Abstract
Purpose: Although nursing homes (NHs) are criticized for offering poor quality continence care, little is known about the organizational processes that underlie this care. This study investigated the influence of organizational culture on continence care practices in two NHs. Design and Methods: This ethnographic study explored continence care from the perspectives of NH stakeholders, including residents and interdisciplinary team members. Data were collected through participant observation, interviews, and archival records. Results: Human relations dimensions of organizational culture influenced continence care by affecting institutional missions, admissions and hiring practices, employee tenure, treatment strategies, interdisciplinary teamwork, and group decision making. Closed system approaches, parochial identity, and an employee focus stabilized staff turnover, fostered evidence-based practice, and supported hierarchical toileting programs in one facility. Within a more dynamic environment, open system approaches, professional identity, and job focus allowed flexible care practices during periods of staff turnover. Neither organizational culture fully supported interdisciplinary team efforts to maximize the bladder and bowel health of residents. Implications: Organizational culture varies in NHs, shaping the continence care practices of interdisciplinary teams and leading to the selective use of treatments across facilities. Human relations dimensions of organizational culture, including open or closed systems, professional or parochial identity, and employee or job focus are critical to the success of quality improvement initiatives. Evidence-based interventions should be tailored to organizational culture to promote adoption and sustainability of resident care programs.
Keywords: Organizational culture, Incontinence, Interdisciplinary teams, Qualitative research
Nursing homes (NHs) are not known as continence-friendly environments (DuBeau, 2005; Ouslander & Johnson, 2004; Palmer & Johnson, 2003). Although people who live in long-term care (LTC) settings rely upon staff for dressing, grooming, and moving (Jones, Dwyer, Bercovitz, & Strahan, 2009), when it comes to managing incontinence, residents must learn to “make the best of it” or “suffer with it” as care providers do not offer much help (Robinson, 2000). NH staff do not adequately assess or document continence status (Schnelle, Cadogan, Grbic, et al., 2003; Watson, Brink, Zimmer, & Mayer, 2003) or assist residents to the toilet often enough to achieve optimal continence levels (Remsburg, Palmer, Langford, & Mendelson, 1999; Schnelle, Cadogan, Yoshii, et al., 2003). Although many residents might prefer toileting programs or medications for incontinence (Johnson, Ouslander, Uman, & Schnelle, 2001), disposable briefs remain the treatment of choice in this setting (Watson et al.). As a result, upwards of 75% of residents are incontinent of urine, feces, or both in some LTC facilities (Landefeld et al., 2008).
Given their everyday experiences, incontinence often seems inevitable to residents and staff in NHs (Resnick et al., 2006; Robinson, 2000). Although evidence-based treatments for urinary incontinence do exist (Fink, Taylor, Tacklind, Rutks, & Wilt, 2008), studies of various toileting programs have struggled with small samples and high attrition rates (Engberg, Kincade, & Thompson, 2004). Most controlled trials have demonstrated only modest statistical improvement in continence rates among treatment groups (Eustice, Roe, & Paterson, 2000; Ostaszkiewicz, Johnston, & Roe, 2004). The most promising intervention, prompted voiding, has limited utility for the majority of residents (Ouslander et al., 1995) and unresolved implementation issues when delivered by employees (Lekan-Rutledge, Palmer, & Belyea, 1998; Remsburg et al., 1999).
Staff may not know how best to manage incontinence, particularly at the facility level (DuBeau, Ouslander, & Palmer, 2007). Many quality assurance strategies, such as process improvement teams, structured assessments, or clinical guidelines, are not implemented into practice, even among facilities in the same corporation (Lawhorne, Ouslander, & Parmelee, 2008). The reasons for this are unclear as few investigators have compared continence treatments and outcomes across facilities. Jirovec (1991) reported significant facility-level disparities in resident response to prompted voiding in two NHs. However, as resident care and administrative practices were not assessed, the author speculated that an unexplored organizational difference may have led to employees’ more faithful adherence to the treatment protocol in one facility.
NH stakeholders have identified several organizational practices that support higher quality continence care. LTC workers and administrators recognize adequate staffing, training, teamwork, and timely feedback as critical components of successful continence care programs (Lekan-Rutledge et al., 1998; Resnick et al., 2006). Continence care also may be driven by other human relations factors, including administrator and clinician leadership (Lekan-Rutledge et al., 1998), staff beliefs (Tannenbaum, Labrecque, & Lepage, 2005), and mutual respect for team members (Mather & Bakas, 2002). Unfortunately, even though employees can articulate how NHs might improve incontinence management, the reasons why most facilities do not meet minimum standards of care remain unclear (Watson et al., 2003).
Smith (1998) proposed that organizational culture has a powerful influence on continence care. Organizational culture is a pattern of shared assumptions that people within an organization learn as a group, pass on to new members, and which influences their social interactions (Schein, 2004). Although health systems researchers have identified variations in NH culture (Anderson, Issel, & McDaniel, 2003; Colon-Emeric et al., 2006; Scott-Cawiezell, Jones, Moore, & Vojir, 2005), how these factors affect continence care is not well known (Roe et al., 2004). Although ethnographers have revealed different ways that persons with incontinence are treated in NHs (Gubrium, 1975; Jervis, 2001; Kayser-Jones, 1981), few researchers have observed the context of continence care in LTC organizations (Taunton, Swagerty, Lasseter, & Lee, 2005; Wright, McCormack, Coffey, & McCarthy, 2007), and none have compared these practices across sites.
An insufficient understanding of the real world context of continence care has impeded the translation of knowledge gained from clinical trials into clinical practice (Wyman et al., 2004). Although quantitative studies have described what NH workers are not doing to manage incontinence (Schnelle, Cadogan, Grbic, et al., 2003; Schnelle, Cadogan, Yoshii, et al., 2003; Watson et al., 2003), the processes by which people develop organization-specific treatment strategies or why they sustain, modify, or suspend these practices over time are not well known. Roe and colleagues (2004) affirmed the need for research to understand the “how and why” of continence care to address institutional barriers and facilitate the adoption of evidence-based practices (p. S59). Toward that aim, this study explored the impact of human relations dimensions of organizational culture on continence care practices of interdisciplinary teams in two NHs.
Theoretical Perspective
Hofstede and Hofstede (2005) described culture as “software of the mind” or the shared patterns of thought, emotion, and action that distinguish one group of people from other groups (p. 4). Organizational culture then is the “collective programming of the mind that distinguishes the members of one organization from another” (pp. 282–283). This culture is manifested at varying levels, with values comprising an unobservable core and practices, including rituals, heroes or models, and symbols and words, forming more readily interpretable external layers. Culture also is a holistic attribute, in that it is socially constructed and maintained by stakeholders invested in the organization; is determined by historical circumstances; and persists through episodes of planned change, periodic transitions, and organizational crises (p. 282). Of note, although cultural values may vary little between companies within an industry, organizational practices, which people adopt through everyday interactions with coworkers, often differ considerably.
Hofstede and Hofstede (2005) discerned six dimensions of organizational culture: process-results orientation, pragmatic–normative outlook, tight–loose control, open–closed systems, professional–parochial identity, and job–employee focus. The first three pairings may be thought of as procedural aspects of organizational culture, whereas the latter three dichotomies represent its human relations facets. More specifically, closed systems are characterized by insiders’ wary attitudes toward new people and ideas, whereas receptive approaches to the unfamiliar exemplify open systems. Cultures that emphasize professional identity hire workers based upon perceived competence, whereas parochial cultures also take into account personal backgrounds. Employee-focused cultures enhance worker welfare, whereas job-focused cultures prioritize organizational needs. These three human relations dimensions provided an analytic framework for exploring the impact of organizational culture on the continence care practices of people in two NHs.
Methods
Focused ethnography is a qualitative research method for exploring a narrowed topic or specific issue with the purposes of understanding its social context and building knowledge for application in clinical practice (Roper & Shapira, 2000). Theoretical and practical insights about continence care were gained from the perspectives of NH stakeholders. Data were gathered for a period of 15 months using ethnographic field methods, including participant observation, interviews, and archival records (Crabtree & Miller, 1999). Verbatim interview quotes are identified with “quotation marks.” The institutional review board of the sponsoring university approved the human subjects protections and data procedures.
Settings
The settings were two NHs located in one Midwestern community with a population of less than 30,000. Facilities with baseline disparities in continence care practices and incontinence rates were sought so cultural patterns underlying their similarities and differences might be isolated and understood (Kleinman, 1978). As in the comparative ethnography of two NHs by Kayser-Jones (1981), these facilities were identified first from professional connections. Then, using data from Nursing Home Compare (Centers for Medicare and Medicaid Services [CMS], 2009) and conversations with administrators, facilities were selected purposively based upon their heterogeneity in organizational characteristics that distinguish higher and lower quality NHs, such as leadership stability, team processes, and active quality programs (Rantz et al., 2004). Facility names were changed and some identifiable details modified in publications to protect the confidentiality of participants, with facility pseudonyms reflecting topographical features of the environment.
Hidden Valley was a 150-bed, multi-nursing home, for-profit chain facility founded 10 years ago by an out-of-state corporation. This NH was marketed as a rehabilitation center with skilled nursing, intermediate care, and dementia unit. Resident rooms were double occupancy with shared toilet. A few single rooms and triples also were available. The facility had no formal continence care policy. The baseline rate of bowel and bladder incontinence among residents was 60%. Midway through the study, the percentage of low-risk residents with incontinence dropped to 52% compared with a state average of 41% and national average of 47% (CMS, 2009).
The Hillcrest was a 135-bed, not-for-profit, nonchain facility sponsored by one religious organization for eight decades. This intermediate care facility was licensed for skilled nursing a few months before the study. Most resident rooms were singles with a private toilet, though several doubles with shared toilets were available. There was an established incontinence care system and a baseline prevalence of bladder and bowel incontinence among residents of 38%. At midpoint, the percentage of low-risk residents with incontinence had risen to 41% (CMS, 2009).
Participants
Participants were NH stakeholders, or adults aged 18 years or older associated with study sites, including employees, residents, families, and consultants. Purposive sampling for interviews sought employees from three groups involved in continence care, with care taken to talk with workers occupying the same positions at the two facilities. Direct care workers were licensed practical nurses, certified nursing assistants (CNAs), and activities and therapy assistants. Professionals were registered nurses (RNs), occupational and physical therapists, social workers, pastoral counselors, and directors or clerks in admissions, activities, health records, purchasing, and environmental services. Executives were administrators, directors of nursing (DON), assistant directors of nursing (ADON), and business managers. Although laundry workers, housekeepers, physicians, and other staff also make key contributions to continence care, individuals in these positions who were asked for formal interviews declined this request.
Data Collection and Analysis
The researcher engaged in an inductive and concurrent process of data collection, coding, and analysis (Crabtree & Miller, 1999). Participant observation on day and evening shifts placed continence care within the daily routines of residents and staff. Observations occurred at each data collection session to lessen the likelihood that participants would change behaviors when the researcher was present. Conversations of varying structures supported these observations (Crabtree & Miller). People interviewed signed an informed consent indicating an understanding of the research process and were offered a gift certificate in appreciation for their time, which most donated to the activities department of their facility. Nearly 60 individuals engaged in semi-structured interviews that lasted about 60 min (range 0.5–2.5 hr). Interview topics were derived from the literature on incontinence and translational research and based upon ongoing participant observations of resident care in both facilities. Interviews were tailored to workers’ roles, but all included questions about the employees’ experiences working in LTC, beliefs about older adults, and understanding of continence care practices. Verbatim transcripts of audiotaped interviews were made. Archival record reviews included procedure manuals, policies, census records, employee job descriptions, facility maps, and documentation forms.
The emergent data collection–analysis process allowed for a contextualized understanding of continence care in each facility informed by participants’ social interactions, organizational processes, and institutional structures as these changed over time and in response to unexpected circumstances and unfolding events. Detailed fieldnotes documented this process and included date and time, location, participants and activities, methodological comments, and theoretical interpretations. Qualitative analysis software was used to manage and code data. The dimensions of organizational culture of Hofstede and Hofstede (2005) were applied to this existing data set to explore how the interactions of interdisciplinary team members influenced continence care in these two NHs. Trustworthiness of the data collection–analysis process was supported through prolonged engagement in the research sites, purposive sampling of persons who could offer key insights as well as circumstances in which continence care was likely, and longitudinal cross-facility observations designed to ascertain a range of organizational factors related to continence care (Crabtree & Miller, 1999). Credibility and confirmability were enhanced through data triangulation using multiple methods, sources, and perspectives; debriefings with experienced research mentors; the use of an established theoretical framework to guide analysis; and member checks with key informants to discuss and expand findings and to uncover researcher biases, whereas transferability was enhanced by presenting sufficient detail on the study context for readers to determine if the findings are applicable to other settings or situations (Lincoln & Guba, 1985).
Results
Open or Closed Organizational Systems
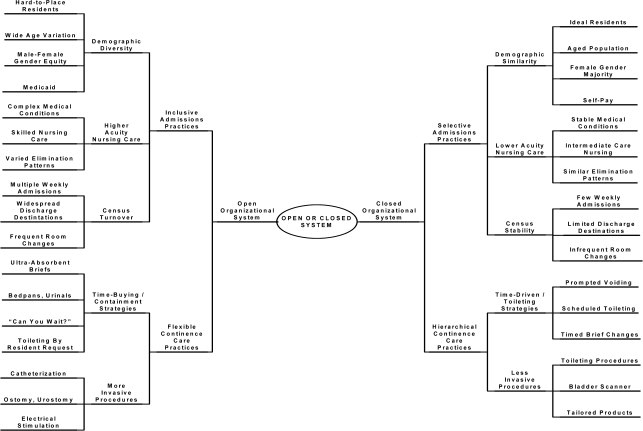
This organizational culture dimension contrasts open and closed systems. Open systems are characterized by members’ acceptance of difference, whereas closed systems are typified by wary attitudes toward the unfamiliar. Whether an NH had an open or closed system influenced two aspects of continence care, resident admissions practices and treatment strategies (Figure 1).
Figure 1.
Impact of open or closed organizational system on continence care practices in nursing homes.
Continence Care as an Open System.—
Hidden Valley approached resident care within an open systems perspective. This NH was part of a multilayered organizational structure composed of corporate headquarters, regional divisions, local facilities, and contractual partners. New people, programs, and technologies were introduced regularly. This organizational openness influenced continence care in two ways. Inclusive admission practices led to an eclectic resident population with rapid census turnover. These residents had varied elimination patterns that could not be addressed solely with toileting programs. Thus, nursing staff used flexible time-buying containment strategies to treat the continence needs of this diverse population.
Inclusive Admissions Practices.—
Hidden Valley had a regional reputation for accepting “hard-to-place” residents, including people with complex medical conditions and high acuity nursing needs. This organizational practice was consistent with the unwritten, but oft repeated, mission: “to provide health care for everyone who needs it.” Inclusive admissions encouraged demographic diversity. Although their average age was 74.5 years, 75 years spanned the lives of the youngest and the oldest residents (24–99 years). Men and women were equally represented. Most residents received Medicaid, so meager reimbursement was applied to incontinence treatments.
With its rehabilitation focus, Hidden Valley experienced rapid census turnover as staff admitted, transferred, or discharged many skilled and long-stay residents each week. The census averaged 90 residents (78% occupancy for 115 beds in use) and ranged from 75 to 105 residents (65%–91% occupancy) for a period of 1 year. Room changes to “open up male or female beds” also were common. Census fluctuations made it difficult for staff to learn residents’ elimination patterns and preferences and reinforced the use of flexible continence care practices.
Flexible Continence Care Practices.—
Hidden Valley residents had complex health needs that challenged staff in terms of time, costs, comfort, and complications. Many residents required invasive or time-consuming treatments, such as people with spinal cord injuries, ostomy, urinary catheters, or antibiotic-resistant infections. Some people had amputations and many were obese, which made restroom transfers “tricky” or “impossible.” Skilled residents were relearning their toileting skills, but required much staff assistance. When caring for people with higher acuity needs, employees asked long-stay residents to “wait their turn” or “hold it a little longer.” Thus, continence care was not based upon health assessments but was in response to the most pressing organizational needs. Nurses and CNAs relied on “time-buying” containment strategies, such as bedpans, urinals, and diapers, for these residents. Toileting was by request, and only when staff could “squeeze it in.” Call lights alarmed for 5 min as staff attended to other residents. Few treatments optimized bladder and bowel health and some, such as infrequent pad changes or extended periods placed on a bedpan, put residents at risk for skin breakdown or infections.
Continence Care as a Closed System.—
At The Hillcrest, continence care was approached from a closed system perspective. The board of directors, administrators, and department heads limited potential problems by carefully fitting new people and innovations into the organization. This closed system affected continence care in two ways. First, selective admissions practices fostered census stability and assured minimal demographic variation among residents. Second, as long-stay residents shared similar elimination patterns and required fewer invasive procedures, staff could organize toileting interventions along an efficient time-driven treatment hierarchy.
Selective Admissions.—
Admissions staff sought out people who fit the ideal of “a Hillcrest resident.” A social worker’s questions about a prospective resident outlined potential problems to avoid: “Your wife cries? Is she incontinent? How is her memory? How would you pay for her stay?” Another individual also was described in exclusionary terms: “He’s really not our type of person. He’s only 56. He wouldn’t have much in common with our residents.” This screening process matched the institutional mission: We provide quality care to the aged and the infirm. Two resident demographics predominated: female gender (>80%) and very old age (mean of 90 years, range 65–104 years). With between three and eight admissions and discharges per month, there were modest census fluctuations, which averaged 121 residents (89% occupancy) and ranged from 112 to 125 residents (82%–93% occupancy) for a period of 12 months. Selective admissions and stable census allowed interdisciplinary teams to use less invasive procedures and treatment hierarchies.
Hierarchical Continence Care Practices.—
The Hillcrest residents’ similar elimination patterns allowed CNAs to predict their continence care needs and to manage these with individualized toileting programs. A hierarchical incontinence management system mirrored the three-story architecture of the building and was time driven. Third floor residents toileted independently or received prompted voiding. Second floor residents with physical limitations were on scheduled toileting programs. First floor residents with memory loss had briefs changed on a timed basis. Nursing staff wore pagers and were contacted if a resident needed to toilet outside this schedule. Although toileting was effective for most residents, employees resisted any intervention considered “invasive or potentially dangerous,” including pessaries, medications, and pelvic floor exercises.
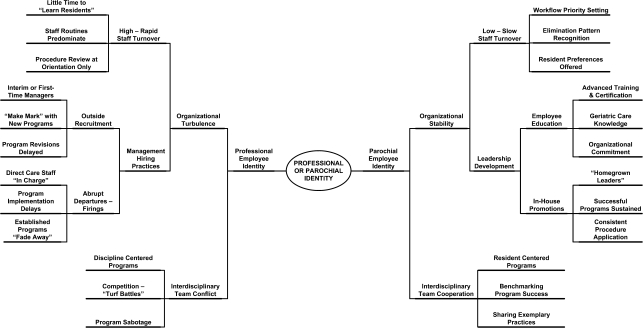
Professional or Parochial Employee Identity
This dimension posits that employees derive a sense of working self from either the work they do or from the place where they work. Professional organizations attract workers who view jobs as steps along a career path, whereas employees in parochial cultures make long-term commitments to one workplace. In these NHs, employee identity affected continence care with organizational turbulence and in the working relationships of interdisciplinary teams (Figure 2).
Figure 2.
Impact of professional or parochial employee identity on continence care practices in nursing homes.
Continence Care in a Professional Culture.—
Hidden Valley typified a professional culture where employees identified with their occupational group rather than the workplace. Voluntary turnover was endemic among direct care and professional staff and cyclical among managers as they moved onto “better jobs.” The corporation also fired administrators about every 3 years, often after a state survey. For a period of 15 months, five administrators (three interims); five DONs (three interim); four care plan coordinators (two interim); and two directors each in the rehabilitation, social services, and admissions departments led the facility. Organizational turbulence, management hiring practices, and interdisciplinary team conflicts delayed program implementation and threatened the sustainability of new and existing continence care interventions.
Organizational Turbulence.—
Although many employees had worked at Hidden Valley for 5 years or more, annual turnover rates in the nursing and therapy departments were greater than 50%. Due to these brief work histories, direct care and professional staff had little time to learn residents’ elimination patterns. Employees had short orientations with few opportunities to refine their skills through coworker feedback. Many workers were unaware of facility policies. Only one procedure manual, not updated in the 10 years since the company incorporated, was available and this was locked in the DON’s office for more than 12 hr each day. Staff provided continence care using their own routines rather than residents’ preferences or facility policies.
Management tenure sometimes lasted only weeks or months. Department managers were usually hired from outside the facility. Many administrators and DONs worked as interim directors and focused on day-to-day management rather than program development. Other directors were first-time managers who embraced the professional challenge of “changing this place for the better” by initiated new programs. In 1 year, new management staff initiated six incontinence programs: “Tea Time” toileting, a new product line, electrical stimulation (twice), “toileting in advance of need,” and a revised bladder record. Although directors experimented with new programs, no procedure was formalized into a written policy, which prevented direct care staff from learning the new practice standards. For 15 months, a yellow sticky note placed in the policy binder outlined the continence care program: B & B policy under revision. Many new and interim directors were not aware of cultural norms and did not engage informal leaders in new initiatives. With the exception of the latest line of incontinence briefs, direct care staff rarely changed their clinical practices to align with new programs introduced by management.
Interdisciplinary Conflict.—
Continence care treatments were difficult to sustain at Hidden Valley, as interdisciplinary conflicts occurred when implementation efforts involved more than one department. Without team meetings to bring staff together, employees connected with their occupational groups rather than the organization, so “turf battles” were common. For instance, Medicaid residents could not enroll in a pelvic floor rehabilitation program until they failed a 6-week trial of scheduled toileting. Therapists needed the nursing staff to implement the toileting program, but did not provide training, assess residents’ continence status, or help set up toileting schedules, as this was “the nurses’ job.” The nurses and aides were inconsistent in completing bladder records and toileting residents, as they viewed this program as “the therapists’ thing.” This lack of interdisciplinary and interdepartmental collaboration prohibited the implementation of therapeutic interventions for residents with incontinence.
Continence Care in a Parochial Culture.—
The organizational culture of The Hillcrest epitomized parochial culture. People worked at The Hillcrest because it was The Hillcrest. Employees reminisced about their relatives who had lived here, and many saw their pasts and futures as connected with this facility. Parochial culture affected the continence care practices at The Hillcrest in two ways. First, although job turnover was not uncommon among the CNAs and ancillary department workers, the professional staff was loyal, which brought stability to the organization. Secondly, with their strong belief in the organizational mission, members of the interdisciplinary team worked together to achieve organizational excellence in resident care.
Organizational Stability.—
The former administrator was in her position for three decades prior to retirement. During that time, the nursing home administrator actively cultivated an environment based upon organizational stability. Turnover was “low and slow,” which allowed long-tenured nursing staff to develop an awareness of residents’ elimination patterns and care preferences. Staff prioritized their workflow to meet those needs. Residents rarely were asked to wait to use the restroom, as a nurse or aide either toileted the individual herself or found another person to assist.
Leadership development also brought about organizational stability. The administrator was an insightful “talent scout” who, according to one staff member, “could look at anyone and see who that person could be. Then she’d get to work until you could see that in yourself.” Employees attended college or became professionally certified through an organizational educational fund, which increased their expertise in geriatric care and commitment to the organization. Supervisors were promoted within the facility and in-house nurses and CNAs succeeded them into clinical leadership roles. These “homegrown experts” assured that key principles, policies, and procedures were applied in resident care.
Interdisciplinary Cooperation.—
Employees believed in the mission of The Hillcrest, which was caring for older adults. As one nursing assistant said, “My job is resident care. Whatever a resident needs, that is my job.” Leadership staff modeled the mission by answering call bells and assisting residents with activities of daily living, including toileting. The management team, clinicians, and ancillary staff were committed to providing excellent resident care. Employees believed that the facility was among the best in the nation and benchmarked their progress toward this goal. Staff enrolled in state and national quality improvement and safety initiatives and became leaders among facilities participating in these programs. One initiative disseminated evaluation tools designed or revised by The Hillcrest interdisciplinary staff.
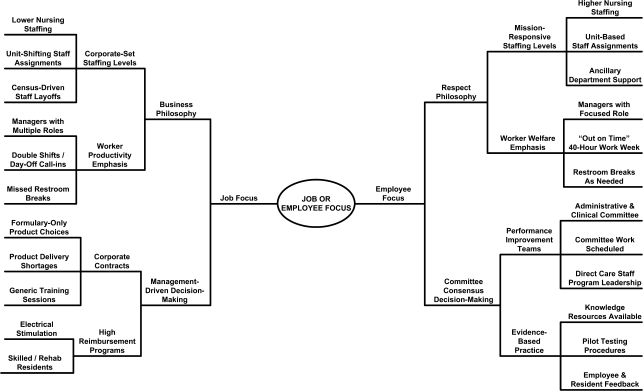
Job- or Employee-Focused Cultures
This dimension balances job-focused cultures that prioritize work tasks with employee-focused cultures that assure worker welfare. Organizational philosophy related to staffing, productivity, and decision making influenced continence care at these facilities (Figure 3).
Figure 3.
Impact of job or employee focus on continence care practices in nursing homes.
Continence Care in a Job-Focused Culture.—
Hidden Valley was one facility in a national for-profit elder care corporation. The board of directors codified its expectations in a mission statement that declared business units would achieve operational and clinical excellence by reducing costs, improving efficiency, and delivering exceptional shareholder returns. Resident care was framed within this business philosophy and its management-driven decision making.
Business Philosophy.—
The business philosophy of Hidden Valley emphasized corporate staffing policies. The maximum staffing level for CNAs was set at less than 2 hr per resident per day or 45 min below expert recommendations (Harrington et al., 2000). CNAs worked varying shifts and moved between units, which negatively affected their knowledge of residents’ care preferences. CNAs and ancillary staff worked part-time hours and had temporary layoffs during low census. At these times, paperwork was misplaced, supplies were not delivered, and Minimum Data Set (MDS) data were unavailable. The Tea Time program also faded away due to staffing shortages.
Business philosophy maximized worker productivity. Salaried staff worked long hours and covered multiple roles. The DON or ADON spent 2–3 hr each day phoning staff to fill open shifts, leaving little time for program planning or evaluation. Employees worked double shifts, were called in on days off, and did not receive rest breaks. CNAs expressed frustration when they could not take restroom breaks and linked their own lack of toilet time to resident care. As one aide said, “I’d like to be able to take every resident to the bathroom as soon as they need to go. But I cannot get to everyone. Today there wasn’t enough staff for me to pee.”
Management-Driven Decisions.—
Management-driven decision-making practices were related to corporate contracts or programs with high reimbursement levels, such as skilled care. Administrative staff reported that they had little input into programmatic decisions but, rather, learned about many policy changes through corporate e-mail messages or conference calls. In addition, corporate contracts restricted resident and staff choices to formulary products with low per unit costs. For example, the DON learned about a contract with a different supplier during a conference call less than a week before the new briefs were delivered. Impromptu trainings were scheduled and the DON assigned CNAs to act as resource people for briefs they had not selected or used before. Aides then were assigned the task of informing residents that these new briefs were “extra absorbent” and “could be urinated into many times” between changes. The CNAs stated that residents objected to this infrequent changing schedule, but that the contract-based policy was not discussed further or revised for individual resident preferences.
Continence Care in an Employee-Focused Culture.—
The Hillcrest philosophy included among its tenets respect for the dignity and self-worth of residents and staff. Toward this ideal, administrators engaged in organizational practices that maximized worker welfare within the financial constraints of a not-for-profit facility. Although few employees received health, disability, or retirement benefits, most agreed that The Hillcrest was a “good place to work,” as the respect philosophy supported worker-friendly practices and decision-making was built on consensus.
Respect Philosophy.—
Staffing patterns at The Hillcrest were based upon the mission of the organization, which was to provide quality care. CNAs were staffed slightly above the national average of 2 hr and 18 min per resident per day (CMS, 2004). The facility employed many ancillary personnel, such as unit clerks and staff schedulers, to complete clerical tasks so nursing staff could focus on resident care. Nurses and aides were assigned to units where their skills and preferences matched resident needs. Worker welfare was emphasized by scheduling practices that assured both salaried and hourly employees were “out on time” and not working overtime. Staffing levels and teamwork assured that employees could take timely restroom and lunch breaks while making sure enough nurses and aides were available for resident care.
Consensus Decision-Making.—
Consensus was important to decision-making processes and knowledge building at The Hillcrest. Performance improvement teams composed of managers, professionals, and direct care staff were convened around clinical issues, such as the implementation of a prompted voiding protocol. Schedules allotted time for meetings and assignments. Employees accessed the in-house library and Internet for research. Procedures were piloted and revised based upon resident and staff feedback. Direct care workers took on program leadership to sustain initiatives. A rehab aide managed the incontinence management system, completing protocol-based assessments, consulting on resident problems, and ordering products 8 hr each month. Staff suggested program changes through these leaders, who brought concerns back to the team for further revision.
Discussion
Inadequate knowledge and staffing, employee attitudes, and ineffective leadership are cited often as reasons why employees fail to implement best practices for continence care in NHs (DuBeau, Ouslander, & Palmer, 2007; Lekan-Rutledge, Palmer, & Belyea, 1998; Resnick et al., 2006). Many authors contend that the best solutions for affecting incontinence in this setting may be initiatives from the external environment, such as clinical guidelines, standardized assessments, quality assurance programs, regulatory enforcement, and financial inducements (Landefeld et al., 2008; Lawhorne et al., 2008; Ouslander & Johnson, 2004; Schnelle, Ouslander, & Cruise, 1997). An alternate position explored in this qualitative study is that an understanding of the social, cultural, and organizational contexts of health care practices must precede efforts to change provider behavior and service delivery processes within a health system (Tripp-Reimer & Doebbeling, 2004).
The findings from this research offer new insights on the cumulative and enduring impact of organizational culture on the treatment of incontinence in LTC settings. This study is among the first to explore continence care in relation to its organizational context and to observe this single resident care practice over an extended period of time and in more than one setting. A novel use of the theoretical framework of Hofstede and Hofstede (2005) supported the comparison of continence care practices in two NHs along three established dimensions of organizational culture. By investigating incontinence as a sociocultural and organizational process, our customary explanations for poor quality continence care shift into unfamiliar territory. We learn how the mundane task of helping a person empty his or her bladder and bowels in a manner that is considered socially acceptable underscores the collective beliefs, unspoken rules, and cultural norms operating among people associated with an organization.
In this study, human relations–related dimensions of organizational culture created the conditions by which distinctive continence care environments were sustained in two different NHs. Stakeholders’ maintenance of open or closed social systems, their emphasis on parochial or professional employee identity, and the focus on either task completion or worker welfare in staff interactions helped to determine which incontinence treatments were possible in a particular facility. Institutional philosophy, time orientation, admissions policies, employee career goals, organizational turbulence, interdisciplinary team interactions, and decision-making processes were newly identified factors that influenced continence care practices in these two NH settings.
This research extends findings from two case studies that delved into the role of the organization in the treatment of incontinence in elder care settings. Taunton and colleagues (2005) reported that staff definitions, program priorities, practice standards, and worker attitudes influenced incontinence treatments among interdisciplinary staff in three NHs in the United States. In contrast, professional boundaries, receptivity to change, leadership styles, and regard for individualized care shaped continence care among staff in two geriatric rehabilitation centers in Ireland (Wright et al., 2007). Those studies, however, summarized findings, which obscures our understanding of how organizational culture uniquely contributes to the widening disparities in incontinence rates and continence care quality in LTC settings.
By comparing organizational practices across NHs and along the same cultural dimensions, care processes are revealed as expressions of the philosophies, values, and goals of stakeholders. Wright and colleagues (2007) noted the importance of professional boundaries, but did not elaborate upon how boundary issues affected continence care differently in the facilities they studied. In the present study, boundary concerns were related to employee identity. Within the professional culture of Hidden Valley, where many workers focused upon their own career goals, professional boundaries were a major source of interdisciplinary conflict. Turf battles between the nursing and therapy departments hindered the implementation of toileting programs, whereas staff resignations or firings left leadership gaps that diminished program sustainability. In the parochial culture of The Hillcrest, managers made commitments to the organization. These employees modeled the importance of interdisciplinary cooperation as a means of achieving excellence in resident care. The shared values of cooperation and excellence allowed employees from nursing, therapy, health records, purchasing, environmental services, and administration to work together to perfect resident care processes, such as the incontinence management system.
The findings also broaden those of a recent descriptive study of continence care processes in LTC settings. Lawhorne and colleagues (2008) reported insignificant differences on the MDS toileting quality indicators in 34 facilities from one for-profit NH chain. A key difference between good and poor performers was not typical facility-level factors (e.g., occupancy, staff turnover, guideline use, product costs), but rather the reported presence of a process improvement team for incontinence. Although PITs may allow staff to take systematic approaches to the documentation and delivery of continence care services, the current study suggests that not every NH upholds an organizational culture that supports a PIT.
At Hidden Valley, different dimensions of the organizational culture seemed to work at cross-purposes. Although the professional identity dimension encouraged new program start-ups by individual employees, the job-focused culture of the parent corporation promoted management-driven decisions and discouraged the local quality assurance committee from working together to improve care processes. A business philosophy that maximized worker productivity by staffing as few people as possible led to a time-pressured environment where staff had little opportunity to meet the basic needs of residents, much less foster collaboration on planning and evaluation projects. Staffing levels were so strained that employees could not take restroom breaks. Several workers noted the irony of trying to maintain resident toileting programs in an environment that did not allow staff enough time to empty their own bladders. The Hillcrest organizational culture was aligned more harmoniously with its institutional mission. Administrative practices structured worker time so staff delivered resident care per organizational procedures, received rest breaks, and participated in “PIT-team” meetings to develop, test, and revise organizational policies.
This study is not without its limitations. This project was conducted in only two NHs of the more than 16,000 LTC facilities in the United States (Jones et al., 2009). The facilities were located in a micropolitan city in the Midwest and reported bed sizes and resident censuses above the national average. In addition, the baseline incontinence rates among residents were relatively divergent, not all workers (i.e., physicians, environmental services staff) involved in continence care were represented, and the selected facilities could be viewed as somewhat extreme examples of NHs. Given the small sample and its deviations from “typical” NHs, how can these findings inform a broader understanding of continence care in NHs everywhere?
An important lesson to take away from this study is that organizational culture matters. In one small community where residents and employees shared similar sociocultural backgrounds, NH stakeholders fashioned and sustained facilities with vastly different organizational cultures. These cultures, in turn, supported the implementation of different continence care interventions in each facility. One might look at these findings, point a finger, and proclaim that one NH provided “the best” continence care. However, the continence care practices in these NHs were far from the idealized goal of maximal bladder and bowel health for all LTC residents. Although the open systems of Hidden Valley created space for a diverse group of people with complex medical conditions, the time-buying containment strategies preferred by staff placed residents at risk for treatment-related complications. Similarly, although the closed system approach favored by The Hillcrest enabled staff to toilet residents using a time-driven treatment hierarchy, the selective admissions practices on which this hierarchy was based excluded many.
Is there an ideal NH culture that might support equitable and high quality programs for all residents and all residents’ needs? What organizational structures might support best practices for toileting, feeding, dressing, grooming, social activities, medical care, family interactions, and spiritual well-being of persons living in NHs? From this study, the ideal NH culture appears to be that which most closely aligns the organization’s practices with its institutional mission. For the Hidden Valley and The Hillcrest NHs, gaps in continence care practices emerged in the inconsistencies between the explicit and tacit missions of the facilities and in the tangible and intangible organizational structures created by its stakeholders. Future studies incorporating participatory methods are needed to explore the processes through which interdisciplinary teams, residents, and other stakeholders learn to recognize the strengths and limitations of their organizational cultures and to make informed decisions about which administrative and resident care practices to adopt, given those strengths and limitations. Such information could influence how and why people associated with NHs create, change, and sustain evidence-based practices for persons living in this setting.
Funding
This work was supported by the National Institutes of Health National Institute of Nursing Research (NR007058, NR008081, NR007091), Sigma Theta Tau International—Gamma Chapter, The University of Iowa College of Nursing, The University of Iowa Graduate College, and The University of Iowa College of Nursing John A. Hartford Center of Geriatric Nursing Excellence.
Acknowledgments
I want to express my appreciation to the NHs that served as the settings for this research and to offer my gratitude to all the people who participated in this study. My thanks to K Reeder for her thoughtful critiques. Thanks also to Barbara Mark and Shoou-Yih Daniel Lee for teaching me many new ways of looking at NHs as organizations. I thank Janet Specht, Meridean Maas, Keela Herr, and Robert Baller for their undivided support of this project. And I shall always be grateful to Toni Tripp-Reimer for her steadfast encouragement and insightful feedback throughout the research, writing, and rewriting process.
References
- Anderson R, Issel L, McDaniel R. Nursing homes as complex adaptive systems: Relationship between management practices and resident outcomes. Nursing Research. 2003;52:12–21. doi: 10.1097/00006199-200301000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services. Nursing Home Compare Nursing Staffing Measures. 2004. Washington, DC: U.S. Department of Health & Human Services. Retrieved July 7, 2004, from http://www.medicare.gov/NHCompare. [Google Scholar]
- Centers for Medicare and Medicaid Services. Nursing Home Compare. 2009. Washington, DC: U.S. Department of Health & Human Services. Retrieved March 21, 2009, from http://www.medicare.gov/NHCompare. [Google Scholar]
- Colon-Emeric C, Ammarell N, Bailey D, Corazzini K, Lekan-Rutledge D, Piven M, et al. Patterns of medical and nursing staff communication in nursing homes: Implications and insights from complexity science. Qualitative Health Research. 2006;16:173–188. doi: 10.1177/1049732305284734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crabtree B, Miller W. Doing qualitative research. Thousand Oaks, CA: Sage; 1999. [Google Scholar]
- DuBeau C. Improving urinary incontinence in nursing home residents: Are we FIT to be tied? Journal of the American Geriatrics Society. 2005;53:1254–1256. doi: 10.1111/j.1532-5415.2005.53366.x. [DOI] [PubMed] [Google Scholar]
- DuBeau C, Ouslander J, Palmer M. Knowledge and attitudes of nursing home staff and surveyors about the revised federal guidance for incontinence care. The Gerontologist. 2007;47:468–479. doi: 10.1093/geront/47.4.468. [DOI] [PubMed] [Google Scholar]
- Engberg S, Kincade J, Thompson D. Future directions for incontinence research with frail elders. Nursing Research. 2004;53:S22–S29. doi: 10.1097/00006199-200411006-00004. [DOI] [PubMed] [Google Scholar]
- Eustice S, Roe B, Paterson J. Prompted voiding for the management of urinary incontinence in adults. Cochrane Database of Systematic Reviews. 2000;(2) doi: 10.1002/14651858.CD002113. CD002113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fink H, Taylor B, Tacklind J, Rutks I, Wilt T. Treatment interventions in nursing home residents with urinary incontinence: A systematic review of randomized trials. Mayo Clinic Proceedings. 2008;83:1332–1343. doi: 10.1016/S0025-6196(11)60781-7. [DOI] [PubMed] [Google Scholar]
- Gubrium J. Living and dying at Murray Manor. New York: St. Martin’s Press; 1975. [Google Scholar]
- Harrington C, Kovner C, Mezey M, Kayser-Jones J, Burger S, Mohler M, et al. Experts recommend minimum nurse staffing standards for nursing facilities in the United States. The Gerontologist. 2000;40:5–16. doi: 10.1093/geront/40.1.5. [DOI] [PubMed] [Google Scholar]
- Hofstede G, Hofstede GJ. Cultures and organizations: Software of the mind. New York: McGraw-Hill; 2005. [Google Scholar]
- Jervis L. The pollution of incontinence and the dirty work of caregiving in a U.S. nursing home. Medical Anthropology Quarterly. 2001;15:84–99. doi: 10.1525/maq.2001.15.1.84. [DOI] [PubMed] [Google Scholar]
- Jirovec M. Effect of individualized prompted toileting on incontinence in nursing home residents. Applied Nursing Research. 1991;4:188–191. doi: 10.1016/s0897-1897(05)80096-5. [DOI] [PubMed] [Google Scholar]
- Johnson T, Ouslander J, Uman G, Schnelle J. Urinary incontinence treatment preferences in long-term care. Journal of the American Geriatrics Society. 2001;49:710–718. doi: 10.1046/j.1532-5415.2001.49146.x. [DOI] [PubMed] [Google Scholar]
- Jones A, Dwyer L, Bercovitz A, Strahan G. The National Nursing Home Survey: 2004 summary. Vital & Health Statistics. 2009;13 Retrieved August 7, 2009, from http://www.cdc.gov/nchs/data/series/sr_13/sr13_167.pdf. [PubMed] [Google Scholar]
- Kayser-Jones J. Old, alone, and neglected: Care of the aged in the United States and Scotland. Berkeley, CA: University of California Press; 1981. [Google Scholar]
- Kleinman A. Concepts and a model for the comparison of medical systems as cultural systems. Social Science & Medicine. 1978;12:85–93. doi: 10.1016/0160-7987(78)90014-5. [DOI] [PubMed] [Google Scholar]
- Landefeld C, Bowers B, Feld A, Hartmann K, Hoffman E, Ingber M, et al. National Institutes of Health state-of-the-science conference statement: Prevention of fecal and urinary incontinence in adults. Annals of Internal Medicine. 2008;148:449–458. doi: 10.7326/0003-4819-148-6-200803180-00210. [DOI] [PubMed] [Google Scholar]
- Lawhorne L, Ouslander J, Parmelee P. Clinical practice guidelines, process improvement teams, and performance on a quality indicator for urinary incontinence: A pilot study. Journal of the American Medical Directors Association. 2008;9:504–508. doi: 10.1016/j.jamda.2008.04.007. [DOI] [PubMed] [Google Scholar]
- Lekan-Rutledge D, Palmer M, Belyea M. In their own words: Nursing assistants’ perceptions of barriers to implementation of prompted voiding in long-term care. The Gerontologist. 1998;38:370–378. doi: 10.1093/geront/38.3.370. [DOI] [PubMed] [Google Scholar]
- Lincoln Y, Guba E. Naturalistic inquiry. Newberry Park, CA: Sage; 1985. [Google Scholar]
- Mather K, Bakas T. Nursing assistants’ perceptions of their ability to provide continence care. Geriatric Nursing. 2002;23:76–81. doi: 10.1067/mgn.2002.123788. [DOI] [PubMed] [Google Scholar]
- Ostaszkiewicz J, Johnston L, Roe B. Habit training for the management of urinary incontinence in adults. Cochrane Database of Systematic Reviews. 2004;(2) doi: 10.1002/14651858.CD002801.pub2. CD002801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouslander J, Johnson T. Continence care for frail older adults: It is time to go beyond assessing quality. Journal of the American Medical Directors Association. 2004;5:213–216. doi: 10.1097/01.JAM.0000126426.05045.18. [DOI] [PubMed] [Google Scholar]
- Ouslander J, Schnelle J, Uman G, Fingold S, Nigam JG, Tuico E, et al. Predictors of successful prompted voiding among incontinent nursing home residents. Journal of the American Medical Association. 1995;273:1366–1370. [PubMed] [Google Scholar]
- Palmer M, Johnson T. Quality of incontinence management in US nursing homes: A failing grade. Journal of the American Geriatrics Society. 2003;51:1810–1812. doi: 10.1046/j.1532-5415.2003.51570.x. [DOI] [PubMed] [Google Scholar]
- Rantz M, Hicks L, Grando V, Petroski G, Madsen R, Mehr D, et al. Nursing home quality, cost, staffing, and staff mix. The Gerontologist. 2004;44:24–38. doi: 10.1093/geront/44.1.24. [DOI] [PubMed] [Google Scholar]
- Remsburg R, Palmer M, Langford A, Mendelson G. Staff compliance with and ratings of effectiveness of a prompted voiding program in a long-term care facility. Journal of Wound, Ostomy and Continence Nursing. 1999;26:261–269. doi: 10.1016/s1071-5754(99)90056-6. [DOI] [PubMed] [Google Scholar]
- Resnick B, Keilman L, Calabrese B, Parmelee P, Lawhorne L, Pailet J, et al. Nursing staff beliefs and expectations about continence care in nursing homes. Journal of Wound, Ostomy and Continence Nursing. 2006;33:610–618. doi: 10.1097/00152192-200611000-00004. [DOI] [PubMed] [Google Scholar]
- Robinson J. Managing urinary incontinence in the nursing home: Residents’ perspectives. Journal of Advanced Nursing. 2000;31:68–77. doi: 10.1046/j.1365-2648.2000.01258.x. [DOI] [PubMed] [Google Scholar]
- Roe B, Watson N, Palmer M, Mueller C, Vinsnes A, Wells M. Translating research on incontinence into practice. Nursing Research. 2004;53:S56–S60. doi: 10.1097/00006199-200411006-00009. [DOI] [PubMed] [Google Scholar]
- Roper J, Shapira J. Ethnography in nursing research. Thousand Oaks, CA: Sage; 2000. [Google Scholar]
- Schein E. Organizational culture and leadership. San Francisco: John Wiley & Sons; 2004. [Google Scholar]
- Schnelle J, Cadogan M, Grbic D, Bates-Jensen B, Osterweil D, Yoshii J, et al. A standardized quality assessment system to evaluate incontinence care in the nursing home. Journal of the American Geriatrics Society. 2003;51:1754–1761. doi: 10.1046/j.1532-5415.2003.51560.x. [DOI] [PubMed] [Google Scholar]
- Schnelle J, Cadogan M, Yoshii J, Al-Samarrai N, Osterweil D, Bates-Jensen B, et al. The Minimum Data Set urinary incontinence quality indicators: Do they reflect differences in care processes related to incontinence? Medical Care. 2003;41:909–922. doi: 10.1097/00005650-200308000-00005. [DOI] [PubMed] [Google Scholar]
- Schnelle J, Ouslander J, Cruise P. Policy without technology: A barrier to improving nursing home care. The Gerontologist. 1997;37:527–532. doi: 10.1093/geront/37.4.527. [DOI] [PubMed] [Google Scholar]
- Scott-Cawiezell J, Jones K, Moore L, Vojir C. Nursing home culture: A critical component in sustained improvement. Journal of Nursing Care Quality. 2005;20:321–348. doi: 10.1097/00001786-200510000-00010. [DOI] [PubMed] [Google Scholar]
- Smith D. The culture of long-term care: Impact on a continence care program. Urologic Nursing. 1998;18:291–295. [PubMed] [Google Scholar]
- Tannenbaum C, Labrecque D, Lepage C. Understanding barriers to continence care in institutions. Canadian Journal on Aging. 2005;24:151–159. doi: 10.1353/cja.2005.0070. [DOI] [PubMed] [Google Scholar]
- Taunton R, Swagerty D, Lasseter J, Lee R. Continent or incontinent? That is the question. Journal of Gerontological Nursing. 2005;31:36–44. doi: 10.3928/0098-9134-20050901-08. [DOI] [PubMed] [Google Scholar]
- Tripp-Reimer T, Doebbeling B. Qualitative perspectives in translational research. Worldviews on Evidence-Based Nursing. 2004;1:S65–S72. doi: 10.1111/j.1524-475X.2004.04041.x. [DOI] [PubMed] [Google Scholar]
- Watson N, Brink C, Zimmer J, Mayer R. Use of the Agency for Health Care Policy and Research Urinary Incontinence Guideline in nursing homes. Journal of the American Geriatrics Society. 2003;51:1779–1786. doi: 10.1046/j.1532-5415.2003.51564.x. [DOI] [PubMed] [Google Scholar]
- Wright J, McCormack B, Coffey A, McCarthy G. Evaluating the context within which continence care is provided in rehabilitation units for older people. International Journal of Older People Nursing. 2007;2:9–19. doi: 10.1111/j.1748-3743.2007.00046.x. [DOI] [PubMed] [Google Scholar]
- Wyman J, Bliss D, Dougherty M, Gray M, Kaas M, Newman D, et al. Shaping future directions for incontinence research in aging adults. Nursing Research. 2004;53:S1–S10. doi: 10.1097/00006199-200411006-00001. [DOI] [PubMed] [Google Scholar]