Abstract
Introduction:
While CBT has been found to be an effective treatment for anxious older children, it has not been empirically validated in children younger than 8 years. In this study we report on an open pilot trial to establish whether a modified form of CBT can benefit young children.
Methods:
Participants were 37 anxious children aged 37–89 months attending a university anxiety specialty clinic. Symptom severity and functioning were assessed before and after treatment by independent evaluators. Feasibility and acceptability of the intervention were high. Parents attended part of each treatment session and were considered part of the treatment team.
Results:
Patients exhibited significant improvement from pre – to post-treatment assessments after an average of 8.3 treatment sessions, using the Strengths and Difficulties Questionnaire (SDQ) and the Global Assessment of Functioning Scale (GAF) ratings.
Conclusions:
A modified form of CBT with active parent involvement may be a useful tool in treating anxiety disorders in preschool and early school aged children.
Keywords: anxiety, preschool, CBT
Résumé
Introduction:
Bien que la TCC ait fait ses preuves dans le traitement de l’anxiété chez les enfants plus âgés, elle n’a pas été validée empiriquement chez les enfants de moins de huit ans. L’objet de cet essai clinique est de constater si une forme modifiée de la TCC peut être utile aux jeunes enfants.
Méthodologie:
Trente-sept enfants anxieux, âgés de 37 à 89 mois, ont été suivis dans la clinique de l’anxiété d’un hôpital universitaire. Des évaluateurs indépendants ont noté la gravité des symptômes et le fonctionnement des enfants avant et après traitement. La faisabilité et l’acceptabilité de l’intervention étaient élevées. Les parents assistaient à une partie de chaque séance du traitement, et étaient considérés comme faisant partie de l’équipe traitante.
Résultats:
La comparaison, avant et après traitement, des notes obtenues au Questionnaire sur les forces et faiblesses (Strengths and Difficulties Questionnaire - SDQ) et à l’Échelle d’évaluation globale du fonctionnement (Global Assessment of Functioning Scale - GAF) après 8,3 séances de traitement attestait d’une amélioration significative chez les sujets.
Conclusions:
Une forme modifiée de la TCC, assortie de la participation active des parents, est utile pour traiter les troubles anxieux des enfants de trois à sept ans.
Keywords: anxiété, âge préscolaire, TCC
Introduction
Anxiety disorders are the most common form of psychopathology in children and adolescents although there are great variations reported in the actual rates of the conditions. Klein and Pine (2002) reported that 5 – 15% of children exhibit symptoms of an anxiety disorder at some time during their development while Verhulst et al. (1997) found 23% of a large adolescent cohort to show such a disorder. These differences may reflect variations in defining “a disorder” by different authors, but may also be related to age specific peak onset times for specific anxiety disorders. For example, separation anxiety disorder has its onset most often during early childhood while social phobia is more common in adolescence (Wittchen et al., 1999).
Nevertheless, it appears that the overall prevalence of anxiety disorders is virtually identical in preschoolers (ages 2 to 5) and children and adolescents aged 5 to 17 (Egger & Angold, 2004). Egger and colleagues used their recently developed Preschool Age Psychiatric Assessment (PAPA) to assess 307 children aged 2 – 5 for 8 diagnoses and found a rate of 9.5% for anxiety disorders. The PAPA has shown good test-retest reliability over 2 months (Egger et al., 2006) but has not yet been validated against other established preschool symptom check lists such as the CBCL (Achenbach, 1985).
One additional challenge in diagnosing anxious young children is their inability to reliably report on their feelings and behaviours, necessitating questionnaire based information from parents to obtain a diagnosis. This limits the use of traditional assessment tools such as the MASC (March et al., 1997) in young children and may also affect the validity of the PAPA (Egger & Angold, 2004) as it is also based on ratings by caretakers. However, Eggers and her colleagues claim that their reliability data provide good evidence for the observational accuracy of involved parents.
The treatment of young anxious children has received little scientific study. Thus, while there is good evidence for the efficacy of CBT in children aged 8 and older (Kendall et al., 2004), there is presently only one empirically validated psychosocial treatment outcome study for anxious preschool and early school aged children (Monga et al., 2009). In this pilot study, Monga and her group enrolled a total of 32 children aged 5–7 years in a 12-week, carefully developed manualized, CBT group program and compared them to 11 children on a 2.5 -5 months wait period. Groups comprised 5–8 children and parents were mostly seen separately during the time of the group meetings. Results showed that, among others, 43.8% of children no longer met criteria for any Axis I anxiety disorder after the group treatment, based on well validated assessment measures. There is also one promising report of an individualized approach by Scheeringa and colleagues (2007). They discussed two children aged 4 and 6 who had experienced the flooding of New Orleans and showed signs of PTSD, as did their mothers. The results of both these studies indicate that a CBT program including mothers and their young children is not only practically feasible but can lead to a significant decrease of anxiety in both. While commonly used manualized CBT programs for older children, such as the Coping Cat program (Kendall et al., 1992), involve the parents of the treated children only in a few specified sessions, the data by Monga and Scheeringa et al. indicate that parents have to play a more important role in the treatment of preschoolers. Moreover, since the relative cognitive immaturity of young children limits the use of some traditional strategies, such as exploring the evidence for faulty beliefs, the treatment approach must be based on more concrete cognitive abilities as well as external support. Finally, a recent meta-analytic review showed a substantial association between child anxiety and parental control, further highlighting the need to actively involve the parents (van der Bruggen et al., 2008).
The present study is an attempt to evaluate a modified cognitively based individual treatment approach with a larger sample of young anxious children, using age appropriate valid tools and actively involving the parents in the treatment process. More specifically, we hypothesized that preschool aged children will show a significant decrease in anxiety symptoms and improvement of their global psychological functioning following a two to three month period of weekly CBT.
Methods
Sample and Measures:
The present study involves 20 boys and 17 girls, mean age 71.1 months (37 – 89 months), a sub-sample of 250 children who were consecutively referred to a university hospital based child psychiatric anxiety clinic for young children by their respective physicians. This clinic accepted only children younger than 11 years and the present sample made up 73% of the children who were younger than 8 years at the time of referral. Fourteen children in this youngest age group were excluded because their primary diagnosis was Selective Mutism, a condition requiring different forms of treatment (Manassis et al., 2007). All 37 children were English speaking and attended some type of day care or preschool program at least on a part time basis. Eleven had previously been evaluated by community based psychologists and their parents had received advice about appropriate management techniques. When this proved of little or no help, the psychologists either suggested or supported the referral of the children to our clinic. Thirty-two of the children lived with both their biological parents and a majority came from middle class families, using Hollingshead 5 social economic class categories (SES: 1 + 2 = 16; 3 = 19; 4 + 5 = 2). Thirty-five were of Caucasian ethnicity. As the instruments and questionnaires used in this study were routinely given to all children assessed in the OPD of the Department of Psychiatry of the Montreal Children’s Hospital, the study was declared to fall into the category of “quality control” and did not require a specific IRB.
All families were initially screened by the department based intake team, consisting of a social worker and an experienced intake worker who took a brief history of the presenting complaints and family background over the telephone. Parents were asked to fill in questionnaires concerning family background and the child’s development, and to provide a written referral from their physician. Parents and the teacher most familiar with the child at the day care center or school were requested to fill in the Strengths & Difficulties Questionnaire (SDQ) (Goodman, 1997). This is a relatively short (25 items), well validated instrument (Bourdon et al., 2005) that assesses 5 behavioural components (emotional, conduct, ADHD symptoms, peer relationships and prosocial behaviours) in children aged 3 to 17 years. It has an additional scale which records the impact of the child’s behaviour on either parents or teachers. Only when the history (present for at least 3 months) and reported clinical symptoms strongly suggested the presence of an anxiety disorder was a referral to the anxiety clinic accepted.
As the waiting period for an appointment in the clinic was between 3 and 4 months, the primary author phoned each family shortly after receiving the referral to arrange the assessment date and time. This contact allowed for a discussion of the parents’ main concerns and was used to initiate a supportive working alliance between the clinician and the family. Parents were encouraged to contact the primary author during their waiting time if necessary. They were also informed that they would meet with a team of about 6 people at the actual assessment (2 medical students, a social worker, a psychiatric resident, and a master student in drama and art therapy) and that both parents and all siblings attend the first meeting. Families were also told that we would collect follow-up data at the end of the treatment. All families agreed to these conditions.
Assessment and Treatment
The assessment of the family took about 2 hours and consisted of a detailed history of the present illness of the identified patient, past psychiatric, social and medical histories of all family members, a developmental history, a mental status examination of the referred child and a formulation of the case. After the assessment, the team decided on one or more appropriate diagnoses, using DSM-IV criteria, as well as a GAF score for the patient.
The treatment program offered to the children was a modified CBT model, consisting of exposure or exposure and response prevention, learning how to ‘talk back to the brain’ as well as psycho-education for the parents. The modifications were expressly developed for our young patients, i.e., special emphasis was placed on concrete ways to overcome fears and emotional vulnerabilities. In weekly sessions children spent approximately 40 minutes with the primary author, followed by a 20-minute period when one or both parents joined their child. This allowed parents to report on the progress made during the preceding week, be informed about the main issues discussed with the youngster during the initial part of the hour and the home work the therapist and child had agreed on for the following week. They received psycho-education as appropriate.
The actual time with the child was quite structured. During session 1 we reviewed the intake interview and confirmed that the child wanted to get rid of his worries, scary thoughts or obsessive behaviours. We identified the individual worries again, wrote them on the blackboard and established a hierarchy, using a severity rating between 0 and 10. Then the “String Test” was done. Here the child was shown the picture of a boy standing with his eyes closed and holding a string with a small weight (Vollmar, 2004). The therapist would demonstrate with a similar string how it could be moved simply by imagining that this would happen. The child would then do the same test, always with the same result, allowing the therapist to introduce the concept of “mind power” that can be used to “talk back to our brain when it tells us unnecessary scary thoughts”.
Subsequent sessions were structured by having the children initially report on ‘good’ and ‘not so good’ experiences of the past week and recalibrating their anxieties. This was followed by working on one or two individual anxieties or fears, choosing those lower down on the hierarchy, to practice ‘talking back to the brain’ by not listening to it or finding specific distractions. This could involve drawing the demise of a scary thought, use of puppet play or concomitant breathing techniques. The children generally worked very hard on their specific tasks and usually agreed to pursue a specific goal during the subsequent week. During the last 20 minutes parents were given feedback about that session and new goals and their implementation were discussed. In addition, parents received relevant information ranging from the neuro-chemical aspects of anxiety disorders to advice about how to manage their children’s comorbid conditions. At the same time we talked about the neuro-chemical and information processing abnormalities these children showed, e.g., narrow attentional focus on threat cues or distorted memories for scary rather than happy day-to-day events (Pine, 2007). Families also received literature they could use to help their children (e.g., Huebner, 2006). In 2 cases where children appeared to be overwhelmed by their symptoms, medication was offered immediately in addition to the psychological treatment. Otherwise medication was added if no improvement had been observed after 4 to 5 weeks. The standard prescribed medication was Fluoxetine in doses between 4 or 12 mg/day because of its overall safety level and availability in liquid form which allows better titration to provide appropriately small doses. If needed, children were titrated up from 4mg/day to the next higher level after 2–3 weeks.
When the children showed significant clinical improvement, i.e., were reported to have gained either full control over more than 65% of their worries or showed only occasional symptoms overall, appointments were spaced out to biweekly or even monthly treatment sessions. A follow-up visit was arranged 4 to 6 weeks after the last regular appointment. At that time a post-treatment GAF was obtained by the main author and parents were asked to complete another SDQ and to have the child’s teacher do so as well.
Results
As stated above, our sample came primarily from middle class families and most of the parents were married. Interestingly, only 57% of the mothers in our sample were employed, a significantly lower number than the 82.6% of women aged 25 to 44 who work at least on a part time basis in Canada (Canada Year Book, 2008).
Concerning the parents’ life time psychiatric history, table 1 indicates that in 86% of the families at least one parent (N=32) had a history of a psychiatric condition. The severity of the parental disorders was rated on a 4 - point scale (none; diagnosis by a healthcare professional but no treatment, outpatient treatment, and inpatient treatment). In total, 15 parents (41%) had received outpatient treatment and 5 (14%) had been hospitalized for a psychiatric condition at some time in the past. The most common diagnoses among the parents were any Anxiety Disorder and/or Depression (20 cases). There were 2 cases of Substance abuse.
Table 1.
Primary Psychiatric Diagnoses
| Children | Parents | ||
|---|---|---|---|
| Phobia | 4 | Anxiety and/or depression | 20 |
| GAD | 7 | Alcohol + drugs | 2 |
| SAD | 11 | More than one diagnosis | 8 |
| OCD | 8 | Other diagnoses | 2 |
| Other | 7 | No diagnosis | 5 |
GAD: general anxiety disorder
OCD: obsessive compulsive disorder
SAD: separation anxiety disorder
Table 1 also presents the primary diagnosis of the children. As can be seen, they showed a wide range of anxiety disorders.
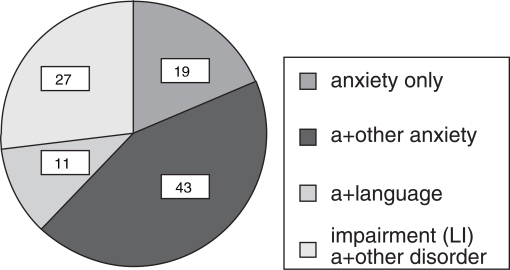
Figure 1 shows the different patterns of comorbidities for the child sample. As shown, 43% of children had more than one anxiety disorder, and another 38% showed comorbidities (mainly ODD) and language disorders.
Figure 1.
Child Comorbidities
Differences between initial and follow up ratings on the SDQ by parents and teachers are presented in table 2. Post-treatment parental ratings show a statistically significant improvement in total as well as emotional functioning and of the impact on the family after treatment. Teacher ratings concur, their somewhat lower overall ratings reflecting the published standardization data. The p-values reported are uncorrected for number of comparisons. The mean ratings on the other four SDQ scales (ADHD, conduct, peer relationships and prosocial behaviours) were within normal range before and after treatment, confirming the validity of the instrument. This must be seen within the context of the overall length of treatment which on average lasted 8.3 sessions for the children, spaced out over an average of 17.2 weeks.
Table 2.
Clinical Results – SDQ Ratings
| Parent Ratings | Teacher Ratings | |
|---|---|---|
| Sum Total - B | 14.2 (1.0) | 11.2 (1.5) |
| Sum Total - A | 9.1 (0.7) | 7.3 (0.9) |
| Difference B-A | 5.1 (0.6)*** | 3.8 (0.8)*** |
| Emotional B | 6.9 (0.4) | 5.7 (0.6) |
| Emotional A | 3.6 (0.3) | 3.7 (0.4) |
| Difference B-A | 3.3 (0.3)*** | 2.0 (0.3)*** |
| Impact B | 5.0 (0.3) | 2.7 (0.4) |
| Impact A | 2.6 (0.3) | 2.3 (0.3) |
| Difference B-A | 2.4 (0.4)*** | 0.4 (0.2)* |
Note: Cells contain mean values for each SDQ measure. The difference and statistical significance is estimated using a two-tailed uncorrected t-test. Standard errors reported in parenthesis. B = before treatment / A = after treatment.
P<.001
P<.05
GAF results support the SDQ data (see table 3), with pre-treatment average GAF ratings of 54.6 (SE 1.3) and post-treatment mean ratings of 67.2 (SE 1.7), a significant improvement.
Table 3.
GAF Scores of Children
| Before treatment | 54.6 (1.3) |
| After treatment | 67.2 (1.7) |
| Difference B-A 12.7 (1.3)*** |
Note: Cells contain mean values for each GAF measure. The difference and statistical significance is estimated using a two-tailed t-test. Standard errors reported in parenthesis. B = before treatment A = after treatment.
P<.001
The presence of a life time psychiatric diagnosis in a parent was not associated with higher baseline SDQ or lower GAF scores of their respective children although it was associated with significantly greater improvement both on SDQ scores and GAF ratings (p<.05). In fact, there was a trend for children with higher initial SDQ and lower GAF ratings to show less improvement overall (p< .1). There was no statistical relationship between the age of the child and the post-treatment outcome, using a 2- group design (children aged 3–5 vs 6–7 years). Mother’s marital and work status was also not related to any outcome data.
Another question was to what extent the use of medication would influence the outcome. Table 4 shows that 10 children (27%) received medication. The dosage of Fluoxetine given varied between 4 and 12 mg/day, while the Risperidone dosage of the one child was 0.25 mg/day. The use of medication was not related to any family variables, including the history of a parental psychiatric diagnosis. However, children who received medication had significantly lower GAF scores (p<.01) and higher baseline sum SDQ ratings by both their parents and teachers at baseline (p<.05 and p<.01 respectively) but not at follow-up. The medicated children also received more treatment sessions (p<.05).
Table 4.
Number of Children Receiving Medication
| None | 27 |
| Fluoxetine | 6 |
| Concerta | 3 |
| Risperidone | 1 |
We finally looked at nine potentially high risk background variables (age; SES, gender; work status of mother; marital status; severity of problem; length of treatment; medication and life time parental psychiatric diagnosis), in an attempt to predict overall CBT success. Only the presence of a past parental psychiatric diagnosis was found to have a statistically significant effect predicting positive treatment outcome (r=.64). This supports the notion that parents with such a history have a better understanding of anxiety, possibly motivating them more to collaborate with professionals in helping their children and/or benefiting personally from being part of the treatment team.
Discussion
Results from this open trial provide initial support for the feasibility and clinical efficacy of CBT for anxious children below the age of 7.5 years in a moderately to highly symptomatic sample, confirming the experiences of Monga et al. (2009). All 37 children and their families completed their individual treatment program, and significant improvement from pre- to post-treatment was evident in the children’s level of anxiety and overall behaviour at home and at school. Parents also reported that their children after treatment placed a significantly lower burden on them and their families. While we obtained follow-up reports from all parents, three teachers did not feel they knew the children well enough because treatment had been terminated during the summer and the children worked with a new teacher or had recently graduated from day care to a preschool setting. In two cases parents did not want new teachers to know about their children’s past problems. However, a separate analysis of the 32 children who had a full data set did not change the overall statistical significance of the results.
The study was done within a university based specialty clinic where assessments are routinely done by a team and different team members are involved in the treatment process. An exception was made in the cases of the present sub-sample of very young children, all of whom were treated by the primary author to limit confounding variables and assure the continuity of care. The cognitive behavioural treatment of this age group presents both advantages and challenges. Strategies like positive self-statements, modeling, positive reinforcement as well as exposure, i.e., thoughtfully initiated desensitization or shaping procedures work well with young children. While their ability to conceptualize and systematically explore evidence is less developed, they grasp abstract concepts when presented in concrete ways. Thus, the “string test” was uniformly seen by the children as evidence that thoughts can change behaviours and that they can be challenged, i.e., one “can talk back to one’s brain”. With the help of their parents, they also generally did their “homework” conscientiously and were often amazed to discover their own strengths.
Our sample was primarily middle class, and in more than 80% one parent presented a life time history of a psychiatric disorder. Many parents told us that they had struggled since childhood to get their own anxieties or depression under control, some having managed to do so only in the recent past. They hoped to cut this struggle short for their children and consequently were eager to work with us. Even though the mothers as a group were highly educated, comparatively few chose to work outside the home, which may be another sign, at least in some cases, of their own anxiety.
The assessment of family psychopathology was restricted to the parents of our child patients because of the clinical nature of the study. While we have no documented evidence for the accuracy of our findings here, the parent’s reports on their own past treatment experience would support the validity of their information. Moreover, the relatively high incidence of anxiety disorders and depression in these parents is in keeping with the literature (Beidel & Turner, 1997). The same applies to the high rate of co-morbid conditions the children displayed (Merikangas, 2005). While neither of those studies dealt with preschool children, the early presentation of anxiety symptoms clearly supports the strong familial base seen in our sample.
As far as the treatment outcome is concerned, a number of points stand out. The children, on average, required only 8 treatment sessions to move from borderline or abnormal to normal SDQ ratings and from moderate or severe symptoms to some mild or transient symptoms according to their ratings on the GAF Scale. While we have no formal data concerning subsequent functioning, only three of the children have returned to the clinic in 3 years and for two of those a couple of booster sessions resolved the apparent setback.
Another question is whether the modified CBT was the sole active ingredient in our treatment or whether non-specific treatment aspects were at play, such as our emotional commitment to the children’s families and their subsequent support of our work. The rather rapid response of the children and their long past history of anxieties (i.e., at least 6 months, as a 3 months history of the condition was required to have an assessment at our clinic and there was an additional 3–4 months wait for the actual appointment) would make the second option more likely. However, the sample contained 10 children who required additional help in the form of medication as this is known to be helpful to more children than CBT alone in older children (Walkup et al., 2008). In contrast to these authors, who compared groups who were assigned to either CBT or combination treatments, we in most cases added medication only after CBT treatment seemed not effective as this was more in line with the wishes of our families.
The fact that CBT was provided by the same therapist made it impossible to explore the transferability of our treatment model. Yet the enhanced treatment response in children whose parents had a history of anxiety/depression suggests being part of the treatment team clearly represented an emotionally meaningful learning experience for them.
Finally, the use of medication needs some discussion. Studies examining the effectiveness of treatment in older anxious or depressed children have repeatedly reported that a combination of pharmacological and psychological therapy is the best strategy for dealing with serious disorders (Brent et al., 1997, Kendall et al., 2004, Walkup et al., 2008). Similar data do not exist for children aged 3 – 7 years. In fact, many of the parents were quite reluctant to accept medication for their children even when they showed serious symptoms such as severe obsessional rituals, or symptoms which made it difficult for them to leave the house. Therefore psychopharmacological treatment of any sort was only provided in the most serious cases.
Clinical implications and limitations
In the present paper we suggest that a modified CBT program can be helpful in assisting even very young children in managing moderate to severe anxieties and that parents are ready to actively participate in this work. While this appears to be the first report where CBT on an individual basis was used as a clinical tool in a larger sample of young children with a variety of anxiety disorders, and supports the results obtained by using CBT in treating preschool within a group setting (Monga et al., (2009), this is a pilot study that requires replication. The study also did not use a standardized diagnostic interview, provided some children with drugs in addition to CBT and the follow-up rating of the GAF was done only by the primary author who had also treated the children. All of these features are obvious limitations of our clinic based work. Future studies should use a random assignment of CBT versus supportive therapy and use multiple experienced therapists to validate treatment effects. This should involve larger samples to allow examining the effectiveness of this form of treatment for individual anxiety disorders. It may also be useful to assess actual change in specific anxiety symptoms after each CBT session as was done in the two cases reported by Scheeringa and colleagues (2007). Finally, future studies should provide for longer term follow-up evaluations.
Based on our experience of the developmental needs of this population, we predict that close involvement of the family will remain a key aspect of any successful treatment of young anxious children. Given the growing understanding that anxiety disorders frequently begin during the preschool years, it is important to develop evidence based and developmentally appropriate interventions.
Acknowledgements/Conflict of Interest
The authors have no financial relationships or conflicts to disclose.
References
- Achenbach TM. The assessment of anxiety in children. In: Tuma AH, Maser JD, editors. Anxiety and the anxiety disorders. Hillsdale, NJ: Erlbaum; 1985. pp. 707–734. [Google Scholar]
- Beidel DC, Turner SM. At risk for anxiety; I. Psychopathology in the offspring of anxious parents. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:918–924. doi: 10.1097/00004583-199707000-00013. [DOI] [PubMed] [Google Scholar]
- Brent DA, Holder D, Kolko D, Birmaher B, Baugher M, Roth C, et al. A clinical psychotherapy trial for adolescent depression comparing cognitive, family and supportive therapy. Archives of General Psychiatry. 1997;54:877–885. doi: 10.1001/archpsyc.1997.01830210125017. [DOI] [PubMed] [Google Scholar]
- Bourdon KH, Goodman R, Donald RS, Simpson G, Rae DS, Koretz DS. The Strengths and Difficulties Questionnaire: US normative data and psychometric properties. Journal of American Academy of Child and Adolescent Psychiatry. 2005;44:557–564. doi: 10.1097/01.chi.0000159157.57075.c8. [DOI] [PubMed] [Google Scholar]
- Canada Year Book . Statistics Canada. Louiseville, Quebec: Transcontinental Gagné.; 2008. p. 277. [Google Scholar]
- Egger HL, Angold A. The Preschool Age Psychiatric Assessment (PAPA): A structured parent interview for diagnosing psychiatric disorders in preschool children. In: DelCarmen-Wiggins R, Carter A, editors. Handbook of infant, toddler, and preschool mental assessment. New York: Oxford University Press; 2004. pp. 223–243. [Google Scholar]
- Egger HL, Erkanli A, Keeler G, Potts E, Walter BK, Angold A. Test-retest reliability of the Preschool Age Psychiatric Assessment (PAPA) Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:538–549. doi: 10.1097/01.chi.0000205705.71194.b8. [DOI] [PubMed] [Google Scholar]
- Goodman R. The Strengths and Difficulties Questionnaire: A research note. Journal of Child Psychology and Psychiatry. 1997;38:581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- Huebner W. Washington, D.C.: Magination Press; 2006. What to do when you worry too much: a kid’s guide to overcoming anxiety. [Google Scholar]
- Kendall PC. Anxiety disorders in youth: Cognitive-Behavioral Interventions. Needham Heights, MA: Allyn & Bacon; 1992. [Google Scholar]
- Kendall PC, Safford S, Flannery-Schroeder E, Webb A. Child anxiety treatment: Outcomes in adolescence and impact of substance use and depression at 7.4-year follow-up. Journal of Consulting and Clinical Psychology. 2004;62:276–287. doi: 10.1037/0022-006X.72.2.276. [DOI] [PubMed] [Google Scholar]
- Klein RG, Pine DS. Anxiety disorders in child and adolescent psychiatry: modern approaches. In: Rutter M, Taylor E, Hersov L, editors. Children and Adolescents Psychiatry. London: Blackwell Scientific; 2002. pp. 486–509. [Google Scholar]
- Manassis K, Tannock R, Garland EJ, Minde K, McInnes A, Clark G. The sounds of silence: Language, cognition and anxiety in selective mutism. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:1187–1195. doi: 10.1097/CHI.0b013e318076b7ab. [DOI] [PubMed] [Google Scholar]
- March J, Parker R, Sullivan J, Stallings P, Conner CK. The Multidimensional Anxiety Scale for Children (MASC): Factor structure, reliability and validity. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:554–565. doi: 10.1097/00004583-199704000-00019. [DOI] [PubMed] [Google Scholar]
- Merikangas KR. Vulnerability factors for anxiety disorders in children and adolescents. Child and Adolescent Psychiatric Clinics of North America. 2005;14:649–679. doi: 10.1016/j.chc.2005.06.005. [DOI] [PubMed] [Google Scholar]
- Monga S, Young A, Owens M. Evaluating a cognitive behavioural group program for five to seven year old children: a pilot study. Depression and Anxiety. 2009;27:243–250. doi: 10.1002/da.20551. [DOI] [PubMed] [Google Scholar]
- Pine D. Research Review: A neuroscience framework for pediatric anxiety disorders. Journal of Child Psychology and Psychiatry. 2007;48:631–648. doi: 10.1111/j.1469-7610.2007.01751.x. [DOI] [PubMed] [Google Scholar]
- Scheeringa MS, Salloum A, Arnberger RA, Weems CF, Amaya-Jackson L, Cohen JA. Feasibility and effectiveness of cognitive-behavioral therapy for post traumatic stress disorder in preschool children: Two case reports. Journal of Traumatic Stress. 2007;20:631–636. doi: 10.1002/jts.20232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van der Bruggen CO, Stams GJJM, Boegels SM. Research Review: The relation between child and parent anxiety and parental control: a meta-analytic review. Journal of Child Psychology and Psychiatry. 2008;49:1257–1269. doi: 10.1111/j.1469-7610.2008.01898.x. [DOI] [PubMed] [Google Scholar]
- Verhulst FC, van der Ende J, Ferdinand RF, Kasius MC. The prevalence of DSM-III-R diagnoses in a national sample of Dutch adolescents. Archives of General Psychiatry. 1997;54:329–336. doi: 10.1001/archpsyc.1997.01830160049008. [DOI] [PubMed] [Google Scholar]
- Vollmar K.1994Autogenes Training mit Kindern Munich: Graefe & Unzer Verlag; page 28 [Google Scholar]
- Walkup JT, Albano AM, Piacentini J, Birmaher B, Compton SN, Sherill JT, et al. Cognitive behavioural therapy, Sertraline, or a combination in childhood anxiety. New England Journal of Medicine. 2008;359(26):2753–2766. doi: 10.1056/NEJMoa0804633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wittchen HU, Stein MB, Kessler RC. Social fears and social phobia in a community sample of adolescents and young adults: Prevalence, risk factors and co-morbidity. Psychological Medicine. 1999;29:309–323. doi: 10.1017/s0033291798008174. [DOI] [PubMed] [Google Scholar]