Abstract
This study analyzes data from a national survey to estimate the proportion of physicians who currently object to physician-assisted suicide (PAS), terminal sedation (TS), and withdrawal of artificial life support (WLS), and to examine associations between such objections and physician ethnicity, religious characteristics, and experience caring for dying patients. Overall, 69% of the US physicians object to PAS, 18% to TS, and 5% to WLS. Highly religious physicians are more likely than those with low religiosity to object to both PAS (84% vs 55%, P < .001) and TS (25% vs 12%, P < .001). Objection to PAS or TS is also associated with being of Asian ethnicity, of Hindu religious affiliation, and having more experience caring for dying patients. These findings suggest that, with respect to morally contested interventions at the end of life, the medical care patients receive will vary based on their physicians’ religious characteristics, ethnicity, and experience caring for dying patients.
Keywords: religion, ethics, physician-assisted suicide, terminal sedation, withdrawal of life support, ethnicity
In the United States, physicians remain the de facto arbiters for most aspects of medical care, including end-of-life interventions. Although all 50 states allow patients to refuse medical treatments, patients often lack decisional capacity in the final stages of their illness.1,2 Even when surrogates have been appointed, physicians sometimes make critical decisions regarding care without consulting the patient or the patient’s family.2 Many people fear that, should they fall gravely ill, their physician may not follow their wishes.3 For some patients, this could mean not having access to physician-assisted suicide (PAS) or terminal sedation (TS). For others, it could mean overzealous physicians refusing to withdraw life support in the face of imminent death or, conversely, implementing unwanted life-shortening interventions. Although health care policies strive to protect patient preferences, physicians remain influential in end-of-life decision making.
Patients and physicians may disagree about end-of-life care because they have differing interpretations of what a “good death” entails. In a study of the views of patients, clinicians, and other health care workers who had experience caring for the dying, Steinhauser et al3 noted that “pain and symptom management, clear decision making, preparation for death, completion, contributing to others, and affirmation of the whole person” were all core components of a “good death.” They also noted that each component has biomedical, psychological, social, and spiritual aspects and that these aspects were given different emphasis by different groups.
Disagreements about what a good death entails have often become visible in light of controversies about PAS, TS, and withdrawal of artificial life support (WLS), where previous studies have found that physicians’ opinions are associated with their religious characteristics.4–8 In all, 9 of 10 US physicians endorse some religious affiliation, and more than half say their religious beliefs influence their practice of medicine.9 Moreover, studies have consistently found that physician religiosity is associated with physicians’ approaches to a variety of ethically controversial medical practices.10–14 It is, therefore, not surprising that debates about PAS, TS, and WLS have often centered on ways religion influences patient care and public policy.
Different faiths have different perspectives on end-of-life care. Roman Catholicism prohibits suicide but permits the withdrawal of “extraordinary measures,” even if death is anticipated (but not intended) to result.15,16 Some Eastern religions, such as Buddhism and Hinduism, emphasize the karmic nature of pain and the importance of enduring suffering.15,17 For that reason, use of artificial sustenance, life support, and extensive sedation are sometimes discouraged as unnatural and possibly damaging to a peaceful death and a desirable reincarnation.15,17,18 Some traditions in Judaism emphasize an obligation to sustain life above all else, even at great cost and in the context of suffering.15 In a pluralist society like that of the United States, religious traditions may inform physicians’ approaches to end-of-life care in a variety of ways.
Although previous studies have shown that physicians’ religious beliefs influence patient care at the end of life, most of these studies are now somewhat dated and have largely been limited by oversimplified religious measures. Some have divided physicians only into the categories of Protestants, Catholics, Jews, and other,7,8,10,11,19–25 thus potentially missing ways that less represented religious traditions shape physicians’ practice. Others have included only generalized measures of religiousness (eg, frequency of prayer, religious service attendance, the importance of religion in one’s life),21,26 which cannot account for religious traditions’ varying views on suffering and death and the variety of ways in which these views are internalized. In addition, many previous studies are now more than a decade old. In the early 1970s, WLS was controversial. Ten years later, it was both commonplace and widely accepted. It is possible that a similar evolution would occur with respect to TS and even PAS. In light of these issues, an up-to-date examination of the issues is warranted.
This study updates and extends previous research by surveying a national sample of physicians from all specialties to estimate the proportion of US physicians who object to PAS, TS, and WLS, and to clarify the association between such objections and physicians’ religious characteristics. We hypothesized that physicians with higher religiosity would be more likely to object to each of these procedures. We also hypothesized that, compared with Jewish and Christian physicians, Hindus, and those from other religious traditions would be more likely to object to TS and less likely to object to WLS.
Methods
Survey Design and Administration
The methods used in this study have been described elsewhere.9,27,28 In 2003 we mailed a confidential, self-administered, 12-page questionnaire to a stratified random sample of 2000 practicing US physicians older or younger than 65 years of age, chosen from the American Medical Association Physician Masterfile, a database intended to include all physicians in the United States. We included modest oversamples of psychiatrists and several subspecialties that deal particularly with death and severe suffering (including geriatrics, pediatric subspecialties, pulmonary and critical care, oncology, physical medicine and rehabilitation, and pain medicine). Physicians received up to 3 separate mailings of the questionnaire. The third mailing offered US$20 for participation. Characteristics of survey respondents are included in Table 1. This study was approved by the University of Chicago Institutional Review Board.
Table 1.
Respondent Characteristics
| (n = 1144)a | |
|---|---|
| Demographic characteristics | |
| Age, mean (SD), y | 49.0 (8.3) |
| Gender, No. (%) | |
| Women | 300 (26) |
| Men | 842 (74) |
| Ethnicity, No. (%) | |
| White, non-Hispanic | 869 (78) |
| Asian | 158 (12) |
| Hispanic | 57 (5) |
| Black, non-Hispanic | 26 (2) |
| Other | 31 (3) |
| Region, No. (%) | |
| South | 386 (34) |
| Midwest | 276 (24) |
| Northeast | 264 (23) |
| West | 216 (19) |
| Practice characteristics | |
| Primary specialty, No. (%) | |
| Family practice | 158 (14) |
| General internal medicine | 129 (11) |
| Internal medicine subspecialties | 231 (20) |
| Obstetrics and gynecology | 80 (7) |
| Pediatrics and its subspecialties | 147 (13) |
| Psychiatry | 100 (9) |
| Surgical subspecialties | 100 (9) |
| Other | 197 (17) |
| Care of dying patients,b No. (%) | |
| None | 240 (22) |
| 1–0 | 491 (45) |
| >10 | 372 (34) |
| Religious characteristics | |
| Intrinsic religiosity, No. (%) | |
| Low | 407 (37) |
| Moderate | 292 (27) |
| High | 399 (36) |
| Religious affiliation, No. (%) | |
| Protestant | 428 (38) |
| Catholic | 244 (24) |
| Jewish | 181 (16) |
| Hindu | 54 (5) |
| Muslim | 33 (3) |
| Other religion | 70 (4) |
| None | 117 (10) |
| Religious beliefs influence medicine, No. (%) | |
| Disagree | 484 (45) |
| Agree | 633 (55) |
Totals do not all sum to 1144 because of partial nonresponse.
Number of patients who have died in previous 12 months.
Survey Content
On the questionnaire, physicians were asked to indicate whether they objected to “physician-assisted suicide” (PAS), “sedation to unconsciousness in dying patients” (TS), and “withdrawal of artificial life support” (WLS), and to indicate whether their objections were for “religious reasons, reasons unrelated to religion, or both.” Responses to these items were the criterion measures for this analysis.
Primary predictors were measures of physicians’ religious characteristics. Physicians’ religious affiliations were categorized as none (includes atheist, agnostic, and none), Protestant, Catholic, Jewish, Hindu, Muslim, or other. Intrinsic religiosity—the extent to which an individual embraces his or her religion as the master motive that guides and gives meaning to his or her life29—was measured as agreement or disagreement with 2 statements: “I try hard to carry my religious beliefs over into all my other dealings in life,” and “My whole approach to life is based on my religion.” Both statements are derived from Hoge’s Intrinsic Religious Motivation Scale30 and have been validated extensively in previous research.30–32 Intrinsic religiosity was categorized as low if physicians disagreed with both the statements, moderate if they agreed with 1 statement but not the other, and high if they agreed with both the statements. Finally, physicians were asked whether or not they agree with the statement, “My religious beliefs influence my practice of medicine.”
We also expected that physicians’ experiences with dying patients would influence their attitudes toward end-of-life care. We, therefore, asked physicians to estimate how many patients they had cared for in the previous 12 months who had died. Responses were divided into 3 categories: none, 1 to 10, and more than 10. In addition, others have noted that attitudes toward end-of-life care often vary in different ethnic communities.33 We, therefore, examined physician ethnicity as a predictor (categorized as white, non-Hispanic; black, non-Hispanic; Hispanic; Asian; and other). Finally, we examined region of practice as a predictor because we expected that public policy referenda in some Western states would have influenced physicians’ opinions about this subject. In multivariate analyses, age and gender were also included as controls.
Statistical Analysis
Case weights34 were assigned and included in analyses to account for the stratified sampling design and modest differences in response rate by gender and by foreign medical graduation. Missing data and items marked “Does not apply” were excluded from analyses. We first generated estimated proportions for each survey item. We then used the Pearson χ2 test and the multivariate logistic regression to examine differences in dichotomized criterion variables (no objection vs any objection) by each of the predictors. All analyses take into account survey design and case weights using the survey commands of Stata/SE 9.0 (Stata Corp, College Station, Texas).
Results
Survey Response
Of the 2000 potential respondents, an estimated 9% were ineligible because their addresses were incorrect or they were deceased. Details of ineligibility estimation have been reported elsewhere.27,28 Among eligible physicians, our response rate was 63% (1144/1820). Foreign medical graduates were less likely to respond than the US medical graduates (54% vs 65%, P <.01), and men were slightly less likely to respond than women (61% vs 67%, P = .03). These differences were accounted for by assigning case weights. Response rates did not differ by age, region, or board certification.
Objections to End-of-Life Practices
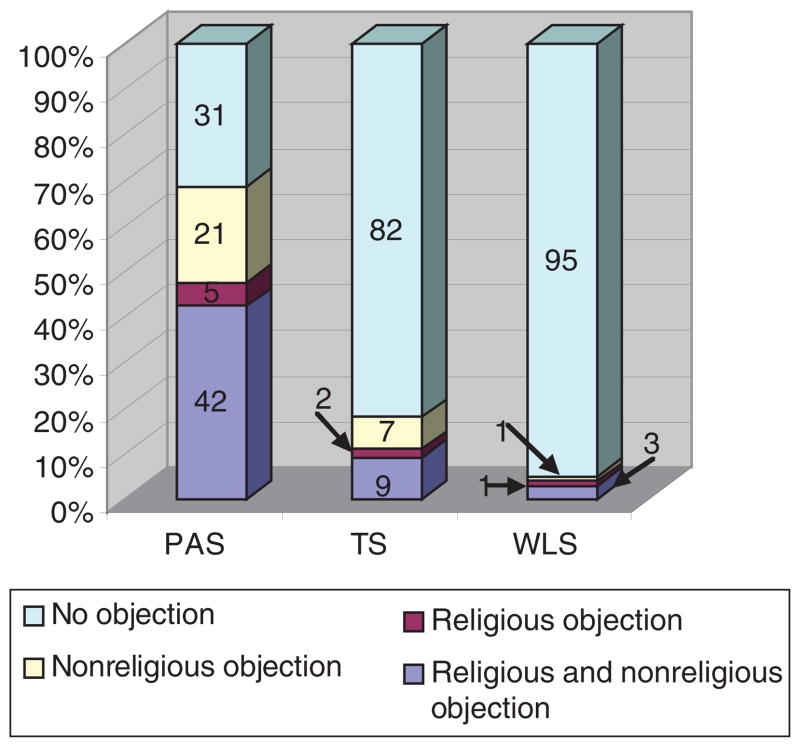
Overall, 69% of the physicians objected to PAS, 18% objected to TS, and 5% objected to WLS (SE ≤ 1.5%). Of the 69% of physicians who objected to 1 or more of these measures, most objected at least partially for religious reasons (Figure 1).
Figure 1.
Percentage of physicians who object, for religious and/or nonreligious reasons, to physician-assisted suicide (PAS), terminal sedation (TS), and withdrawal of artificial life support (WLS).
Characteristics Associated With Objections
Compared with white, non-Hispanic physicians (Table 2), Asians are more likely to object to PAS (odds ratio [OR] = 2.2; 95% confidence interval [CI], 1.3–3.7) and much more likely to object to TS (OR = 4.1; 95% CI, 2.5–6.7) and WLS (OR = 4.3; 95% CI, 2.0–9.3), even after controlling for religiosity and other covariates. Hispanic physicians are also more likely to object to TS (OR = 2.5; 95% CI, 1.2–5.0), and although other associations did not reach statistical significance, point estimates for objection to PAS, TS, and WLS were higher for all nonwhite ethnicities than for white, non-Hispanics (except for PAS, where 65% of blacks objected compared with 67% of whites). Of note, because ethnicity and religious affiliation are highly associated (χ2 [24 df] = 575, P < .0001; eg, 98% of Hindus were Asian and 97% of Jews were white), multivariate analyses examining one excluded the other to reduce the effects of multiple colinearity. Physician age and gender were not associated with any of the criterion variables.
Table 2.
Associations of Physician Ethnicity, Region, and Care of Dying With Objections to End-of-Life Interventionsa
| Physician-Assisted Suicide |
Terminal Sedation |
Withdrawal of Life Support |
||||
|---|---|---|---|---|---|---|
| Bivariate |
Multivariate |
Bivariate |
Multivariate |
Bivariate |
Multivariate |
|
| Predictor | % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) |
| All physicians | 69 | 18 | 5 | |||
| Ethnicity | ||||||
| White, non-Hispanic | 67 | 1.0 (referent) | 13 | 1.0 (referent) | ||
| Asian | 79 | 2.2 (1.3–3.7) | 37 | 1.0 (referent) | 3 | 4.3 (2.0–9.3) |
| Hispanic | 71 ns | 1.3 (0.7–2.6) | 27b | 2.5 (1.2–5.0) | 8b | 1.8 (0.4–7.0) |
| Black, non-Hispanic | 65 | 0.9 (0.4–2.4) | 27 | 2.1 (0.7–6.4) | 6 | 2.3 (0.4–15.3) |
| Other | 79 | 1.1 (0.4–2.9) | 25 | 2.4 (0.9–6.4) | 9 | 4.0 (0.9–17.9) |
| Region | ||||||
| South | 69 | 1.0 (referent) | 21 | 1.0 (referent) | 5 | 1.0 (referent) |
| Midwest | 76c | 1.5 (1.0–2.3) | 19 ns | 0.9 (0.5–1.4) | 6b | 1.0 (0.4–2.7) |
| Northeast | 65 | 1.2 (0.8–1.9) | 15 | 0.6 (0.4–1.1) | 10 | 1.9 (0.8–4.5) |
| West | 61 | 1.1 (0.6–1.5) | 15 | 0.8 (0.4–1.4) | <1 | 0.0 (0.0–0.2) |
| Care of dying | ||||||
| None | 65 | 1.0 (referent) | 18 | 1.0 (referent) | 7 | 1.0 (referent) |
| 1–10 | 68 ns | 1.2 (0.8–1.8) | 19 ns | 1.1 (0.7–1.8) | 6d | 1.0 (0.5–2.1) |
| >10 | 73 | 1.7 (1.1–2.6) | 15 | 0.8 (0.5–1.4) | 2 | 0.3 (0.1–0.9) |
NOTE: OR = odds ratio; CI = confidence interval; ns = not significant.
Bivariate results present estimated (accounting for survey design) percentages of physicians who object to the intervention. Multivariate results present estimated OR with 95% CI after adjustment for age, gender, ethnicity, region, care of dying, intrinsic religiosity, religious affiliation (not included in analyses of ethnicity), and religion influences medicine.
P < .001.
P < .01.
P < .05.
In analyses controlling for other covariates, we found that, compared with physicians from the South, those from the Midwest are modestly more likely to object to PAS (OR = 1.5; 95% CI, 1.0–2.3), and only 1 of more than 200 respondents from the West had any objection to WLS, as compared with 5% to 10% of physicians from other regions (χ2, P < .001). Compared with physicians who cared for no patients who died in the prior year, those who cared for more than 10 were modestly more likely to object to PAS (OR = 1.7; 95% CI, 1.1–2.6), and modestly less likely to object to WLS (OR = 0.3; 95% CI, 0.1–0.9).
Physicians’ religious characteristics were strongly associated with objections to PAS and TS (Table 3). Compared with physicians with low intrinsic religiosity, physicians with high intrinsic religiosity have 4.2 (95% CI, 2.9–6.2) times the odds of objecting to PAS and 2.6 (95% CI, 1.7–4.1) times the odds of objecting to TS. Those who agree that their religious beliefs influence their practice of medicine have 2.7 (95% CI, 2.0–3.7) times the odds of objecting to PAS, and 1.8 (95% CI, 1.2–2.6) times the odds of objecting to TS, and 2.0 (95% CI, 1.0–4.1) times the odds of objecting to WLS. Compared with Protestants, Jews and those with no religious affiliation who are less likely to object to PAS and TS, Hindu physicians have 3.7 (95% CI, 1.8–7.6) times the odds of objecting to TS, and Catholics have 2.8 (95% CI, 1.2–6.6) times the odds of objecting to WLS.
Table 3.
Associations of Physician Intrinsic Religiosity, Religious Affiliation, and Influence of Religion on Medicine With Objections to End of Life Interventionsa
| Physician-Assisted suicide |
Terminal Sedation |
Withdrawal of Life Support |
||||
|---|---|---|---|---|---|---|
| Bivariate |
Multivariate |
Bivariate |
Multivariate |
Bivariate |
Multivariate |
|
| Predictor | % | OR (95% CI) | % | OR (95% CI) | % | OR (95% CI) |
| All physicians | 69 | 18 | 5 | |||
| Intrinsic religiosity | ||||||
| Low | 55 | 1.0 (referent) | 12 | 1.0 (referent) | 4 | 1.0 (referent) |
| Moderate | 71b | 1.9 (1.3–2.8) | 18b | 1.6 (1.0–2.7) | 4 ns | 0.9 (0.3–2.5) |
| High | 84 | 4.2 (2.9–6.2) | 25 | 2.6 (1.7–4.1) | 7 | 2.0 (0.9–4.7) |
| Religious affiliation | ||||||
| Protestant | 75 | 1.0 (referent) | 19 | 1.0 (referent) | 3 | 1.0 (referent) |
| Catholic | 79 | 1.2 (0.8–1.9) | 22 | 1.5 (0.9–2.3) | 10 | 2.8 (1.2–6.6) |
| Jewish | 50 | 0.3 (0.2–0.5) | 4 | 0.2 (0.1–0.5) | 3 | 0.8 (0.3–2.8) |
| Hindu | 74b | 0.9 (0.4–1.9) | 43b | 3.7 (1.8–7.6) | 9c | 2.1 (0.6–7.4) |
| Muslim | 79 | 1.1 (0.4–3.1) | 18 | 1.1 (0.4–3.0) | 8 | 3.4 (0.5–22.2) |
| Other religion | 81 | 1.5 (0.8–3.0) | 25 | 1.5 (0.8–3.1) | 5 | 2.5 (0.6–10.2) |
| None | 39 | 0.2 (0.1–0.4) | 6 | 0.3 (0.1–0.8) | 3 | 0.9 (0.2–3.8) |
| Religion influences medicine | ||||||
| Disagree | 58b | 1.0 (referent) | 13d | 1.0 (referent) | 4 ns | 1.0 (referent) |
| Agree | 78 | 2.7 (2.0–3.7) | 21 | 1.8 (1.2–2.6) | 6 | 2.0 (1.0–4.1) |
NOTE: OR = odds ratio; CI = confidence interval; ns = not significant.
Bivariate results present estimated (accounting for survey design) percentages of physicians who object to the intervention. Multivariate results present estimated OR with 95% CI after adjustment for age, gender, ethnicity (not included in analyses of religious affiliation), region, and care of dying.
P < .001.
P < .05.
P < .01.
Discussion
Physicians’ perspectives on end of life appear to be linked to ethnicity, geographic region, experience caring for the dying, and the religious characteristics. PAS, still illegal in 49 states, naturally remains the most contested of the end-of-life measures examined, but WLS and TS are also somewhat controversial. Physicians usually understand their objections to these measures to be partly religious in nature, which confirms earlier findings linking physicians’ religious characteristics with their views on PAS, TS, and WLS.
The finding that frequent exposure to dying patients affects physicians’ outlook on end-of-life care is consistent with findings from previous studies.5,35,36 Physicians who cared for more patients with critical, life-threatening illnesses, or more patients who died, were more open to WLS, yet more likely to oppose PAS. It may be that physicians who care for the dying are more likely to interpret patients’ requests for PAS as “cries for help” that can and should be answered with pain and symptom management, hospice care, or counseling to help patients deal with anxiety, depression, and other concerns.4,37
With respect to regional differences, the general social conservatism of Midwesterners38 may explain why they are most likely to object to PAS. Physicians from the West may have been least likely to object to WLS because of the highly publicized political referenda there regarding PAS. For physicians who object to PAS, WLS may seem particularly acceptable and preferable in places in which PAS is already, or seems likely to become, a legal option.
Ethnicity also seems to play a role in physicians’ responses. Asians are the most likely to object to PAS, WLS, and TS, a finding that may reflect the influence of Eastern religious traditions and/or other cultural factors, such as filial piety.39,40 The fact that physicians from minority ethnicities were generally more likely than whites to object to these procedures may result from a general mistrust that many minorities have toward the health care system, and a greater fear that treatment will be abandoned prematurely.41 Thus, concern for access to medicine appears to outweigh fears of over treatment.39,40 Unlike previous studies we did not find that African Americans were less likely to support PAS.42 Yet, there were too few black respondents in our study (n = 26) to draw strong inferences about this subpopulation.
Finally, because of the cross-sectional study design, we can only speculate as to why physicians from some religions are more likely to object to certain interventions. That Catholic physicians are more likely to object to WLS than Protestants may reflect Catholic doctrines prohibiting actions intended to shorten life.15,43,44 Another possibility, as suggested during the recent Terri Schiavo controversy, is that there is an ongoing debate among Catholics about whether interventions such as parenteral nutrition and/or hydration should be considered artificial life support at all. The low likelihood that Jewish physicians will object to WLS, TS, or PAS is consistent with other studies.35,45 Jewish religious traditions distinguish actions that hasten death from those that remove impediments to death, permitting the latter but not the former.15 The apparent discord between Jewish affiliation and practice in this area may stem from the fact that Jewish physicians tend to be less religious than physicians from other religious affiliations.9 Finally, the observation that Hindu physicians are more likely to object to TS may be rooted in those Hindu writings that have discouraged measures that unduly sedate or impair mental clarity at the time of death because of concern that individuals have sufficient opportunity to expunge Karma in preparation for the next life.46
Limitations
This study has several important limitations. To begin, the term “terminal sedation” has been inconsistently defined in the medical literature.2,47,48 We used the term in this manuscript as shorthand for “sedation to unconsciousness in dying patients”—the terms used on the questionnaire. Yet, the survey instrument did not distinguish between sedating with the intent of controlling otherwise refractory physical symptoms, and sedating with the intent of making a person unconscious to remove the psychological and spiritual distress that often accompanies consciousness of imminent death. Terminal sedation can also be taken to be a form of “slow euthanasia,” when accompanied by the withdrawal of parenteral nutrition and hydration and/or performed on a patient who is not imminently dying. In addition, because PAS is a widely understood concept, it was not further defined on the survey instrument. Yet, some have found that people are less likely to object to PAS if the practice is described rather than merely being named.49 These definitional ambiguities introduce the possibility of survey error.
Although the response rate was better than average,50 and we did not find substantial evidence to suggest response bias,9,27 unmeasured characteristics may have systematically affected physicians’ willingness to respond in ways that could bias our findings. In addition, this study is not sufficiently powered to form robust estimates about physicians from minority ethnicities and religious affiliations. As such, results for those groups should be considered provisional and preliminary until further in-depth studies can be done. Furthermore, the measures of religious affiliation used here (Protestant, Catholic, Jewish, etc) do not capture important theological differences that exist between subcategories of these traditions (eg, evangelical vs mainline Protestants, or Orthodox vs Reform Jews). Finally, as a cross-sectional survey, this study cannot establish the causative pathways between the predictors and the physicians’ judgments about these end-of-life care issues; nor can it tell whether or how physicians’ judgments translate into their actual practices. Individuals may always choose, however reluctantly, to participate in actions to which they object.
Conclusion
Notwithstanding these limitations, the study findings have important implications. Although many outside the medical profession call for access to patient-directed modes of end-of-life care, individual physicians will ultimately decide whether or not they recommend, or accommodate patients’ requests for, particular medical interventions. Currently, small minorities of physicians in the United States object to TS and WLS, and like the broader public, physicians remain deeply divided about the moral legitimacy of PAS. These findings suggest that, at least with respect to these morally contested interventions, the medical care that patients receive at the end of life is not uniform, but is rather shaped by, among other things, a physician’s ethnicity, culture, religion, and personal experiences. Further study is needed to clarify how these diverse factors shape physicians’ approaches to controversial aspects of end-of-life care in the United States and in other countries. In the meantime, physicians who often deal with the dying would do well to be candid with their patients about reservations they may have regarding PAS, TS, and WLS.
What this study adds
What is already known on this subject
Debates in the United States about PAS, TS, and WLS have often centered on ways religion influences patient care and public policy. Several previous studies have found that physicians’ opinions about these practices are associated with their religious characteristics. Yet, previous studies are now dated and have been constrained by having oversimplified religious measures and by not examining the contribution of physician ethnicity and other factors.
What this study adds
This study updates findings from the last decade and suggests that most US physicians still object to PAS and a substantial minority object to TS. Most physicians’ who object to PAS, TS, or WLS do so at least partially for religious reasons, but physicians’ perspectives on end of life appear also to be linked to ethnicity, geographic region, and experience caring for the dying.
Acknowledgments
This study was funded by grant support from The Greenwall Foundation (FAC, MHC) and the Robert Wood Johnson Clinical Scholars Program (FAC, MHC, JDL). FAC is also supported by a career development award (K23/AT002749) from NCCAM. The study sponsors had no involvement in the design of the study; the collection, analysis, and interpretation of data; the writing of the report; or the decision to submit the paper for publication.
References
- 1.Lynch M. Palliative sedation. Clin J Oncol Nurs. 2003;7:653–657. 667. doi: 10.1188/03.CJON.653-657. [DOI] [PubMed] [Google Scholar]
- 2.Rietjens JA, van der Heide A, Vrakking AM, Onwuteaka-Philipsen BD, van der Maas PJ, van der Wal G. Physician reports of terminal sedation without hydration or nutrition for patients nearing death in the Netherlands. Ann Intern Med. 2004;141:178–185. doi: 10.7326/0003-4819-141-3-200408030-00006. [DOI] [PubMed] [Google Scholar]
- 3.Steinhauser KE, Clipp EC, McNeilly M, Christakis NA, McIntyre LM, Tulsky JA. In search of a good death: observations of patients, families, and providers. Ann Intern Med. 2000;132:825–832. doi: 10.7326/0003-4819-132-10-200005160-00011. [DOI] [PubMed] [Google Scholar]
- 4.Ganzini L, Nelson HD, Schmidt TA, Kraemer DF, Delorit MA, Lee MA. Physicians’experiences with the Oregon Death with Dignity Act. N Engl J Med. 2000;342:557–563. doi: 10.1056/NEJM200002243420806. [DOI] [PubMed] [Google Scholar]
- 5.Doukas DJ, Waterhouse D, Gorenflo DW, Seid J. Attitudes and behaviors on physician-assisted death: a study of Michigan oncologists. J Clin Oncol. 1995;13:1055–1061. doi: 10.1200/JCO.1995.13.5.1055. [DOI] [PubMed] [Google Scholar]
- 6.Essinger D. Attitudes of Tennessee physicians toward euthanasia and assisted death. South Med J. 2003;96:427–435. doi: 10.1097/01.SMJ.0000051144.80620.C1. [DOI] [PubMed] [Google Scholar]
- 7.Kaldjian LC, Jekel JF, Bernene JL, Rosenthal GE, Vaughan-Sarrazin M, Duffy TP. Internists’ attitudes towards terminal sedation in end of life care. J Med Ethics. 2004;30:499–503. doi: 10.1136/jme.2003.004895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaldjian LC, Wu BJ, Kirkpatrick JN, Thomas-Geevarghese A, Vaughan-Sarrazin M. Medical house officers’attitudes toward vigorous analgesia, terminal sedation, and physician-assisted suicide. Am J Hosp Palliat Care. 2004;21:381–387. doi: 10.1177/104990910402100514. [DOI] [PubMed] [Google Scholar]
- 9.Curlin FA, Lantos JD, Roach CJ, Sellergren SA, Chin MH. Religious characteristics of U.S. physicians: a national survey. J Gen Intern Med. 2005;20:629–634. doi: 10.1111/j.1525-1497.2005.0119.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Emanuel EJ, Daniels ER, Fairclough DL, Clarridge BR. The practice of euthanasia and physician-assisted suicide in the United States: adherence to proposed safeguards and effects on physicians. JAMA. 1998;280:507–513. doi: 10.1001/jama.280.6.507. [DOI] [PubMed] [Google Scholar]
- 11.Christakis NA, Asch DA. Physician characteristics associated with decisions to withdraw life support. Am J Public Health. 1995;85:367–372. doi: 10.2105/ajph.85.3.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schmidt TA, Zechnich AD, Tilden VP, et al. Oregon emergency physicians’ experiences with, attitudes toward, and concerns about physician-assisted suicide. [comments] Acad Emerg Med. 1996;3:938–945. doi: 10.1111/j.1553-2712.1996.tb03323.x. [DOI] [PubMed] [Google Scholar]
- 13.Hudson Rosen RA, Werley HH, Ager JW, Shea FP. Health professionals’ attitudes toward abortion. Public Opin Q. 1974;38:159–173. [PubMed] [Google Scholar]
- 14.Snowden R, Kennedy KI, Leon F, et al. Physicians’ views of periodic abstinence methods: a study in four countries. Stud Fam Plann. 1988;19:215–226. [PubMed] [Google Scholar]
- 15.Hamel R, DuBose ER. Views of the major faith traditions. In: Hamel R, editor. Active Euthanasia, Religion and the Public Debate. Chicago, IL: Park Ridge Center; 1991. pp. 45–77. [Google Scholar]
- 16.Clarfield AM, Gordon M, Markwell H, Alibhai SMH. Ethical issues in end-of-life geriatric care: the approach of three monotheistic religions—Judaism, Catholicism, and Islam. J Am Geriatr Soc. 2003;51:1149–1154. doi: 10.1046/j.1532-5415.2003.51364.x. [DOI] [PubMed] [Google Scholar]
- 17.Tanida N. The view of religions toward euthanasia and extraordinary treatments in Japan. J Relig Health. 2000;39:339–354. doi: 10.1023/a:1010361019006. [DOI] [PubMed] [Google Scholar]
- 18.Barham D. The last 48 hours of life: a case study of symptom control for a patient taking a Buddhist approach to dying. Int J Palliative Nurs. 2003;9:245–251. doi: 10.12968/ijpn.2003.9.6.11509. [DOI] [PubMed] [Google Scholar]
- 19.Dickenson D. Are medical ethicists out of touch? Practitioner attitudes in the US and UK towards decisions at the end of life. J Med Ethics. 2000;26:254–260. doi: 10.1136/jme.26.4.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee MA, Nelson HD, Tilden VP, Ganzini L, Schmidt TA, Tolle SW. Legalizing assisted suicide—views of physicians in Oregon. N Engl J Med. 1996;334:310–315. doi: 10.1056/NEJM199602013340507. [DOI] [PubMed] [Google Scholar]
- 21.Miccinesi G, Fischer S, Paci E, et al. Physicians’ attitudes towards end-of-life decisions: a compassion between seven countries. Soc Sci Med. 2005;60:1961–1974. doi: 10.1016/j.socscimed.2004.08.061. [DOI] [PubMed] [Google Scholar]
- 22.Sprung C, Cohen S, Sjokvist P, et al. End-of-life practices in European intensive care units: the Ethicus Study. JAMA. 2003;290:790–797. doi: 10.1001/jama.290.6.790. [DOI] [PubMed] [Google Scholar]
- 23.Suarez-Almazor ME, Belzile M, Bruera E. Euthanasia and physician-assisted suicide: a comparative survey of physicians, terminally ill cancer patients, and the general population. J Clin Oncol. 1997;15:418–427. doi: 10.1200/JCO.1997.15.2.418. [DOI] [PubMed] [Google Scholar]
- 24.Vincent JL. Forgoing life support in western European intensive care units: the results of an ethical questionnaire. Crit Care Med. 1999;27:1626–1633. doi: 10.1097/00003246-199908000-00042. [DOI] [PubMed] [Google Scholar]
- 25.Waddell C, Clarnette R, Smith M, Oldham L, Kellehear A. Treatment decision-making at the end of life: a survey of Australian doctors’ attitudes towards patients’ wishes and euthanasia. Med J Aust. 1996;165:540–544. [PubMed] [Google Scholar]
- 26.Bachman JG, Alcser KH, Doukas DJ, Lichtenstein RL, Corning AD, Brody H. Attitudes of Michigan physicians and the public toward legalizing physician-assisted suicide and voluntary euthanasia. N Engl J Med. 1996;334:303–309. doi: 10.1056/NEJM199602013340506. [DOI] [PubMed] [Google Scholar]
- 27.Curlin FA, Chin MH, Sellergren SA, Roach CJ, Lantos JD. The association of physicians’ religious characteristics with their attitudes and self-reported behaviors regarding religion and spirituality in the clinical encounter. Med Care. 2006;44:446–453. doi: 10.1097/01.mlr.0000207434.12450.ef. [DOI] [PubMed] [Google Scholar]
- 28.Curlin FA, Lawrence RE, Chin MH, Lantos JD. Religion, conscience, and controversial clinical practices. N Engl J Med. 2007;356:593–600. doi: 10.1056/NEJMsa065316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Allport G, Ross J. Personal religious orientation and prejudice. J Pers Soc Psychol. 1967;5:447–457. doi: 10.1037/0022-3514.5.4.432. [DOI] [PubMed] [Google Scholar]
- 30.Hoge DR. A validated intrinsic religious motivation scale. J Sci Study Relig. 1972;11:369–376. [Google Scholar]
- 31.Koenig H, Parkerson GR, Jr, Meador KG. Religion index for psychiatric research. Am J Psychiatry. 1997;154:885–886. doi: 10.1176/ajp.154.6.885b. [DOI] [PubMed] [Google Scholar]
- 32.Gorsuch RL, Mcpherson SE. Intrinsic-extrinsic measurement, I/E-revised and single-item scales. J Sci Study Relig. 1989;28:348–354. [Google Scholar]
- 33.Crawley LM, Marshall PA, Lo B, Koenig BA. Strategies for culturally effective end-of-life care. Ann Intern Med. 2002;136:673–679. doi: 10.7326/0003-4819-136-9-200205070-00010. [DOI] [PubMed] [Google Scholar]
- 34.Groves RM, Fowler FJ, Couper MP, Lepkowski JM, Singer E, Tourangeau R. Survey Methodology. Hoboken, NJ: John Wiley & Sons Inc; 2004. [Google Scholar]
- 35.Meier DE, Emmons C-A, Wallenstein S, Quill T, Morrison RS, Cassel CK. A national survey of physician-assisted suicide and euthanasia in the United States. N Engl J Med. 1998;338:1193–1201. doi: 10.1056/NEJM199804233381706. [DOI] [PubMed] [Google Scholar]
- 36.Weiss G. Attitudes of college students about physician assisted suicide: the influence of life experiences, religiosity, and belief in autonomy. Death Stud. 1996;20:587–599. doi: 10.1080/07481189608252764. [DOI] [PubMed] [Google Scholar]
- 37.Bascom P, Tolle S. Responding to requests for physician assisted suicide. JAMA. 2002;288:91–98. doi: 10.1001/jama.288.1.91. [DOI] [PubMed] [Google Scholar]
- 38.Weakliem DL, Biggert R. Region and political opinion in the contemporary United States. Soc Forces. 1999;77:863–886. [Google Scholar]
- 39.Kwak J, Haley WE. Current research findings on end-of-life decision making among racially or ethnically diverse groups. Gerontologist. 2005;45:634–641. doi: 10.1093/geront/45.5.634. [DOI] [PubMed] [Google Scholar]
- 40.Blackhall LJ, Frank G, Murphy ST, Michel V, Palmer JM, Azen SP. Ethnicity and attitudes towards life sustaining technology. Soc Sci Med. 1999;48:1779–1789. doi: 10.1016/s0277-9536(99)00077-5. [DOI] [PubMed] [Google Scholar]
- 41.Crawley L, Marshall P, Lo B, Koenig B. Strategies for culturally effective end of life care. Ann Intern Med. 2002;136:673–679. doi: 10.7326/0003-4819-136-9-200205070-00010. [DOI] [PubMed] [Google Scholar]
- 42.Lichtenstein RL, Alcser KH, Corning AD, Bachman JG, Doukas DJ. Black/white differences in attitudes toward physician-assisted suicide. J Natl Med Assoc. 1997;89:125–133. [PMC free article] [PubMed] [Google Scholar]
- 43.Domino G. Attitudes toward physician assisted suicide: Poland and the United States. OMEGA (Westport) 2002–2003;46:105–115. doi: 10.2190/qfxy-q06a-mt87-4ygm. [DOI] [PubMed] [Google Scholar]
- 44.McStay R. Terminal sedation: palliative care for intractable pain, post glucksberg and quill. Am J Law Med. 2003;29:45–76. [PubMed] [Google Scholar]
- 45.Miller F, Meier D. Voluntary death: a comparison if terminal dehydration and physician-assisted suicide. Ann Intern Med. 1998;128:559–562. doi: 10.7326/0003-4819-128-7-199804010-00007. [DOI] [PubMed] [Google Scholar]
- 46.Crawford SC. Dilemmas of Life and Death: Hindu Ethics in a North American Context. Albany, NY: State University of New York Press; 1995. [Google Scholar]
- 47.Jansen LA, Sulmasy DP. Proportionality, terminal suffering and the restorative goals of medicine. Theor Med Bioeth. 2002;23:321–227. doi: 10.1023/a:1021209706566. [DOI] [PubMed] [Google Scholar]
- 48.Gillick M. Terminal sedation: an acceptable exit strategy? Ann Intern Med. 2004;141:236–237. doi: 10.7326/0003-4819-141-3-200408030-00018. [DOI] [PubMed] [Google Scholar]
- 49.Parkinson L, Rainbird K, Kerridge I, et al. Cancer patients’ attitudes toward euthanasia and physician-assisted suicide: the influence of question wording and patients’ own definitions on responses. J Bioeth Inq. 2005;2:82–89. doi: 10.1007/BF02448847. [DOI] [PubMed] [Google Scholar]
- 50.Asch DA, Jedrziewski MK, Christakis NA. Response rates to mail surveys published in medical journals. J Clin Epidemiol. 1997;50:1129–1136. doi: 10.1016/s0895-4356(97)00126-1. [DOI] [PubMed] [Google Scholar]