Abstract
Objective
The purpose of this study was to examine trends in the prevalence of rheumatoid vasculitis in a national US dataset representing both hospitalized and ambulatory patients with rheumatoid arthritis (RA).
Methods
This serial cross-sectional study spanned over 20 years of hospital data (1985-2006) and ten years of ambulatory data (1997-2006) to examine the prevalence of rheumatoid vasculitis as defined by ICD-9 codes. The search encompassed 10-million hospitalizations and outpatient encounters including more than 37,000 patients with RA annually. To test for a decline in rheumatoid vasculitis, breakpoint analysis was performed using stepwise Chow and Durbin-Watson tests.
Results
The study showed a clear decline in the prevalence of rheumatoid vasculitis that remained after accounting for decreased hospitalizations. Peak prevalence occurred among inpatients in the 1980’s, and prevalence gradually declined throughout the 1990’s. However, both inpatient and outpatient datasets demonstrated simultaneous breakpoints representing a significant drop in RA vasculitis between the years 2000 and 2001 (p<0.000 and p<0.003). The prevalence of vasculitis dropped 31% among outpatients and 53% among inpatients with RA between 2000 and 2001.
Conclusion
This study demonstrates a significant decline in rheumatoid vasculitis after 2000 in this nationwide sample of predominantly male ambulatory and hospitalized patients. The clear, consistent drop in both the inpatient and outpatient settings provides an opportunity for causal hypothesis generation including considering the impact of biologic agents.
Current rheumatoid arthritis (RA) management is reducing articular damage and some authors report that aggressive treatment is modifying the entire spectrum of rheumatoid disease by reducing the frequency of severe disease (1-3). Arguably, severe extra-articular manifestations such as rheumatoid vasculitis are the most serious sequellae of rheumatoid arthritis. Despite a growing appreciation of the evolving natural history of RA joint disease with new treatments, important gaps remain in our understanding regarding trends in extra-articular manifestations including rheumatoid vasculitis.
Recent studies examining rheumatoid vasculitis reflect a lack of consensus regarding trends (4-8). Two studies reported declines in rheumatoid vasculitis while a third reported no change in rates. All three studies had methodological limitations including two that examined relatively few cases in population-based cohorts, and a third that captured only hospitalized cases. In the absence of representative national datasets, examining extra-articular complications among US patients with RA is challenging.
The purpose of this study was to examine trends in the prevalence of RA vasculitis in a national US dataset representing both hospitalized and ambulatory RA patients. We hypothesized that rheumatoid vasculitis has declined in recent years, not due to shifts in setting of care, but possibly related to aggressive RA treatment including the use of biologic agents.
Patients and Methods
This serial cross-sectional study spanned over 20 years of hospital data (1985-2006) and ten years of ambulatory data (1997-2006) to examine trends in the prevalence of rheumatoid vasculitis. After receiving IRB and Veteran’s Affairs approval, we searched the national Veteran’s Health Administration (VHA) system to assess RA vasculitis prevalence, including paired inpatient and outpatient data from 1997-2006 (Table 1). As of 2000, 26.5 million Veterans qualified for VHA care and approximately 4 million Veterans received services (9).
Table 1.
VHA Population and RA Prevalence Data
| Year | Total Outpatients |
RA Outpatients |
RA Vasculitis Cases (%) |
Prevalence/ 1000 RA |
Total Inpatients |
RA Inpatients |
RA Vasculitis Cases (%) |
Prevalence/ 1000 RA |
|---|---|---|---|---|---|---|---|---|
| 2006 | 5,078,432 | 43,347 | 1440 (3.3) | 33.2 | 366,400 | 3369 | 49 (1.4) | 14.5 |
| 2005 | 4,998,714 | 43,670 | 1370 (3.1) | 31.4 | 370,414 | 3249 | 41 (1.3) | 12.6 |
| 2004 | 4,871,136 | 43,655 | 1328 (3.0) | 30.4 | 364,783 | 3189 | 51 (1.6) | 16.0 |
| 2003 | 4,692,694 | 44,560 | 1156 (2.6) | 25.9 | 356,983 | 3218 | 41 (1.3) | 12.7 |
| 2002 | 4,434,671 | 44,129 | 1148 (2.6) | 26.1 | 357,427 | 3112 | 44 (1.4) | 14.1 |
| 2001 | 4,052,934 | 41,791 | 1179 (2.8) | 28.2 | 356,416 | 3139 | 48 (1.5) | 15.3 |
| 2000 | 3,640,811 | 38,961 | 1600 (4.1) | 41.1 | 351,173 | 3031 | 99 (3.3) | 32.6 |
| 1999 | 3,390,527 | 38,746 | 1630 (4.2) | 42.1 | 357,507 | 3151 | 99 (3.1) | 31.4 |
| 1998 | 3,235,212 | 37,813 | 1586 (4.2) | 41.9 | 369,138 | 3192 | 129 (4.0) | 40.4 |
| 1997 | 2,956,905 | 37,878 | 1585 (4.2) | 41.8 | 404,273 | 3397 | 140 (4.1) | 41.2 |
| 1985- | NA | NA | NA | NA | Mean: 570,184 | 5197 | 245 (4.7) | 47.0 |
| 1996 | Range: 478-635K | 4136-5823 | 171-289 | 41.3-52.0 | ||||
|
| ||||||||
Numbers reflect unique individuals seen each fiscal year, except 1985-96 inpatient data given no outpatient comparison
Cases were identified using ICD-9 discharge and clinic diagnostic codes. RA vasculitis case selection utilized a previously validated ICD-9 coding algorithm capturing the Scott and Bacon rheumatoid vasculitis manifestations (6, 10). The algorithm was modified to improve specificity by excluding diabetes cases. Vasculitis cases were required to include RA (ICD-9 code 714.0), the absence of diabetes mellitus (ICD-9 code 250), AND one of the following additional features: arteritis (ICD-9 code 447.6), mononeuritis multiplex (ICD-9 codes 354.1-3 or 354.8-9 or 355), peripheral neuropathy due to connective tissue disease (ICD-9 code 357.1), gangrene (ICD-9 code 785.4), or chronic ulcers (ICD-9 code 707.1). Cases were captured and sorted to count unique individuals encountered in the inpatient and outpatient settings. An individual may have been counted in both settings in a given year, thus analysis remained separated by setting.
Time series analysis and auto-regression tested the hypothesis that rheumatoid vasculitis prevalence had declined. Time-series analysis employed stepwise Chow tests. Auto-regression models were fit using Durbin Watson tests. Briefly, the Chow test compares a simple linear trend null against a model with a breakpoint and two separate regression lines (representing a change in trend or level), to determine if model performance improves when the period is divided into two parts. Significance for trend and breakpoints was predefined as p</=0.01. The Chow test was performed stepwise for all years with the smallest p-value tested as a break point. Identical analysis examined prevalence trends among Veterans with RA seen in the inpatient and outpatient settings annually.
Results
Throughout the follow-up period greater than 92% of Veterans with RA were male and the mean age was 64.9 years. Total veteran enrollment increased over time and the total number of outpatients with RA increased and then leveled in recent years (Table 1). The number of hospitalizations relative to total enrolled Veterans declined in the mid 1990’s, consistent with US healthcare trends encouraging management of chronic diseases in the outpatient setting. Absolute numbers of patients with RA remained stable.
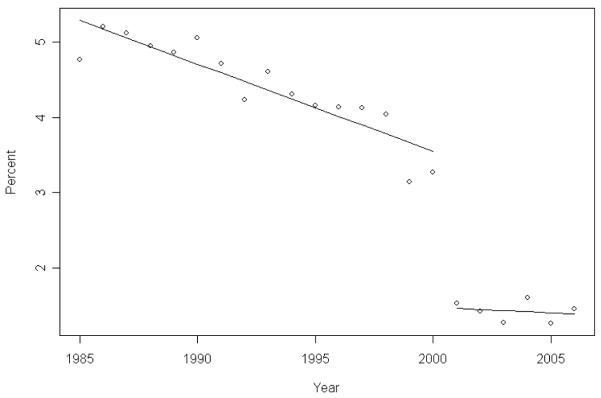
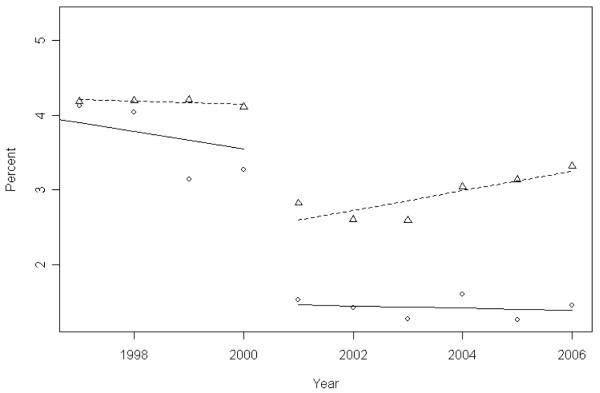
Prevalence of rheumatoid vasculitis demonstrated a clear drop among both hospitalized and ambulatory Veterans with rheumatoid arthritis (Figures 1 & 2). Autoregression using stepwise Chow testing importantly showed a breakpoint in the prevalence of rheumatoid vasculitis among both hospitalized and ambulatory patients (p<0.000 and p<0.003 respectively). Examining both the hospital and ambulatory datasets demonstrated identical breakpoint timing between years 2000 and 2001 (Figure 1).
Figure 1.
Rheumatoid Vasculitis Prevalence in Hospitalized RA Veterans 1985-2006. Points reflect the annual prevalence of rheumatoid vasculitis as a proportion of all patients with rheumatoid arthritis hospitalized between 1985 and 2006. Note the peak prevalence of 5% with a linear decline until 2000, and a subsequent drop to 1.3-1.6%.
Figure 2.
Rheumatoid Vasculitis Prevalence Among Veterans with RA 1997-2006. Circles reflect the annual prevalence of rheumatoid vasculitis as a proportion of all inpatients with rheumatoid arthritis and triangles represent prevalence of rheumatoid vasculitis among outpatients for comparable years 1997-2006. A simultaneous drop emerged between 2000 and 2001 in both settings.
The magnitude of the drop in rheumatoid vasculitis between 2000 and 2001 was approximately 31% among outpatients and 53% among inpatients. Prevalence of vasculitis among outpatients with RA fell from 41 cases per 1000 with RA, and among inpatients fell from 32 to only 15 cases per 1000. Alternate analysis including RA vasculitis inpatients without excluding diabetes demonstrated parallel linear trends and a decrease from 33 to 16 cases per 1000 from 2000 to 2001. Using our original case definition, absolute rates of rheumatoid vasculitis prevalence peaked at 52 cases per 1000 hospitalized veterans with RA in the 1980’s, or roughly 5% (Figure 1). Recently, prevalence of RA vasculitis among Veteran inpatients with RA has fallen below 2% (15 cases per 1000) from around 4% in 1997. Minimal subsequent increases in point prevalence of rheumatoid vasculitis in outpatients were noted between 2004 and 2006. These points did not meet significance for trend (p 0.045), and remained between 26-33 cases per 1000 RA outpatients compared to more than 40 cases per 1000 RA patients in the earlier period.
Discussion
This study demonstrates a significant decline in the prevalence of rheumatoid vasculitis after 2000 in both the inpatient and outpatient settings. Rates of hospitalization decreased in the mid-1990’s demonstrating the importance of also examining the outpatient prevalence of rheumatoid vasculitis prior to formulating conclusions. Ultimately, in this simultaneous analysis, the inpatient and outpatient trends mirrored one another thus demonstrating that reported declines did not merely reflect changes in the setting of care to outpatient management.
Previous studies reported conflicting conclusions regarding trends in the incidence and prevalence of rheumatoid vasculitis. One population-based study from the UK reported a decrease in RA vasculitis (8) but drew conclusions based upon only 51 total cases. A US population-based study reported no change in rheumatoid vasculitis based upon 42 cases (5). However that study truncated follow-up of their most recent onset RA cohort (1985-1994) at 2000, perhaps missing extra-articular events that classically occur later in the natural history of RA (4, 7). A study examining California hospital claims concluded that hospitalizations for RA vasculitis declined between the 1980 and 2001 (6). Analyzing only inpatient claims however left questions regarding whether contemporary RA vasculitis cases may have escaped detection due to evolving outpatient management.
To our knowledge, this study is the first US national examination of both inpatient and outpatient rheumatoid vasculitis prevalence. The study sought to overcome limitations of other studies that examined regional cohorts or included only hospitalized patients by pairing inpatient and outpatient data from the national VHA. Similar to the California study, a significant decline in rates of hospitalization for rheumatoid vasculitis emerged in our study. Importantly, however, we demonstrated a simultaneous drop among ambulatory patients, confirming that the drop was not an artifact of shifts in the setting of RA care. The timing of the decline in our study was also consistent with the UK report citing a nadir three-year average of RA vasculitis 1998-2000 (7, 8).
The serial cross-sectional design and demographics of the Veteran population impose some limits in widely applying results in this study. By design, the study captured only the prevalence of rheumatoid vasculitis and chart review validation of individual cases was not performed. Cases were captured using a previously validated algorithm with modification to exclude diabetes to improve specificity, though the exclusion of diabetes may have impacted case definition due to time trends in diabetes. Nevertheless, prevalence figures in this report are consistent with published incidence rates ranging from <1% to 5.4% (11-13). Furthermore, as a result of the demographics of the studied Veteran population, patients were predominantly male, older than most average RA patients, and tobacco use was likely higher than most RA cohorts. These demographics may limit translating the results to the general RA population. However classic reports have noted higher extra-articular manifestation rates among males, smokers, and persons with older onset RA (14, 15), perhaps making this group more likely to detect changes among the most “at-risk” population.
A key strength of the study was the inclusion of large numbers of patients studied over many years in both the inpatient and outpatient settings to strengthen conclusions regarding overall trends in rheumatoid vasculitis. The structure of the dataset facilitated simultaneous comparison demonstrating a consistent drop in vasculitis prevalence among ambulatory and hospitalized Veterans with RA.
These findings offer an opportunity to propose new testable hypotheses regarding trends in RA vasculitis. Given that prevalence is the product of incidence times duration minus case efflux, we consider that the observed decline may represent: (a) declining incidence (not directly testable here), (b) cure of some cases, (c) case deaths or migration from the VHA, or (d) error. The 1990’s through 2000 marked important changes in RA treatment. One may speculate that biologic agents and more aggressive disease modifying anti-rheumatic drug combination strategies targeted severe-spectrum RA, and may have diminished extra-articular disease including vasculitis by treating existing cases and preventing new cases. Additionally, VHA system-wide efforts to decrease tobacco use may have impacted rates of RA vasculitis. Future studies should examine temporal smoking and pharmacotherapy trends in relationship to RA vasculitis, and ongoing monitoring is merited.
Consistent with our hypothesis, a drop in rheumatoid vasculitis prevalence was demonstrated among ambulatory and hospitalized Veterans with RA even after accounting for shifts to outpatient management. Rather than a gradual linear decline, a breakpoint emerged between 2000 and 2001 in both the inpatient and outpatient settings demonstrating timing similar to a previous UK report (8). The consistent timing provides grounds to query causality. As RA treatment evolves it will be important to continue to follow the evolving natural history of RA including population trends in rheumatoid vasculitis among samples demonstrating a more typical gender ratio.
Acknowledgments
Grant Support: Dr. Bartels receives support through NIH/NCRR (1KL2RR025012-01).
References
- 1.Finckh A, Choi HK, Wolfe F. Progression of radiographic joint damage in different eras: trends towards milder disease in rheumatoid arthritis are attributable to improved treatment. Ann Rheum Dis. 2006;65(9):1192–7. doi: 10.1136/ard.2005.049338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Uhlig T, Heiberg T, Mowinckel P, Kvien TK. Rheumatoid arthritis is milder in the new millennium: Health status in RA patients 1994-2004. Ann Rheum Dis. 2008 doi: 10.1136/ard.2007.084673. [DOI] [PubMed] [Google Scholar]
- 3.Welsing PM, Fransen J, van Riel PL. Is the disease course of rheumatoid arthritis becoming milder? Time trends since 1985 in an inception cohort of early rheumatoid arthritis. Arthritis Rheum. 2005;52(9):2616–24. doi: 10.1002/art.21259. [DOI] [PubMed] [Google Scholar]
- 4.Puechal X. Incidence of vasculitis in rheumatoid arthritis: comment on the article by Turesson et al. Arthritis and Rheumatism. 2005;52(5):1620. doi: 10.1002/art.21046. author reply 1621. [DOI] [PubMed] [Google Scholar]
- 5.Turesson C, McClelland RL, Christianson TJ, Matteson EL. No decrease over time in the incidence of vasculitis or other extraarticular manifestations in rheumatoid arthritis: results from a community-based study. Arthritis and Rheumatism. 2004;50(11):3729–31. doi: 10.1002/art.20590. [DOI] [PubMed] [Google Scholar]
- 6.Ward MM. Decreases in rates of hospitalizations for manifestations of severe rheumatoid arthritis, 1983-2001. Arthritis and Rheumatism. 2004;50(4):1122–31. doi: 10.1002/art.20158. [DOI] [PubMed] [Google Scholar]
- 7.Watts RA, Lane SE, Scott DG. Decrease over time in the incidence of systemic rheumatoid vasculitis: Comment on the article by Turesson et al. Arthritis and Rheumatism. 2005;52(5):1620–1. doi: 10.1002/art.21047. author reply 1621. [DOI] [PubMed] [Google Scholar]
- 8.Watts RA, Mooney J, Lane SE, Scott DG. Rheumatoid vasculitis: becoming extinct? Rheumatology. 2004;43(7):920–3. doi: 10.1093/rheumatology/keh210. [DOI] [PubMed] [Google Scholar]
- 9.Cowper DC, et al. VA health care atlas- Fiscal year 2000. Rehabilitation Outcome Research Center; 2003. [Google Scholar]
- 10.Scott DG, Bacon PA, Tribe CR. Systemic rheumatoid vasculitis: a clinical and laboratory study of 50 cases. Medicine. 1981;60(4):288–97. [PubMed] [Google Scholar]
- 11.Kaye O, Beckers CC, Paquet P, Arrese JE, Pierard GE, Malaise MG. The frequency of cutaneous vasculitis is not increased in patients with rheumatoid arthritis treated with methotrexate. J Rheumatol. 1996;23(2):253–7. [PubMed] [Google Scholar]
- 12.Salvarani C, Macchioni P, Mantovani W, Rossi F, Veneziani M, Boiardi L, et al. Extraarticular manifestations of rheumatoid arthritis and HLA antigens in northern Italy. J Rheumatol. 1992;19(2):242–6. [PubMed] [Google Scholar]
- 13.Wattiaux MJ, Kahn MF, Thevenet JP, Sauvezie B, Imbert JC. [Vascular involvement in rheumatoid polyarthritis. Retrospective study of 37 cases of rheumatoid polyarthritis with vascular involvement and review of the literature] Ann Med Interne (Paris) 1987;138(8):566–87. [PubMed] [Google Scholar]
- 14.Turesson C, Jacobsson LT. Epidemiology of extra-articular manifestations in rheumatoid arthritis. Scandinavian Journal of Rheumatology. 2004;33(2):65–72. doi: 10.1080/03009740310004621. [DOI] [PubMed] [Google Scholar]
- 15.Voskuyl AE, Zwinderman AH, Westedt ML, Vandenbroucke JP, Breedveld FC, Hazes JM. Factors associated with the development of vasculitis in rheumatoid arthritis: results of a case-control study. Ann Rheum Dis. 1996;55(3):190–2. doi: 10.1136/ard.55.3.190. [DOI] [PMC free article] [PubMed] [Google Scholar]