Abstract
Aims
To outline the progress being made in the understanding of acquired resistance to long term therapy with the selective oestrogen receptor modulators (SERMs, tamoxifen and raloxifene) and aromatase inhibitors. The question to be addressed is how we can amplify the new biology of oestrogen-induced apoptosis to create more complete responses in exhaustively antihormone treated metastatic breast cancer.
Methods and Results
Three questions are posed and addressed.
1.) Do we know how oestrogen works? 2.) Can we improve adjuvant antihormonal therapy? 3.) Can we enhance oestrogen-induced apoptosis?
The new player in oestrogen action is GPR30 and there are new drugs specific for this target to trigger apoptosis. Similarly, anti-angiogenic drugs can be integrated into adjuvant antihormone therapy or to enhance oestrogen-induced apoptosis in Phase II antihormone resistant breast cancer. The goal is to reduce the development of acquired antihormone resistance or undermine the ability of breast cancer cells to undergo apoptosis with oestrogen respectively. Finally, drugs to reduce the synthesis of glutathione, a subcellular molecule compound associated with drug resistance, can enhance oestradiol-induced apoptosis.
Conclusions
We propose an integrated approach for the rapid testing of agents to blunt survival pathways and amplify oestrogen-induced apoptosis and tumour regression in Phase II resistant metastatic breast cancer. This Pharma platform will provide rapid clinical results to predict efficacy in large scale clinical trials.
Keywords: selective oestrogen receptor modulators, aromatase inhibitors, targeted therapy, oestrogen receptor, apoptosis, oestradiol, tamoxifen, antihormone resistance
Introduction
Tamoxifen (ICI46,474) was not hailed as an impressive breakthrough in the early 1970’s when it was marketed as an orphan drug that produced modest responses in the treatment of metastatic breast cancer in post menopausal women (1). Only one in three tumours responded to treatment for about a year. Nevertheless, side effects with tamoxifen were less than other available endocrine therapies (diethylstilboestrol (DES) or androgens) (2-4).
Despite initial disinterest in endocrine therapy, significant progress was subsequently made in the treatment and chemoprevention of breast cancer through the clinical application of laboratory principles for the antihormonal therapy of breast cancer (5). Today antihormonal therapies (tamoxifen and aromatase inhibitors) target the oestrogen receptor (ER) present in the majority of breast cancers and long term adjuvant therapy with tamoxifen increases patient survival (6, 7). Aromatase inhibitors that are used exclusively in postmenopausal patients improve disease-free survival when compared to tamoxifen, and reduced the risk of endometrial cancer and blood clots noted with tamoxifen (8). Additionally, the application of SERMs for the chemoprevention of breast cancer either directly with tamoxifen and raloxifene (9, 10) or indirectly with raloxifene for the prevention of osteoporosis (11-13) will surely reduce the incidence of breast cancer in select populations over the next decade.
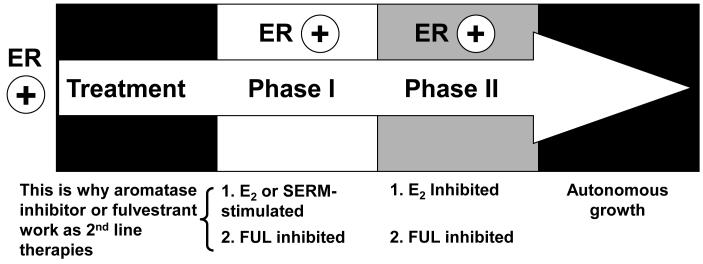
The critical strategy that led to the success of endocrine therapy for the treatment and prevention of breast cancer was the implementation of the laboratory principle of extended durations of treatment (14, 15). However, the consequence of long term treatment is the development of antihormonal drug resistance. Numerous laboratory models of antihormonal drug resistance have been developed over the past 20 years and several valuable principles have emerged. Drug resistance with SERMs evolves through at least two distinct phases: Phase I and Phase II (16) (Figure 1). Phase I resistance to tamoxifen treatment is characterized by either tamoxifen or oestradiol-stimulated growth. Both ligands can exploit the ER signal transduction pathway to aid tumour cell survival. This phase of drug resistance has a clinical equivalent in metastatic breast cancer. When treatment fails during tamoxifen therapy, the tumour has a withdrawal response or regression upon withdrawal of tamoxifen treatment (17). Second line therapy following tamoxifen treatment failure is with either an aromatase inhibitor or fulvestrant (18).
Figure 1.
The evolution of drug resistance to SERMs. Acquired resistance occurs during long-term treatment with a SERM and is evidenced by SERM-stimulated breast tumour growth. Tumours also continue to exploit oestrogen for growth when the SERM is stopped, so a dual signal transduction process develops. The aromatase inhibitors prevent tumour growth in SERM-resistant disease and fulvestrant that destroys the ER is also effective. This phase of drug resistance is referred to as Phase I resistance. Continued exposure to a SERM results in continued SERM-stimulated growth (Phase II), but eventually autonomous growth occurs that is unresponsive to fulvestrant or aromatase inhibitors. The event that distinguishes Phase I from Phase II acquired resistance is a remarkable switching mechanism that now causes apoptosis, rather than growth, with physiologic levels of oestrogen. These distinct phases of laboratory drug resistance (20, 25) have their clinical parallels and this new knowledge is being integrated into the treatment plan.
The description of Phase II resistance to tamoxifen was first presented at the St. Gallen Breast Cancer Conference in 1992 (19). Re-transplantation of tamoxifen-resistant MCF-7 breast tumours into tamoxifen treated athymic mice for 5 or more years causes the signaling networks through the ER, that normally act as a survival network, to become reconfigured to be activated by physiological oestradiol that causes rapid apoptosis and triggers tumour regression (20). The fact that these laboratory data pertaining to the evolution of drug resistance to tamoxifen also applies to antihormonal resistance to raloxifene (21), and oestrogen withdrawal (22-24) creates a valid general principle in breast cancer that can now be exploited in the clinic to enhance patient survivorship (25, 26). Indeed, it has been suggested that these current data (22, 27), can explain the effectiveness of high dose oestrogen therapy to treat metastatic breast cancer in post menopausal women before tamoxifen was available (28). High dose DES produces a 35% response rate in unselected patients (29) and interestingly enough Lonning and colleagues (30) reported a 30% response rate for high dose DES in a population of women who have received exhaustive anti-hormonal therapy to treat metastatic breast cancer. Remarkably, one woman has had a complete remission for more than 8 years after starting DES treatment (Per Lonning, personal communication).
We now choose to amplify the clinical potential of short term low oestradiol therapy to treat breast cancer in those patients whose ER positive tumour has responded and failed at least two consecutive antihormonal therapies. Based on the emerging clinical experience and on an expanding laboratory data base we anticipate a 30% clinical benefit (30) We address the question of why tumour cell survival signaling prevents 70% of Phase II tumours from responding to low dose oestradiol and we will advance short and long term solutions to apply pharmacological interventions to sensitize refractory breast cancers to oestradiol’s apoptotic actions.
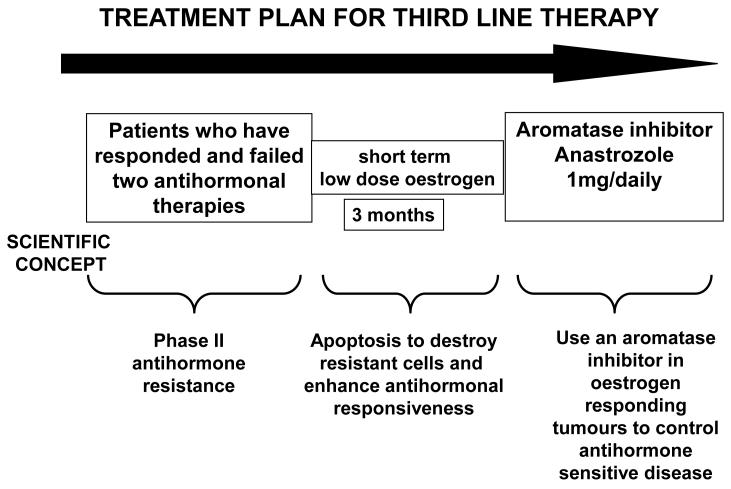
A clinical model to evaluate oestrogen induced apoptosis
We have previously proposed a clinical test bed to define the molecular biology and breast tumour responsiveness to both high doses (30 mg daily) and low dose (6 mg daily) oestradiol. That strategy is based on the translation of our laboratory description of the evaluation of anti-hormone resistance through phase I to phase II resistance where oestradiol switches from being a survival signal to an apoptotic trigger (16, 27, 31) The schema for the trial is illustrated in Figure 2. Breast cancer patients who are eligible for recruitment to the trial must have responded and failed two consecutive anti-hormonal therapies e.g. fail tamoxifen adjuvant therapy during year 3-5 and subsequently respond and fail an aromatase inhibitor during the treatment of metastatic breast cancer. In our first protocol of high dose oestradiol therapy (30 mg daily), we are treating for 12 weeks and then responding patients will be treated with an aromatase inhibitor (anastrazole 1 mg daily) until progression (32) Several other investigators have initiated similar clinical trials but with less rigorous entry criteria concerning failure of repeated endocrine therapies. Nevertheless, we contend that the moment is right to address the issue of the regulation of apoptosis and advance the idea that other agents may be synergistic with oestradiol to trigger apoptosis in the predicted 70% of patients that do not respond to short term oestradiol therapy.
Figure 2.
Clinical protocol to investigate the efficacy of oestradiol induced apoptosis in long-term endocrine refractory breast cancer. An anticipated treatment plan for third-line endocrine therapy. Patients must have responded and experience treatment failure with two successive antihormone therapies to be eligible for a course of low-dose oestradiol therapy for 3 months. The anticipated response rate is 30% and responding patients will be treated with anastrozole until relapse. Validation of the treatment plan will establish a platform to enhance response rates with apoptotic oestrogen by integrating known inhibitors of tumour survival pathways into the 3-month debulking “oestrogen purge”. The overall goal is to increase response rates and maintain patients for longer on antihormone strategies before chemotherapy is required.
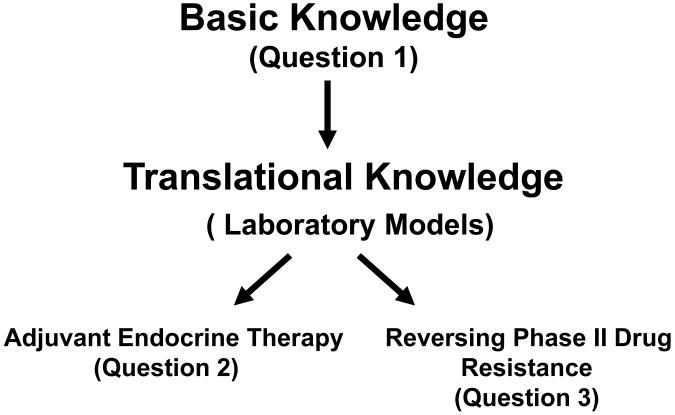
Opportunities in the endocrine regulation of breast cancer
Naturally, it is not possible to consider all of the opportunities that could be exploited for patient benefit but we pose three questions that will be answered with an example of current research from our laboratory. The questions will be addressed as an integrated translational research scheme summarized in Figure 3.
Figure 3.
The interactive translational research model employed to address new hypotheses and opportunities to amplify oestrogen-induced apoptosis for the treatment of Phase II endocrine resistant breast cancer. The questions posed are described in the text.
Question 1: Do we know how oestrogen works in target tumours?
The ER with its modulation through co-activators and co-repressors (33) has been investigated extensively through the structure function relationships of ligands that create novel folding of the receptor complex (34). However the array of SERMs is only able to add marginally to advancing cancer therapeutics. We are beginning to understand the cross talk between the ER pathway and growth factor receptor pathways but our basic knowledge is in its infancy. There is an increasing menu of medicines to block growth factor pathways, but the challenge is to place the right targeted agent in the endocrine treatment paradigms. We will return to this challenge in our summary.
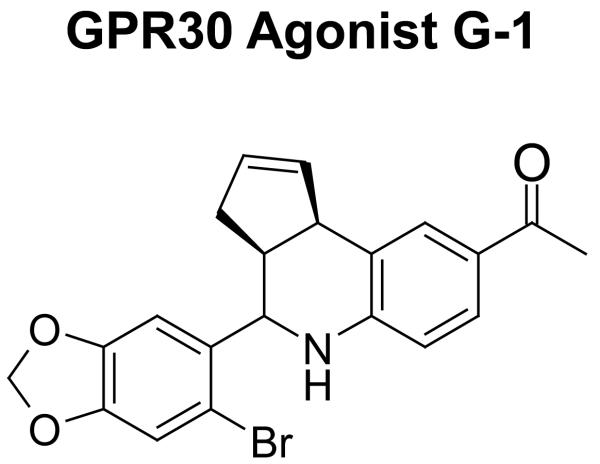
Our confidence in the position that “we understand how oestradiol works” has been challenged twice in recent times firstly with the discovery of a second ER referred to as ER-β (ER-α is the classical ER), and secondly with the discovery of the G protein-coupled receptor GPR30, an oestrogen-, SERM- and fulvestrant-binding protein. The role of ER-β in breast cancer is controversial but there is evidence that overexpression of ER-β can inhibit proliferation (35) and cause apoptosis (36). However, ER-β specific ligands have yet to find a role in cancer therapeutics. The G protein-coupled receptor GPR30 is the latest putative receptor that can modulate oestrogen action specifically (37). The molecule, a seven-pass transmembrane receptor located in the endoplasmic reticulum, mediates rapid non-genomic actions of oestradiol to initiate mobilization of intracellular Ca ++ stores.
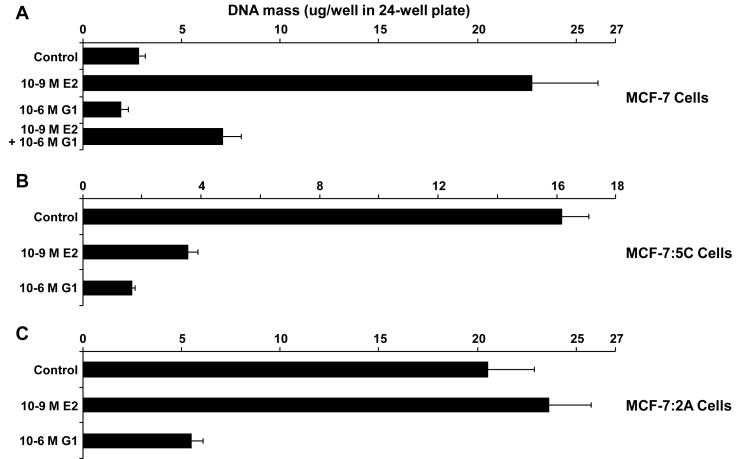
Based on high through put screening assays a new class of molecules specific for GPR30 has been identified (38), and one compound G1 (Figure 4) is available for laboratory investigations. We have addressed the question of whether the GPR30 agonist G1 is a stimulator or blocker of oestradiol-stimulated growth in the wild-type ER-positive MCF-7 breast cancer cell line and whether G1 can provoke apoptosis in our oestrogen deprivation-resistant cell lines MCF-7:5C (23) and MCF-7:2A (39) data shown in Figure 5 illustrates the fascinating pharmacology of the new drug group. G1 is anti-oestrogenic in the wild type MCF-7 cell line, and enhances apoptosis in both the MCF-7:5C and MCF-7:2A cell lines. Most importantly, G1 induces apoptosis in the MCF-7:2A cells more rapidly than oestradiol. This is important as it provides evidence that in endocrine resistant breast cancer cells, which are initially refractory to the immediate apoptotic actions of oestradiol, there is the potential to circumvent survival and initiate apoptosis quickly via a new pathway. The mechanism of action of G1 in all breast cancer cell lines is the rapid mobilization of high levels of Ca++ from intracellular stores. This increase of Ca++ is cytotoxic, thus, the new drug group has potential to enhance apoptosis in anti-hormone resistant cell lines and further development of these agents may find an application for short term treatment of patients whose tumours are Phase II anti-hormone resistant.
Figure 4.
G1, the first of a new class of agents that act as selective agonists of GPR30. A range of antagonists is also being developed.
Figure 5.
The selective GPR30 agonist G1 inhibits growth of (A) wild-type MCF-7 cells and of oestrogen deprivation-resistant (B) MCF-7:5C and (C) MCF-7:2A cells. Cells were cultured under oestrogen-free conditions for 4 days, and then seeded into 24-well plates. Wild-type MCF-7 cells were seeded at 15,000 cells per well, MCF-7:5C cells at 25,000 cells per well, and MCF-7:2A cells at 30,000 cells per well. Beginning 24 hours after seeding (day 0) and every 2 days thereafter up to 6 days (days 2, 4, and 6), the cells were treated with 1 nM E2, 1 μM G1, 1 nM E2 + 1 μM G1, or Control (0.1% EtOH)-treated. The experiment was stopped on day 7. As a measure of proliferation, the amount of DNA per well was determined using a fluorescence-based DNA quantitation assay (CyQuant GR, Invitrogen, Carlsbad, CA). Data are shown as the mean of 8 replicate wells per group ± SD. (A) In wild-type MCF-7 cells, G1 significantly inhibited E2-stimulated growth by 78% (E2 vs. E2+G1, P < 0.0001), and inhibited growth relative to control-treated cells (control vs. G1, P = 0.0003). (B) In estrogen deprivation-resistant MCF-7:5C cells, E2 induced apoptosis as expected leading to a 78% reduction in growth (control vs. E2, P < 0.0001). G1 also significantly inhibited growth by 90% (control vs. G1, P < 0.0001), and further, was more potent than E2 (G1 vs. E2 P < 0.0001). (C) The oestrogen deprivation-resistant MCF-7:2A cells grew independently of E2 within the 7 day course of the experiment, as expected, yet G1 significantly inhibited growth by 73% (P < 0.0001).
Question 2: Can we improve adjuvant antihormonal therapy?
We have probably reached a zenith with what can be achieved with adjuvant antihormonal therapy. Nevertheless, significant increases in efficacy can be achieved by improving compliance for long term adjuvant therapy or selecting out those patients that have variant CYP2D6 that does not metabolize tamoxifen to the active metabolite endoxifen (40). What is required is a new initiative that can significantly enhance the effectiveness of antihormonal therapy and reduce the development of acquired drug resistance and possibly block intrinsic resistance. It could be, that the 40% of ER positive breast cancers that do not respond initially to antihormones could be encouraged to do so by pharmacologic intervention.
Angiogenesis is critical for the growth of tumours and the establishment of metastatic lesions (41). However, antiangiogenic drugs must be integrated into the cancer treatment plan as there are no advantages to monotherapy. As a result there is increasing interest in combining antiangiogenic drugs with cytotoxic chemotherapy with the goal of achieving better tumour responses (42). There has however, been little interest in combining antiangiogenic agents with antihormonal therapy primarily because such long term treatments are required and the effective doses of antiangiogenic drugs have significant side effects that are often life threatening.
The development of acquired resistance to SERMs implies that angiogenic mechanisms must be activated in cancer cells to permit SERM stimulated growth. Indeed, recent research has demonstrated that an autocrine Vascular Endothelial Growth Factor (VEGF) VEGF receptor 2 (VEGFR2) and P38 signaling loop confers resistance to 4-hydroxytamoxifen in MCF-7 breast cancer cells (43). Thus, the rationale of combining antihormonal therapy with antiangiogenic therapy has conceptual merit.
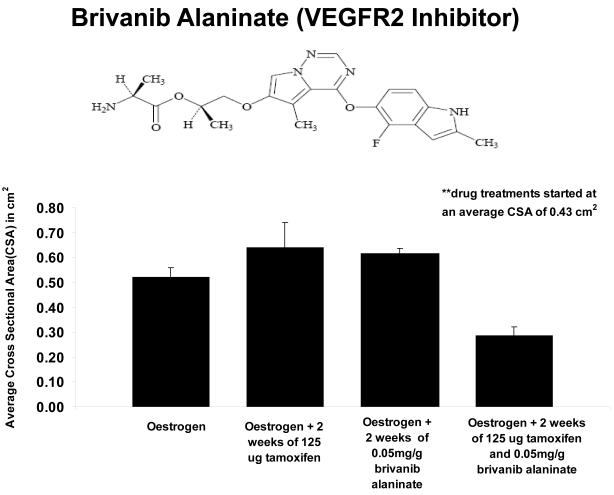
We have addressed the idea that low doses of an inhibitor of the VEGFR2 tyrosine kinase could be synergistic with tamoxifen to enhance the control of tumour cell growth in vivo. There is merit to using low doses of small molecule inhibitors of VEGFR2 in treatment regimens as side effects will be reduced and the drug may be sufficient to block the modest, but significant, angiogenic action of tamoxifen. In preliminary studies, we show (Figure 6) that a combination of tamoxifen and a VEGFR2 inhibitor brivanib alaninate is superior to tamoxifen alone at inhibiting oestradiol induced tumour growth in athymic animals. The low dose of brivanib alaninate used does not significantly affect oestradiol-stimulated tumour growth when used alone. We conclude that the angiogenic signal from oestradiol is too strong but that the inhibition of the cell cycle with tamoxifen and the antiangiogenic brivanib alaninate in combination is synergistic.
Figure 6.
Established MCF-7 E2 tumours and their response to various drug treatments. Tumours were implanted bilaterally into the mammary fat pads of athymic mice and 0.3 cm estradiol capsules were implanted subcutaneously into the dorsum of each mouse. Tumours were grown to 0.43 cm^2 and then drug treatments were initiated. Tumours that were treated with 125 ug of tamoxifen or 0.05 mg/g brivanib alaninate were unable to overcome oestradiol stimulated growth (p=0.65, p=0.21). . Tumours continued to grow in the presence of oestrogen. When 125 ug of tamoxifen was combined with 0.05 mg/g brivanib alaninate, the effect was synergistic (p=.009) and the tumours decreased in size. The tumours were 38% smaller than the oestrogen treated tumours, even though the observed difference was not significant (p=0.16). However, the decrease in average cross sectional area was significant when comparing the combination treatment to tamoxifen treated tumours (p=.01) or those treated with brivanib alaninate (p=007).
The issue to be addressed is how to test the concept before committing to large scale adjuvant trials. One approach would be to evaluate efficacy and safety in our proposed model of oestradiol induced apoptosis in Phase II resistant breast cancer (Figure 2). The goal would be to evaluate short term antiangiogenesis treatment by limiting toxicity during the 12 week treatment period and to assess improvements in response rates to physiologic (6mg dose) oestradiol treatment alone. This would also address the third question we pose.
Question 3 Can we enhance oestrogen-induced apoptosis?
An effective treatment strategy for breast cancer must have a clear goal with the aim of enhancing patient survivorship. The progress (44) being made by translating the laboratory studies(45) of low dose apoptotic oestradiol therapy into clinical practice must be amplified to bring further benefits to a select group of patients. Those patients with Phase II resistant metastatic breast cancer are a significant proportion of all those who respond initially to adjuvant endocrine therapy. The goal is to harness the apoptotic trigger and create an enhanced sensitivity to oestrogen so that a higher proportion of tumours have a complete response to treatment. An application of general pharmacologic principles can be seen as a first step in amplifying oestrogen-induced apoptosis. Inhibitors of angiogenesis would be a logical innovation to aid oestrogen-induced apoptosis. By denying the ability of resistant cells to grow by restricting angiogenesis, may result in cellular instability and to enhance sensitivity to apoptosis. However, it is the critical players in the inhibition of apoptosis that need to be targeted in a broad strategy of combination therapy. It is generally agreed that Bcl-2 plays a central role in preventing the intrinsic apoptosis trigger through the mitochondrial pathway of cytochrome C release. One mechanism by which Bcl-2 may function is as an anti-oxidant by up-regulation of glutathione leading to rapid detoxification of reactive oxygen species and inhibition of free-radical mediated mitochondrial damage.
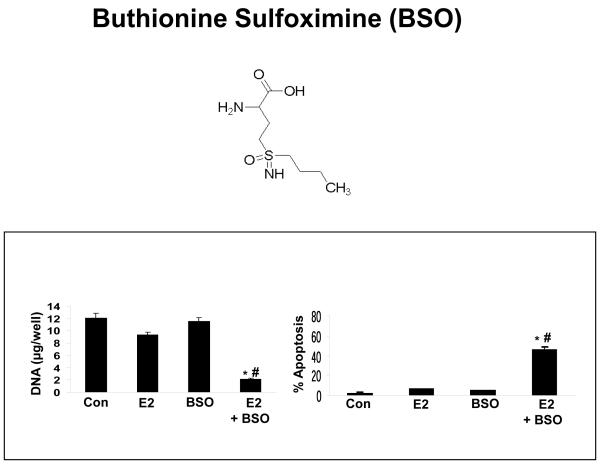
Glutathione is a water soluble tripeptide composed of glutamine, cysteine, and glycine. Elevated levels prevent apoptotic cell death whereas depletion of glutathione facilitates apoptosis (46) L-Buthionine sulfoximine (BSO) (Figure 7) is a specific inhibitor of glutanylcysteine synthase that blocks the rate limiting step of glutathione biosyntheses.
Figure 7.
The combination treatment of BSO plus oestradiol inhibits the growth of antihormone-resistant MCF-7:2A breast cancer cells. MCF-7:2A cells (30,000/well) were seeded in 24-well plates and after 24 hours were treated with < 0.1% ethanol vehicle (control), 1 nM E2 (E2), 100 μM BSO (chemical structure shown above), or 100 μM BSO plus 1 nM E2 for 7 days. At the indicated time point, cells were harvested and total DNA (μg/well) was quantitated as described in Materials and Methods. The data represent the mean of three independent experiments; bars, ±SE. **, P < 0.001 compared with control cells; ##, P < 0.001 compared with oestradiol-treated cells. Annexin V staining for apoptosis was performed in MCF-7:2A cells following BSO plus E2 treatment. Quantitation of apoptosis (percent of control) in the different treatment groups is shown on the right. bars, ±SEs. *, P < 0.05 compared with control cells; #, P < 0.01 compared with oestradiol-treated cells.
Recent laboratory studies demonstrate (39) that oestrogen deprived MCF7 cells that are initially refractory to oestradiol induced apoptosis are sensitized to the immediate apoptotic action of oestrogen by BSO at concentrations that can be achieved clinically (47) (Figure 7) Since there is an extensive clinical experience with BSO it would not be unreasonable to integrate the antioxidant concept into the clinical test model (48).
An integrated clinical strategy to target survival pathways in Phase II breast cancer
Overall, we are making significant progress towards understanding oestrogen-induced apoptosis and there is evidence that a new drug group based on GPR30 agonists could be developed to provide additional specificity and induce apoptosis in breast cancer. This approach could overcome some resistance in tumour cells observed with oestradiol alone. This, however, is a long term goal and builds on an evolving understanding of the complexities of oestrogen action in cancer. Similarly the anti-angiogenic drugs that block the tyrosine kinase activity of VEGFR2 could undermine the survival of tumours that are refractory to the apoptotic oestrogen trigger. But in practical terms, the application of BSO with an apoptotic oestrogen trigger has immediate clinical applications in our clinical test model (Figure 2). We have presented developing laboratory evidence to support each of these pharmacologic strategies to amplify the apoptotic oestrogen therapy in Phase II resistant breast cancer. However, the mechanism based clinical test model is more than a translational research tool.
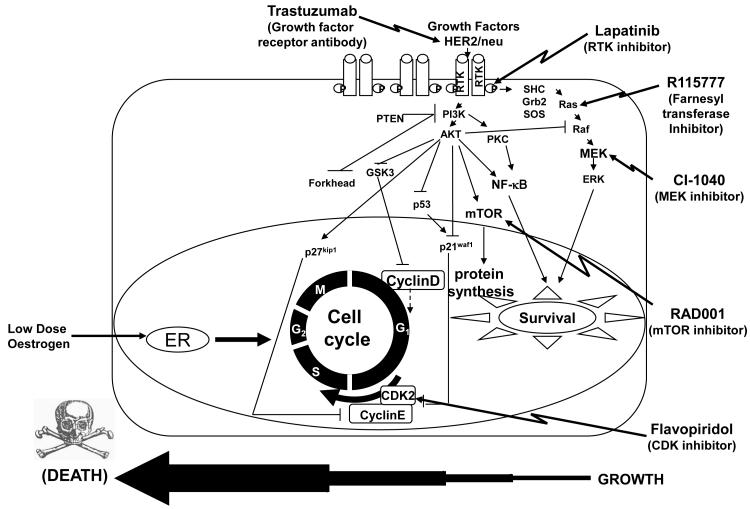
Rapid clinical results can be developed through mechanism based targeting of several pathways that have the potential to amplify the apoptotic oestrogen trigger to create a significant increase in complete tumour responses. In Figure 8 are examples of agent classes that could potentially be tested rapidly in the 12 week model against oestrogen alone. This will establish efficacy of a new targeted agent as a clinically useful drug.
Figure 8.
Hypothetical apoptosis enhancement strategy to amplify the tumouricidal action of low dose oestradiol treatment. The strategy is to employ targeted agents from the pharmacological industry to block several pathways and shift the cellular equilibrium to apoptosis in oestrogen refractory Phase II resistant cells. The diagram illustrates candidate drugs to create a cocktail in the proposed Pharma platform. Drugs would be tested singly with oestradiol against alone or in increasing combinations.
The hypothetical, yet systematic, strategy to evaluate selectively the inhibition of survival signals has a foundation in laboratory science. The obvious strategy of blocking the growth factor receptor signal cascade using either trastuzumab or the tyrosine kinase inhibitor lapatinib as an immediate practical approach in the 12 week test model. Recent studies demonstrate that antihormone responsiveness can be restored by aromatase resistant cells using trastuzumab (49) and lapatinib (50) is showing promise in clinical trials of breast cancer with chemotherapy (51).
The mammalian target-of-rapamycin (mTOR) is emerging as an important target for therapeutic intervention in multiple cancer tissue types including breast cancer. mTOR integrates signals from multiple pathways to sense cellular nutrient and energy levels. mTOR is a serine/threonine kinase downstream of PI3K/Akt that, in the presence of mitogenic stimulation and sufficient nutrients, promotes protein translation by activating 40S ribosomal protein S6 kinases (S6K1-2) and inhibiting the eukaryotic initiation factor 4E binding proteins (4E-BP1-3) (52). RAD001 (everolimus) is an orally available mTOR inhibitor that alone and synergistically in combination with the aromatase inhibitor letrozole (53) blocks proliferation and induced apoptosis in MCF-7 and T47D breast cancer cells stably expressing aromatase (53). These and other data have lead to the evaluation of RAD001 in combination with letrozole in a recently completed Phase I clinical trial in patients with advanced breast cancer (54). RAD001 is also currently under evaluation in 15 other breast cancer clinical trials (search of clinicaltrials.gov on 2/26/2009) either as a single agent or in combination with various chemotherapeutics, fulvestrant, aromatase inhibitors, and agents which target EGFR and HER2/ErbB2.
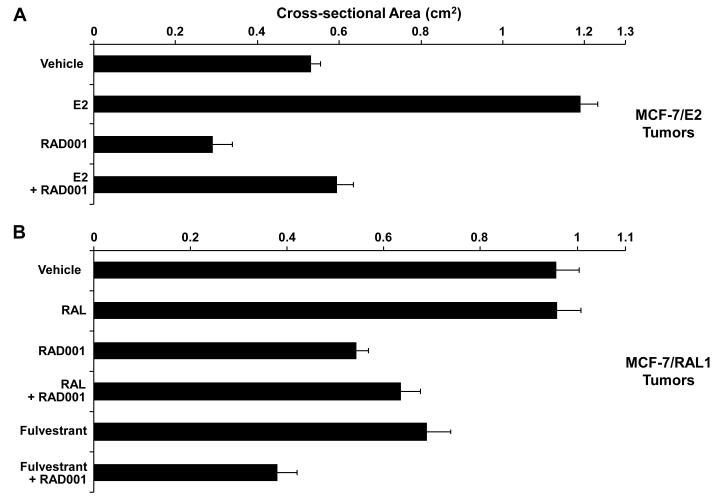
We evaluated RAD001 in an MCF-7 breast cancer xenograft tumour model (MCF-7/E2) grown in athymic mice (Figure 9A) that represents the therapeutic stage of antihormone-based therapy, and in a SERM-resistant (MCF-7/RAL1) xenograft tumour model (Figure 9B) that was selected in vivo by continuous treatment with the SERM raloxifene for greater than 3 years (31, 55). RAD001 inhibited MCF-7/E2 tumour growth in the presence of E2 (E2 + RAD001 vs E2 alone). Additionally, RAD001 in the absence of E2, a situation comparable to combination therapy of RAD001 plus an aromatase inhibitor in the clinic, further reduced MCF-7/E2 growth (RAD001 alone vs. E2 + RAD001). These MCF-7/RAL1 tumours can be considered cross-resistant to oestrogen deprivation (or aromatase inhibitors). However, RAD001 was still effective at blocking growth despite resistance to oestrogen deprivation (RAD001 vs. vehicle). Fulvestrant can be used clinically as a second-line therapy after failure of a first-line antihormone therapy, as illustrated here by fulvestrant inhibiting growth in the MCF-7/RAL1 tumours (fulvestrant vs. vehicle or RAL). Yet the combination of RAD001 plus fulvestrant was superior at blocking growth than either agent alone (Fulvestrant + RAD001 vs. fulvestrant alone and vs. RAD001 alone). Taken together, RAD001 represents a promising therapeutic for use in antihormone-sensitive, and importantly, in antihormone-resistant breast cancer, especially in combination with fulvestrant.
Figure 9. Growth inhibition of naïve MCF-7/ E2 tumours and SERM-resistant MCF-7/RAL1 tumours in response to RAD001 (everolimus).
(A) RAD001 inhibition of MCF-7/ E2 tumour growth. Twenty ovariectomized athymic nude mice were bilaterally transplanted with MCF-7/ E2 tumour pieces 1 mm3 in size in the axillary mammary fat pads, and implanted with a 0.3 cm E2 silastic capsule sc. Once the tumours grew to an average cross-sectional area of 0.39 cm2, the animals were randomized into 4 treatment groups of 5 mice per group (10 tumours per group) corresponding to Vehicle (of the RAD001 formulation), E2 (0.3 cm E2 capsule sc), RAD001 [40 mg/kg/day (6.25 mg/day) RAD001 given 5 days/week], and E2 + RAD001 (0.3 cm E2 capsule sc plus 6.25 mg/day RAD001 given 5 days/week). The average cross-sectional area of RAD001-treated MCF-7/ E2 tumours was significantly smaller than Vehicle-treated tumours (P = 0.0066, T test). Similarly, the average cross-sectional are a of E2 + RAD001-treated tumours was significantly smaller than E2 alone -treated tumours (P < 0.0001). (B) RAD001 inhibition of MCF-7/RAL1 tumour growth. Thirty ovariectomized athymic nude mice were bilaterally implanted in the axillary mammary fat pads with 1 mm3 MCF-7/RAL1 tumour pieces. Mice were treated with 1.5 mg/day RAL po until the MCF-7/RAL1 tumours grew to an average cross-sectional area of 0.26 cm2, and then the animals were separated into 6 treatment groups of 5 mice each (10 tumours per group) corresponding to Vehicle (of the RAD001 formulation), 1.5 mg/day RAL po, RAD001 (6.25 mg/day RAD001 given 5 days/week), RAL + RAD001 (1.5 mg/day RAL po plus 6.25 mg/day RAD001 given 5 days/week), Fulvestrant (2 mg/day sc of the clinically used Faslodex preparation given 5 days/week), Fulvestrant + RAD001 (2 mg/day Faslodex sc plus 6.25 mg/day RAD001 given 5 days/week). The average cross-sectional areas of RAD001-treated and Fulvestrant-treated tumours were each significantly smaller than Vehicle-treated tumours (P < 0.0001 and P = 0.0015, respectively). Similarly, RAL + RAD001 –treated tumours were significantly smaller than RAL-treated tumours (P = 0.0002). Additionally, Fulvestrant + RAD001 –treated tumors were significantly smaller than RAD001 alone –treated tumors (P = 0.0026) or Fulvestrant alone –treated tumors (P = 0.0004). The data shown represent the average cross-sectional tumour area (cm2) per group ± SE. Tumor cross-sectional area was calculated using the equation: (l/2) × (w/2) × π. The cross-sectional areas of MCF-7/E2 tumours were compared at day 41, and of MCF-7/RAL1 tumours at day 54.
It is clear that other inhibitors of signal transduction pathways (Figure 8)may be useful to enhance estrogen-induced apoptosis such as the MEK inhibitor CI-1040 (56), the farnesyl transferase inhibitor lonafarnib (57) and the cyclin-dependent kinase inhibitor flavopiridol (58). Indeed, inhibitors of CDK may have merit as a short term blocking strategy to enhance apoptosis. The cyclin-dependent kinase inhibitory drugs such as flavopiridol that have been tested clinically and causes apoptosis through an intrinsic pathway dependent on BAX and BAK (58) would be of significant interest in combination with oestradiol to amplify apoptosis.
In summary a whole spectrum of new compounds can now be tested to enhance tumour response to oestrogen with the added advantage that this testing platform can document rapid tumour responses. Combinations could create an optimal cocktail for individual tumours to predict a complete response triggered by oestrogen.
Acknowledgements
We thank Marybeth Jannotti for preparing the manuscript. Supported by the Department of Defense Breast Program under Award No. BC050277 (VCJ), Center of Excellences SPORE in Breast Cancer CA 89018 (VCJ), R01 GM067156 (VCJ), Fox Chase Cancer Center Core Grant No. NIH P30 CA006927, BMS research grant on angiogenesis (VCJ) the Avon Foundation (VCJ), the Genuardi’s Fund (VCJ), the Weg Fund of the Fox Chase Cancer Center (VCJ), the American Cancer Society Grant IRG-92-027-14 (JSLW), the Hollenbach Family Fund (JSLW), the NIH Career Development Grant K01CA120051-01A2 (JSLW), and 5T32CA10365-03 (RRP).
References
- 1.Jordan VC. Tamoxifen: a most unlikely pioneering medicine. Nature Reviews Drug Discovery. 2003;2:205–13. doi: 10.1038/nrd1031. [DOI] [PubMed] [Google Scholar]
- 2.Cole MP, Jones CT, Todd ID. A new anti-oestrogenic agent in late breast cancer. An early clinical appraisal of ICI 46474. Br J Cancer. 1971;25:270–5. doi: 10.1038/bjc.1971.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ward HW. Anti-oestrogen therapy for breast cancer: a trial of tamoxifen at two dose levels. Br Med J. 1973;1:13–4. doi: 10.1136/bmj.1.5844.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ingle JN, Ahmann DL, Green SJ, Edmonson JH, Bisel HF, Kvols LK, et al. Randomized clinical trial of diethylstilbestrol versus tamoxifen in postmenopausal women with advanced breast cancer. N Engl J Med. 1981;304:16–21. doi: 10.1056/NEJM198101013040104. [DOI] [PubMed] [Google Scholar]
- 5.Jordan VC. Tamoxifen: catalyst for the change to targeted therapy. Eur J Cancer. 2008;44:30–8. doi: 10.1016/j.ejca.2007.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.EBCTCG Tamoxifen for early breast cancer: an overview of the randomised trials. Lancet. 1998;354:1451–67. [PubMed] [Google Scholar]
- 7.EBCTCG Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;365:1687–717. doi: 10.1016/S0140-6736(05)66544-0. [DOI] [PubMed] [Google Scholar]
- 8.Howell A, Cuzick J, Baum M, Buzdar A, Dowsett M, Forbes JF, et al. Results of the ATAC (Arimidex, Tamoxifen, Alone or in Combination) trial after completion of 5 years’ adjuvant treatment for breast cancer. Lancet. 2005;365:60–2. doi: 10.1016/S0140-6736(04)17666-6. [DOI] [PubMed] [Google Scholar]
- 9.Fisher B, Costantino JP, Wickerham DL, Cecchini RS, Cronin WM, Robidoux A, et al. Tamoxifen for the prevention of breast cancer: current status of the National Surgical Adjuvant Breast and Bowel Project P-1 study. J Natl Cancer Inst. 2005;97:1652–62. doi: 10.1093/jnci/dji372. [DOI] [PubMed] [Google Scholar]
- 10.Vogel VG, Costantino JP, Wickerham DL, Cronin WM, Cecchini RS, Atkins JN, et al. The Study of Tamoxifen and Raloxifene (STAR): Report of the National Surgical Adjuvant Breast and Bowel Project P-2 Trial. JAMA. 2006;295:2727–41. doi: 10.1001/jama.295.23.joc60074. [DOI] [PubMed] [Google Scholar]
- 11.Cummings SR, Eckert S, Krueger KA, Grady D, Powles TJ, Cauley JA, et al. The effect of raloxifene on risk of breast cancer in postmenopausal women: results from the MORE randomized trial. Multiple Outcomes of Raloxifene Evaluation. JAMA. 1999;281:2189–97. doi: 10.1001/jama.281.23.2189. [DOI] [PubMed] [Google Scholar]
- 12.Martino S, Cauley JA, Barrett-Connor E, Powles TJ, Mershon J, Disch D, et al. For the CORE Investigators Continuing Outcomes Relevant to Evista: breast cancer incidence in postmenopausal osteoporotic women in a randomized trial of raloxifene. J Natl Cancer Inst. 2004;96:1751–61. doi: 10.1093/jnci/djh319. [DOI] [PubMed] [Google Scholar]
- 13.Jordan VC. The rise of raloxifene and the fall of invasive breast cancer. J Natl Cancer Inst. 2008;100:831–3. doi: 10.1093/jnci/djn177. [DOI] [PubMed] [Google Scholar]
- 14.Jordan VC, Dix CJ, Allen KE. The effectiveness of long term tamoxifen treatment in a laboratory model for adjuvant hormone therapy of breast cancer. Adjuvant Therapy of Cancer. 1979;2:19–26. [Google Scholar]
- 15.Jordan VC, Allen KE. Evaluation of the antitumour activity of the non-steroidal antioestrogen monohydroxytamoxifen in the DMBA-induced rat mammary carcinoma model. Eur J Cancer. 1980;16:239–51. doi: 10.1016/0014-2964(80)90156-5. [DOI] [PubMed] [Google Scholar]
- 16.Jordan VC. Selective estrogen receptor modulation: concept and consequences in cancer. Cancer Cell. 2004;5:207–13. doi: 10.1016/s1535-6108(04)00059-5. [DOI] [PubMed] [Google Scholar]
- 17.Howell A, Dodwell DJ, Anderson H, Redford J. Response after withdrawal of tamoxifen and progestogens in advanced breast cancer. Ann Oncol. 1992;3:611–7. doi: 10.1093/oxfordjournals.annonc.a058286. [DOI] [PubMed] [Google Scholar]
- 18.Howell A, Robertson JFR, Quaresma Albano J, Aschermannova A, Mauriac L, Kleeberg UR, et al. Fulvestrant, formerly ICI 182,780, is as effective as anastrozole in postmenopausal women with advanced breast cancer progressing after prior endocrine treatment. J Clin Oncol. 2002;20:3396–403. doi: 10.1200/JCO.2002.10.057. [DOI] [PubMed] [Google Scholar]
- 19.Wolf DM, Jordan VC. Recent Results in Cancer Research. Springer-Verlag; Heidelberg: 1993. A laboratory model to explain the survival advantage observed in patients taking adjuvent tamoxifen therapy; pp. 23–33. [DOI] [PubMed] [Google Scholar]
- 20.Yao K, Lee ES, Bentrem DJ, England G, Schafer JI, O’Regan RM, et al. Antitumor action of physiological estradiol on tamoxifen-stimulated breast tumors grown in athymic mice. Clin Cancer Res. 2000;6:2028–36. [PubMed] [Google Scholar]
- 21.Liu H, Lee ES, Gajdos C, Pearce ST, Chen B, Osipo C, et al. Apoptotic action of 17beta-estradiol in raloxifene-resistant MCF-7 cells in vitro and in vivo. J Natl Cancer Inst. 2003;95:1586–97. doi: 10.1093/jnci/djg080. [DOI] [PubMed] [Google Scholar]
- 22.Song RX, Mor G, Naftolin F, McPherson RA, Song J, Zhang Z, et al. Effect of long-term estrogen deprivation on apoptotic responses of breast cancer cells to 17beta-estradiol. J Natl Cancer Inst. 2001;93:1714–23. doi: 10.1093/jnci/93.22.1714. [DOI] [PubMed] [Google Scholar]
- 23.Lewis JS, Osipo C, Meeke K, Jordan VC. Estradiol induced apoptosis in a breast cancer cell line resistant to estrogen deprivation. J Steroid Biochem. 2005;94:131–41. doi: 10.1016/j.jsbmb.2004.12.032. [DOI] [PubMed] [Google Scholar]
- 24.Lewis JS, Meeke K, Osipo C, Ross EA, Kidawi N, Li T, et al. Intrinsic mechanism of estradiol-induced apoptosis in breast cancer cells resistant to estrogen deprivation. J Natl Cancer Inst. 2005;97:1746–59. doi: 10.1093/jnci/dji400. [DOI] [PubMed] [Google Scholar]
- 25.Lewis JS, Cheng D, Jordan VC. Targeting oestrogen to kill the cancer but not the patient. British J Cancer. 2004;90:822–32. doi: 10.1038/sj.bjc.6601627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maximov PY, Lewis-Wambi JS, Jordan VC. The paradox of oestradiol-induced breast cancer cell growth and apoptosis. Curr Signal Transduct Ther. 2009:4. doi: 10.2174/157436209788167484. (In Press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jordan VC. The 38th David A. Karnofsky lecture: the paradoxical actions of estrogen in breast cancer--survival or death? J Clin Oncol. 2008;26:3073–82. doi: 10.1200/JCO.2008.17.5190. [DOI] [PubMed] [Google Scholar]
- 28.Haddow A, Watkinson JM, Paterson E. Influence of synthetic oestrogens upon advanced malignant disease. Br Med J. 1944;2:393–8. doi: 10.1136/bmj.2.4368.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kennedy BJ. Hormone therapy for advanced breast cancer. Cancer. 1965;18:1551–7. doi: 10.1002/1097-0142(196512)18:12<1551::aid-cncr2820181206>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 30.Lonning PE, Taylor PD, Anker G, Iddon J, Wie L, Jorgensen LM, et al. High-dose estrogen treatment in postmenopausal breast cancer patients heavily exposed to endocrine therapy. Breast Cancer Res Treat. 2001;67:111–6. doi: 10.1023/a:1010619225209. [DOI] [PubMed] [Google Scholar]
- 31.Ariazi EA, Lewis-Wambi JS, Gill SD, Pyle JR, Ariazi JL, Kim HR, et al. Emerging principles for the development of resistance to antihormonal therapy: implications for the clinical utility of fulvestrant. J Steroid Biochem Mol Biol. 2006;102:128–38. doi: 10.1016/j.jsbmb.2006.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jordan VC, Lewis-Wambi J, Kim H, Cunliffe H, Ariazi E, Sharma CG, et al. Exploiting the apoptotic actions of oestrogen to reverse antihormonal drug resistance in oestrogen receptor positive breast cancer patients. Breast. 2007;16(Suppl 2):S105–13. doi: 10.1016/j.breast.2007.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Smith CL, O’Malley BW. Coregulator function: a key to understanding tissue specificity of selective receptor modulators. Endocrine Reviews. 2004;25:45–71. doi: 10.1210/er.2003-0023. [DOI] [PubMed] [Google Scholar]
- 34.Ariazi EA, Jordan VC. Estrogen Receptors as Therapeutic Targets in Breast Cancer. In: Ottow E, Weinmann H, editors. Nuclear Receptors as Drug Targets. Wiley-VCH Verlag GmbH & Co. KGaA; Weinheim: 2008. pp. 127–99. [Google Scholar]
- 35.Strom A, Hartman J, Foster JS, Kietz S, Wimalasena J, Gustafsson JA. Estrogen receptor beta inhibits 17beta-estradiol-stimulated proliferation of the breast cancer cell line T47D. Proc Natl Acad Sci U S A. 2004;101:1566–71. doi: 10.1073/pnas.0308319100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Helguero LA, Faulds MH, Gustafsson JA, Haldosen LA. Estrogen receptors alpha (ERalpha) and beta (ERbeta) differentially regulate proliferation and apoptosis of the normal murine mammary epithelial cell line HC11. Oncogene. 2005;24:6605–16. doi: 10.1038/sj.onc.1208807. [DOI] [PubMed] [Google Scholar]
- 37.Prossnitz ER, Arterburn JB, Smith HO, Oprea TI, Sklar LA, Hathaway HJ. Estrogen Signaling through the Transmembrane G Protein-Coupled Receptor GPR30. Annu Rev Physiol. 2008;70:165–90. doi: 10.1146/annurev.physiol.70.113006.100518. [DOI] [PubMed] [Google Scholar]
- 38.Bologa CG, Revankar CM, Young SM, Edwards BS, Arterburn JB, Kiselyov AS, et al. Virtual and biomolecular screening converge on a selective agonist for GPR30. Nat Chem Biol. 2006;2:207–12. doi: 10.1038/nchembio775. [DOI] [PubMed] [Google Scholar]
- 39.Lewis-Wambi JS, Kim HR, Wambi C, Patel R, Pyle JR, Klein-Szanto AJ, et al. Buthionine sulfoximine sensitizes antihormone-resistant human breast cancer cells to estrogen-induced apoptosis. Breast Cancer Res. 2008;10:R104. doi: 10.1186/bcr2208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Goetz MP, Rae JM, Suman VJ, Safgren SL, Ames MM, Visscher DW, et al. Pharmacogenetics of tamoxifen biotransformation is associated with clinical outcomes of efficacy and hot flashes. J Clin Oncol. 2005;23:9312–8. doi: 10.1200/JCO.2005.03.3266. [DOI] [PubMed] [Google Scholar]
- 41.Folkman J. Angiogenesis: an organizing principle for drug discovery? Nat Rev Drug Discov. 2007;6:273–86. doi: 10.1038/nrd2115. [DOI] [PubMed] [Google Scholar]
- 42.Ma J, Waxman DJ. Combination of antiangiogenesis with chemotherapy for more effective cancer treatment. Mol Cancer Ther. 2008;7:3670–84. doi: 10.1158/1535-7163.MCT-08-0715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Aesoy R, Sanchez BC, Norum JH, Lewensohn R, Viktorsson K, Linderholm B. An autocrine VEGF/VEGFR2 and p38 signaling loop confers resistance to 4-hydroxytamoxifen in MCF-7 breast cancer cells. Mol Cancer Res. 2008;6:1630–8. doi: 10.1158/1541-7786.MCR-07-2172. [DOI] [PubMed] [Google Scholar]
- 44.Ellis M, Dehdahti F, Kommareddy A, Jamalabadi-Majidi S, Crowder R, Jeffe DB, Gao F, Fleming G, Silverman P, Dickler M, et al. A randomized phase 2 trial of low dose (6 mg daily) versus high dose (30 mg daily) estradiol for patients with estrogen receptor positive aromatase inhibitor resistant advanced breast cancer. Cancer Research. 2009;69(Supp):67s. [Google Scholar]
- 45.Swaby RF, Jordan VC. Low-dose estrogen therapy to reverse acquired antihormonal resistance in the treatment of breast cancer. Clin Breast Cancer. 2008;8:124–33. doi: 10.3816/CBC.2008.n.012. [DOI] [PubMed] [Google Scholar]
- 46.Schnelldorfer T, Gansauge S, Gansauge F, Schlosser S, Beger HG, Nussler AK. Glutathione depletion causes cell growth inhibition and enhanced apoptosis in pancreatic cancer cells. Cancer. 2000;89:1440–7. [PubMed] [Google Scholar]
- 47.Bailey HH, Ripple G, Tutsch KD, Arzoomanian RZ, Alberti D, Feierabend C, et al. Phase I study of continuous-infusion L-S,R-buthionine sulfoximine with intravenous melphalan. J Natl Cancer Inst. 1997;89:1789–96. doi: 10.1093/jnci/89.23.1789. [DOI] [PubMed] [Google Scholar]
- 48.Lewis-Wambi JS, Swaby R, Kim H, Jordan VC. Potential of l-buthionine sulfoximine to enhance the apoptotic action of estradiol to reverse acquired antihormonal resistance in metastatic breast cancer. J Steroid Biochem Mol Biol. 2009 doi: 10.1016/j.jsbmb.2008.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sabnis G, Schayowitz A, Goloubeva O, Macedo L, Brodie A. Trastuzumab reverses letrozole resistance and amplifies the sensitivity of breast cancer cells to estrogen. Cancer Res. 2009;69:1416–28. doi: 10.1158/0008-5472.CAN-08-0857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Medina PJ, Goodin S. Lapatinib: a dual inhibitor of human epidermal growth factor receptor tyrosine kinases. Clin Ther. 2008;30:1426–47. doi: 10.1016/j.clinthera.2008.08.008. [DOI] [PubMed] [Google Scholar]
- 51.Di Leo A, Gomez HL, Aziz Z, Zvirbule Z, Bines J, Arbushites MC, et al. Phase III, double-blind, randomized study comparing lapatinib plus paclitaxel with placebo plus paclitaxel as first-line treatment for metastatic breast cancer. J Clin Oncol. 2008;26:5544–52. doi: 10.1200/JCO.2008.16.2578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hay N, Sonenberg N. Upstream and downstream of mTOR. Genes & Development. 2004;18:1926–45. doi: 10.1101/gad.1212704. [DOI] [PubMed] [Google Scholar]
- 53.Boulay A, Rudloff J, Ye J, Zumstein-Mecker S, O’Reilly T, Evans DB, et al. Dual inhibition of mTOR and estrogen receptor signaling in vitro induces cell death in models of breast cancer. Clin Cancer Res. 2005;11:5319–28. doi: 10.1158/1078-0432.CCR-04-2402. [DOI] [PubMed] [Google Scholar]
- 54.Awada A, Cardoso F, Fontaine C, Dirix L, De Greve J, Sotiriou C, et al. The oral mTOR inhibitor RAD001 (everolimus) in combination with letrozole in patients with advanced breast cancer: results of a phase I study with pharmacokinetics. Eur J Cancer. 2008;44:84–91. doi: 10.1016/j.ejca.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 55.O’Regan RM, Osipo C, Ariazi E, Lee ES, Meeke K, Morris C, et al. Development and therapeutic options for the treatment of raloxifene-stimulated breast cancer in athymic mice. Clin Cancer Res. 2006;12:2255–63. doi: 10.1158/1078-0432.CCR-05-2584. [DOI] [PubMed] [Google Scholar]
- 56.Sebolt-Leopold JS. MEK inhibitors: a therapeutic approach to targeting the Ras-MAP kinase pathway in tumors. Curr Pharm Des. 2004;10:1907–14. doi: 10.2174/1381612043384439. [DOI] [PubMed] [Google Scholar]
- 57.Morgillo F, Lee HY. Lonafarnib in cancer therapy. Expert Opin Investig Drugs. 2006;15:709–19. doi: 10.1517/13543784.15.6.709. [DOI] [PubMed] [Google Scholar]
- 58.Garrofe-Ochoa X, Melero-Fernandez de Mera RM, Fernandez-Gomez FJ, Ribas J, Jordan J, Boix J. BAX and BAK proteins are required for cyclin-dependent kinase inhibitory drugs to cause apoptosis. Mol Cancer Ther. 2008;7:3800–6. doi: 10.1158/1535-7163.MCT-08-0655. [DOI] [PubMed] [Google Scholar]