Abstract
Essential amino acids (EAA) stimulate skeletal muscle mammalian target of rapamycin complex 1 (mTORC1) signaling and protein synthesis. It has recently been reported that an increase in amino acid (AA) transporter expression during anabolic conditions is rapamycin-sensitive. The purpose of this study was to determine whether an increase in EAA availability increases AA transporter expression in human skeletal muscle. Muscle biopsies were obtained from the vastus lateralis of seven young adult subjects (3 male, 4 female) before and 1–3 h after EAA ingestion (10 g). Blood and muscle samples were analyzed for leucine kinetics using stable isotopic techniques. Quantitative RT-PCR, and immunoblotting were used to determine the mRNA and protein expression, respectively, of AA transporters and members of the general AA control pathway [general control nonrepressed (GCN2), activating transcription factor (ATF4), and eukaryotic initiation factor (eIF2) α-subunit (Ser52)]. EAA ingestion increased blood leucine concentration, delivery of leucine to muscle, transport of leucine from blood into muscle, intracellular muscle leucine concentration, ribosomal protein S6 (Ser240/244) phosphorylation, and muscle protein synthesis. This was followed with increased L-type AA transporter (LAT1), CD98, sodium-coupled neutral AA transporter (SNAT2), and proton-coupled amino acid transporter (PAT1) mRNA expression at 1 h (P < 0.05) and modest increases in LAT1 protein expression (3 h post-EAA) and SNAT2 protein expression (2 and 3 h post-EAA, P < 0.05). Although there were no changes in GCN2 expression and eIF2α phosphorylation, ATF4 protein expression reached significance by 2 h post-EAA (P < 0.05). We conclude that an increase in EAA availability upregulates human skeletal muscle AA transporter expression, perhaps in an mTORC1-dependent manner, which may be an adaptive response necessary for improved AA intracellular delivery.
Keywords: nutrient signaling, mammalian target of rapamycin, L-type amino acid transporter type 1, sodium-coupled neutral amino acid transporter type 2, protein metabolism
essential amino acids (EAA) stimulate skeletal muscle protein synthesis (4, 7, 29, 42, 46). Within the last decade, great strides have been made to unravel the molecular mechanisms responsible for how EAA, and leucine in particular, enhance muscle protein synthesis. One focus of attention has been on the activation of the mammalian target of rapamycin (mTOR) complex 1 (mTORC1), an amino acid sensor (5) and central regulator of translation initiation and elongation (3). Although the mTORC1 pathway has been extensively studied in skeletal muscle of human and rodent models following EAA ingestion or infusion (4, 11, 14, 44), less information is available describing the relationship between amino acid transport mechanisms and mTORC1 signaling, especially in human skeletal muscle.
Amino acid transporters are ubiquitously expressed in the plasma membrane of many cell types, including human skeletal muscle (33). Recent classification of these proteins has termed them solute-linked carrier (SLC) family members (34). One group of amino acid transporters is the system L-type, which includes a heterodimeric complex made up of a permease [L-type amino acid transporter (LAT1/SLC7A5)] and a glycoprotein (CD98/SLC3A2). Another class of amino acid transporters is the system A-type, which includes the sodium-coupled neutral amino acid transporters (i.e., SNAT2/SLC38A2). Baird et al. (6) examined a novel coupling mechanism involving the cooperative activity of the protein complex LAT1-CD98 and SNAT2 and their role in activating mTORC1 by increasing the intracellular leucine concentration. SNAT2 transports glutamine into the cell in order for the LAT1-CD98 bitransport system to export glutamine and increase the influx of leucine (6). These two systems of transporters have been highlighted here not only because of evidence implying their role in muscle growth (28) but because expression of both LAT1/CD98 and SNAT2 is correlated with positive mTORC1 activation (28, 38), while inhibitors of SNAT2 and CD98 reduce mTORC1 activity and protein synthesis (8, 21).
A decrease in the intracellular amino acid pool reduces mTORC1 signaling (41), activates the general control nonrepressed (GCN2) pathway, and inhibits muscle protein synthesis via an increase in phosphorylation (Ser52) of eukaryotic initiation factor 2 α-subunit (eIF2α) (12, 19, 47, 48, 52). GCN2 activation also results in an increased expression of the activating transcription factor 4 (ATF4) (2). This protein has been found to upregulate amino acid transporters such as SNAT2 (18, 37) apparently to enable amino acid efflux during conditions associated with muscle catabolism (9, 39). On the other hand, ATF4 can also be upregulated in response to anabolic conditions such as insulin and amino acid sufficiency, and this effect is independent of GCN2 and is rapamycin-sensitive (1, 31). However, the cellular mechanisms responsible for the increase in ATF4 and amino acid transporters in response to these anabolic conditions are not known.
To date, no study has characterized amino acid transporter expression in human skeletal muscle in response to an increase in EAA availability. Therefore, the primary aim of this experiment was to determine the expression levels of L-type (LAT1/SLC7A5, y+LAT1/SLC7A7, LAT3/SLC43A1, and CD98/SLC3A2) and A-type (SNAT2/SLC38A2 and SNAT4/SLC38A4) amino acid transporters in relation to leucine kinetics in human skeletal muscle following the ingestion of EAA. A secondary aim was to determine the effect of an increase in EAA availability on the response of additional amino acid transporters associated with muscle growth and mTOR signaling [proton-coupled amino acid transporter (PAT1/SLC36A1 and PAT2/SLC36A2)] (16, 40), transporters that have not been linked to the mTORC1 signaling pathway [cationic amino acid transporter (CAT2/SLC7A2) and excitatory amino acid transporter (EAAT1/SLC1A3)], and members of the general amino acid control pathway [GCN2, eIF2α (Ser52), and ATF4]. We hypothesized that an increase in EAA availability would stimulate ATF4 and amino acid transporter expression.
MATERIALS AND METHODS
Subjects.
We studied 7 young subjects (3 male, 4 female; 29 ± 2 yr of age, 167 ± 6 cm height, 71 ± 6 kg body wt, 25 ± 1 kg/m2 body mass index). The subjects were not engaged in regular exercise training at the time of enrollment in the study, although they were physically active and healthy. Screening of subjects was performed with clinical history, physical examination, and laboratory tests, including complete blood count with differential, liver and kidney function tests, coagulation profile, fasting blood glucose and oral glucose tolerance test, hepatitis B and C screening, human immunodeficiency virus test, thyroid-stimulating hormone, lipid profile, urinalysis, and drug screening. All subjects gave informed written consent before participating in the study, which was approved by the Institutional Review Board of the University of Texas Medical Branch (which is in compliance with the Declaration of Helsinki).
Experimental design.
All subjects were admitted to the Clinical Research Center of the University of Texas Medical Branch on the day prior to the study, and a dual-energy X-ray absorptiometry scan (Hologic QDR 4500W, Bedford, MA) was performed to measure body composition and lean mass. The subjects were then fed a standard dinner and a snack at 2200. All subjects were studied following an overnight fast under basal conditions, refrained from exercise for 24 h prior to study participation, and were studied at the exact same time (i.e., between 0700 and 1600).
On the morning of the study, polyethylene catheters were inserted into a forearm vein for tracer infusion, into the contralateral hand vein, which was heated for arterialized blood sampling, and into the femoral artery and vein (retrograde placement) of the leg for blood sampling. The femoral lines were placed in the same leg from which muscle biopsies were obtained. The arterial catheter was also used for the infusion of indocyanine green (ICG; Akorn, Buffalo Grove, IL) to determine blood flow.
After a background blood sample was drawn, a primed continuous infusion of l-[1-13C]leucine (Isotec, Sigma-Aldrich, St. Louis, MO) was started and maintained at a constant rate until the end of the experiment. The priming dose for the labeled leucine was 4.8 μmol/kg, and the infusion rate was 0.08 μmol·kg−1·min−1 set at a constant pump rate of ∼6.5 ml/h.
At 2 h after initiation of the tracer infusion, the first muscle biopsy was obtained from the lateral portion of the vastus lateralis of the leg. The biopsy was performed using a 5-mm Bergström biopsy needle, under sterile procedure and local anesthesia (1% lidocaine). Immediately after the first biopsy, a continuous infusion of ICG was started in the femoral artery (0.5 mg/min) and maintained for 50 min. At 10 min after ICG infusion was started, four blood samples were drawn, at 10-min intervals, from the femoral vein and the arterialized hand vein for measurement of ICG concentration. In addition to the blood obtained for ICG measurement, blood samples were also taken from the femoral artery and vein and from the arterialized hand vein for measurement of amino acid enrichments. At the end of the baseline period, a second biopsy was obtained.
Immediately after the second baseline biopsy, subjects ingested a solution (500 ml) that contained 10 g of EAA mixed in a noncaloric, noncaffeinated carbonated beverage. The composition of the EAA mixture was as follows: 8% l-histidine, 8% l-isoleucine, 35% l-leucine, 12% l-lysine, 3% l-methionine, 14% l-phenylalanine, 10% l-threonine, and 10% l-valine (Sigma-Aldrich). Muscle biopsies were then sampled at 1, 2, and 3 h following the ingestion of the amino acid mixture. The two baseline and 1-h muscle biopsies were sampled from the same incision, while the 2- and 3-h muscle biopsies were sampled from a separate incision on the same leg 7 cm proximal to the previous incision site. To minimize changes in muscle due to the previous biopsy sampling, muscle biopsies were angled in such a way that ∼5 cm separated each sampling location (45). The tissue was immediately blotted and frozen in liquid nitrogen and stored at −80°C until analysis. Blood sampling and ICG infusion for amino acid concentrations and blood flow measurements, respectively, took place at baseline, after the ingestion of the amino acid mixture, and subsequently between the 1- to 2-h and 2- to 3-h postingestion time periods.
Fasting control group.
To determine if changes in amino acid transporter gene expression were due to biopsy trauma interference and/or circadian variation, we performed a small pilot experiment on four subjects (3 male, 1 female; 31 ± 2 yr of age, 87 ± 6 kg body wt, 1.77 ± 0.05 cm height) in the fasted state. Muscle samples were taken in the basal state and 2, 3, 4, and 5 h following the first biopsy and were sampled at essentially the same time at which biopsies were obtained from the EAA group. Biopsies were taken from the vastus lateralis in a manner identical to that used to obtain samples from the EAA group, such that biopsies 1–3 were sampled from a single incision and biopsies 4 and 5 were obtained from a separate single incision.
Determination of blood flow, insulin, amino acid concentrations, and muscle protein synthesis.
Serum ICG concentration for the determination of leg blood flow was measured spectrophotometrically (Beckman Coulter, Fullerton, CA) at a wavelength of 805 nm (24). Insulin concentrations were measured via a commercially available radioimmunoassay kit (Diagnostic Products, Los Angeles, CA). Concentrations and enrichments of blood leucine were determined on its tert-butyldimethylsilyl derivatives using l-leucine 5-5-5-d3 as an internal standard and gas chromatography/mass spectrometry (GCMS 6890 Plus GC, 5973N MSD/DS, and 7683 autosampler, Agilent Technologies, Palo Alto, CA) as previously described (50). The rate of incorporation of leucine into muscle protein was calculated as described by Borsheim et al. (10).
RNA extraction.
Total RNA was isolated by homogenizing 30–40 mg tissue with a homogenizing dispenser (T10 Basic Ultra Turrax, IKA, Wilmington, NC) in a solution containing 1.0 ml of TRI Reagent. The RNA was separated into an aqueous phase using 0.2 ml of chloroform and precipitated from the aqueous phase using 0.50 ml of isopropanol. Extracted RNA was washed with 1 ml of 75% ethanol, dried, and then suspended in a known amount (1.5 μl/mg tissue) of nuclease-free water. RNA concentration and integrity were assessed using the Agilent 2100 BioAnalyzer (Agilent Technologies). The average RNA integrity number was 8.7 ± 0.1 (on a scale of 1–10, where 10 is the highest score) and a 1.30 ± 0.02 28S-to-18S ratio. RNA was treated with DNase using a commercially available kit (DNA-free, Ambion, Austin, TX).
cDNA synthesis.
One microgram of total RNA was reverse transcribed into cDNA according to the manufacturer's directions (iScript, Bio-Rad, Hercules, CA). Briefly, a 20-μl reaction mixture consisting of 1 μg of total RNA, 4 μl of 5× iScript reaction mix, 1 μl of iScript reverse transcriptase, and a known amount of nuclease-free water was placed into the thermocycler (IQ5 Real-Time PCR cycler, Bio-Rad) with the following temperature/time protocol: 25°C for 5 min, 42°C for 30 min, and 85°C for 5 min. All isolated RNA and cDNA samples were stored at −80°C until further analysis.
PCR primers.
Primer pairs were customized using Beacon Designer 5.0 software (Premier Biosoft International, Palo Alto, CA) in which they were designed to avoid homology (BLAST analysis) and secondary structures. Primers, which were purchased from Invitrogen (Carlsbad, CA) or Sigma-Aldrich, were considered optimal if they produced 1) primer efficiencies between ∼90% and 100% and 2) a single DNA product of predicted size as identified with a melt analysis and DNA agarose gel. Primer sequences and accession numbers are provided in Table 1.
Table 1.
Primer sequences used for real-time quantitative RT-PCR
| Protein/Gene | Accession No. | Primer Sequence (5′ to 3′) | Position | Product Size, bp |
|---|---|---|---|---|
| LAT1/SLC7A5 | NM_003486 | 102 | ||
| Sense | GTGC C GTC CC TC GTGTTC | 1192 | ||
| Antisense | GC AGA GCC AG TTGAAGA AGC | 1274 | ||
| y+LAT1/SLC7A7 | NM_003982 | 189 | ||
| Sense | CA TCATC AGA GTGCC AG AAC | 1963 | ||
| Antisense | G CTTT CC AC ATC AGG ATTCC | 2132 | ||
| LAT3/SLC43A1 | NM_003627 | 85 | ||
| Sense | GC CT GCC TTAT CTTT CTGA AC | 872 | ||
| Antisense | TC TTC TTC GTGTAA TTGACTTCC | 934 | ||
| CD98/SLC3A2 | NM_001012661 | 100 | ||
| Sense | AGCATCCGTGTCATTCTG | 1218 | ||
| Antisense | G AGCATCCT TCA CCTTGG | 1300 | ||
| SNAT2/SLC38A2 | NM_018976 | 198 | ||
| Sense | AA GACCGCAGCCGTAGA AG | 1390 | ||
| Antisense | CAGCCA TTAA CACAGCCA GAC | 1567 | ||
| SNAT4/SLC38A4 | NM_018018 | 114 | ||
| Sense | A GGTGGTGGTGTTGA TTGGCTT G | 133 | ||
| Antisense | TTTGGA ATGGCAGA CCCGT GTAAC | 223 | ||
| PAT1/SLC36A1 | NM_078483 | 144 | ||
| Sense | CACCA ATA ACTGCCA CA AC | 745 | ||
| Antisense | GCCAA CA GGGAGA AGATG | 871 | ||
| PAT2/SLC36A2 | NM_181776 | 97 | ||
| Sense | GGTGT GGTTCT GCCTCTGG | 936 | ||
| Antisense | CA ATGTA TAGGGA AGTGACGATGG | 1009 | ||
| CAT2/SLC7A2 | NM_003046 | 132 | ||
| Sense | GA CA TTCCA CA ACTTCCA G | 4067 | ||
| Antisense | ATGCCTACAGTCCCTA CC | 4181 | ||
| EAAT1/SLC1A3 | NM_004172 | 88 | ||
| Sense | ACAGCAGGG GCAT TAGTTTC | 3611 | ||
| Antisense | CAGCGTCTTTGACTGGAT ATTC | 3677 | ||
| GCN2 | NM_001013703 | 103 | ||
| Sense | GG GAAGA AA GGA GATGTTTGG | 1476 | ||
| Antisense | CTGG TAAGT CA CTA GGGATGG | 1558 | ||
| ATF4 | NM_001675 | 130 | ||
| Sense | TCCT CCACTCCA GATCATT CC | 1393 | ||
| Antisense | GGGTGTCTTCCTCCTTTATGC | 1502 |
LAT, L-type amino acid transporter; SNAT, sodium-coupled neutral amino acid transporter; PAT, proton-coupled amino acid transporter; CAT, cationic amino acid transporter; EAAT, excitatory amino acid transporter; GCN, general control nonrepressed; ATF, activating transcription factor.
Semiquantitative real-time PCR.
Relative mRNA expression was determined by real-time RT-PCR using the iQ5 Multicolor Real-Time PCR cycler (Bio-Rad). cDNA was analyzed using SYBR Green fluorescence (iQ SYBR Green Supermix, Bio-Rad). Each reaction contained SYBR Green, a mixture of forward and reverse primers, cDNA template, and a known amount of sterile water. The total volume of the reaction tube was 25 μl. All samples were run in duplicate. An initial cycle for 5 min at 95°C was used to denature the cDNA. This was followed with 40 PCR cycles consisting of denaturation at 95°C for 20 s and primer annealing and extension at 55°C for 30 s. After all PCR runs, a melt analysis was performed. The geometric means of GAPDH and β2-microglobulin were used to normalize the genes of interest as recommended by Vandesompele et al. (43). Relative fold changes were determined from the cycle threshold (CT) values using the method as described by Livak and Schmittgen (30).
Immunoblot analysis.
Immunoblot analysis is described elsewhere (13). Briefly, equal amounts of total protein were loaded into each lane, and the samples were separated by electrophoresis (150 V for 60 min) on a 7.5% or 15% polyacrylamide gel as determined by the size of the target protein (Criterion, Bio-Rad). The separated proteins were transferred to a polyvinylidene difluoride membrane (Bio-Rad) at 50 V for 60 min and then incubated overnight in the primary antibody of interest and then for 1 h in secondary antibody at room temperature (see antibody concentrations below). After application of chemiluminescent solution (ECL plus, Amersham BioSciences, Piscataway, NJ) to each blot, optical density was measured (ChemiDoc, Bio-Rad) and densitometric analysis was performed using Quantity One 4.5.2 software (Bio-Rad). Immunoblot data were normalized to an internal control (loaded on every gel) for comparison across blots and then normalized to baseline values (expressed as fold change from basal).
Antibodies.
The polyclonal antibodies and dilutions were as follows: LAT1/SLC7A5 (1:1,000 dilution; Abcam, Cambridge, MA), CD98/SLC3A2 (1:250 dilution; Santa Cruz Biotechnology, Santa Cruz, CA), SNAT2/SLC38A2 (1:500 dilution; Santa Cruz Biotechnology), ribosomal protein S6 (rpS6, Ser240/244, 1:500 dilution; Cell Signaling, Beverley, MA), GCN2 (1:500 dilution; Santa Cruz Biotechnology), ATF4 (1:500 dilution; Santa Cruz Biotechnology), and eIF2α (Ser52, 1:1,000 dilution; Invitrogen). Anti-rabbit IgG horseradish peroxidase-conjugated secondary antibody was purchased from Amersham Bioscience (1:2,000 dilution).
Statistical methods.
To determine differences across time in our dependent variables of interest, data were statistically analyzed using a two-way repeated-measures ANOVA. When a main time effect existed, Bonferroni's post hoc tests were conducted to assess interaction effects at specific time points. Significance was set at P < 0.05. Values are means ± SE. All analyses were performed with SigmaStat software (version 3.5).
RESULTS
Leucine kinetics, insulin, and muscle protein synthesis.
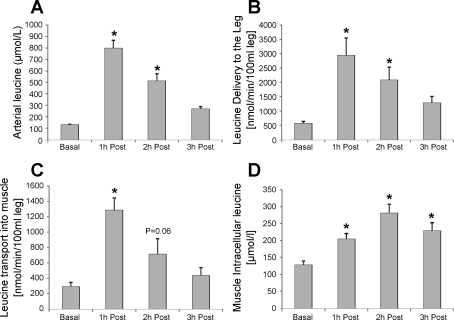
Leucine arterial concentration (Fig. 1A) and leucine delivery to the leg (Fig. 1B) were higher at 1 and 2 h post-EAA ingestion (P < 0.05), while leucine transport into the muscle (Fig. 1C) was significantly elevated at 1 h (P < 0.05) and nearly elevated at 2 h (P = 0.06) post-EAA. Additionally, muscle intracellular leucine concentrations were significantly increased at all time points (1–3 h) post-EAA (P < 0.05). Plasma insulin concentrations increased by 2.8-fold at 30 min and remained elevated by 1.7-fold at 60 min post-EAA (P < 0.05). Insulin concentrations returned to baseline values at 2 h post-EAA (P > 0.05). Muscle protein synthesis increased 2.4-fold from baseline (0.28 ± 0.04), to 0.67 ± 0.13 μmol·min−1·100 ml leg−1, during the 1st h post-EAA (P < 0.05) and returned to baseline levels by 2 h post-EAA (data not shown).
Fig. 1.
Leucine kinetics indicating arterial concentration (A), delivery (B), and transport (C) into the muscle and intracellular concentrations (D) in the basal state (Basal) and 1, 2, and 3 h following essential amino acid (EAA) ingestion. Each time point represents hourly averages as described in materials and methods. *Significantly different from Basal (n = 7, P < 0.05).
Amino acid transporter expression.
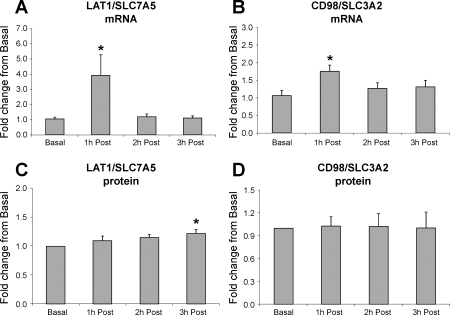
To determine whether selected amino acid transporters were upregulated following EAA ingestion, we measured the expression of the system L-type amino acid transporters, a primary transport mechanism of large neutral solutes such as leucine. We show that LAT1 mRNA expression was significantly elevated at 1 h following EAA ingestion (Fig. 2A; P < 0.05), while LAT1 protein was slightly (25%), but significantly, increased by 3 h post-EAA (Fig. 2C; P < 0.05). The mRNA associated with the heavy subunit of the L-type transporter, CD98, was also significantly elevated at 1 h post-EAA (Fig. 2B; P < 0.05); however, CD98 protein expression was unchanged from basal levels (Fig. 2D). There were no significant differences across time for y+LAT1 or LAT3 mRNA expression (Table 2).
Fig. 2.
L-type amino acid transporter [LAT1/SLC7A5 mRNA (A) and protein (C) and CD98/SLC3A2 mRNA (B) and protein (D)] expression in young, healthy subjects in the basal state and 1, 2, and 3 h following EAA ingestion. *Significantly different from Basal (n = 7, P < 0.05).
Table 2.
Expression level of genes and proteins associated with amino acid transporters, mTORC1 activity, and amino acid control after EAA ingestion
| 1 h Post-EAA | 2 h Post-EAA | 3 h Post-EAA | |
|---|---|---|---|
| Marker of mTORC1 activity | |||
| rpS6 protein (Ser240/244) | 5.62 ± 2.14* | 1.98 ± 0.76 | 2.66 ± 0.97 |
| Additional amino acid transporters | |||
| y+LAT1/SLC7A7 mRNA | 1.05 ± 0.26 | 0.94 ± 0.19 | 0.98 ± 0.16 |
| LAT3/SLC43A1 mRNA | 1.13 ± 0.21 | 1.32 ± 0.19 | 1.04 ± 0.39 |
| SNAT4/SLC38A4 mRNA | 1.08 ± 0.32 | 1.58 ± 0.23 | 1.52 ± 0.34 |
| CAT2/SLC7A2 mRNA | 1.22 ± 0.10 | 1.13 ± 0.11 | 1.07 ± 0.31 |
| EAAT1/SLC1A3 mRNA | 1.56 ± 0.25 | 1.43 ± 0.23 | 1.32 ± 0.25 |
| General amino acid control | |||
| GCN2 mRNA | 0.81 ± 0.07 | 1.00 ± 0.07 | 1.05 ± 0.14 |
| GCN2 protein | 1.20 ± 0.18 | 1.23 ± 0.28 | 1.20 ± 0.34 |
| ATF4 mRNA | 1.10 ± 0.05 | 0.86 ± 0.10 | 0.93 ± 0.10 |
| ATF4 protein | 1.14 ± 0.06 | 1.27 ± 00.12* | 1.10 ± 0.12 |
| eIF2α protein (Ser52) | 1.10 ± 0.12 | 1.04 ± 0.16 | 1.15 ± 0.23 |
Values are means ± SE, expressed as fold change from basal. mTORC1, mammalian target of rapamycin complex 1; rpS6, ribosomal protein S6; eIF2α, eukaryotic initiation factor type 2 α-subunit.
Significantly different from basal (P < 0.05).
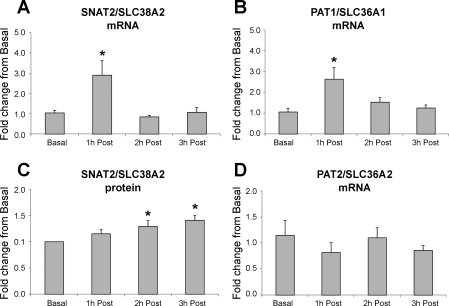
We next evaluated system A-type transporters that are proposed to work in conjunction with system L-type amino acid transporters (6). We found that SNAT2 mRNA expression was significantly elevated at 1 h following EAA ingestion (Fig. 3A; P < 0.05), while SNAT2 protein expression was elevated by ∼25% at 2 and 3 h post-EAA (Fig. 3C; P < 0.05). There was no significant change in SNAT4 mRNA expression (Table 2).
Fig. 3.
A-type and amino acid transporter [SNAT2/SLC38A2 mRNA (A) and protein (C), PAT1/SLC36A1 mRNA (B), and PAT2/SLC36A2 mRNA (D)] expression in young, healthy subjects in the basal state and 1, 2, and 3 h following EAA ingestion. *Significantly different from Basal (n = 7, P < 0.05).
Furthermore, we determined the expression pattern of the PAT transporters, newly reported transporters with a role in muscle growth and associated mTOR signaling (16, 40), following EAA ingestion. PAT1 mRNA expression was increased at 1 h following EAA ingestion (Fig. 3B; P < 0.05), while no differences were found across time for PAT2 (Fig. 3D; P > 0.05). Additionally, we evaluated the expression of amino acid transporters not reported to have an association with mTORC1 signaling with the purpose of determining if the L- and A-type transporters are uniquely regulated following an acute anabolic stimulus. We report that CAT2 and EAAT1 mRNA expression was unchanged following EAA ingestion (Table 2).
Marker of mTORC1 activity.
To determine if EAA ingestion was associated with an increase in the activity of the mTORC1 pathway, we measured the phosphorylation of rpS6 at Ser240/244. Phosphorylation of rpS6 was significantly elevated at 1 h post-EAA (P < 0.05) but returned to baseline thereafter (Table 2).
Potential regulators of amino acid transporters.
Finally, we examined key genes and proteins associated with general amino acid control (Table 2). There were no differences in the mRNA or protein expression for GCN2 post-EAA. ATF4 mRNA expression was unchanged, but ATF4 protein expression was increased by ∼25%, at 2 h post-EAA (P < 0.05). Lastly, the phosphorylation status of eIF2α (Ser52) was not different across time following EAA ingestion.
Control group.
In our fasting control group, we measured the same transporters that were increased from baseline (LAT1, CD98, SNAT2, and PAT1) in the EAA group to determine whether the increase in amino acid transporter expression could have been due to a biopsy effect and/or circadian changes. Overall, there were no changes across time for any of the genes measured within the control group (Table 3). These data strongly suggest that the robust changes at 1 h post-EAA in the experimental group were largely due to the increase in EAA availability, rather than biopsy trauma or circadian rhythms.
Table 3.
Expression levels of select amino acid transporter mRNAs in control (no EAA) group
| Basal | 3 h Post | 4 h Post | 5 h Post | |
|---|---|---|---|---|
| LAT1/SLC7A5 | 1.06 ± 0.21 | 1.69 ± 0.58 | 1.21 ± 0.35 | 1.49 ± 0.31 |
| CD98/SLC3A2 | 1.06 ± 0.22 | 1.19 ± 0.15 | 0.80 ± 0.06 | 1.01 ± 0.15 |
| SNAT2/SLC38A2 | 1.04 ± 0.17 | 1.26 ± 0.13 | 1.78 ± 0.63 | 1.39 ± 0.34 |
| PAT1/SLC36A1 | 1.01 ± 0.06 | 1.13 ± 0.08 | 1.06 ± 0.15 | 1.13 ± 0.08 |
Values are means ± SE, expressed as fold change from basal. Data were normalized to GAPDH and β2-microglobulin using the 2(−ΔΔCT) method. Time points represent biopsies sampled (in hours) following the basal biopsy.
DISCUSSION
The novel finding of this study was that EAA ingestion in humans resulted in a robust and transient increase in the mRNA expression of LAT1 and CD98 (L-type amino acid transporters), an increase in SNAT2 (an A-type amino acid transporter), and an increase in PAT1. These increases were followed by a modest increase in LAT1 and SNAT2 transporter protein expression. These data likely occurred downstream of mTORC1 signaling, suggesting a cellular adaptation mechanism to improve amino acid transport and, hence, mTORC1 signaling, during prolonged amino acid sufficiency or in response to a future protein anabolic stimulus. Alterations in amino acid transporter expression and function may be essential for regulating rates of in vivo muscle protein synthesis following anabolic stimuli (e.g., feeding and/or resistance exercise) or under circumstances in which muscle protein synthesis is attenuated (e.g., bed rest, sepsis, and burns).
In a review by Wolfe (49), it is highly evident that the increases in amino acid availability are strongly correlated with the change in muscle protein synthesis, especially when leucine concentrations are monitored. This would suggest that the accumulation of amino acids is a central event that leads to changes in protein turnover. Depending on the method of amino acid delivery (e.g., infusion or ingestion), we previously showed a rapid increase of amino acids in the plasma (ingestion: ∼15 min) immediately followed by activation of the mTORC1 pathway and muscle protein synthesis (14). Indeed, as we show in Fig. 1, arterial leucine concentrations and leucine delivery and transport into the muscle increase 1–2 h post-EAA ingestion, while intracellular leucine concentrations remain elevated for at least an additional hour. The increase in EAA availability caused a transient increase in mTORC1 signaling (e.g., rpS6 phosphorylation; Table 2) and muscle protein synthesis during the 1st h following nutrient ingestion. The accumulation of intracellular leucine during the 2nd and 3rd h after ingestion was likely due to continued transport and a gradual decrease in the cellular utilization of leucine as a substrate for protein synthesis. However, little is known of the relationship between mTORC1 signaling and amino acid transport mechanisms (5).
Hundal and Taylor (20) report that nutrient activation of mTORC1 (in particular, leucine) occurs through a novel class of L- and A-type amino acid transporters. We report for the first time in human skeletal muscle that the expression of LAT1 (Fig. 2A), CD98 (Fig. 2B), and SNAT2 (Fig. 3A) mRNA was increased at 1 h and quickly returned to baseline following EAA ingestion (P < 0.05). As expected, changes in mRNA levels were followed with a slight (∼25%) accumulation of transporter protein (Figs. 2C and 3C). These data are in agreement with findings of McDowell et al. (32) that indicate that leucine availability increases SNAT2 transporter activity in L6 muscle cells. Additionally, we did not identify changes in expression of other members of these systems (e.g., y+LAT1, LAT3, and SNAT4; Table 2), highlighting the uniqueness of LAT1-CD98 and SNAT2 transporters among members of the same family following a protein anabolic stimulus.
Increases in transporter mRNA and protein expression following an acute bolus of EAA are likely events that follow mTORC1 signaling and muscle protein synthesis. We suggest that elevated amino acid transporter levels are an adaptive response to increase the sensitivity of amino acid influx during sustained amino acid availability and/or during exposure to a subsequent anabolic stimulus. Perhaps adaptations in amino acid transport are necessary to enhance mTORC1 signaling and muscle protein synthesis. It is also possible that the accumulation of transporter protein at 2 and 3 h post-EAA may have joined the pool of amino acid transporters that translocated to the plasma membrane for the maintenance of leucine transport noted at 2 h post-EAA (Fig. 1C). A proposed sequence of events may include an increase in EAA availability, resulting in an increase in amino acid transport and intracellular concentration that stimulates mTORC1 signaling and muscle protein synthesis. This is followed with an upregulation of mTORC1-related amino acid transporter mRNA and protein expression to adapt to an altered nutritional state.
Another novel finding was that PAT1, but not PAT2, mRNA expression increased 1 h post-EAA (Fig. 3, B and D). Much attention has been given to the L- and A-type amino acid transporters as central for delivering substrates to nutrient sensors upstream of mTORC1. However, a scan of the literature shows that PAT transporters are important for cell growth in Drosophila and also operate through an mTORC1-related mechanism (16, 40). Godberdhan and colleagues (17) proposed a model in which PAT transporters not only transport amino acids directly into the cytosol but may also act as a shuttle to transport amino acids, such as leucine, directly to mTORC1. Therefore, these findings highlight PAT1 as another transporter that may be linked to mTORC1 signaling in humans.
Paradoxically, SNAT2 amino acid transport is increased following amino acid deprivation (15, 27, 35, 36) and amino acid sufficiency (present study; 32), and both occur by an ATF4-mediated mechanism (18, 37). However, the means of ATF4 activation are different between the two cellular conditions. During amino acid deprivation (e.g., starvation), uncharged tRNAs accumulate and GCN2 is activated and phosphorylates eIF2α, resulting in a downregulation of translation initiation and protein synthesis (12, 19, 47, 48, 52). In this circumstance, GCN2 increases ATF4 expression, which serves as a transcription factor for upregulating amino acid transporter gene transcription (1, 31, 37). Elevating transporter expression during periods of amino acid deprivation may be a mechanism to increase amino acid transport out of the cell for survival (9, 39). When amino acids are in abundance, as can be seen from this study following the ingestion of 10 g of EAA, anabolic signals (i.e., leucine and/or insulin) increase the translocation of existing amino acid transporter proteins to the plasma membrane (22) and trigger a rapamycin-sensitive ATF4 activation of amino acid transporters (1, 31), all steps necessary to increase the intracellular pool of amino acids and stimulate muscle protein synthesis. In either case, upregulation of amino acid transporter expression provides a quick means to meet the energy demands of the cell. Whether amino acids are transported into or out of the plasma membrane is likely dependent on the activation of the mTORC1 or GCN2 amino acid-sensing pathways, respectively.
Our data indicate that the GCN2 does not play a role during an increase in EAA availability in humans (Table 2). This finding is consistent with a recent report showing that insulin and amino acid sufficiency promote an increase in ATF4 expression independent of the GCN2 pathway (31). In the present study, ingestion of 10 g of EAA caused a small and transient increase in insulin concentration during the 1st h that returned to baseline by 2 h after ingestion. Interestingly, ATF4 protein expression did not reach significance until 2 h post-EAA and was independent of any changes in ATF4 mRNA. In any event, these findings do not eliminate ATF4 as a regulator of amino acid transporter expression following EAA ingestion. It is possible that, during the 1st h after ingestion, the overall activity of ATF4 increased or ATF4 may have translocated to the nucleus, upregulating amino acid transporter expression. Indeed, ATF4 has been reported to undergo variations of posttranslational modification (i.e., phosphorylation, ubiquidation, and acetylation) (25, 26, 51). In addition, we cannot determine from our study whether the increase in amino acid transporter expression was solely due to changes in EAA availability, since an increase in EAA availability does induce an increase in circulating insulin. Therefore, it remains to be determined whether an increase in EAA can upregulate amino acid transporter expression independent of insulin and whether enhanced amino acid transporter expression can occur independent of ATF4, as new evidence suggests that other mechanisms can upregulate amino acid transporter expression. For example, in placental trophoblast cells, signal transducer and activator of transcription (STAT3), through an IL-6-mediated mechanism, can upregulate SNAT2 expression (23).
In summary, we found that the expression of several transporters (LAT1, CD98, SNAT2, and PAT1) associated with mTORC1 signaling was rapidly and transiently upregulated following EAA ingestion in humans. These changes likely occurred downstream of mTORC1 signaling (via ATF4) and may serve as a cellular adaptation to improve amino acid transport. We conclude that the expression of amino acid transporters is a unique regulatory mechanism associated with the muscle protein anabolic response following an increase in EAA availability and should be given attention in future muscle protein metabolism studies.
GRANTS
This study was supported by an American College of Sports Medicine Research Endowment Grant (M. J. Drummond), National Institute on Aging/National Institute of Arthritis and Musculoskeletal and Skin Diseases Grant AR-049877 (B. B. Rasmussen), and National Institute of Child Health and Human Development Predoctoral Training Grant T32 HD-07539 (C. S. Fry). Additional support was provided by National Institute on Aging Grant P30 AG-024832 and Grant 1UL1RR029876-01 from the National Center for Research Resources.
DISCLOSURES
No conflicts of interest are declared by the author(s).
ACKNOWLEDGMENTS
We thank the nurses and staff at the Clinical Research Center for assistance in screening and admitting the subjects and for assistance with the subjects during data collection.
REFERENCES
- 1.Adams CM. Role of the transcription factor ATF4 in the anabolic actions of insulin and the anti-anabolic actions of glucocorticoids. J Biol Chem 282: 16744–16753, 2007 [DOI] [PubMed] [Google Scholar]
- 2.Ameri K, Harris AL. Activating transcription factor 4. Int J Biochem Cell Biol 40: 14–21, 2008 [DOI] [PubMed] [Google Scholar]
- 3.Anthony JC, Anthony TG, Kimball SR, Jefferson LS. Signaling pathways involved in translational control of protein synthesis in skeletal muscle by leucine. J Nutr 131: 856S–860S, 2001 [DOI] [PubMed] [Google Scholar]
- 4.Anthony JC, Yoshizawa F, Anthony TG, Vary TC, Jefferson LS, Kimball SR. Leucine stimulates translation initiation in skeletal muscle of postabsorptive rats via a rapamycin-sensitive pathway. J Nutr 130: 2413–2419, 2000 [DOI] [PubMed] [Google Scholar]
- 5.Avruch J, Long X, Ortiz-Vega S, Rapley J, Papageorgiou A, Dai N. Amino acid regulation of TOR complex 1. Am J Physiol Endocrinol Metab 296: E592–E602, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baird FE, Bett KJ, MacLean C, Tee AR, Hundal HS, Taylor PM. Tertiary active transport of amino acids reconstituted by coexpression of system A and L transporters in Xenopus oocytes. Am J Physiol Endocrinol Metab 297: E822–E829, 2009 [DOI] [PubMed] [Google Scholar]
- 7.Bennet WM, Connacher AA, Scrimgeour CM, Smith K, Rennie MJ. Increase in anterior tibialis muscle protein synthesis in healthy man during mixed amino acid infusion: studies of incorporation of [1-13C]leucine. Clin Sci (Lond) 76: 447–454, 1989 [DOI] [PubMed] [Google Scholar]
- 8.Bevington A, Brown J, Butler H, Govindji S, M-Khalid K, Sheridan K, Walls J. Impaired system A amino acid transport mimics the catabolic effects of acid in L6 cells. Eur J Clin Invest 32: 590–602, 2002 [DOI] [PubMed] [Google Scholar]
- 9.Bode BP. Recent molecular advances in mammalian glutamine transport. J Nutr 131: 2475S–2487S, 2001 [DOI] [PubMed] [Google Scholar]
- 10.Borsheim E, Tipton KD, Wolf SE, Wolfe RR. Essential amino acids and muscle protein recovery from resistance exercise. Am J Physiol Endocrinol Metab 283: E648–E657, 2002 [DOI] [PubMed] [Google Scholar]
- 11.Cuthbertson D, Smith K, Babraj J, Leese G, Waddell T, Atherton P, Wackerhage H, Taylor PM, Rennie MJ. Anabolic signaling deficits underlie amino acid resistance of wasting, aging muscle. FASEB J 19: 422–424, 2005 [DOI] [PubMed] [Google Scholar]
- 12.de Haro C, Mendez R, Santoyo J. The eIF-2α kinases and the control of protein synthesis. FASEB J 10: 1378–1387, 1996 [DOI] [PubMed] [Google Scholar]
- 13.Dreyer HC, Fujita S, Cadenas JG, Chinkes DL, Volpi E, Rasmussen BB. Resistance exercise increases AMPK activity and reduces 4E-BP1 phosphorylation and protein synthesis in human skeletal muscle. J Physiol 576: 613–624, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fujita S, Dreyer HC, Drummond MJ, Glynn EL, Cadenas JG, Yoshizawa F, Volpi E, Rasmussen BB. Nutrient signalling in the regulation of human muscle protein synthesis. J Physiol 582: 813–823, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gazzola RF, Sala R, Bussolati O, Visigalli R, Dall'Asta V, Ganapathy V, Gazzola GC. The adaptive regulation of amino acid transport system A is associated to changes in ATA2 expression. FEBS Lett 490: 11–14, 2001 [DOI] [PubMed] [Google Scholar]
- 16.Goberdhan DC, Meredith D, Boyd CA, Wilson C. PAT-related amino acid transporters regulate growth via a novel mechanism that does not require bulk transport of amino acids. Development 132: 2365–2375, 2005 [DOI] [PubMed] [Google Scholar]
- 17.Goberdhan DC, Ogmundsdottir MH, Kazi S, Reynolds B, Visvalingam SM, Wilson C, Boyd CA. Amino acid sensing and mTOR regulation: inside or out? Biochem Soc Trans 37: 248–252, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harding HP, Zhang Y, Zeng H, Novoa I, Lu PD, Calfon M, Sadri N, Yun C, Popko B, Paules R, Stojdl DF, Bell JC, Hettmann T, Leiden JM, Ron D. An integrated stress response regulates amino acid metabolism and resistance to oxidative stress. Mol Cell 11: 619–633, 2003 [DOI] [PubMed] [Google Scholar]
- 19.Hinnebusch AG. Translational regulation of GCN4 and the general amino acid control of yeast. Annu Rev Microbiol 59: 407–450, 2005 [DOI] [PubMed] [Google Scholar]
- 20.Hundal HS, Taylor PM. Amino acid transceptors: gate keepers of nutrient exchange and regulators of nutrient signaling. Am J Physiol Endocrinol Metab 296: E603–E613, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hyde R, Hajduch E, Powell DJ, Taylor PM, Hundal HS. Ceramide down-regulates system A amino acid transport and protein synthesis in rat skeletal muscle cells. FASEB J 19: 461–463, 2005 [DOI] [PubMed] [Google Scholar]
- 22.Hyde R, Peyrollier K, Hundal HS. Insulin promotes the cell surface recruitment of the SAT2/ATA2 system A amino acid transporter from an endosomal compartment in skeletal muscle cells. J Biol Chem 277: 13628–13634, 2002 [DOI] [PubMed] [Google Scholar]
- 23.Jones HN, Jansson T, Powell T. IL-6 stimulates system A amino acid transporter activity in trophoblast cells through STAT3 and increased expression of SNAT2. Am J Physiol Cell Physiol 297: C1228–C1235, 2009 [DOI] [PubMed] [Google Scholar]
- 24.Jorfeldt L, Wahren J. Leg blood flow during exercise in man. Clin Sci 41: 459–473, 1971 [DOI] [PubMed] [Google Scholar]
- 25.Lassot I, Estrabaud E, Emiliani S, Benkirane M, Benarous R, Margottin-Goguet F. p300 modulates ATF4 stability and transcriptional activity independently of its acetyltransferase domain. J Biol Chem 280: 41537–41545, 2005 [DOI] [PubMed] [Google Scholar]
- 26.Lassot I, Segeral E, Berlioz-Torrent C, Durand H, Groussin L, Hai T, Benarous R, Margottin-Goguet F. ATF4 degradation relies on a phosphorylation-dependent interaction with the SCF(βTrCP) ubiquitin ligase. Mol Cell Biol 21: 2192–2202, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ling R, Bridges CC, Sugawara M, Fujita T, Leibach FH, Prasad PD, Ganapathy V. Involvement of transporter recruitment as well as gene expression in the substrate-induced adaptive regulation of amino acid transport system A. Biochim Biophys Acta 1512: 15–21, 2001 [DOI] [PubMed] [Google Scholar]
- 28.Liu XM, Reyna SV, Ensenat D, Peyton KJ, Wang H, Schafer AI, Durante W. Platelet-derived growth factor stimulates LAT1 gene expression in vascular smooth muscle: role in cell growth. FASEB J 18: 768–770, 2004 [DOI] [PubMed] [Google Scholar]
- 29.Liu Z, Jahn LA, Wei L, Long W, Barrett EJ. Amino acids stimulate translation initiation and protein synthesis through an Akt-independent pathway in human skeletal muscle. J Clin Endocrinol Metab 87: 5553–5558, 2002 [DOI] [PubMed] [Google Scholar]
- 30.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(−ΔΔCT) method. Methods 25: 402–408, 2001 [DOI] [PubMed] [Google Scholar]
- 31.Malmberg SE, Adams CM. Insulin signaling and the general amino acid control response. Two distinct pathways to amino acid synthesis and uptake. J Biol Chem 283: 19229–19234, 2008 [DOI] [PubMed] [Google Scholar]
- 32.McDowell HE, Christie GR, Stenhouse G, Hundal HS. Leucine activates system A amino acid transport in L6 rat skeletal muscle cells. Am J Physiol Cell Physiol 269: C1287–C1294, 1995 [DOI] [PubMed] [Google Scholar]
- 33.Nishimura M, Naito S. Tissue-specific mRNA expression profiles of human solute carrier transporter superfamilies. Drug Metab Pharmacokinet 23: 22–44, 2008 [DOI] [PubMed] [Google Scholar]
- 34.Palacin M, Estevez R, Bertran J, Zorzano A. Molecular biology of mammalian plasma membrane amino acid transporters. Physiol Rev 78: 969–1054, 1998 [DOI] [PubMed] [Google Scholar]
- 35.Palii SS, Chen H, Kilberg MS. Transcriptional control of the human sodium-coupled neutral amino acid transporter system A gene by amino acid availability is mediated by an intronic element. J Biol Chem 279: 3463–3471, 2004 [DOI] [PubMed] [Google Scholar]
- 36.Palii SS, Kays CE, Deval C, Bruhat A, Fafournoux P, Kilberg MS. Specificity of amino acid regulated gene expression: analysis of genes subjected to either complete or single amino acid deprivation. Amino Acids 37: 79–88, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Palii SS, Thiaville MM, Pan YX, Zhong C, Kilberg MS. Characterization of the amino acid response element within the human sodium-coupled neutral amino acid transporter 2 (SNAT2) system A transporter gene. Biochem J 395: 517–527, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Peyrollier K, Hajduch E, Blair AS, Hyde R, Hundal HS. l-Leucine availability regulates phosphatidylinositol 3-kinase, p70 S6 kinase and glycogen synthase kinase-3 activity in L6 muscle cells: evidence for the involvement of the mammalian target of rapamycin (mTOR) pathway in the l-leucine-induced up-regulation of system A amino acid transport. Biochem J 350: 361–368, 2000 [PMC free article] [PubMed] [Google Scholar]
- 39.Rennie MJ, Ahmed A, Khogali SE, Low SY, Hundal HS, Taylor PM. Glutamine metabolism and transport in skeletal muscle and heart and their clinical relevance. J Nutr 126: 1142S–1149S, 1996 [DOI] [PubMed] [Google Scholar]
- 40.Reynolds B, Laynes R, Ogmundsdottir MH, Boyd CA, Goberdhan DC. Amino acid transporters and nutrient-sensing mechanisms: new targets for treating insulin-linked disorders? Biochem Soc Trans 35: 1215–1217, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sancak Y, Peterson TR, Shaul YD, Lindquist RA, Thoreen CC, Bar-Peled L, Sabatini DM. The Rag GTPases bind raptor and mediate amino acid signaling to mTORC1. Science 320: 1496–1501, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Smith K, Barua JM, Watt PW, Scrimgeour CM, Rennie MJ. Flooding with l-[1-13C]leucine stimulates human muscle protein incorporation of continuously infused l-[1-13C]valine. Am J Physiol Endocrinol Metab 262: E372–E376, 1992 [DOI] [PubMed] [Google Scholar]
- 43.Vandesompele J, De Preter K, Pattyn F, Poppe B, Van Roy N, De Paepe A, Speleman F. Accurate normalization of real-time quantitative RT-PCR data by geometric averaging of multiple internal control genes. Genome Biol 3: 0034.0031–0034.0012, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vary TC, Jefferson LS, Kimball SR. Amino acid-induced stimulation of translation initiation in rat skeletal muscle. Am J Physiol Endocrinol Metab 277: E1077–E1086, 1999 [DOI] [PubMed] [Google Scholar]
- 45.Volpi E, Chinkes DL, Rasmussen BB. Sequential muscle biopsies during a 6-h tracer infusion do not affect human mixed muscle protein synthesis and muscle phenylalanine kinetics. Am J Physiol Endocrinol Metab 295: E959–E963, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Volpi E, Mittendorfer B, Rasmussen BB, Wolfe RR. The response of muscle protein anabolism to combined hyperaminoacidemia and glucose-induced hyperinsulinemia is impaired in the elderly. J Clin Endocrinol Metab 85: 4481–4490, 2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wek RC, Cavener DR. Translational control and the unfolded protein response. Antioxid Redox Signal 9: 2357–2371, 2007 [DOI] [PubMed] [Google Scholar]
- 48.Wek RC, Jiang HY, Anthony TG. Coping with stress: eIF2 kinases and translational control. Biochem Soc Trans 34: 7–11, 2006 [DOI] [PubMed] [Google Scholar]
- 49.Wolfe RR. Regulation of muscle protein by amino acids. J Nutr 132: 3219S–3224S, 2002 [DOI] [PubMed] [Google Scholar]
- 50.Wolfe RR, Chinkes DL. Isotope Tracers in Metabolic Research Principles and Practice of Kinetic Analysis Hoboken, NJ: Wiley-Liss, 2005 [Google Scholar]
- 51.Yang X, Karsenty G. ATF4, the osteoblast accumulation of which is determined post-translationally, can induce osteoblast-specific gene expression in non-osteoblastic cells. J Biol Chem 279: 47109–47114, 2004 [DOI] [PubMed] [Google Scholar]
- 52.Zhang P, McGrath BC, Reinert J, Olsen DS, Lei L, Gill S, Wek SA, Vattem KM, Wek RC, Kimball SR, Jefferson LS, Cavener DR. The GCN2 eIF2α kinase is required for adaptation to amino acid deprivation in mice. Mol Cell Biol 22: 6681–6688, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]