (0.3) | 0.04 |
| Age of first use of any illicit drug, mean years (SD) | 11.9 (3.6) | 12.5 (3.9) | 13.1 (3.5) | 12.2 (2.7) | 0.55 |
| Use of primary drug, mean years (SD) | 9.0 (6.7) | 7.8 (5.5) | 9.0 (7.3) | 8.7 (5.8) | 0.85 |
| Prior arrests, mean (SD) | 6.7 (4.0) | 6.7 (4.1) | 6.4 (5/1) | 7.8 (5.2) | 0.60 |
| Prior incarceration, mean months (SD) | 8.4 (11.6) | 9.9 (17.3) | 16.8 (37.0) | 24.8 (36.5) | 0.06 |
Based on ANOVA for continuous variables and on chi-square for categorical variables.
Measures
Participants were assessed at baseline. In addition, drug testing and voucher data were collected weekly for 26 weeks starting at baseline. Baseline interviews were conducted at the Matrix treatment program. Participants were not reimbursed for the baseline interview.
The baseline assessment included questions on demographic characteristics, physical health, mental health, criminal history, criminal justice involvement, drug use history, and quality of life. In addition, the assessments included two standard measures of addiction and psychological functioning: the Addiction Severity Index and the Brief Symptom Inventory. The Addiction Severity Index (ASI) is widely used for clinical and research purposes to determine problem severity and service needs in seven domains of functioning: alcohol problems, drug problems, employment/education, family/social, legal, medical, and psychological. The index has excellent inter-rater and test-retest reliability as well as discriminant and concurrent validity (Bovasso, Alterman, Cacciola, & Cook, 2001; Kosten, Rounsaville, & Kleber, 1983; McLellan, Alterman, Cacciola, Metzger, & O'Brien, 1992). The Brief Symptom Inventory (BSI) (Derogatis & Melisaratos, 1983) is a 53-item questionnaire that assesses nine medical and psychological symptom dimensions: somatization, obsessive-compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism. The scores can be combined to form a Global Severity Index. Across the dimensions, internal consistency estimates (Cronbach's alpha) range from .71 to .85, and test-retest reliability estimates range from .68 to .91. As part of the CM intervention, on-site urine tests were conducted twice a week during the 26-week intervention to detect opiates, cocaine, methamphetamine, benzodiazepines, and marijuana. Specimens were screened by the enzyme multiplied immunoassay technique and confirmed by gas chromatography/mass spectrometry at standard cut-off points. Breathalyzer tests to detect alcohol use were conducted at the same times as the urine tests. In addition, urine and breath samples were obtained at the baseline and the 26-week interviews. Data for analysis also included treatment attendance from program records.
Analysis
The current analysis includes data from baseline through the 26-week intervention period. To determine the extent to which randomization resulted in equivalence across study conditions, we examined the following background variables assessed at baseline: age, gender, race/ethnicity, educational level, marital status, employment, living situation, primary drug, first year of illicit drug use, years of primary drug use, drug injection, Brief Symptom Inventory global score, prior arrests, and prior incarceration. Descriptive information on the voucher intervention includes the mean dollar amount of voucher earnings.
The independent variable of interest was treatment condition, as defined above. The dependent variables included treatment retention and drug use. Specifically, treatment retention was defined by two measures: the percentage of participants who completed the full 26-week voucher intervention and the number of weeks that participants spent in treatment (i.e., even if attendance was sporadic, each week in which participants participated in the intervention was counted up to 26 weeks). Based on drug and alcohol test results, several drug use measures over the course of treatment were examined: the mean number of negative tests, the mean number of tests to the first positive test (for participants who were negative at baseline), and the mean longest number of consecutive negative tests. We also determined the percentage of negative tests (for all drugs over 26 weeks), the percentage of positive tests, and the percentage of missing tests.
For bivariate analysis, continuous variables were compared using ANOVA; categorical variables were compared using chi-squire. For tests comparing means, missing drug tests (due to either a refusal or a missed session) were coded as positive (the most conservative approach).
Cox regression survival analysis was chosen for time-to-event analyses because it does not require a normal distribution (time to an event is rarely normally distributed), allows the inclusion of cases who remained in treatment, or remained abstinent from drugs/alcohol, and allows the inclusion of covariates to assess their effects on the probability of survival time. Treatment Group (with Standard treatment as the reference group) was entered as the predictor variable. The analyses included as covariates those variables on which the four groups significantly differed at baseline. The following control variables were entered into the Cox regression analyses: gender (1 = Male, -1 = Female), BSI Global Severity Index score (continuous), number of months of prior incarceration (continuous), and number of years of education (continuous). Time to treatment drop out was calculated in weeks (range 0-26), with treatment retention defined as the week number of the participant's last treatment attendance. Time to first drug use was calculated as the total number of tests until the first positive drug test. In order to account for those who tested positive during the first week of the intervention but then became abstinent, the analysis for time to first drug use started at the beginning of the second week of the intervention. In addition, missing drug tests that were preceded and followed by clean tests were counted as clean. This was done so that one missed test would not result in a participant being dropped prematurely from the analysis (two tests per week possible, starting the second week, range 0-50). Similar procedures for handling missing drug tests have been employed by other researchers in CM studies (Petry, et al., 2005). The Cox regression survival analyses were performed using SPSS for Windows, release 14.0.2.
Weekly drug test results were compared across conditions using Generalized Estimating Equations (GEE). The GEE approach provides a flexible way of modeling longitudinal, repeated measures data and can be used for a broad range of data distributions, such as normal, Poisson, binomial, and gamma. We selected the GEE with a binomial distribution to examine weekly drug test results (Diggle, Heagerty, Liang, & Zeger, 2002; Stokes, Davis, & Koch, 2000), with the variables listed above as covariates. The GEE analysis was performed using SAS 9.1.3.
Results
Voucher Earnings
The Standard Group, by design, received no vouchers ($0); the Drug Testing Group earned a mean of $227 (SD $199); the Treatment Plan group earned a mean of $103 (SD $142); and the Combined Group earned a mean of $266 (SD $243). Apparently, participants in the Drug Testing Group found it easier to earn vouchers than did those in the Treatment Plan Group. Participants in the Combined Group earned a higher amount than did the other groups since they could earn vouchers both for testing negative and for completing treatment plan tasks. Each of the groups earned less than half of the maximum earnings amount.
Treatment Retention
Bivariate analysis shows that less than half of SACPA participants in each group completed the intervention (30%−43%) and that retention (mean weeks in the intervention) was 17 − 19 weeks (out of 26). As Table 2 indicates, the differences in completion and retention across groups were not significant.
Table 2. Retention of Participants over the 26-Week Intervention.
| Variable | Study Condition | p* | |||
|---|---|---|---|---|---|
| Standard n=37 | Drug Testing n=35 | Treatment Plan n=34 | Combined n=30 | ||
| Participants who completed intervention, % | 35 | 43 | 38 | 30 | 0.75 |
| Number of weeks in intervention, mean (SD) | 18.5 (9.6) | 16.9 (10.3) | 19.2 (8.6) | 16.5 (9.8) | 0.63 |
Based on ANOVA for continuous variables and on chi-square for categorical variables.
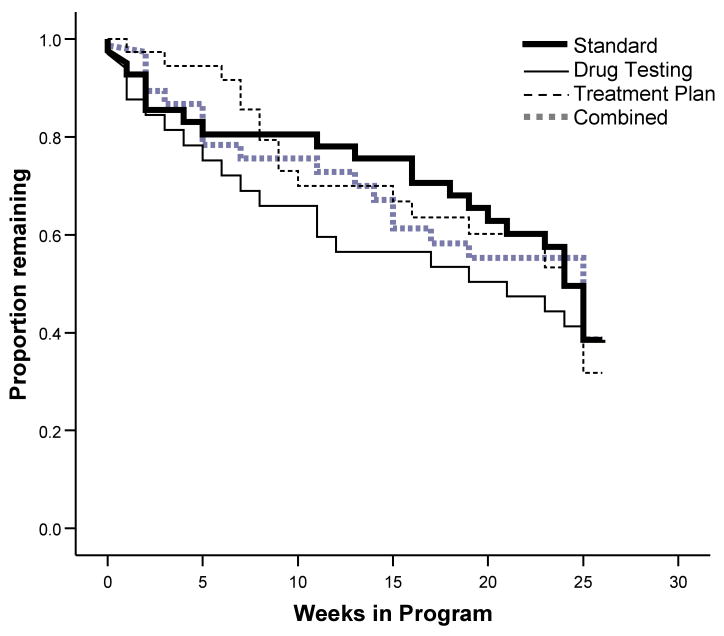
Table 3 presents the results of the Cox regression analysis of time to treatment drop out for study participants. Data were complete for 136 participants, and 50 cases were censored because they remained in treatment to the end of the study. Time to treatment drop out was predicted by the model as a whole (likelihood ratio chi-square statistic [7] = 15.53, p = .03). Although no CM effect is evident, education was significantly associated with differing rates of treatment retention; those with greater education were significantly less likely to drop out of treatment. In addition, the association between gender and treatment retention neared significance. Men were 1.33 times more likely than women to drop out of treatment. Figure 2 presents the survival curves associated with the Cox regression analysis of time to treatment drop out.
Table 3. Time to Treatment Drop Out During the 26-Week Intervention (Cox Regression Survival Analysis, with Covariates).
| β Coefficient | Standard Error | p | Odds Ratio (OR) | 95% Confidence Interval of OR | ||
|---|---|---|---|---|---|---|
| Combined1 | -.05 | .21 | .80 | .95 | .63 | 1.43 |
| Drug Testing1 | .11 | .20 | .58 | 1.12 | .75 | 1.67 |
| Treatment Plan1 | .00 | .19 | .99 | 1.00 | .69 | 1.47 |
| Gender (female) | .28 | .17 | .09 | 1.33 | .96 | 1.84 |
| Years of education | -.23 | .08 | .01 | .79 | .67 | .93 |
| BSI 2 | -.27 | .23 | .25 | .77 | .49 | 1.21 |
| Months of prior incarceration2 | .01 | .00 | .21 | 1.01 | 1.00 | 1.01 |
Compared to Standard Treatment group
Continuous variable
Figure 2. Cox Regression Survival Analysis: Retention in Treatment for Four Treatment Conditions.
During-Treatment Changes in Drug Use
Urine tests were conducted twice a week during the 26-week intervention for a total of 52 tests. Like Silverman et al. (Silverman, Robles, Mudric, Bigelow, & Stitzer, 2004), we examined individual patterns of drug abstinence, use, and missed tests. However, unlike Silverman's findings, there were no differences evident among the groups. In all four groups, approximately one-third of study participants were able to maintain abstinence for extended periods of time, while the other two-thirds struggled with drug use and treatment attendance.
Table 4 presents three measures of drug use over the 26 weeks of the intervention: mean number of negative tests, mean number of tests to the first positive test, and mean number of consecutive negative tests. For these analyses, missed tests were counted as positive. None of the differences among the study groups on the three measures was significant. Additionally, separate analyses were made for the percentage of negative tests (for all drugs over 26 weeks), the percentage of positive tests, and the percentage of missing tests, and are presented in Table 4.
Table 4. Urine Test Results for Participants during the 26-Week Intervention Period.
| Variable | Study Condition | p* | |||
|---|---|---|---|---|---|
| Standard n=37 | Drug Testing n=35 | Treatment Plan n=34 | Combined n=30 | ||
| Number of negative tests, mean (SD) | 25.3 (18.2) | 23.9 (19.5) | 25.4 (16.7) | 21.6 (16.8) | 0.81 |
| Number of tests to first positive test (for those negative at baseline), mean (SD) | 3.2 (5.8) | 2.7 (4.8) | 4.9 (10.5) | 4.0 (8.0) | 0.64 |
| Longest number of consecutive negative tests, mean (SD) | 13.1 (11.6) | 12.4 (11.6) | 11.8 (11.1) | 11.6 (11.7) | 0.99 |
| Negative tests (for all drugs), % | 48.8 | 46.0 | 49.2 | 41.7 | 0.81 |
| Positive tests (for all drugs), % | 4.6 | 4.4 | 4.2 | 4.9 | 0.96 |
| Missing tests, % | 46.6 | 49.6 | 46.7 | 53.5 | 0.83 |
Note: Maximum number of tests is 52. Percentages may not add up to 100% due to rounding error.
Based on ANOVA for continuous variables and on chi-square for categorical variables.
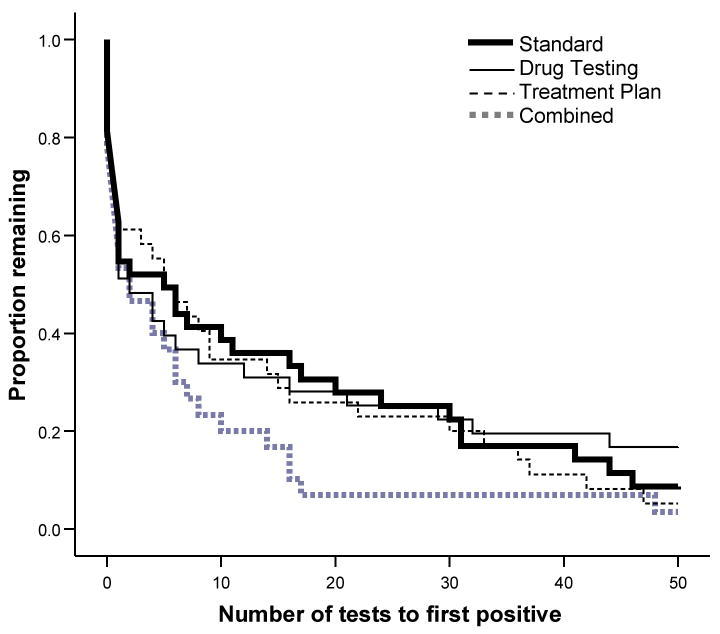
The Cox regression analysis of time to first drug use is presented in Table 5. Data were complete for 136 participants, and 12 cases were censored because they tested negative throughout the study. Time to first drug use was not predicted by the model (likelihood ratio chi-square statistic [7] = 3.15, p = .87). Figure 3 presents the survival curves associated with the Cox regression analysis of time to first drug use at the mean of covariates. Although not significant, the Combined group appears to trend toward a more rapid return to drug use.
Table 5. Time to First Drug Use for Participants during the 26-Week Intervention (Cox Regression Survival Analysis, with Baseline Covariates).
| β Coefficient | Standard Error | p | Odds Ratio (OR) | 95% Confidence Interval of OR | ||
|---|---|---|---|---|---|---|
| Combined1 | .23 | .17 | .18 | 1.26 | .90 | 1.77 |
| Drug Testing1 | -.14 | .18 | .42 | .87 | .62 | 1.22 |
| Treatment Plan1 | -.01 | .16 | .94 | .99 | .73 | 1.35 |
| Gender (female) | .08 | .12 | .49 | 1.09 | .86 | 1.38 |
| Years of education | -.01 | .06 | .83 | .99 | .87 | 1.12 |
| BSI2 | -.02 | .20 | .92 | .98 | .66 | 1.45 |
| Months of prior incarceration2 | -.00 | .00 | .90 | 1.00 | .99 | 1.01 |
Compared to Standard Treatment group
Continuous variable
Figure 3. Cox Regression Survival Analysis: Time to First Drug Use for Four Treatment Conditions.
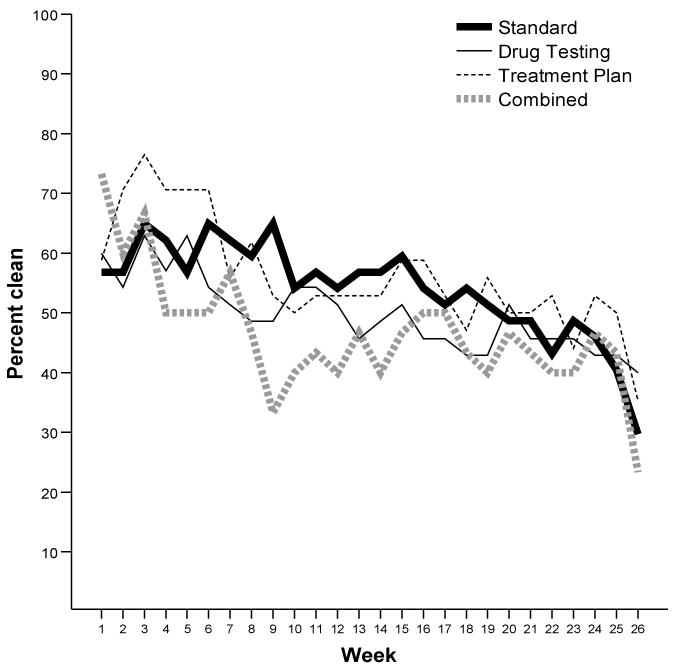
Figure 5 shows the weekly percentage of participants testing negative for drugs/alcohol. The GEE analysis of participants testing negative each week (Table 6) indicates no difference among the treatment groups over the intervention period (χ2 = 1.85, df = 3, p = 0.60). However, the percentage of participants testing negative each week declined over time, showing there was a strong time effect (χ2 = 25.35, df = 1, p < .0001).
Table 6. Weekly Percentage of Participants Testing Negative during the 26-Week Intervention (GEE, with Baseline Covariates).
| β Coefficient | Standard Error | p | 95% Confidence Interval | ||
|---|---|---|---|---|---|
| Combined1 | 0.19 | 0.50 | 0.71 | -0.80 | 1.17 |
| Drug Testing1 | -0.32 | 0.46 | 0.49 | -1.22 | 0.59 |
| Treatment Plan1 | 0.19 | 0.45 | 0.66 | -0.68 | 1.07 |
| Week | -0.04 | 0.02 | 0.01 | -0.07 | -0.01 |
| Gender (female) | 0.12 | 0.31 | 0.70 | -0.49 | 0.73 |
| Years of education | 0.12 | 0.08 | 0.14 | -0.04 | 0.28 |
| BSI2 | 0.50 | 0.25 | 0.04 | 0.01 | 0.99 |
| Months of prior incarceration2 | -0.01 | 0.01 | 0.22 | -0.02 | 0.00 |
| Week × Drug Testing1 | 0.02 | 0.02 | 0.64 | -0.03 | 0.05 |
| Week × Treatment Plan1 | 0.00 | 0.02 | 0.96 | -0.04 | 0.04 |
| Week × Combined1 | -0.02 | 0.03 | 0.52 | -0.07 | 0.03 |
Compared to Standard Treatment group
Continuous variable
Discussion
The purpose of the study was to determine the effectiveness of the use of vouchers to reinforce abstinence and treatment-related activities within the context of a treatment program that provided services to substance-abusing offenders referred from court under drug diversion legislation (California's SACPA program). Within the four-group design, all study participants received a standard evidence-based model for treating stimulant abuse; one group received the standard treatment only, one group received vouchers for testing negative, one group received vouchers for performing treatment plan activities, and one group received vouchers for testing negative and/or performing treatment plan activities. This analysis used data from measures taken at baseline and during treatment. Unlike virtually all other studies that have examined the effectiveness of contingency management protocols, the participants in this study were participant both to the contingencies available in the voucher study and to those imposed by the judge and other criminal justice agents involved in SACPA.
Contrary to what has been reported in many previous studies regarding the positive and strong impact of vouchers on drug use and other behaviors (Higgins & Silverman, 1999; Lussier, et al., 2006; Prendergast, et al., 2006), the findings from this study with offenders in a drug diversion treatment program indicated that voucher reinforcement of negative urines and of treatment plan tasks showed no statistically significant effect on measures of retention or drug use relative to standard treatment. A similar outcome was found in another study conducted with drug court participants with the same judge and the same treatment program (Prendergast, et al., 2008).
There are a number of possible explanations for why we were unable to detect a CM-treatment effect. One likely explanation is that the SACPA drug diversion treatment court program in conjunction with the Matrix model treatment overrode or competed with the effect of CM. Although the SACPA and drug court models represent different approaches to drug diversion treatment, at the court used in this study, the judge used elements from the drug court model in dealing with SACPA participants. This notion of treatment court effects overriding CM effects is supported by a finding by Rawson, et al. (2004) in a multi-site study of the Matrix Model for stimulant treatment. One of the eight study sites was a drug court treatment program, and, unlike in all the other sites, the model did not increase the mean number of methamphetamine-free urine samples over treatment as usual in the drug court program. Of greater interest is that of all eight study sites, the drug court site had the highest mean number of urine negative samples in both conditions, suggesting that the effect was mainly due to the influence of the judge or to other elements of the drug court model. The fact that retention in the current study at 25 weeks (approximately 40%) was better than that in a previous study of the Matrix Model alone (approximately 30%) conducted at the same site (Huber et al., 1997) also argues for the SACPA court effect.
Two elements of the drug court model that are particularly important are the periodic status hearings that participants must attend and the rewards and sanctions that the judge imposes for positive or negative behaviors (Marlowe, Festinger, & Lee, 2004; Marlowe, Festinger, Lee, Dugosh, & Benasutti, 2006). Although in the case of our study, the SACPA legislation did not permit positive urines or similar program violations to be sanctioned with short-term incarceration (as is typical in drug courts), the judge did respond to positive tests or other treatment lapses by requiring participants to perform community service, attend additional self-help meetings, or return to an earlier phase of treatment. Observational data and previous research indicate that the judge is a key element in the drug court model and has a strong effect on treatment outcomes, and in SACPA the judge also plays an important, although less prominent, role in the monitoring of offender behavior. It may be that the influence of the judge within the courtroom on the attitudes and behavior of SACPA participants had a stronger impact on drug use and other outcomes than did the relatively low-value vouchers awarded as part of the treatment protocol used in this study. Marlowe et al. (2005; 2006) had a similar finding in their drug court study. It was only when they analyzed results by risk level were they able to uncover a CM effect.
A limitation of the study is that data on court proceedings were not collected. Although we would expect that as a result of random assignment, variations in rewards and sanctions would be randomly distributed across the four research conditions, it is possible that rewards and sanctions delivered by the court varied significantly across the four research conditions and influenced the findings. Were we to redesign the study, we would collect data on court proceedings and other criminal justice system rewards and sanctions. Specifically, we would capture the judge's use of praise, verbal censure, rewards, sanctions, and formal court orders (i.e., warrants). Because all SACPA participants (often along with family members) are together observing court proceedings and participating (through applause) when the judge uses these tools, we would also try to capture the effect of seeing others rewarded or sanctioned.
Another study limitation is the schedule of the reinforcements used in the intervention protocol. Lussier et al. (2006) found that studies with delayed reinforcement schedules and lower levels of daily possible earnings had smaller effect sizes than those with immediate reinforcement and higher earnings levels (see also Higgins, et al, 2006). In this study, participants receiving reinforcement for drug testing had to wait for the next session (2-4 days) to receive a voucher, possibly weakening the salience of the voucher and reducing its reinforcement of behavior. An additional study limitation is the use of a low-value, flat reinforcement schedule in which the voucher provided for each desired behavior (abstinence or prosocial activity) had the same value ($10). Compared with such a flat reinforcement schedule, research has demonstrated that schedules that include an escalation in reinforcer magnitude for consecutive instances of abstinence, when combined with a reset contingency for use, promotes more in-treatment abstinence (Roll, Higgins, & Badger, 1996; Roll & Shoptaw, 2006). A more immediate receipt of vouchers and a more powerful reinforcement schedule may have produced larger effects, even in the face of the apparent effects of the punishment contingencies imposed by the judge.
Another limitation was that the present study employed a twice-weekly random urine sample collection procedure rather than a more frequent (3 times per week) procedure such as that found effective by Higgins et al. (2002). Because of the criminal justice context in which it was embedded, this study targeted abstinence from all drugs plus alcohol rather than a single drug. While appropriate to the context, this may have unintentionally decreased the effect of the reinforcement procedure used in this study (Lussier, et al., 2006).
Our sample size may have limited our ability to detect a treatment effect. The number of participants available for analysis in the study (19-24 across the four conditions) is not untypical for studies of contingency management (Lussier, et al., 2006; Prendergast, et al., 2006). With a larger sample, we might have been able to detect significant differences between groups on at least some of the outcomes variables. Additionally, the characteristics of the participant pool for this study, primarily male white and Latino methamphetamine users, may limit generalizability.
In conclusion, the use of vouchers (using a flat reinforcement schedule) to reinforce negative urine tests and performance of prosocial behaviors within a diversion treatment program (California's SACPA program) did not have a statistically significant impact on treatment retention or drug use, even though contingency management has been found to be effective in non-criminal justice treatment settings. It is likely that punishment and contingent reinforcement (positive and negative) operating within the context of the SACPA drug treatment court created an effect that overrode the potentially reinforcing effect of vouchers. Future research is needed on the use of the contingency management within diversion treatment programs where the positive reinforcement is combined with judicial monitoring and punishment.
Figure 4. Weekly Percentage of Participants Testing Negative over 26 Weeks.
Acknowledgments
The work presented here was supported by NIDA Grants R01DA13114 and R01DA13114S. The authors wish to express their appreciation to Commissioner Ronald Gilbert, Rancho Cucamonga Superior Court; Deborah Service, Matrix Institute Treatment Program; and our project staff: David Bennett, Jaime Buhl, Jennifer Dacey, Yanscy Flores, Cora Garcia, Jordana Hemberg, Carolyn Potter, Sharlyn Prakash, Kimberly Richardson, Keeli Sorenson, and Ronald Zuniga for helping to make this project possible. We are also grateful to M. Douglas Anglin, Mary Lynn Brecht, and Richard Rawson for their helpful comments on earlier versions of this manuscript.
Biographies
Biographical Sketch
Elizabeth A. Hall is a researcher in UCLA Integrated Substance Abuse Programs' Criminal Justice Research Group. She has managed multi-site projects investigating drug abuse treatment, including as UCLA Pacific Coast Research Center Project Director for Criminal Justice Drug Abuse Treatment Studies (NIDA), and as co-investigator for Gender-Responsive Treatment Services for Women Offenders (NIDA) and Evaluation of Cost Avoidance and Child Welfare Outcomes of Dependency Drug Court Participants (California Department of Social Services).
Michael L. Prendergast is Director of Criminal Justice Research Group at the UCLA Integrated Substance Abuse Programs. He has directed various projects to study drug treatment strategies in the criminal justice system, including treatment for women offenders. He has been Principal Investigator of several NIDA-funded studies and of evaluations of treatment programs in correctional settings throughout California.
John M. Roll is Associate Dean for Research, Intercollegiate College of Nursing, at Washington State University. He is also Director of the Program of Excellence in the Addictions at Washington State University and has authored numerous publications on contingency management.
Umme Warda is a Senior Statistician at the UCLA Integrated Substance Abuse Programs and has contributed to numerous articles on substance abuse, ethnicity, gender, and health.
Footnotes
The CM methods of this study were identical to those in a study of vouchers with a sample of drug court participants at the same treatment program (Prendergast, et al., 2008). However, participants in this study had a less severe criminal history, experienced less intense judicial supervision, judicial sanctions did not include jail time, and treatment was of a shorter duration.
Contributor Information
Elizabeth A. Hall, Integrated Substance Abuse Programs, Semel Institute for Neuroscience and Human Behavior, University of California, Los Angeles
Michael L. Prendergast, Integrated Substance Abuse Programs, Semel Institute for Neuroscience and Human Behavior, University of California, Los Angeles
John M. Roll, Intercollegiate College of Nursing, Program of Excellence in the Addictions, Washington State University, Spokane
Umme Warda, Integrated Substance Abuse Programs, Semel Institute for Neuroscience and Human Behavior, University of California, Los Angeles.
References
- Bickel WK, Amass L, Higgins ST, Badger GJ, Esch RA. Effects of adding behavioral treatment to opioid detoxification with Buprenorphine. Journal of Consulting and Clinical Psychology. 1997;65(5):803–810. doi: 10.1037//0022-006x.65.5.803. [DOI] [PubMed] [Google Scholar]
- Bovasso GB, Alterman AI, Cacciola JS, Cook TG. Predictive validity of the Addiction Severity Index's composite scores in the assessment of 2-year outcomes in a methadone maintenance population. Psychology of Addictive Behaviors. 2001;15:171–176. [PubMed] [Google Scholar]
- Budney AJ, Higgins ST. NIDA Therapy Manuals 2, NIH Pub No 98-4309. Washington, DC: U.S. Government Printing Office; 1998. A community reinforcement plus vouchers approach: Treating cocaine addiction. [Google Scholar]
- Carroll KM, Easton CJ, Nich C, Hunkele KA, Neavins TM, Sinha R, Ford HL, Vitolo SA, Doebrick CA, Rounsaville BJ. The Use of Contingency Management and Motivational/Skills-Building Therapy to Treat Young Adults with Marijuana Dependence. Journal of Consulting & Clinical Psychology. 2006;74(5):955–966. doi: 10.1037/0022-006X.74.5.955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowley T. Contingency management and relapse prevention as stimulant abuse treatment interventions. In: Higgins ST, Silverman K, editors. Research on contingency management treatment of drug dependence: Clinical implications and future directions. Washington, DC: American Psychological Association; 1999. pp. 345–370. [Google Scholar]
- Derogatis LR, Melisaratos N. The Brief Symptom Inventory: An introductory report. Psychological Medicine. 1983;13:595–605. [PubMed] [Google Scholar]
- Diggle P, Heagerty P, Liang K, Zeger S. Analysis of longitudinal data. Oxford: Oxford University Press; 2002. [Google Scholar]
- Farabee D, Hser YI, Anglin MD, Huang D. Recidivism among an early cohort of California's Proposition 36 offenders. Criminology & Public Policy. 2004;3(4):563–584. [Google Scholar]
- Funderburk FR, Mackenzie A, DeHaven GP, Stefan R. Evaluation of the Multiple Offender Alcoholism Project: Quasiexperimental Evaluation Strategy with a focus on individual change and quality of life. Evaluation and Program Planning. 1993;16:181–191. [Google Scholar]
- Higgins ST, Silverman K, editors. Motivating behavior change among illicit-drug abusers: Research on contingency management interventions. Washington, D.C.: American Psychological Association; 1999. [Google Scholar]
- Higgins ST, Alessi SM, Dantona RL. Voucher-based incentives: A substance abuse treatment innovation. Addictive Behaviors. 2002;27:887–910. doi: 10.1016/s0306-4603(02)00297-6. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Budney AJ, Bickel WK, Foerg FE, Donham R, Badger GJ. Incentives improve outcome in outpatient behavioral treatment of cocaine dependence. Archives of General Psychiatry. 1994;51:568–76. doi: 10.1001/archpsyc.1994.03950070060011. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Budney AJ, Bickel WK, Hughes JR, Foerg F, Badger GJ. Achieving cocaine abstinence with a behavioral approach. American Journal of Psychiatry. 1993;150:763–769. doi: 10.1176/ajp.150.5.763. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Heil SH, Dantona R, Donham R, Matthews M, Badger GJ. Effects of varying the monetary value of voucher-based incentives on abstinence achieved during and following treatment among cocaine-dependent outpatients. Addiction. 2006;102:271–281. doi: 10.1111/j.1360-0443.2006.01664.x. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Roll JM, Wong CJ, Tidey JW, Dantona R. Clinic and laboratory studies on the use of incentives to decrease cocaine and other substance use. In: Higgins ST, Silverman K, editors. Motivating behavior change among illicit-drug abusers: Research on contingency management interventions. Washington, DC: American Psychological Association; 1999. pp. 35–56. [Google Scholar]
- Hser YI, Teruya C, Evans EA, Longshore D, Grella C, Farabee D. Treating drug-abusing offenders. Initial findings from a five-county study on the impact of California's Proposition 36 on the treatment system and patient outcomes. Evaluation Review. 2003;27(5):479–505. doi: 10.1177/0193841X03255774. [DOI] [PubMed] [Google Scholar]
- Huber A, Ling WL, Shoptaw S, Gulati V, Brethen P, Rawson R. Integrating treatments for methamphetamine abuse: A psychosocial perspective. Journal of Addictive Diseases. 1997;16(4):41–50. doi: 10.1080/10550889709511142. [DOI] [PubMed] [Google Scholar]
- Iguchi MY, Belding MA, Morral AR, Lamb RJ, Husband SD. Reinforcing operants other than abstinence in drug abuse treatment: An effective alternative for reducing drug use. Journal of Consulting and Clinical Psychology. 1997;65(3):421–428. doi: 10.1037//0022-006x.65.3.421. [DOI] [PubMed] [Google Scholar]
- Kidorf M, Stitzer ML. Contingent access to clinic privileges reduces drug abuse in methadone maintenance patients. In: Higgins ST, Silverman K, editors. Motivating behavior change among illicit-drug abusers: Research on contingency management interventions. Washington, DC: American Psychological Association; 1999. pp. 221–242. [Google Scholar]
- Klein D, Miller RE, Noble A, Speiglman R. Incorporating a public health approach in drug law: Lessons from local expansion of treatment capacity and access under California's Proposition 36. Milbank Quarterly. 2004;82(4):723–757. doi: 10.1111/j.0887-378X.2004.00329.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosten TR, Rounsaville BJ, Kleber HD. Concurrent validity of the Addiction Severity Index. Journal of Nervous and Mental Disease. 1983;171:606–610. doi: 10.1097/00005053-198310000-00003. [DOI] [PubMed] [Google Scholar]
- Leitenberg H, Rawson RA, Bath K. Reinforcement of competing behavior during extinction. Science. 1970;169:301–303. doi: 10.1126/science.169.3942.301. [DOI] [PubMed] [Google Scholar]
- Lussier JP, Heil SH, Mongeon JA, Badger GJ, Higgins ST. A meta-analysis of voucher-based reinforcement therapy for substance use disorders. Addiction. 2006;101:192–203. doi: 10.1111/j.1360-0443.2006.01311.x. [DOI] [PubMed] [Google Scholar]
- Longshore D, Urada D, Evans E, Hser YI, Prendergast M, Hawken A, et al. Evaluation of the Substance Abuse and Crime Prevention Act, 2003 Report. Los Angeles, CA: University of California, Los Angeles, Integrated Substance Abuse Programs; 2004. Report prepared for the Department of Alcohol and Drug Programs, California Health and Human Services Agency. [Google Scholar]
- Longshore D, Urada D, Evans E, Hser YI, Prendergast M, Hawken A. Evaluation of the Substance Abuse and Crime Prevention Act, 2004 Report. Los Angeles, CA: University of California, Los Angeles, Integrated Substance Abuse Programs; 2005. Report prepared for the Department of Alcohol and Drug Programs, California Health and Human Services Agency. [Google Scholar]
- Marlowe DB, Wong CJ. Contingency management in adult criminal drug courts. In: Higgins ST, Silverman K, Heil SH, editors. Contingency management in substance abuse treatment. New York: Guilford; 2008. pp. 334–354. [Google Scholar]
- Marlowe DB, Festinger DS, Lee PA. The judge is a key component of drug court. Drug Court Review. 2004;4(2):1–34. [Google Scholar]
- Marlowe DB, Festinger DS, Lee PA, Fox F, Alseander R, Mastro NK, et al. Contingency management in drug court. Paper presented at the 67th annual scientific meeting of the College on Problems of Drug Dependence; Orlando, FL. 2005. Jun, [Google Scholar]
- Marlowe DB, Festinger DS, Lee PA, Dugosh KL, Benasutti KM. Matching judicial supervision to clients' risk status in drug court. Crime & Delinquency. 2006;52(1):52–76. doi: 10.1177/0011128705281746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan AT, Alterman AI, Cacciola J, Metzger D, O'Brien CP. A new measure of substance abuse treatment: Initial studies of the Treatment Services Review. Journal of Nervous and Mental Disorders. 1992;180(2):101–110. doi: 10.1097/00005053-199202000-00007. [DOI] [PubMed] [Google Scholar]
- Morral AR, Iguchi MY, Belding MA. Reducing drug use by encouraging alternative behaviors. In: Higgins ST, Silverman K, editors. Motivating behavior change among illicit-drug abusers: Research on contingency management interventions. Washington, DC: American Psychological Association; 1999. pp. 203–220. [Google Scholar]
- National Institute on Drug Abuse. NIH Publication No 06-5316. Washington, DC: National Institutes of Health; 2006. Principles of drug abuse treatment for criminal justice populations: A research-based guide. [Google Scholar]
- Obert JL, McCann MJ, Marinelli-Casey P, Weiner A, Minsky S, Brethen P, et al. The Matrix Model of outpatient stimulant abuse treatment: History and description. Journal of Psychoactive Drugs. 2000;32(2):157–164. doi: 10.1080/02791072.2000.10400224. [DOI] [PubMed] [Google Scholar]
- Percival GL. The influence of local contextual characteristics on the implementation of a statewide voter initiative: The case of California's Substance Abuse and Crime Prevention Act (Proposition 36) Policy Studies Journal. 2004;32(4):589–610. [Google Scholar]
- Petry NM, Alessi SM, Carroll KM, Hanson T, MacKinnon S, Rounsaville B, et al. Contingency management treatments: Reinforcing abstinence versus adherence with goal-related activities. Journal of Consulting and Clinical Psychology. 2006;74(3):592–601. doi: 10.1037/0022-006X.74.3.592. [DOI] [PubMed] [Google Scholar]
- Petry NM, Peirce JM, Stitzer ML, Blaine J, Roll JM, Cohen A, et al. Effect of prize-based incentives on outcomes in stimulant abusers in outpatient psychosocial treatment programs: A national drug abuse treatment clinical trials network study. Archives of General Psychiatry. 2005;62(10):1148–1156. doi: 10.1001/archpsyc.62.10.1148. [DOI] [PubMed] [Google Scholar]
- Petry NM, Tedford J, Martin B. Reinforcing compliance with non-drug-related activities. Journal of Substance Abuse Treatment. 2001;20:33–44. doi: 10.1016/s0740-5472(00)00143-4. [DOI] [PubMed] [Google Scholar]
- Polakow RL, Doctor RM. A behavioral modification program for adult drug offenders. The Journal of Research in Crime and Delinquency. 1974;11(1):63–69. [Google Scholar]
- Prendergast ML, Hall EA, Roll J, Warda U. Use of vouchers to reinforce abstinence and positive behaviors among clients in a drug court treatment program. Journal of Substance Abuse Treatment. 2008;35(2):125–136. doi: 10.1016/j.jsat.2007.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prendergast M, Podus D, Finney J, Greenwell L, Roll J. Contingency management for treatment of substance use disorders: A meta-analysis. Addiction. 2006;101:1546–1560. doi: 10.1111/j.1360-0443.2006.01581.x. [DOI] [PubMed] [Google Scholar]
- Rawson RA, Leitenberg H. Reinforced alternative behavior during punishment and extinction with rats. Journal of Comparative and Physiological Psychology. 1973;85:593–600. [Google Scholar]
- Rawson RA, Marinelli-Casey P, Anglin MD, Dickow A, Frazier Y, Gallagher C, et al. A multi-site comparison of psychosocial approaches for the treatment of methamphetamine dependence. Addiction. 2004;99:708–717. doi: 10.1111/j.1360-0443.2004.00707.x. [DOI] [PubMed] [Google Scholar]
- Remington B, Remington M. Behavior modification in probation work: A review and evaluation. Criminal Justice and Behavior. 1987;14(2):156–174. [Google Scholar]
- Roll JM, Prendergast ML, Sorensen K, Prakash S, Chudzynski JE. A comparison of voucher exchanges between criminal justice involved and noninvolved participants enrolled in voucher-based contingency management drug abuse treatment programs. American Journal of Drug & Alcohol Abuse. 2005;31(3):393–401. doi: 10.1081/ada-200056774. [DOI] [PubMed] [Google Scholar]
- Roll JM, Shoptaw S. Contingency management: Schedule effects. Psychiatry Research. 2006;144(1):91–93. doi: 10.1016/j.psychres.2005.12.003. [DOI] [PubMed] [Google Scholar]
- Roll JM, Higgins ST, Badger GJ. An experimental comparison of three different schedules of reinforcement of drug abstinence using cigarette smoking as an exemplar. Journal of Applied Behavior Analysis. 1996;29:495–505. doi: 10.1901/jaba.1996.29-495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutherford A. The social control of behavior control: Behavior modification, individual rights, and research ethics in America, 1971-1979. Journal of the History of the Behavioral Sciences. 2006;42(3):203–220. doi: 10.1002/jhbs.20169. [DOI] [PubMed] [Google Scholar]
- Silverman K. Exploring the limits and utility of operant conditioning in the treatment of drug addiction. Behavior Analyst. 2004;27:209–230. doi: 10.1007/BF03393181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman K, Chutuape MA, Bigelow GE, Stitzer ML. Voucher-based reinforcement of attendance by unemployed methadone patients in a job skills training program. Drug and Alcohol Dependence. 1996;41(3):197–207. doi: 10.1016/0376-8716(96)01252-5. [DOI] [PubMed] [Google Scholar]
- Silverman K, Preston KL, Stitzer ML, Schuster CR. Efficacy and versatility of voucher-based reinforcement in drug abuse treatment. In: Higgins ST, Silverman K, editors. Motivating behavior change among illicit-drug abusers: Research on contingency management interventions. Washington, DC: American Psychological Association; 1999. pp. 163–181. [Google Scholar]
- Silverman K, Robles E, Mudric T, Bigelow GE, Stitzer ML. A randomized trial of long-term reinforcement of cocaine abstinence in methadone-maintained patients who inject drugs. Journal of Consulting and Clinical Psychology. 2004;72:839–854. doi: 10.1037/0022-006X.72.5.839. [DOI] [PubMed] [Google Scholar]
- Stitzer ML, Bigelow GE, Leibson I. Reducing drug use among methadone maintenance clients: Contingent reinforcement for morphine-free urines. Addictive Behaviors. 1980;4:245–252. doi: 10.1016/0306-4603(80)90007-6. [DOI] [PubMed] [Google Scholar]
- Stitzer ML, Bigelow GE, Leibson IA, Hawthorne JW. Contingent reinforcement for benzodiazepine-free urines: Evaluation of a drug abuse treatment intervention. Journal of Applied Behavioral Analysis. 1982;15:493–503. doi: 10.1901/jaba.1982.15-493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stokes ME, Davis CS, Koch GG. Categorical data analysis using the SAS system. 2nd. Cary, NC: SAS Institute, Inc; 2000. [Google Scholar]
- Urada D, Hawken A, Anglin MD, Conner B, Evans E, Longshore D. Evaluation of the Substance Abuse and Crime Prevention Act: Final Report (University of California, Los Angeles Integrated Substance Abuse Programs) 2007 Retrieved November 27, 2007 from: http://www.uclaisap.org/Prop36/documents/SACPAEvaluationReport.pdf.