Abstract
Behavior analysis is a generic science, and Skinner's vision for it was that it would become a mainstream force, relevant for most if not all human concerns, major and minor. Clearly his vision has not been realized. Determining why this is the case would require a complex multifactorial analysis. One likely factor is that the majority of its basic science findings have been obtained from the study of rats and pigeons. Another likely factor, one directly addressed by this paper, is that the majority of its applied science findings have been obtained from the study of people in only one tail of the normal distribution. Regardless, those outside the field see the relevance of behavior analysis to general human affairs as very limited. Whether the path behavior analysis is on will lead to widespread perception of mainstream relevance anytime soon seems doubtful. An alternative route would involve integrating it with a field that has already made the trip successfully. A premier example involves primary medical care. This paper argues for the integration of behavior analysis with pediatric primary care, sketches a method for its accomplishment, and uses diurnal enuresis to illustrate the requirements of the method.
Keywords: behavior analysis, pediatrics
Skinner's vision of behavior analysis was that it would become a mainstream science relevant to all aspects of human behavior and that it would be harnessed to improve the human condition substantively. Alas, that vision has yet to materialize. This is not to say behavior analysis has not contributed. On the contrary, behavior analysis has flourished in one tail of the distribution of human concerns. For example, merging behavior analysis with the philosophy of normalization (Wolfensberger, 1982) in the latter part of the 20th century substantially reduced the populations of most residential “treatment” facilities (i.e., institutions) for persons with severe developmental disabilities, thus allowing them a chance at a more normalized, satisfactory, and productive life. When used, behavior-analytic treatments have in many cases eliminated and, in most cases, significantly reduced the disfiguring and sometimes life-threatening self-injurious behavior exhibited by persons with developmental disabilities. Behavior-analytic treatments have proven to be among the most effective of all methods used to address symptoms of autism spectrum disorders (ASD). In fact, mounting evidence suggests that using intensive behavior-analytic methods with very young children with ASD can normalize their development. There are multiple other examples of the effectiveness of behavior analysis. However, even though these accomplishments are impressive, sometimes to the point of seeming miraculous, they have been achieved with a population whose problems are far removed from the concerns of people in the mainstream of everyday life. To attain mainstream relevance, behavior analysis will have to continue not only to produce results helpful for people in the one tail of the distribution, it will have to produce, more frequently and vigorously, results that are helpful for persons and problems that are under the dome of the distribution.
I realize this is a very tall order. Other forms of psychology do much less and yet obtain abundant mainstream attention. In fact, most forms of psychology do little scientific work in the area of intervention, even when their primary predicates include intervention. For example, the contents of flagship journals, such as the Journal of Clinical and Consulting Psychology, the Journal of Pediatric Psychology, or even Behavior Therapy, typically yield small ratios between papers that pertain to intervention and those that do not. I cannot remember the last time the Psychological Review provided an actual review of an area of intervention or that the Psychological Bulletin provided a bulletin on intervention. It happens so infrequently that I no longer consult those journals for information on intervention.
In contrast, the applied dimension of behavior analysis, applied behavior analysis, is dedicated to intervention, and its flagship journal, the Journal of Applied Behavior Analysis (JABA), very rarely publishes a paper that does not pertain to intervention. But, consistent with the point made above, most of the papers involve people who reside in one tail of the normal distribution and, thus, applied behavior analysis and JABA share almost none of the mainstream light that shines on other forms of psychology. Although these forms of psychology do little in the area of intervention, they routinely study the concerns of people in the mainstream of everyday life. An abbreviated sample of these concerns includes confidence, morality, loneliness, success, self-esteem, sexual attraction, happiness, envy, jealousy, and personality. Behavior analysts look upon these popular constructs with a jaundiced eye (or worse, a supercilious smile), focus very little research on them, and then bemoan the fact that the mainstream of psychological thinking in the industrialized world has either left behavior analysis behind or up on the banks while pet issues from other approaches to psychology bob merrily down the middle.
Does this mean that to enter the mainstream behavior analysis must abandon some of its core principles? Does it mean that behavior analysis must now begin to mimic the mostly correlational analyses of popular hypothetical constructs that densely populate the flagship journals of other forms of psychology? The answer to both questions is a firm denial. To achieve mainstream status, behavior analysis needs to compromise neither its principles nor its practices. A much more practical and efficient way to enter the mainstream is to integrate with a field that is already there. One that is essentially up for grabs, so to speak, is primary care medicine. Successfully integrating with primary care would require no new conceptual tools, no new scientific discoveries; in fact, it could be accomplished with two or three principles of behavior and a handful of applications. Below I will explain further and, because my area of interest is pediatrics, I will use pediatric primary care as my illustration, but I could easily have used internal medicine, family practice, or geriatrics. In particular, I will focus on child behavior problems in primary care.
CHILD BEHAVIOR PROBLEMS IN PEDIATRIC PRIMARY CARE
There is a skewed idea of child normality in this country. Unfortunately, normal has come to mean problem free. Picture the Gerber baby or any widely distributed photograph of babies, young children, or even teenagers. The children that make it to center stage (e.g., magazine covers, television programs, advertising campaigns, movies; venues seen by all) are the perfect or near-perfect ones. The ubiquity of images of perfect or near-perfect children gives rise to the mistaken notion that these images accurately depict how normal children look and act. As another example, consider any movie or television series that involves children rated G or PG. The children in these movies and series are always very attractive physically and socially, they are emotionally mature (often more so than the adults who surround them), confident, funny, engaged, and engaging. These ubiquitous depictions powerfully yield widespread, but woefully mistaken, notions about child normality: essentially that normal means problem free. However, as anyone who studies, works with, or has children quickly and often painfully comes to know, these notions are very far removed from the truth.
This is not to say there are not problem-free children; there probably are, but certainly they should not be thought of as the standard bearers of normality. Above I mentioned that applied behavior analysts spend most of their time with people in one tail of the normal distribution. These problem-free kids are in the other tail. Neither group is normal; both are deviant in the statistical sense of the term. Because of this bogus notion of normality, our culture is not well equipped to help normal kids; kids with problems that are tough for parents but that do not rise to the level of clinical significance and so do not qualify for professional help (at least not the kind of help covered by insurance).
Those Pesky 3-Year-Olds
For example, some influential research has ranked the behavior problems of 3-year-old children in terms of how bothersome and difficult the problems are for the parents. A representative list, derived from the classic paper by Richman, Stevenson, and Graham (1975) is in Table 1 (also see Earls, 1980, for a replication). I will summarize briefly here: pooping, peeing, pouting, pushing, pestering, perturbing, poking, procrastinating, picking, puking, and a few other problems that cannot be labeled with words beginning with the letter p. When child behavior problems are spoken of in this slightly facetious way, they sound pretty normal for such young children, because they are. They are not pathologies in 3-year-olds; they are developmentally expected skill deficits. That does not make them easy to solve, however. They can daunt even the most astute parents, which is why they are on the list. Yet, as I pointed out above, because they are not pathologies, parents are pretty much on their own when trying to solve them. True, they try to (and sometimes actually do) get help from their family doctor (the limits of which I will mention below), but mostly they use tactics that are freely available to nonprofessionals in the western hemisphere. A reasonably comprehensive list includes ignoring, warning, yelling, spanking, rewarding, reasoning, placating, and indulging. Use of these requires no professional assistance; everyone has access to them and, it seems safe to say, most parents use all or just about all at one time or another.
Table 1.
Parent-ranked behavior problems in 3-year-old children
Vast Unmet Behavioral Needs
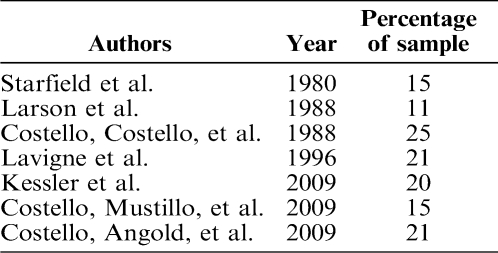
So how well do these tactics work for these common problems exhibited by these pesky 3-year-olds? From a persnickety adult's perspective (one prone to scowling while saying such things as “these kids today”), it might look as if these freely available tactics do not work so well. A more precise way of answering this question, and yet used here for mostly heuristic purposes (not to be mistaken for an accurate epidemiological estimate), involves the “rule of thirds” (i.e., a third changes in one direction, a third remains the same, the final third changes in a direction opposite of the first). Mysteriously, this rule of thirds shows up in multiple fields that manipulate independent variables to bring about change (e.g., Beahrs, Theuerkauf, & Hill, 1973), but the best known example involves its appearance in early evaluations of the effectiveness of psychotherapy (e.g., Smith, Glass, & Miller, 1980). Using these evaluations as a basis, I estimate that behavior problems of one third of 3-year-olds to whom the freely available tactics applied improve, one third stay the same, and one third get worse. This discussion will not involve children in the first two thirds; for their sake, I will assume they live happily ever after. But what happens to the third that gets worse? Apparently they land on other, much more alarming, lists such as the one in Table 2, a list of epidemiological surveys of unmet mental health needs of children in the United States. Although there are various ways these surveys select children, they use most frequently criteria specified in the Diagnostic and Statistical Manual of Mental Disorders of the American Psychiatric Association (DSM-IV; APA, 1994). According to this list, between 11% and 25% of all the children in the United States have at least one diagnosable mental health problem for which they are receiving few or no services. The Surgeon General of the United States has provided consonant estimates of this problem, specifically that 20% of children in the United States have a diagnosable mental health problem or addictive disorder (U.S. Department of Health and Human Services, 1999).
Table 2.
Surveys of unmet child mental health needs
Success Results from Finding a Need and Filling It
A time-honored maxim for developing a successful business is to find a need and fill it. The children on the Table 2 list represent an unmet need. A central assumption of this paper is that behavior analysts have the tools to meet that need. Risking redundancy (because I mentioned this above) and oversimplification, I assert that a significant portion of the need could be met with two to three principles of behavior and handful of applications (e.g., Blum & Friman, 2000; Christophersen, 1982; Friman, 2005, 2008b; Friman & Blum, 2003). Furthermore, the size of the unmet need places it away from the tail of the normal distribution where most applied behavior analysis is conducted and toward the large area under the dome. In other words, the statistical location of the unmet need within the normal distribution moves it toward the mainstream and, thus, by addressing it, behavior analysts would move toward the mainstream too. They would merely need a locus where they could proffer their services; primary medical care, if not an ideal locus, is certainly a suitable one.
PRIMARY CARE PEDIATRICS
By its broadest goals, medical care is subdivided into three domains, primary care with the broad goal of prevention, secondary care with the broad goal of cure, and tertiary care with the broad goal of rehabilitation. Clearly there is overlap among domains. For example, early cure of a high-frequency low-intensity problem such as urinary tract infection can prevent a low-frequency high-intensity problem such as kidney failure from occurring later. The reason I am touting primary care in this paper is because all children in the United States have a primary care doctor. For brevity's sake I will refer to them as pediatricians, although many general and family practitioners also serve in this capacity. In other words, primary care medicine is not only in the mainstream, in terms of pediatric medicine, it is the mainstream. All children receive services there, both the pesky 3-year-olds whose problems are listed in Table 1 and the more seriously troubled children surveyed in the studies listed in Table 2.
Hey, These Kids Are Not Sick
Adding even more weight to my point is that as many as half of all pediatric primary care visits involve behavioral rather than medical problems. Surveying their waiting rooms, pediatricians frequently discover, much to their dismay, that many of the waiting children are not sick, they are merely misbehaving. This is not surprising. Pediatricians have long been the first professionals to whom parents express their concerns about their children's behavior problems (Clarke-Stewart, 1978). In fact, child behavior problems are so common in primary care that they have been described as “the new hidden morbidity” (Costello, Edelbrock, et al., 1988) Primary care has also been described as the “de facto US mental health services system” (Regier, Goldberg, & Taube, 1978) and pediatricians as the “gatekeepers” (Costello, Burns, et al., 1988).
Why Don't Pediatricians Fix These Problems?
There are two fundamental answers to this question. The first involves limited time. Historically, average pediatric visits have been short, between 11 and 15 min (e.g., Bergman, Dassel, & Wedgewood, 1966). Recent research shows that there has been a slight increase, but the average is still only about 16 min (Merline, Olson, & Cull, 2009). Although behavior problems brought to primary care may not always be highly complicated, it likely takes more than 16 min to solve even simple ones. Furthermore, pediatricians allocate little time to behavioral concerns (Reisinger & Bires, 1980) and focus mostly on medical issues even when behavioral problems are clearly present (Lavigne et al., 1993). The second reason involves training. Pediatricians are primarily medically trained (which is exactly as it should be); they are not specifically trained to assess and treat diagnosable mental health problems. True, some pediatric residents may take an elective behavioral pediatric rotation, but these typically last only a month (e.g., Glasscock, O'Brien, Friman, Christophersen, & MacLean, 1989). Contrast that with the years of graduate school, practicum, and internship training required for licensed mental and behavioral health providers.
Why Don't Mainstream Mental Health Providers Fix These Problems?
There is one simple answer to this question. Parents are reluctant to seek mental health services for their children. Whereas medicine is very much in the mainstream of everyday life, psychotherapy is on the sidelines. This is partly due to the skewed idea of normality mentioned above. Because problem free is viewed as normal, having problems is viewed as abnormal; thus, seeking the services of a psychotherapist is to acknowledge one has problems and to suffer the prospect of the stigma of being abnormal. Unfortunately, this stigma, whether real or imagined, frequently deters people from seeking needed mental health services (Corrigan, 2004; Pescosolido, 2007). Another reason mental health services are avoided is that there is no standard of care beyond ethical. That is, as long as therapists behaves in an ethical way, they can pretty much do anything they want, call it therapy, and charge for it.
For example, despite the evidence-based practice movement, a recent provocative paper showed that most psychologists still do not use scientifically supported practices (Baker, McFall, & Shoham, 2009; see also Begley, 2009). In an accompanying editorial, Mischel (2009) recounted how the late Paul Meehl, in one of his last public speeches, noted that most clinical psychologists selected their methods like children making choices in a candy store—sampling a bit and choosing what feels good to them. This may make the psychologist feel good, but it is not likely to do much for the client. The stigma and variability in the quality of psychological care lend support for the caricatures of psychotherapists in movies and television. These therapist characters, with very few exceptions, are made to look like fools who have as many or more problems than their clients and who are virtually helpless to help themselves, not to mention those clients. For example, the psychologist character on the television series Bones is often hapless and clueless and made to look as if the only knowledge he possesses came from books, not experience. For these and multiple other reasons (e.g., insurance coverage, access) parents are reluctant to seek services from psychotherapists unless their need is great and alternatives are absent.
TARGETED HEALTH EDUCATION AND PRESCRIPTIVE TREATMENT
In adversity there is often opportunity and, although the gap between pediatric medicine and mainstream mental health care is a problem for afflicted children and their parents, it is a real opportunity for professionals who can supply what this underserved population needs and wants; specifically, targeted health education and prescriptive treatment, both based on solid science (Blum & Friman, 2000; Friman, 2005, 2008b; Friman & Blum, 2003). A major point of this paper is that behavior analysts can deliver both, more about which I will say below. For now, note that primary care medicine and behavior analysis have something very important in common that apparently is not shared by mainstream mental health care: a scientific basis for practice.
Health education
Although health education is not a subject typically associated with behavior analysis, supplying it is entirely consistent with Skinner's career-long focus. He sought to teach the culture at large how to describe behavior, how it emerges and changes, and how knowing such things could be harnessed to improve the human condition. In the context of health education, the provider describes health-related behavior to the patient, how it emerges and changes, and how knowing such things can be harnessed to improve his or her condition. And, there are multiple examples of health education supplied from a behavior-analytic perspective (e.g., Friman, 1988; 2007; 2008a; Friman & Finney, 1990; Friman, Finney, Glasscock, Weigel, & Christophersen, 1986). Thus, although health education has not historically been an obvious or large focus in behavior analysis, demonstrably it could become one and would have to if behavior analysis were to successfully move into primary care.
There are several aspects of health-related behavior that need to be addressed in the delivery of health education, and some of the more obvious are description of the behavior, prevalence, prognosis, causes, correlates, differential diagnosis, relevant physiology, comorbidities, and diagnostic procedures. The latter aspect (physiology) is one that behavior analysis has mostly avoided over the years of its existence (but see Honig & Staddon, 1977, for early examples to the contrary) and yet, because primary care is a medical domain, physiology is a critically necessary consideration. In other words, for behavior analysts to enter successfully into primary care they must become reasonably conversant with the key physiological dynamics of behaviors they will offer to assess and treat. For example, if the concern involves headache, some knowledge of the physiology of pain will be needed. If it involves urinary incontinence, knowledge of the physiology of urination will be needed. If it involves fecal incontinence, knowledge of the physiology of defecation will be required. There are numerous other examples, including diurnal enuresis, that I will illustrate in the section below.
Prescriptive treatment
Prescriptive behavioral treatment is not entirely synonymous with applied behavior analysis, but it is consistent with it. If prescriptive behavioral treatment and applied behavior analysis were blood relatives, they would be at least siblings and quite possibly fraternal twins, with prescriptive treatment being the smaller of the two twins. Prescriptive treatment merely involves specific steps patients or their parents are to follow as they work to resolve the behavior problem of concern. Prescriptive behavioral treatment also complements and amplifies the benefits of health education. In fact, behaviorally oriented prescriptive treatment has been described as the ideal method for enhancing health education (Christophersen, 1985; Friman & Finney, 1990; Friman et al., 1986).
Returning to Skinner, his vision was for the basic science of behavior analysis to be harnessed and used to address problems afflicting humankind. The primary vehicle for that purpose was and is applied behavior analysis. Although applied behavior analysis in primary care has many sources, one of the first, as well as most productive and influential, is Edward R. Christophersen, an applied behavior analyst. In 1982 he edited a special issue of the prestigious Pediatric Clinics of North America devoted to what he called “behavioral pediatrics,” and his contribution, “Behavioral Pediatrics in Primary Care,” is a foundational document for that field. His paper discusses the behavior problems most frequently seen by pediatricians in primary care and supplies descriptions of behavior-analytic methods for addressing them in a prescriptive treatment program. It clearly depicts that two or three principles of behavior and a handful of applications can adequately supply the armamentarium necessary for successful behavioral pediatric practice. More generally, that paper, coupled with several other papers by Christophersen (e.g., Christophersen, Finney, & Friman, 1986) and others (e.g., Allen, Barone, & Kuhn, 1993; Blum & Friman, 2000; Friman, 2005, 2008b; Friman & Blum, 2003), provides a guide for merging behavior analysis with pediatric medicine. As a group, these papers supply a broad description of the field and a method for behavior analysts to enter it successfully. Rather than reiterate what has already been published on the subject, I refer readers to these papers and especially to Christophersen (1982) and Allen et al. To further illustrate health education and prescriptive treatment here, I will use one child behavior problem frequently seen in pediatric primary care settings.
DIURNAL ENURESIS: A CLASSIC EXAMPLE
I selected diurnal enuresis as my example for several reasons, foremost among which are its frequency, the extent to which health education and prescriptive treatment synergistically unite in its remediation, its response to treatment, and the surprisingly small body of empirically derived literature devoted to it. For these reasons, diurnal enuresis presents a classic example of how behavior analysis can contribute to primary care.
Health Education for Diurnal Enuresis
Recall that health education, in general, involves explaining how a particular area of health-related behavior emerges and changes and, in particular, involves specifics such as description, prevalence, prognosis, causes, correlates, differential diagnosis, relevant physiology, comorbidities, and diagnostic procedures.
Definition and description
Enuresis, the technical term for chronic urinary accidents after the conventional age of full toilet training, comes in three forms: nocturnal, diurnal, and mixed. The vast majority of cases are nocturnal and, correspondingly, most of the literature on enuresis is devoted to the nocturnal type. Nonetheless, enuresis cases that involve a diurnal component are a notable concern, especially in late preschool and early elementary school. The DSM-IV (APA, 1994) criteria for diurnal enuresis specifies that a child be at least 5 years of age and have two or more diurnal accidents a week over a period of at least 3 months that are not due to physiopathic variables. Although the pertinent literature is small, it strongly suggests that, for afflicted children, their caretakers, and teachers, diurnal enuresis is a justifiable cause of concern. Along with a risk of secondary psychological problems (discussed below), there are public health concerns associated with daytime wetting. For example, the increase in the prevalence of infectious disease (e.g., hepatitis, infectious diarrhea) seen in day-care settings and preschools over the past few decades has been partially attributed to the spread of bacteria through child incontinence (Berk & Friman, 1990).
Prevalence
Due to the limited research on diurnal enuresis, virtually all aspects of it are less understood than parallel aspects of nocturnal enuresis. This is true even for something as straightforward as prevalence. One reason is that, although the DSM-IV diagnostic criteria are clear, they may be too exclusive. For example, a 5-year-old who wets his bed once or twice per week poses no serious problem for himself or his family. But a 4-year-old boy who wets his pants at preschool once or twice per week may indeed pose problems for his teachers, parents, classmates, and himself. Yet the DSM-IV criteria would capture the former and not the latter case. Prevalence estimates for the two ages also vary widely. Most papers on enuresis as a general topic supply epidemiological information only for the nocturnal version. The most widely cited published estimate of troublesome daytime wetting between the ages of 5 (the cutoff age for the DSM criteria) and 7 years, whether it be strictly diurnal or mixed, is 0.5% to 2% of children (Blomfield & Douglas, 1956; also see Berk & Friman, 1990; Meadow, 1990). A slight majority of these cases are girls, as distinct from nocturnal enuresis, where a clear majority of cases are boys.
Prognosis
For most cases of diurnal enuresis, the prognosis is very good, especially with treatment. Yet even without treatment there is a high rate of remission of functional daytime wetting in middle school. Beyond middle school, daytime wetting is rare and usually associated with developmental disabilities, major psychiatric conditions, postpartum complications, or old age.
Causes, correlates, and differential diagnosis
There are multiple causes of diurnal enuresis, and they can be grouped into medical and functional categories. The literature subdivides the medical category into various types of infection, disease, and anatomical abnormalities. Although these medical conditions may all require behavioral interventions as part of a comprehensive treatment plan, the initial and primary management is medical. Despite the priority of medicine in treatment, some responsibility for delivering health education about medical causes must be taken by the behavior analyst in primary care.
The literature also subdivides the functional category, although there is much less agreement as to its components. Typically included are excessive urinary deferral, vaginal reflux, labial fusion, daytime frequency syndrome, giggle incontinence, stress incontinence, emotional stress, deficient functional bladder capacity, the unstable bladder of childhood, and idiopathic (“garden variety”) diurnal enuresis. There is strong evidence that genetics play a role. There is also a small, but increasing, amount of evidence that toileting practices (e.g., prolonged use of absorptive undergarments) plays a role. Behavior analysts are the primary source of these studies (e.g., Simon & Thompson, 2006; Tarbox, Williams, & Friman, 2004). More fully describing these causes is beyond the scope of this paper, but knowledge of them and the ability to describe them clearly to a layperson are critical tasks for the behavior analyst in primary care (for further information, consult Christophersen & Friman, 2010; Friman, 2007, 2008a).
Physiology of urination
Some knowledge of the physiology of urination is necessary to understand the mechanics of urinary incontinence and the logic behind treatment. A complex physiological system governs urination, and its central component is the bladder. The bladder is an elastic hollow organ resembling an upside down water balloon with a long narrow neck; it has two primary mechanical functions, storage and release of urine. Extended storage and timed intentional release into an appropriate receptacle are the defining properties of urinary continence. Contraction of the bladder walls and relaxation of the bladder neck precede elimination, but the body of the bladder is composed of smooth muscle and its nerve supply is autonomic. Therefore, the bladder cannot be controlled directly; one cannot “will” the bladder walls to contract or the neck to relax. The autonomic basis of bladder contraction and relaxation presents an apparent paradox, because the essence of complete continence is the exercise of personal control over bladder functions.
The paradox is resolved by other components of the urogenital system that actually can be directly controlled so that a child can learn to time and locate urination appropriately. These components include three large muscle groups, sometimes referred to as the pelvic floor muscles, including the thoracic diaphragm, lower abdominal musculature, and pubococcygeus (anterior end of the levator ani). Deliberate urination at all levels of bladder filling involves a coordination of these three muscle groups, resulting in intra-abdominal pressure directed to the bladder neck. This coordinated action relaxes and lowers the bladder neck, resulting in reflexive contractions of the bladder body, opening of its internal and external sphincters, and bladder emptying (Muellner, 1951, 1960; Vincent, 1974).
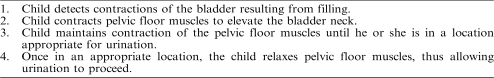
Urine retention generally involves a retrograded version this process (see Table 3). That is, except during imminent or actual urination, the pelvic floor muscles remain in a state of static partial contraction or tonus that maintains the bladder neck in an elevated position and sphincter muscles closed. Even after urination has begun, contraction of the pelvic floor muscles can abruptly raise the bladder neck and interrupt urine flow, but this requires some training and concentrated effort (Christophersen & Friman, 2010; Friman, 2007, 2008a). The capacity to terminate and reinitiate urination is a prerequisite for Kegel exercises, a treatment method discussed below.
Table 3.
Four physiological or anatomical steps to urinary control
A colloquial description of the physiologic process
As indicated implicitly and explicitly above, the behavior analyst must not only technically understand various aspects of the behavior problems that present in primary care, he or she will also need to be able to explain them in nontechnical terms (i.e., colloquial). The following is a colloquial description of how the physiology of urination operates. At the moment the captain of a commercial airliner announces to passengers that the “fasten seat belt” sign will soon be illuminated prior to landing, many passengers look towards the lavatories to determine whether they can be successfully used. A long line precludes their use, leaving the passengers' urinary urge unsatisfied and unsatisfiable in the short term. For most passengers in this situation, a collection of preventive physiological responses is initiated, typically with minimal or no conscious awareness. The responses include strategically using pelvic floor muscles to elevate the bladder neck and complete a “dry” Kegel exercise (see section below on Kegel exercises). Successful execution of the responses will typically allow the afflicted passengers to complete the flight, gather luggage, and in many instances get to their desired location prior to finding a bathroom and urinating successfully. In other words, the responses extend the passengers' capacity for continence well beyond the emergence of the urinary urge.
The role of awareness
Although the process used by the passengers with urinary urgency described above occurs largely beneath awareness, a cardinal variable in the behavioral approach to diurnal enuresis is awareness—awareness of bladder distension and incipient or actual bladder neck descent. The contradiction in this is illusory. Initial full awareness is instrumental in learning most complex skills (e.g., driving, dancing) but as facility and fluency increase, the need for awareness decreases. Bladder distension or descent sets the occasion for postural changes and limb movements suggestive of urinary urgency. The function of these movements is maintenance of bladder neck ascent. For example, when children scissor their legs or compress their thighs, the movements produce upward pressure on the bladder neck, thus preventing urination. These movements are much more overt and less subtle versions of the behaviors emitted by the airline passengers described above. As with those passengers, children are usually unaware of the movements and their functions. In successful toilet training, parents draw children's attention to the movements, thus elevating the children's awareness and promoting independent urinations. As we shall see, successful treatment of diurnal enuresis also elevates awareness of the process.
Comorbidities
As part of the delivery of health education, behavior analysts will often need to dispel misinformation pertaining to behavior problems that present in primary care. Unfortunately for afflicted children down through the ages, enuresis has been associated with a very large amount of misinformation, a significant amount of which involves the assumption of psychopathological causes and correlates. It is very important that behavior analysts address such concerns empirically and not ideologically. From an ideological perspective, concerns about psychopathology are moot in behavior analysis because the concept has no status in the field. Therefore, behavior analysts will usually have to consult literature outside behavior analysis to address questions of comorbidities. Regarding enuresis, the literature on underlying psychopathology is composed primarily of descriptive findings from uncontrolled examinations conducted more than 20 years ago. Although multiple sources attempt to attribute enuresis to underlying psychological causes (e.g., Sperling, 1994), none have provided data-based support (Christophersen & Friman, 2010; Friman, 2007, 2008a), and there is some clear data-based evidence to the contrary (Friman, Handwerk, Swearer, McGinnis, & Warzak, 1998).
However, enuresis itself could be the source of significant psychological distress, possibly leading to psychopathology. Diurnal enuresis has a public presentation that extends beyond the family. Because of the extent to which modern culture reviles incontinence after a certain age, psychological stressors such as increased social distance and reduced social standing emerge in the lives of afflicted children. For this reason, it is surprising that comorbidity and diurnal enuresis have received so little scientific attention, especially in contrast with the abundant attention paid to nocturnal enuresis and comorbidity. In part, this scientific gap reflects the more general differential between scientific interest in nocturnal versus diurnal enuresis. The scientific literature on the former is vast, but literature on the latter is scant (a hint for the behavior-analytic researcher interested in primary care).
Diagnostic procedures
Despite the fact that the majority of cases of diurnal enuresis are not associated with any medical causes, the seriousness of the minority that do requires that all afflicted children receive a medical evaluation to rule out such causes—prior to the inauguration of behavioral treatment—which begins with behavioral diagnostics. The important behavioral diagnostic procedures for diurnal enuresis involve (a) screening for other behavioral or psychological problems that may complicate treatment (e.g., oppositional behavior) or that may also require treatment (e.g., attention deficit hyperactivity disorder); (b) establishing toileting readiness (e.g., pincer grasp, ambulation, instructional control, independent sitting); (c) determining prevailing parent opinions, approaches, and practices; (d) determining prevailing child opinions, approaches, and practices; and (e) systematic “pants checks” by the parent on the child. There are two functions for the checks, one for assessment and one for treatment. The assessment function involves determining the presence and size of urinary accidents. The treatment function involves setting the occasion for a parent to deliver a reward for dryness or corrective steps for an accident. The intervals between checks can range from every 5 min to once per day. I recommend beginning with hourly checks and reducing the frequency as success is achieved.
A less invasive measurement system involves parents checking their child's clothing once it has been removed for bed. This type of monitoring should be employed for assessment only; it should not initiate a treatment response because the time between the response and the accident may be so long that the child may not be able to form helpful associations. In either form of measurement, exact accident volumes will be difficult to establish but knowledge of exact volumes is not critical. Rather, it is merely necessary to determine whether a child's accidents involve dribbling or full bladder emptying.
PRESCRIPTIVE TREATMENT FOR DIURNAL ENURESIS
Alarm-Based Treatment
There are few published studies describing effective treatment of any sort, behavioral or nonbehavioral, for diurnal enuresis in typically developing children (once again, behavior-analytic researchers interested in primary care take note). Furthermore, the extant few did not appear until the 1980s (e.g., Halliday, Meadow, & Berg, 1987), which is puzzling because they used the urine alarm, and papers documenting the benefits of alarm-based treatment for nocturnal urine accidents have appeared regularly since the 1930s (e.g., Mowrer & Mowrer, 1938). The urine alarm involves a device with a moisture-sensitive switching system that attaches to bedding or pajamas. When a child wets, the switch closes and activates either a sound-based or vibrating alarm. Why it took almost 50 years to initiate tests of the alarm for diurnal enuresis is unknown, and to my knowledge, not even discussed in the literature (cf. Christophersen & Friman, 2010). Another puzzling issue, one directly pertinent to this paper, is that behavior analysts have been studying treatment for diurnal enuresis since the early 1970s but only in persons with developmental disabilities (e.g., Azrin, Bugle, & O'Brien, 1971). But the millions of typically developing children who exhibit diurnal enuresis need help too. In supplying that help, behavior analysts would be marking some territory in the mainstream.
The Halliday et al. (1987) study was a group trial using the urine alarm, and two thirds of the participants enrolled became dry. A systematic replication produced complete continence in a controlled case study of a 15-year-old girl with diurnal enuresis (Friman & Vollmer, 1995). A recent larger, although much less rigorous, study also systematically replicated the results of Halliday et al. The records of 63 children whose daytime wetting was treated with a urine alarm were examined and revealed that two thirds of the children achieved full dryness or substantial improvement (Van Laecke et al., 2006).
In sum, although late in arriving on the diurnal enuresis scene, a modest amount of empirical evidence that supports the use of the urine alarm is now published. Each of the existing three studies has limitations, however, and even when these studies are considered as a group, their collective findings are merely suggestive rather than definitive. Nonetheless, with one exception (mentioned below), alarm-based treatment is the only treatment approach to diurnal enuresis with substantive empirical support. Furthermore, recent advances in the technology of urine alarms could enhance their potential as a primary treatment for diurnal enuresis. A number of alarm makers now provide alarms that vibrate rather than emit noise, resulting in private but not public detection of accidents—a feature that could enhance the acceptability of the alarm as a treatment.
Kegel Exercises
The one additional treatment for diurnal enuresis with empirical support, albeit only from one study, involves the practice of Kegel exercises. These involve either starting and stopping urine flow during the act of urination (“wet practice”) or engaging the anatomical manipulations that are used to start and stop urine flow at times when urination is not occurring (“dry practice”). The lone study reported that training 79 day-wetting children to practice Kegel exercises at least three times a day eliminated accidents in 44 and substantively reduced them in another 9 (Schneider, King, & Surwitt, 1994).
DIURNAL ENURESIS: AN OPPORTUNITY FOR BEHAVIOR ANALYSIS
The previous section provides a complete description of the empirical treatment literature on diurnal enuresis. Contrast it with any review of treatment of nocturnal enuresis and it yields a large discrepancy. As indicated previously, the former is tiny and the latter is vast (e.g., Christophersen & Friman, 2010; Friman, 2007, 2008a). As discussed in the section on comorbidity, the public dimension of daytime accidents, and the resulting detrimental effect their detection can have on social distance, relations, and standing, would seem to supply more urgency for research on effective treatment. In the absence of clear empirically supported options, most primary care medical providers, the professionals that will almost always be the first to encounter diurnal enuresis in the child, are likely to use medication or unnecessarily intensive medical procedures. Unfortunately, medications used for treatment of diurnal enuresis have serious side effects, and intensive medical procedures have not been evaluated scientifically (Christophersen & Friman; Friman). This state of affairs may be frustrating for some, but it actually represents an excellent opportunity for behavior analysts in primary care. Primary care physicians would much prefer to prescribe treatments that pose less risk and have more scientific support. With such a diminutive literature, they do not have ready access to such treatments and, thus, their practice devolves to standard medical care. Behavior analysts could address this problem in at least two ways. One would be to do more research on treatment of diurnal enuresis and publish at least some of it in pediatric medical journals. Another would be to court collaboration with physicians that results in referrals of incontinent children to behavior analysts for treatment (cf. Allen et al., 1993; Christophersen, 1982). Below I will discuss some variations and combinations of treatments for diurnal enuresis and end with a representative behaviorally based treatment that can be prescribed in one or two clinic visits.
MULTICOMPONENT BEHAVIORAL TREATMENT
In contrast to the contemporary literature on treatment of nocturnal enuresis, which includes numerous empirical analyses of multicomponent treatments, the literature on diurnal enuresis includes no such analyses of multicomponent treatments for typically developing children, at least none I could find. As is the case with many types of child behavior problems, however, there are published accounts of multicomponent treatments for diurnal enuresis in persons with developmental disabilities (e.g., Azrin & Foxx, 1971). Presumably enuresis in this population would be much more difficult to treat, given the deficiencies in learning that define disability. If true (and I strongly suspect it is), this too presents an opportunity. Specifically, if behavior analysts can successfully treat diurnal enuresis in a population characterized by delayed development and learning deficiencies, surely they could successfully treat it in children who do not have these problems.
Put more plainly, diurnal enuresis is not a difficult problem to treat with behavioral methods. Its tiny empirical literature and the fact that it is all but untouched by behavior-analytic hands stand in stark contrast to how readily it responds to observational and contingency management methods. I have three bits of evidence to support this claim. First the tiny literature is one to which I have contributed (Friman & Vollmer, 1995). Second, the clinics in which I have worked have successfully treated hundreds of children. Failures are so unusual that they may qualify for anomalous case reports. Third, diurnal enuresis virtually disappears by middle school. Regarding this later point, some may say this is the result of development. Fine, but children do not unfold like a flower; their development occurs as a result of the dynamic between their behavior and environmental events. I submit that as the social consequences for diurnal accidents mount with the onset of adolescence, afflicted children who have not had the benefit of behavioral treatment take on the problem themselves, and do so successfully. So the point here is not whether behavior analysts can successfully treat diurnal enuresis; they can. It is a question of whether they will. In the event that after reading this article someone (anyone) decides to take on treatment of diurnal enuresis, the section to follow includes a representative, comprehensive treatment, and one that can easily be supplied in one or two clinic visits.
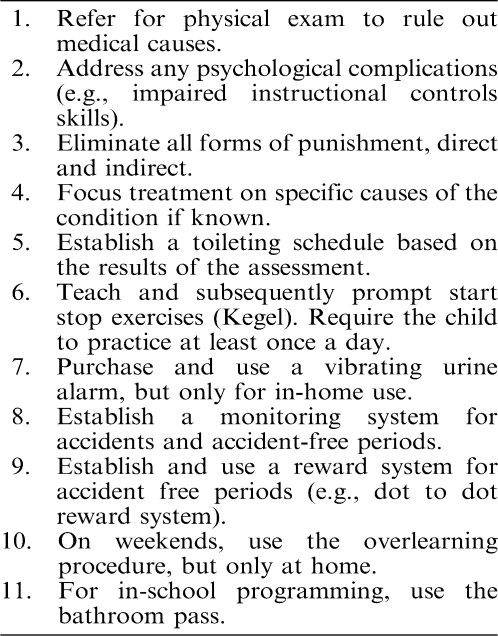
Representative Multicomponent Treatment
As with all problems that have a medical dimension, the medical causes of diurnal enuresis need to be identified and medically treated or ruled out by a physician before behavioral treatment ensues. In addition, major psychological complications need to be addressed prior to treatment. All forms of punishment, implicit and explicit, should be eliminated. Treatment should focus on known causes of urinary accidents that can be addressed with health education and behavioral treatment methods. Some cases may be resolved with only two components: health education about the condition and some condition-specific health recommendations. For example, a toileting schedule consistent with healthful urination patterns may be all that is needed for children who excessively defer urination. Teaching parents to teach their girls afflicted with vaginal reflux to more fully open the labia during urination can solve that problem. Girls who release urine during laughter can be taught to exhibit their response to humorous episodes in a more demure fashion. Unmotivated children can be placed on a motivational program. Providing counseling about stress management could resolve incontinence in children whose wetting accidents are associated with emotional stress.
For children whose urinary incontinence is more likely due to maturational factors (the majority of cases), the three likely causes are reduced awareness of urge, insufficient use of pelvic floor musculature, and low motivation. For these children, several components may be necessary for optimal outcomes. Treatment could begin with an assessment of the timing of urinations (accidents and successes) throughout the day. A toileting schedule linked to the outcome of the assessment could be established. Kegel exercises could be taught and subsequently used to increase pelvic floor involvement. A clothing-based urine alarm could be used to increase awareness of urinary urge and to cue the need for pelvic floor muscle manipulation. Because of its reduced social saliency, the vibrating alarm may be preferable to the sound-based alarm. It is difficult to imagine cases that would not benefit from a motivational component. However, the construction of the multicomponent program is important. Prior to contact with professionals, parents may be inclined to offer large incentives (e.g., bicycle, recreational electronics) for full continence. Unfortunately, such offers can actually have a detrimental effect on motivation. When full continence is the criteria for the incentive, one accident can reset the program to its starting point, thus actually adding existing costs to the problem for the child. To be optimally effective, incentive programs should provide children with the experience of success for small steps toward continence. An example involves a method using a dot-to-dot drawing. The child or parent draws a dotted picture of an item the child would like and one that the parents are willing to buy. For every accident-free day, he or she would connect one dot. Alternatives include allowing a dot for all successful dry pants checks or successful urinations in the toilet. When all the dots are connected, the parent buys the item and gives it to the child (e.g., Jenson & Sloane, 1979). This method allows parents to reward their incontinent child for small amounts of progress made on the way to continence and, thus, potentially to increase motivation.
On weekends, learning trials can be increased by allowing children to drink abundant amounts of their favorite beverages, sometimes referred to as overlearning (Christophersen & Friman, 2010). For children at risk for accidents in school, a classroom pass program can be used. In the program, the child is given a pass that allows him or her to leave class to use the bathroom without penalty (cf. Friman et al., 1999). To discourage abuse of the pass program, children can be provided small incentives for unused passes at the end of the school day. Finally, within the context of appropriate developmental expectations, children should be required to change their soiled clothing and take it to the laundry, sometimes referred to as responsibility training (Christophersen & Friman).
As discussed previously, multicomponent treatments drawn from these various components have yet to be empirically evaluated for diurnal enuresis. However, two likely core components—Kegel exercises and the urine alarm—have empirical support. The other components mentioned above are typically included in treatments for nocturnal enuresis, and evaluations of those programs have shown that, as the number of components increase, so too does the chance of success. Thus, for optimal treatment, I recommend including as many components that are related to the type of diurnal enuresis a child has that his or her parents are willing to implement and the child is willing to accept. In Table 4, I provide clinicians with a summary of a representative multicomponent treatment for diurnal enuresis.
Table 4.
Representative multicomponent treatment for diurnal enuresis
CONCLUSION
This final point, the one about how responsive diurnal enuresis is to behavioral treatment, reflects an obstacle to behavior analysts entering the mainstream of the primary care route and a concomitant opportunity. Regarding the obstacle, day-wetting in typically developing children may seem too trivial for behavior analysts, both in terms of its importance as a clinical target and its interest as a research target. More generally, most of the problems that first present in primary care may seem trivial as well (recall the list—pooping, peeing, pestering, etc.). These problems may seem especially trivial when they are compared with the types of problems that afflict people with developmental disabilities that behavior analysts routinely address. But the problems that first present in primary care are not trivial to the children who have them, the parents who have to contend with them, and the medical providers asked to treat them. These three groups of people are not just in the mainstream, they are the mainstream. Help them, and behavior analysts help themselves occupy the illusive but eminently available mainstream role that Skinner envisioned so long ago. The most strategic locus for delivering this help is one all children pass through at one time or another—pediatric primary care.
REFERENCES
- Allen K.D, Barone V.J, Kuhn B.R. A behavioral prescription for promoting applied behavior analysis within pediatrics. Journal of Applied Behavior Analysis. 1993;26:493–502. doi: 10.1901/jaba.1993.26-493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed.) Washington, DC: Author; 1994. [Google Scholar]
- Azrin N.H, Bugle C, O'Brien F. Behavioral engineering: Two apparatuses for toilet training retarded children. Journal of Applied Behavior Analysis. 1971;4:249–253. doi: 10.1901/jaba.1971.4-249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azrin N.H, Foxx R.M. A rapid method of toilet training the institutionalized retarded. Journal of Applied Behavior Analysis. 1971;4:89–99. doi: 10.1901/jaba.1971.4-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker T.B, McFall R.M, Shoham V. Current status and future prospects of clinical psychology: Toward a scientifically principled approach to mental and behavioral health care. Psychological Science in the Public Interest. 2009;9:67–103. doi: 10.1111/j.1539-6053.2009.01036.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beahrs O.H, Theuerkauf F.J, Hill J.R. Procidentia: Surgical treatment. Diseases of the Colon and Rectum. 1973;15:337–346. doi: 10.1007/BF02587407. [DOI] [PubMed] [Google Scholar]
- Begley S. Ignoring the evidence: Why do psychologists reject science? Newsweek. 2009 Oct 12;:30. [PubMed] [Google Scholar]
- Bergman A.B, Dassel S.W, Wedgewood R.J. Time-motion study of practicing pediatricians. Pediatrics. 1966;29:254–263. [PubMed] [Google Scholar]
- Berk L.B, Friman P.C. Epidemiological aspects of toilet training. Clinical Pediatrics. 1990;29:278–282. doi: 10.1177/000992289002900505. [DOI] [PubMed] [Google Scholar]
- Blomfield J.M, Douglas J.W.B. Bedwetting: Prevalence among children 4 to 7 years old. Lancet. 1956;1:850–852. doi: 10.1016/s0140-6736(56)91316-2. [DOI] [PubMed] [Google Scholar]
- Blum N, Friman P.C. Behavioral pediatrics: The confluence of applied behavior analysis and pediatric medicine. In: Carr J, Austin J, editors. Handbook of applied behavior analysis. Reno, NV: Context Press; 2000. pp. 161–186. [Google Scholar]
- Christophersen E.R. Incorporating behavioral pediatrics into primary care. Pediatric Clinics of North America. 1982;29:261–296. doi: 10.1016/s0031-3955(16)34141-4. [DOI] [PubMed] [Google Scholar]
- Christophersen E.R. Enhancing the effectiveness of health education strategies. Clinics in Perinatology. 1985;12:381–389. [PubMed] [Google Scholar]
- Christophersen E.R, Finney J.W, Friman P.C. Prevention in primary care. Pediatric Clinics of North America. 1986;33:no. 4. doi: 10.1016/s0031-3955(16)36081-3. [DOI] [PubMed] [Google Scholar]
- Christophersen E.R, Friman P.C. Encopresis and enuresis. Cambridge, MA: Hogrefe; 2010. [Google Scholar]
- Clarke-Stewart A. Popular primers for parents. American Psychologist. 1978;33:359–369. [Google Scholar]
- Corrigan P. How stigma interferes with mental health care. American Psychologist. 2004;59:614–625. doi: 10.1037/0003-066X.59.7.614. [DOI] [PubMed] [Google Scholar]
- Costello E.J, Angold A, Burns B.J, Stangl D.K, Tweed D.L, Worthman C.M. The Great Smoky Mountains study of youth: Goals, design, methods, and the prevalence of DSM-III-R disorders. Archives of General Psychiatry. 2009;53:1129–1136. doi: 10.1001/archpsyc.1996.01830120067012. [DOI] [PubMed] [Google Scholar]
- Costello E.J, Burns B.J, Costello A.J, Edelbrock C, Dulcan M, Brent D. Service utilization and psychiatric diagnosis in pediatric primary care: The role of the gatekeeper. Pediatrics. 1988;82:435–441. [PubMed] [Google Scholar]
- Costello E.J, Costello A.J, Edelbrock C, Burns B, Dulcan M, Brent D, et al. Psychiatric disorders in pediatric primary care. Archives of General Psychiatry. 1988;45:1107–1116. doi: 10.1001/archpsyc.1988.01800360055008. [DOI] [PubMed] [Google Scholar]
- Costello E.J, Edelbrock C, Costello A.J, Dulcan M.K, Burns B.J, Brent D. Psychopathology in pediatric primary care: The new hidden morbidity. Pediatrics. 1988;82:415–424. [PubMed] [Google Scholar]
- Costello E.J, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2009;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Earls F. Prevalence of behavior problems in 3-year-old children. Archives of General Psychiatry. 1980;37:1153–1157. doi: 10.1001/archpsyc.1980.01780230071010. [DOI] [PubMed] [Google Scholar]
- Friman P.C. Chronic thumb sucking: A threat to wellness in middle childhood. Wellness Perspectives. 1988;5:7–12. [Google Scholar]
- Friman P.C. Behavioral pediatrics. In: Hersen M, editor. Encyclopedia of behavior modification and therapy. Thousand Oaks, CA: Sage; 2005. (Vol. 2, pp. 731–739). [Google Scholar]
- Friman P.C. Encopresis and enuresis. In: Hersen (Ed. in Chief) M, Reitman (Vol. Ed.) D, editors. Handbook of assessment, case conceptualization, and treatment: Vol. 2. Children and adolescents. Hoboken, NJ: Wiley; 2007. pp. 589–621. [Google Scholar]
- Friman P.C. Evidence based therapies for enuresis and encopresis. In: Steele R.G, Elkin T.D, Roberts M.C, editors. Handbook of evidence-based therapies for children and adolescents. New York: Springer; 2008a. pp. 311–333. [Google Scholar]
- Friman P.C. Primary care behavioral pediatrics. In: Hersen M, Gross A, editors. Handbook of clinical psychology. New York: Wiley; 2008b. (Vol. 2, pp. 728–758). [Google Scholar]
- Friman P.C, Blum N.J. Primary care behavioral pediatrics. In: Hersen M, Sledge W, editors. Encyclopedia of psychotherapy. New York: Academic Press; 2003. pp. 379–399. [Google Scholar]
- Friman P.C, Finney J.W. Health education for testicular cancer. Health Education Quarterly. 1990;17:443–453. doi: 10.1177/109019819001700408. [DOI] [PubMed] [Google Scholar]
- Friman P.C, Finney J.W, Glasscock S.G, Weigel J.W, Christophersen E.R. Testicular self-examination: Validation of a training strategy for early cancer detection. Journal of Applied Behavior Analysis. 1986;19:87–92. doi: 10.1901/jaba.1986.19-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friman P.C, Handwerk M.L, Swearer S.M, McGinnis C, Warzak W.J. Do children with primary nocturnal enuresis have clinically significant behavior problems? Archives of Pediatrics and Adolescent Medicine. 1998;152:537–539. doi: 10.1001/archpedi.152.6.537. [DOI] [PubMed] [Google Scholar]
- Friman P.C, Hoff K.E, Schnoes C, Freeman K, Woods D, Blum N. The bedtime pass: An approach to bedtime crying and leaving the room. Archives of Pediatrics and Adolescent Medicine. 1999;153:1027–1029. doi: 10.1001/archpedi.153.10.1027. [DOI] [PubMed] [Google Scholar]
- Friman P.C, Vollmer D. Successful use of the nocturnal urine alarm for diurnal enuresis. Journal of Applied Behavior Analysis. 1995;28:89–91. doi: 10.1901/jaba.1995.28-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasscock S.G, O'Brien S.O, Friman P.C, Christophersen E.R, MacLean W.E. Residency training in behavioral pediatrics. Journal of Developmental and Behavioral Pediatrics. 1989;10:262–263. [PubMed] [Google Scholar]
- Halliday S, Meadow S.R, Berg I. Successful management of daytime enuresis using alarm procedures: A randomly controlled trial. Archives of Diseases in Children. 1987;62:132–137. doi: 10.1136/adc.62.2.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honig W.K, Staddon J.E.R. Handbook of operant behavior. Englewood Cliffs, NJ: Prentice Hall; 1977. [Google Scholar]
- Jenson W.R, Sloane H.N. Chart moves and grab bags: A simple contingency management. Journal of Applied Behavior Analysis. 1979;12:334. [Google Scholar]
- Kessler R.C, Berglund P, Demier O, Jin R, Walters E.E. Life-time prevalence and age of onset distribution of DSM-IV disorders in the national co-morbidity survey replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Larson C.P, Pless I.B, Miettinen O. Preschool behavior disorders: Their prevalence in relation to determinants. Journal of Pediatrics. 1988;113:278–285. doi: 10.1016/s0022-3476(88)80265-8. [DOI] [PubMed] [Google Scholar]
- Lavigne J.V, Binns H.J, Christoffel K.K, Rosenbaum D, Arend R, Smith K, et al. Behavioral and emotional problems among preschool children in pediatric primary care: Prevalence and pediatricians' recognition. Pediatrics. 1993;91:649–655. [PubMed] [Google Scholar]
- Lavigne J.V, Giggons R.D, Christoffel K.K, Arend R, Rosenbaum D, Binns H, et al. Prevalence rates and correlates of psychiatric disorders among preschool children. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:204–214. doi: 10.1097/00004583-199602000-00014. [DOI] [PubMed] [Google Scholar]
- Meadow S.R. Day wetting. Pediatric Nephrology. 1990;4:178–184. doi: 10.1007/BF00858838. [DOI] [PubMed] [Google Scholar]
- Merline A, Olson L, Cull W. Length of pediatric visits actually increasing. 2009. May, Paper presented at the annual meeting of the Pediatric Academic Society, Baltimore, MD. [Google Scholar]
- Mischel W. Connecting clinical practice to scientific progress. Psychological Science in the Public Interest. 2009;9:i–ii. doi: 10.1111/j.1539-6053.2009.01035.x. [DOI] [PubMed] [Google Scholar]
- Mowrer O.H, Mowrer W.M. Enuresis: A method for its study and treatment. American Journal of Orthopsychiatry. 1938;8:436–459. [Google Scholar]
- Muellner R.S. The physiology of micturition. Journal of Urology. 1951;65:805–813. doi: 10.1016/S0022-5347(17)68554-9. [DOI] [PubMed] [Google Scholar]
- Muellner R.S. Development of urinary control in children. Journal of the American Medical Association. 1960;172:1256–1261. doi: 10.1001/jama.1960.03020120034007. [DOI] [PubMed] [Google Scholar]
- Pescosolido B.A. Culture, children, and mental health treatment: Special section on the national stigma study—children. Psychiatric Services. 2007;58:611–612. doi: 10.1176/ps.2007.58.5.611. [DOI] [PubMed] [Google Scholar]
- Regier D.A, Goldberg I.D, Taube C.A. The de facto US mental health services system. Archives of General Psychiatry. 1978;35:685–693. doi: 10.1001/archpsyc.1978.01770300027002. [DOI] [PubMed] [Google Scholar]
- Reisinger K.S, Bires J.A. Anticipatory guidance in pediatric practice. Pediatrics. 1980;66:889–892. [PubMed] [Google Scholar]
- Richman N, Stevenson J.E, Graham P.J. Prevalence of behaviour problems in 3-year old children: An epidemiological study in a London borough. Journal of Child Psychology and Psychiatry. 1975;16:277–287. doi: 10.1111/j.1469-7610.1975.tb00362.x. [DOI] [PubMed] [Google Scholar]
- Schneider M.S, King L.R, Surwitt R.S. Kegel exercises and childhood incontinence: A new role for an old treatment. Journal of Pediatrics. 1994;124:91–92. doi: 10.1016/s0022-3476(94)70259-4. [DOI] [PubMed] [Google Scholar]
- Simon J.L, Thompson R.H. The effects of undergarment type on the urinary continence of toddlers. Journal of Applied Behavior Analysis. 2006;39:363–368. doi: 10.1901/jaba.2006.124-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith M.L, Glass G.V, Miller T.I. The benefits of psychotherapy. Baltimore: Johns Hopkins University Press; 1980. [Google Scholar]
- Sperling M. The major neuroses & behavior disorders in children. Northvale, NJ: Aronoson; 1994. [Google Scholar]
- Starfield B, Gross E, Wood M, Pantell R, Allen C, Gordon B, et al. Psychosocial and psychosomatic diagnoses in primary care of children. Pediatrics. 1980;66:159–167. [PubMed] [Google Scholar]
- Tarbox R, Williams L, Friman P.C. Extended diaper wearing: Effects on continence in and out of the diaper. Journal of Applied Behavior Analysis. 2004;37:97–101. doi: 10.1901/jaba.2004.37-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Mental health: A report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration; 1999. [Google Scholar]
- Van Laecke E, Wille S, Vande Walle J, Raes A, Renson C, Peeren F, et al. The daytime alarm: A useful device for the treatment of children with daytime incontinence. Journal of Urology. 2006;176:325–327. doi: 10.1016/S0022-5347(06)00303-X. [DOI] [PubMed] [Google Scholar]
- Vincent S.A. Mechanical, electrical and other aspects of enuresis. In: Johnston J.H, Goodwin W, editors. Reviews in pediatric urology. New York: Elsevier; 1974. pp. 280–313. [Google Scholar]
- Wolfensberger W. Normalization. Toronto: National Institute of Mental Retardation; 1982. [Google Scholar]