The 2006 outbreak of contact lens–associated Fusarium keratitis resulted in more than 300 cases in the United States in which a commercial lens care product was implicated. In the current study, Fusarium grown as biofilm on silicone hydrogel lenses induced keratitis in a murine model and severity of disease and survival of the organisms were dependent on MyD88, IL-1R1, and TLR4.
Abstract
Purpose.
Fusarium solani and F. oxysporum were the causative organisms of the 2005/2006 outbreak of contact lens–associated fungal keratitis in the United States. The present study was an investigation of the ability of F. oxysporum grown as a biofilm on silicone hydrogel contact lenses to induce keratitis.
Methods.
A clinical isolate of F. oxysporum was grown as a biofilm on lotrafilcon A contact lenses, and a 2-mm diameter punch was placed on the abraded corneal epithelium of either untreated or cyclophosphamide-treated C57BL/6 mice or of IL-1R1−/−, MyD88−/−, TLR2−/−, or TLR4−/− mice. After 2 hours, the lens was removed, and corneal opacification, colony forming units (CFUs), and histopathology were evaluated.
Results.
C57BL/6 mice developed severe corneal opacification within 24 hours and resolved after four days. In contrast, corneal opacification progressed in cyclophosphamide-treated mice, and was associated with unimpaired fungal growth in the cornea, and with hyphae penetrating into the anterior chamber. The phenotype of MyD88−/− and IL-1R−/− mice was similar to that of cyclophosphamide-treated animals, with significantly impaired cellular infiltration and fungal clearance. Although TLR4−/− mice developed a cellular infiltrate and corneal opacification similar to C57BL/6 mice, the CFU count was significantly and consistently higher.
Conclusions.
Fusarium grown as a biofilm on silicone hydrogel contact lenses can induce keratitis on injured corneas, with disease severity and fungal killing dependent on the innate immune response, including IL-1R1, MyD88, and TLR4.
Filamentous fungi such as Fusarium and Aspergillus are an important cause of microbial keratitis in hot and humid regions of the world such as India and southern China, where agriculture-related activity is a major risk factor.1–3 Although these organisms are not a frequent cause of disease in more temperate climates, an outbreak of Fusarium keratitis was reported in 2005 and 2006 in regions of the United States not usually associated with fungal keratitis4,5 and also in France, Hong Kong, and Singapore.6–9 A Centers for Disease Control (CDC) Fusarium investigation team reported 318 cases of Fusarium keratitis in the United States, of which 94% involved soft contact lens wear.10 A subsequent CDC report reported an association with contact lens wear and that the number of cases of Fusarium keratitis dropped sharply after the withdrawal of a commercial lens care solution (ReNu with MoistureLoc; Bausch & Lomb, Tampa, FL).11
Fusarium attaches firmly to and can even penetrate soft contact lenses12; therefore, the ability of Fusarium to form a biofilm on lenses or lens cases is a possible risk factor for developing keratitis.13–15 We demonstrated previously that clinical isolates of Fusarium can form biofilm on soft contact lenses, that biofilm architecture depends on the type of contact lens, and that Fusarium growing as a biofilm is more resistant to antimycotics and contact lens solutions than are planktonic forms of the same organisms.16 We also characterized the host response in the cornea in a prior study using a murine model of keratitis in which conidia are injected into the corneal stroma.17
In the present study, we developed a model of contact lens–associated Fusarium keratitis, in which organisms are grown as biofilm on silicone hydrogel lenses and are then placed on an abraded mouse cornea. We found that Fusarium grown under those conditions, where hyphae rather than conidia are the stage of growth that infect the cornea, induce keratitis that is regulated by innate immunity, in particular by the IL-1 receptor, Toll-like receptor (TLR)-4, and the common adaptor molecule MyD88.
Methods
Source of Fusarium
Fusarium oxysporum FOCS3-a strain (MRL8996) was isolated from a case of contact lens–associated fungal keratitis during the 2005 to 2006 outbreak, and was used in our previous studies on biofilm formation and in trauma-induced keratitis.16,17 Animals were managed according to the ARVO Statement for the Use of Animals in Ophthalmic and Vision Research.
Fusarium Culture and Biofilm Formation
Fusarium was cultured at 37°C in Sabouraud dextrose broth (SDB; Difco Laboratories, Detroit, MI) in a shaking incubator. For biofilm development, conidia were harvested from a 40-hour broth culture by standard filtration methods and counted, and 1 × 106 conidia in PBS were incubated with lotrafilcon A contact lenses (purchased from CibaVision, Duluth, MN) for 90 minutes at 37°C (adherence phase). After the lenses were gently washed in 4 mL PBS, they were incubated in SDB at 37°C for 48 hours on a rocking platform (biofilm growth phase). We have reported that these culture conditions lead to development of densely packed, live hyphae on the contact lens, which were positive to tetrazolium XTT for live organisms and to concanavalin A (ConA), which stains mannan residues on the fungal cell wall and in extracellular matrix.16
Source of Mice
C57BL/6 mice and IL-1R1−/− mice (6–8 weeks old) were purchased from the Jackson Laboratory (Bar Harbor, ME). TLR2−/−, TLR4−/−, and MyD88−/− mice were obtained from Shizuo Akira (Research Institute for Microbial Disease; Osaka University, Osaka, Japan).
Murine Model of Fusarium Biofilm-Induced Keratitis
Mice were anesthetized by intraperitoneal injection of 0.4 mL 2,2,2-tribromoethanol, and the corneal epithelium was subjected to either three parallel scratches or abrasion of a 1-mm diameter area of the central corneal epithelium (Algerbrush; Richmond Products, Albuquerque, NM), as described in our previous studies.18,19 A 2-mm diameter punch from the contact lenses with attached biofilm was then placed on the abraded corneal surface. After 2 hours in which the mice remained anesthetized on a heating pad, the contact lenses were removed. At each time point thereafter, corneas were examined by bright field microscopy, mice were euthanatized, and eyes were either homogenized and the number of CFUs was determined, or eyes were processed for histology.
Quantification of Fungi in Infected Eyes
Whole eyes were homogenized under sterile conditions in 1 mL PBS (Mixer Mill MM300; Qiagen, Valencia, CA) at 33 Hz for 4 minutes. A series of log dilutions were performed in replicate, and plated onto Sabouraud's agar (Difco). The plates were incubated at 37°C for 40 hours, and the number of CFUs (in the lowest dilution) was determined by direct counting. The lower limit of detection was 10 organisms.
Histologic Preparations
For histologic analysis, the eyes were fixed in formaldehyde and embedded in paraffin. Five-micrometer sections were stained by periodic acid-Schiff (PAS) solution (Sigma-Aldrich, St. Louis, MO), counterstained with hematoxylin, and examined by light microscopy.
Detection of Cytokines in the Cornea
Mouse corneas were excised using a 2-mm trephine, and corneal tissue was homogenized (Mixer Mill MM300; Qiagen) for 4 minutes at 30 cycles per second. After centrifugation, cytokine levels in soluble corneal extracts were determined by sandwich ELISA according to the manufacturer's directions (R&D Systems, Minneapolis, MN). Absorption was measured at 450 nm on a microplate reader (VersaMax with SoftMaxPro software 4.7.1; Molecular Devices, Sunnyvale, CA).
Statistics
Statistical significance (P < 0.05) was determined with either an unpaired Students t-test or ANOVA with the Tukey post hoc analysis for multiple comparisons (Prism 4; GraphPad, San Diego, CA).
Results
Contact Lens–Associated Fusarium Keratitis in Normal and Immunosuppressed C57BL/6 Mice
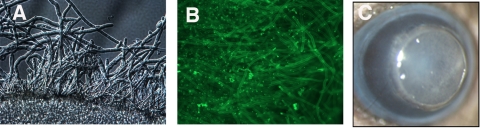
We reported that biofilm architecture varies according to silicone hydrogel lens type and that a more adherent biofilm forms on lotrafilcon lenses than on other lens types.16 Fusarium conidia were therefore incubated with lotrafilcon A silicone hydrogel contact lenses (CibaVision) for 2 hours and washed, and biofilm was allowed to develop over 48 hours, as described.16 Figure 1A shows a fully developed biofilm imaged by DIC microscopy. Extracellular matrix, including mannan residues on hyphae, were detected by FITC-labeled ConA (Fig. 1B).
Figure 1.
Murine model of Fusarium biofilm keratitis. Fusarium conidia were incubated 90 minutes with lotrafilcon A contact lenses, washed, and incubated a further 48 hours. (A) Fusarium hyphae associated with the contact lens (DIC microscopy). (B) After incubation with FITC-ConA, showing hyphae and extracellular matrix. (C) Murine model: 2-mm-diameter punch of a contact lens with attached Fusarium biofilm on the corneal surface of a C57BL/6 mouse. Original magnification: (A, B) ×400; (C) ×20.
To determine the role of the host response in development of keratitis, C57BL/6 mice were either left untreated (immunocompetent) or given systemic cyclophosphamide (immunosuppressed), the corneas were abraded, and a 2-mm diameter silicone hydrogel soft contact lens containing Fusarium biofilm was placed on the ocular surface for 2 hours (Fig. 1C). The lens was then removed, and CFUs were assessed at day 1 to day 4.
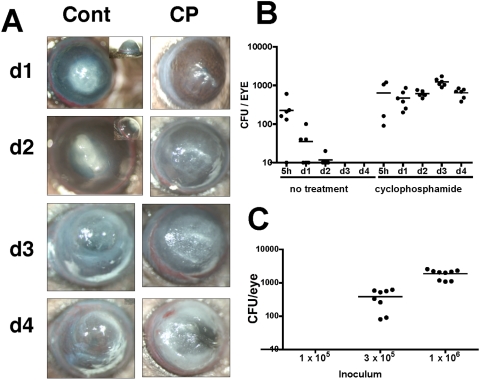
Figure 2A shows representative infected corneas of either normal, immunocompetent C57BL/6 mice, or cyclophosphamide-treated C57BL/6 mice. Immunocompetent C57BL/6 mice developed severe opacification within 24 hours, which progressed for 72 hours but did not develop into more severe disease. In contrast, immunosuppressed C57BL/6 mice developed severe corneal opacification, and the corneas were found to perforate by day 5 (not shown). Corneal opacification was not detected when uninfected contact lenses were added to an abraded cornea; furthermore, intact corneas incubated with Fusarium biofilm did not induce keratitis, indicating that the intact corneal epithelium is an effective barrier to infection.
Figure 2.
Biofilm-associated Fusarium keratitis in untreated and cyclophosphamide-treated C57BL/6 mice. C57BL/6 mice were either untreated or immunosuppressed by intraperitoneal injection of cyclophosphamide (CP). The corneas were abraded, and silicone hydrogel contact lenses (lotrafilcon) with Fusarium biofilm were placed on the ocular surface for 2 hours and examined at indicated time points thereafter. (A) Representative corneas of immunocompetent C57BL/6 mice, which were given a 1-mm-diameter abrasion, exhibited severe opacification on day 1 and day 2, and resolved after day 4. In contrast, corneas of CP-treated mice, which received three parallel scratches, showed increasing opacity, over time and perforation after day 4 (not shown). (B) Eyes of immunocompetent and immunosuppressed (CP) mice were enucleated on days 1 to 4, and CFUs were counted. Data points represent individual corneas and mice, and the data are combined from two repeat experiments. P < 0.05 between untreated and CP-treated mice at each time point except 5 hours. (C) The limit of detection of Fusarium colonies in CP-treated mice. Biofilm was generated with a starting inoculum as shown (1 × 105, 3 × 105, and 1 × 106 conidia per mL PBS). Corneas were then abraded and incubated with contact lenses with adherent biofilm, mice were euthanatized and CFUs were counted on day 1.
Figure 2B shows that in C57BL/6 mice with a 1-mm epithelial abrasion, the number of Fusarium CFUs decreased over 72 hours. In marked contrast, cyclophosphamide-treated mice showed no reduction in CFUs during this time period. The minimum number of conidia required for biofilm formation and for development of keratitis in cyclophosphamide-treated mice is between 1 × 105 and 3 × 105/mL PBS, as shown in Figure 2C. Together, these findings demonstrate that the host response in immunocompetent animals inhibits growth and replication of Fusarium, thereby preventing corneal perforation.
Regulation of Contact Lens–Associated Fusarium Keratitis by IL-1R1 and MyD88
MyD88 is a common adaptor molecule in the signaling pathways of IL-1R1 and all TLRs except TLR3.20 The role of IL-1R1 and My88 in contact lens biofilm–associated fungal keratitis was determined by abrading corneas of C57BL/6, IL-1R1−/−, and MyD88−/− mice with three parallel scratches, and placing contact lenses with adherent Fusarium biofilm on the corneal surface as before.
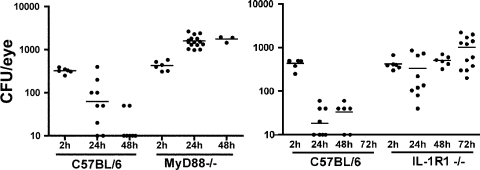
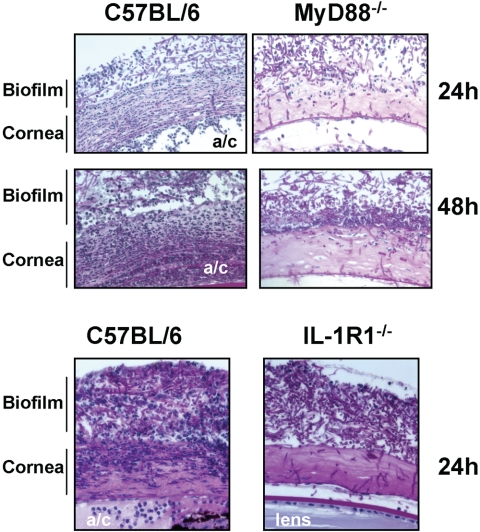
As shown in Figure 3, the number of CFUs recovered from the C57BL/6 mice decreased at 24 hours and 48 hours, and Fusarium were not detected after 72 hours. In contrast, CFUs were significantly elevated in IL-1R1−/− and MyD88−/− mice, implicating a specific role for this pathway in killing Fusarium. Conversely, histologic analysis of C57BL/6 corneas (Fig. 4) showed a pronounced cellular infiltrate on days 1 and 2 after infection, comprised mostly of neutrophils (not shown). In contrast, cellular infiltration was impaired in MyD88−/− and IL-1R1−/− mice at 24 and 48 hours after infection. These observations indicate that IL-1R1 and MyD88 regulate neutrophil recruitment to the corneal stroma in addition to regulating fungal growth.
Figure 3.
Fusarium survival in MyD88−/− and IL-1R1−/− mice. Corneas of C57BL/6, MyD88−/−, and IL-1R1−/− mice were abraded with three parallel scratches and exposed to contact lenses with adherent Fusarium biofilm. At each time point, the eyes were homogenized and the CFUs were assessed. Data points represent individual corneas and mice combined from two similar experiments. P < 0.05 between C57BL/6 and MyD88−/− mice at 24 and 48 hours, and between C57BL/6 and IL-1R1−/− mice at 24, 48, and 72 hours.
Figure 4.
Histopathology of Fusarium keratitis in MyD88−/− and IL-1R1−/− mice. C57BL/6, MyD88−/−, and IL-1R1−/− mice were given a 1-mm diameter corneal abrasion and a contact lens with adherent Fusarium biofilm was placed on the corneal surface, as described in the legend to Figure 1. After 24 or 48 hours, the eyes were processed for histology and stained with PAS. Representative images of five mice per group are shown. Note that cellular infiltration of the corneal stroma was impaired in the MyD88−/− and IL-1R1−/− mice compared with that in the C57BL/6 mice. a/c, anterior chamber.
Dependence of CXCL1/KC Production on MyD88
Earlier reports from our laboratory and others noted that the neutrophil chemokine CXCL1/KC is rapidly produced in the corneal stroma and that neutrophil recruitment to this site is dependent on production of CXCL1 and on expression of CXCR2 on neutrophils.21–24 We therefore examined CXCL1 expression in corneas after exposure to Fusarium biofilm. Corneas of the C57BL/6 and MyD88−/− mice were abraded by three parallel scratches, and a 2-mm diameter punch from a contact lens with attached Fusarium biofilm was placed on the corneal surface. After 3 hours, the corneas were dissected and homogenized, and CXCL1 production was measured by ELISA.
As shown in Figure 5, CXCL1 levels were significantly higher in biofilm-coated corneas than in the trauma control in which the corneas were similarly abraded and exposed to contact lenses with no biofilm. In contrast to the infected C57BL/6 mice, CXCL1 production in MyD88−/− mice exposed to Fusarium biofilm was significantly reduced, indicating that this adaptor molecule is essential for production of CXCL1.
Figure 5.
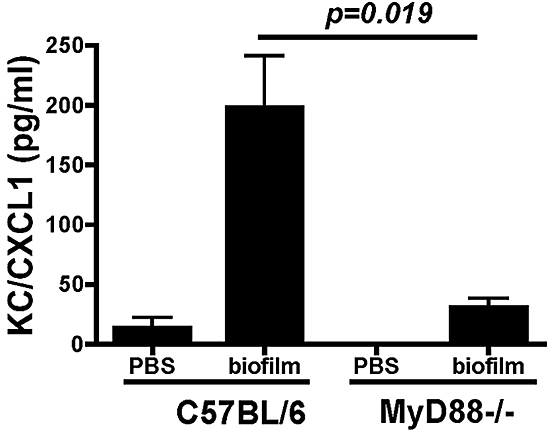
CXCL1/KC production in MyD88−/− mice after infection with Fusarium biofilm on contact lenses. The corneas of the C57BL/6 and MyD88−/− mice were abraded with three parallel scratches and exposed to lenses with adherent Fusarium biofilm. After 3 hours, the corneas were dissected and homogenized, and CXCL1/KC was measured by ELISA. Data are expressed as the mean ± SEM of five mice per group and are representative of results in two experiments.
TLR4-Dependent Fungal Killing in Contact Lens–Associated Fusarium Keratitis
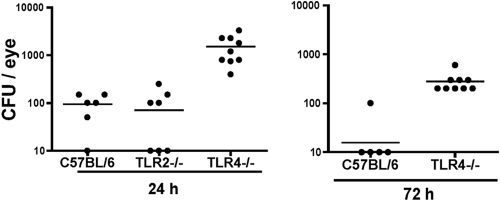
In addition to IL-1R1, MyD88 is recruited to the TIR domain of all Toll-like receptors except TLR3.20 Given that TLR2 and TLR4 mediate the host response to pathogenic fungi in other models of infection,25,26 we next examined their role in Fusarium keratitis. Corneas of C57BL/6, TLR2−/−, and TLR4−/− mice were abraded by three parallel scratches as before, and a silicone hydrogel lens punch with adherent Fusarium biofilm was placed on the ocular surface. After 24 hours, the eyes were homogenized and the number of CFUs was determined. As shown in Figure 6, the mean CFUs in TLR4−/− mice was >1 log higher than in the C57BL/6 and TLR2−/− mice at 24 and 72 hours. There were no significant differences in corneal opacity or cellular infiltration between the TLR4−/− and C57BL/6 mice (data not shown), indicating that TLR4 regulates fungal killing but not cell recruitment to the cornea.
Figure 6.
Fusarium keratitis in TLR2−/− and TLR4−/− mice. Corneas of C57BL/6, TLR2−/−, and TLR4−/− mice were abraded with three parallel scratches and exposed to contact lenses with Fusarium biofilm, as described in the legend to Figure 2. At 24 and 72 hours, the eyes were homogenized and CFUs were assessed. Data points represent individual corneas in two separate experiments. P < 0.001; ANOVA at 24 hours between C57BL/6 and TLR4−/− mice and between the TLR2−/− and TLR4−/− mice and 72-hour data between the C57BL/6 and TLR4−/− mice.
Discussion
Biofilm formation allows bacteria and fungi to reside within an environmental matrix that is relatively resistant to antimicrobial agents.27,28 Organisms can also form biofilm on abiotic surfaces such as catheters, contact lenses, and intraocular lenses.27 For example, Candida albicans forms biofilm on catheters that is dependent on downregulation of alcohol dehydrogenase28,29; however, the biochemical basis for Fusarium biofilm formation has yet to be determined. We reported in a prior study that the morphology of Fusarium biofilm differs according to the chemistry and water content of silicone hydrogel contact lenses and noted that Fusarium forms a dense, tightly adherent biofilm on lotrafilcon A lenses.16
In the current study, we demonstrated that incubation of lotrafilcon A lenses containing Fusarium biofilm with the abraded cornea resulted in the development of severe keratitis in immunocompetent C57BL/6 mice, with corneal opacification evident within 24 hours and remaining high for more than 72 hours. Histologic examination showed the biofilm on the abraded corneal epithelium, with hyphae present at the corneal surface, in the corneal stroma, and in the anterior chamber, having penetrated Descemet's membrane. Our findings also showed an intense neutrophil infiltrate in each of these sites, apparently from limbal and iris vessels. The tissue damage is most likely a result of secretion of proteolytic enzymes by Fusarium and by neutrophils. Neutrophils can also kill Fusarium and other filamentous fungi by binding to the hyphae and secreting reactive oxygen species such as superoxide and hydrogen peroxide.31 In addition to neutrophils, a recent study showed a role for macrophages in Fusarium keratitis,32 and we found a role for macrophages in Aspergillus keratitis (Pearlman E, unpublished results, 2009).
Given that the incidence of infection is low despite the widespread presence of Fusarium in the environment, susceptibility is most likely related to trauma to the corneal surface that is sufficient to allow penetration of fungal hyphae on the contact lenses. Infection is also associated with poor lens care habits that can lead to development of biofilm.12,13
Earlier reports of experimental fungal keratitis showed an important role of the host response in regulating disease, as immunosuppressed animals showed impaired cellular infiltration of the cornea and impaired fungal killing.33–36 Our current findings using cyclophosphamide-immunosuppressed mice infected with Fusarium grown as biofilm on contact lenses are consistent with those reports, as the cyclophosphamide-treated mice had significantly impaired capability of killing the fungus.36 We extended these studies by identifying specific mediators of the host cell response. We found that the IL-1R1−/− and MyD88−/− mice had a phenotype similar to that of the cyclophosphamide-treated mice, with uncontrolled fungal growth, leading to corneal perforation. MyD88 is an adaptor molecule that is recruited early in the signaling pathway of IL-1R1 and which serves as a platform for recruitment of IRAK, IRAK4, and TRAF6. Phosphorylation of these kinases leads to NFκB formation and translocation into the nucleus and production of neutrophil chemotactic cytokines such as CXCL1.37,38 MyD88 is also essential for TLR2 and TLR4 signaling, and although TLR2 and TLR4 have no apparent role in the development of corneal opacification, TLR4−/− mice have an impaired ability to clear the infection, implicating this receptor in fungal killing as. We reported similar results in a model of trauma-induced Fusarium keratitis in which conidia are injected directly into the corneal stroma.17 In that study, the TLR4−/− and TLR2/4−/− mice had impaired fungal clearance, although the organisms were eventually cleared. Taken together with current findings, we suggest that TLR4 expression on neutrophils is important in recognition and killing of fungal hyphae.27 These independent observations demonstrate that despite differences in fungal biofilm and resident corneal cell type that recognize conidia and hyphae (Table 1), there are common mediators that regulate the host response to fungal pathogens. Similar results were detected in a model of Aspergillus keratitis (Pearlman E, unpublished observations, 2009).
Table 1.
Trauma versus Contact Lens–Associated Fusarium Keratitis
| Trauma | Contact Lenses | |
|---|---|---|
| Invasive stage | Conidia | Hyphae |
| Site of initial infection | Corneal stroma | Corneal epithelium |
| Primary responding (bone marrow derived) resident cells | Macrophages and dendritic cells in corneal stroma | Langerhans cells in corneal epithelium |
| Secondary responding cells | Keratocytes/fibroblasts | Epithelial cells |
| Infiltrating cells | Neutrophils, macrophages | Neutrophils, macrophages |
| Innate immune response | IL- 1R1/MyD88 | IL- 1R1/MyD88 |
| Role for TLRs | TLR4-dependent killing | TLR4-dependent killing |
As noted earlier, epidemiologic evidence indicates that contact lens wear is a major risk factor for Fusarium keratitis in industrialized countries, whereas agriculture-related trauma is the primary risk factor for Fusarium and Aspergillus keratitis in the southern United States and in developing countries. Table 1 shows a comparison of contact lens–associated with trauma or agriculture–associated clinical manifestations based on the most likely life cycle stage that initiates infection and a comparison of the host responses as examined in our current and recent studies in murine models of Fusarium keratitis.17 First, in Fusarium keratitis caused by biofilm on contact lenses, hyphae are in direct contact with the ocular surface and are therefore likely to be the invading life cycle stage. In contrast, trauma- and agriculture-associated disease is most likely due to penetration of conidia into the corneal stroma after injury. Conidia then germinate in the stroma and develop into hyphae, which actively penetrate the corneal stroma and anterior chamber. Although it is difficult to measure directly, there also appeared to be a greater fungal mass in the biofilm model than the trauma model in which 10,000 conidia are injected. Differences in host cell recognition of hyphae compared with swollen conidia may involve expression of fungal cell wall components such as β-glucan, which depends on the lifecycle stage of Aspergillus26,39 and likely also of Fusarium. Expression of dectin 1, which is the receptor for β-glucan, may also determine the outcome of disease. Future studies will focus on the role of pathogen-recognition molecules such as C-type lectins, which regulate pulmonary infections caused by Candida and Aspergillus species.40–43
Second, the host response will depend on which resident cells in the cornea recognize invading fungal pathogens at any stage. For example, the primary cells that respond to Fusarium hyphae on contact lenses are likely to be the resident population of Langerhans-like cells in the corneal epithelium, and a secondary responding cell population is likely to be the epithelial cells. In contrast, germinating conidia in the stroma are likely to activate resident stromal macrophages and dendritic cells as first-responder cells, with stromal fibroblasts, derived from activated keratocytes as the secondary responders. The role of resident bone marrow–derived cells may therefore determine the outcome of fungal infection, as we recently demonstrated in chimeric mice and fas-expressing macrophages and dendritic cells that resident bone marrow–derived cells are essential for LPS/TLR4–induced corneal inflammation.44
Third, in the present study, as in trauma-induced keratitis, IL-1R1/MyD88 signaling regulated chemokine production and neutrophil recruitment in biofilm-induced keratitis (Table 1), whereas TLR4, but not TLR2, regulated fungal killing.17 Independent observations from both models strengthen the notion that the IL-1R1/MyD88 and the TLR4/MyD88 pathways are important in Fusarium keratitis.
Although we used a single clinical isolate of Fusarium oxysporum, human traumatic- and contact lens–associated Fusarium keratitis is also caused by F. solani. In future studies, we will examine other clinical isolates to determine whether there are differences in the host response.
Acknowledgments
The authors thank Catherine Dollar and Scott Howell for assistance and expertise in histology and imaging, respectively, and Ahmed Tarabishy and Sixto Leal for many helpful discussions.
Footnotes
Supported by National Institutes of Health Grants R01EY18612 (EP), P30EY11373 (EP), and R01DE17846 (MAG), and by The Research to Prevent Blindness Foundation, and the Ohio Lions Eye Research Foundation.
Disclosure: Y. Sun, None; J. Chandra, None; P. Mukherjee, None; L. Szczotka-Flynn, None; M.A. Ghannoum, None; E. Pearlman, None
References
- 1.Bharathi MJ, Ramakrishnan R, Meenakshi R, Padmavathy S, Shivakumar C, Srinivasan M. Microbial keratitis in South India: influence of risk factors, climate, and geographical variation. Ophthalmic Epidemiol 2007;14:61–69 [DOI] [PubMed] [Google Scholar]
- 2.Chowdhary A, Singh K. Spectrum of fungal keratitis in North India. Cornea 2005;24:8–15 [DOI] [PubMed] [Google Scholar]
- 3.Xie L, Zhong W, Shi W, Sun S. Spectrum of fungal keratitis in north China. Ophthalmology 2006;113:1943–1948 [DOI] [PubMed] [Google Scholar]
- 4.Alfonso EC, Cantu-Dibildox J, Munir WM, et al. Insurgence of Fusarium keratitis associated with contact lens wear. Arch Ophthalmol 2006;124:941–947 [DOI] [PubMed] [Google Scholar]
- 5.Alfonso EC, Miller D, Cantu-Dibildox J, O'Brien TP, Schein OD. Fungal keratitis associated with non-therapeutic soft contact lenses. Am J Ophthalmol 2006;142:154–155 [DOI] [PubMed] [Google Scholar]
- 6.Khor WB, Aung T, Saw SM, et al. An outbreak of Fusarium keratitis associated with contact lens wear in Singapore. JAMA 2006;295:2867–2873 [DOI] [PubMed] [Google Scholar]
- 7.Saw SM, Ooi PL, Tan DT, et al. Risk factors for contact lens-related fusarium keratitis: a case-control study in Singapore. Arch Ophthalmol 2007;125:611–617 [DOI] [PubMed] [Google Scholar]
- 8.Gaujoux T, Chatel MA, Chaumeil C, Laroche L, Borderie VM. Outbreak of contact lens-related Fusarium keratitis in France. Cornea 2008;27:1018–1021 [DOI] [PubMed] [Google Scholar]
- 9.Ma SK, So K, Chung PH, Tsang HF, Chuang SK. A multi-country outbreak of fungal keratitis associated with a brand of contact lens solution: the Hong Kong experience. Int J Infect Dis 2009;13:443–448 [DOI] [PubMed] [Google Scholar]
- 10.Chang DC, Grant GB, O'Donnell K, et al. Multistate outbreak of Fusarium keratitis associated with use of a contact lens solution. JAMA 2006;296:953–963 [DOI] [PubMed] [Google Scholar]
- 11.Grant GB, Fridkin S, Chang DC, Park BJ. Postrecall surveillance following a multistate fusarium keratitis outbreak: 2004 through 2006. JAMA 2007;298:2867–2868 [DOI] [PubMed] [Google Scholar]
- 12.Ahearn DG, Simmons RB, Zhang S, et al. Attachment to and penetration of conventional and silicone hydrogel contact lenses by Fusarium solani and Ulocladium sp. in vitro. Cornea 2007;26:831–839 [DOI] [PubMed] [Google Scholar]
- 13.Ahearn DG, Zhang S, Stulting RD, et al. Fusarium keratitis and contact lens wear: facts and speculations. Med Mycol 2008;46:397–410 [DOI] [PubMed] [Google Scholar]
- 14.Dyavaiah M, Ramani R, Chu DS, et al. Molecular characterization, biofilm analysis and experimental biofouling study of Fusarium isolates from recent cases of fungal keratitis in New York State. BMC Ophthalmol 2007;7:1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang S, Ahearn DG, Stulting RD, et al. Differences among strains of the Fusarium oxysporum-F. solani complexes in their penetration of hydrogel contact lenses and subsequent susceptibility to multipurpose contact lens disinfection solutions. Cornea 2007;26:1249–1254 [DOI] [PubMed] [Google Scholar]
- 16.Imamura Y, Chandra J, Mukherjee PK, et al. Fusarium and Candida albicans biofilms on soft contact lenses: model development, influence of lens type, and susceptibility to lens care solutions. Antimicrob Agents Chemother 2008;52:171–182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tarabishy AB, Aldabagh B, Sun Y, et al. MyD88 regulation of Fusarium keratitis is dependent on TLR4 and IL-1R1 but not TLR2. J Immunol 2008;181:593–600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Johnson AC, Heinzel FP, Diaconu E, et al. Activation of toll-like receptor (TLR)2, TLR4, and TLR9 in the mammalian cornea induces MyD88-dependent corneal inflammation. Invest Ophthalmol Vis Sci 2005;46:589–595 [DOI] [PubMed] [Google Scholar]
- 19.Khatri S, Lass JH, Heinzel FP, et al. Regulation of endotoxin-induced keratitis by PECAM-1, MIP-2, and toll-like receptor 4. Invest Ophthalmol Vis Sci 2002;43:2278–2284 [PubMed] [Google Scholar]
- 20.O'Neill LA, Bowie AG. The family of five: TIR-domain-containing adaptors in Toll-like receptor signalling. Nat Rev Immunol 2007;7:353–364 [DOI] [PubMed] [Google Scholar]
- 21.Hall LR, Diaconu E, Patel R, Pearlman E. CXC chemokine receptor 2 but not C-C chemokine receptor 1 expression is essential for neutrophil recruitment to the cornea in helminth-mediated keratitis (river blindness). J Immunol 2001;166:4035–4041 [DOI] [PubMed] [Google Scholar]
- 22.Lin M, Carlson E, Diaconu E, Pearlman E. CXCL1/KC and CXCL5/LIX are produced selectively by corneal fibroblasts and mediate neutrophil infiltration to the corneal stroma in LPS keratitis. J Leukoc Biol 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Khan S, Cole N, Hume EB, et al. The role of CXC chemokine receptor 2 in Pseudomonas aeruginosa corneal infection. J Leukoc Biol 2007;81:315–318 [DOI] [PubMed] [Google Scholar]
- 24.Lin M, Jackson P, Tester AM, et al. Matrix metalloproteinase-8 facilitates neutrophil migration through the corneal stromal matrix by collagen degradation and production of the chemotactic peptide Pro-Gly-Pro. Am J Pathol 2008;173:144–153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Netea MG, Brown GD, Kullberg BJ, Gow NA. An integrated model of the recognition of Candida albicans by the innate immune system. Nat Rev Microbiol 2008;6:67–78 [DOI] [PubMed] [Google Scholar]
- 26.Netea MG, Gow NA, Munro CA, et al. Immune sensing of Candida albicans requires cooperative recognition of mannans and glucans by lectin and Toll-like receptors. J Clin Invest 2006;116:1642–1650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Behlau I, Gilmore MS. Microbial biofilms in ophthalmology and infectious disease. Arch Ophthalmol 2008;126:1572–1581 [DOI] [PubMed] [Google Scholar]
- 28.Mukherjee PK, Mohamed S, Chandra J, et al. Alcohol dehydrogenase restricts the ability of the pathogen Candida albicans to form a biofilm on catheter surfaces through an ethanol-based mechanism. Infect Immun 2006;74:3804–3816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mukherjee PK, Zhou G, Munyon R, Ghannoum MA. Candida biofilm: a well-designed protected environment. Med Mycol 2005;43:191–208 [DOI] [PubMed] [Google Scholar]
- 30.Norred WP, Bacon CW, Plattner RD, Vesonder RF. Differential cytotoxicity and mycotoxin content among isolates of Fusarium moniliforme. Mycopathologia 1991;115:37–43 [DOI] [PubMed] [Google Scholar]
- 31.Hu J, Wang Y, Xie L. Potential role of macrophages in experimental keratomycosis. Invest Ophthalmol Vis Sci 2009;50:2087–2094 [DOI] [PubMed] [Google Scholar]
- 32.Nathan C. Neutrophils and immunity: challenges and opportunities. Nat Rev 2006;6:173–182 [DOI] [PubMed] [Google Scholar]
- 33.Kiryu H, Yoshida S, Suenaga Y, Asahi M. Invasion and survival of Fusarium solani in the dexamethasone-treated cornea of rabbits. J Med Vet Mycol 1991;29:395–406 [PubMed] [Google Scholar]
- 34.O'Day DM, Ray WA, Head WS, Robinson RD, Williams TE. Influence of corticosteroid on experimentally induced keratomycosis. Arch Ophthalmol 1991;109:1601–1604 [DOI] [PubMed] [Google Scholar]
- 35.Forster RK, Rebell G. Animal model of Fusarium solani keratitis. Am J Ophthalmol 1975;79:510–515 [DOI] [PubMed] [Google Scholar]
- 36.Wu TG, Keasler VV, Mitchell BM, Wilhelmus KR. Immunosuppression affects the severity of experimental Fusarium solani keratitis. J Infect Dis 2004;190:192–198 [DOI] [PubMed] [Google Scholar]
- 37.Takeda K, Akira S. TLR signaling pathways. Semin Immunol 2004;16:3–9 [DOI] [PubMed] [Google Scholar]
- 38.Kawai T, Akira S. TLR signaling. Semin Immunol 2007;19:24–32 [DOI] [PubMed] [Google Scholar]
- 39.Gersuk GM, Underhill DM, Zhu L, Marr KA. Dectin-1 and TLRs permit macrophages to distinguish between different Aspergillus fumigatus cellular states. J Immunol 2006;176:3717–3724 [DOI] [PubMed] [Google Scholar]
- 40.Bellocchio S, Moretti S, Perruccio K, et al. TLRs govern neutrophil activity in aspergillosis. J Immunol 2004;173:7406–7415 [DOI] [PubMed] [Google Scholar]
- 41.Netea MG, Van der Graaf C, Van der Meer JW, Kullberg BJ. Recognition of fungal pathogens by Toll-like receptors. Eur J Clin Microbiol Infect Dis 2004;23:672–676 [DOI] [PubMed] [Google Scholar]
- 42.Luther K, Torosantucci A, Brakhage AA, Heesemann J, Ebel F. Phagocytosis of Aspergillus fumigatus conidia by murine macrophages involves recognition by the dectin-1 beta-glucan receptor and Toll-like receptor 2. Cell Microbiol 2007;9:368–381 [DOI] [PubMed] [Google Scholar]
- 43.van der Graaf CA, Netea MG, Verschueren I, van der Meer JW, Kullberg BJ. Differential cytokine production and Toll-like receptor signaling pathways by Candida albicans blastoconidia and hyphae. Infect Immun 2005;73:7458–7464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chinnery HR, Carlson EC, Sun Y, et al. Bone marrow chimeras and c-fms conditional ablation (Mafia) mice reveal an essential role for resident myeloid cells in lipopolysaccharide/TLR4-induced corneal inflammation. J Immunol 2009;182:2738–2744 [DOI] [PMC free article] [PubMed] [Google Scholar]