Abstract
Objective
To evaluate lifetime prevalence and specificity of DSM-IV psychiatric disorders and severity of depressive and manic symptoms at intake in preschool offspring of parents with Disorder I–II.
Methods
121 offspring ages 2–5 years old of 83 parents with Bipolar Disorder and 102 offspring of 65 demographically matched control parents (29 with non-Bipolar psychiatric disorders and 36 without any lifetime psychopathology) were recruited. Parents with Bipolar Disorder were recruited through advertisement and adult outpatient clinics and control parents were ascertained at random from the community. Subjects were evaluated with standardized instruments. All staff were blind to parental diagnoses.
Results
After adjusting for within-family correlations and both biological parents’ non-Bipolar psychopathology, compared to the offspring of the control parents, offspring of parents with Bipolar Disorder, particularly those older than 4 years old, showed an 8-fold increased life-time prevalence of Attention Deficit Hyperactive Disorder (ADHD) and significantly higher rates of ≥ 2 psychiatric disorders. While only 3 offspring of parents with Bipolar Disorder had mood disorders, offspring of parents with Bipolar Disorder, especially those with ADHD and Oppositional-Defiant Disorder, had significantly more severe current manic and depressive symptomatology than the offspring of the controls.
Conclusions
Preschool offspring of parents with Bipolar Disorder are at increased risk for ADHD and demonstrate increased subthreshold manic and depressive symptomatology. Longitudinal follow-up is warranted to evaluate whether these children are at high-risk to develop mood and other psychiatric disorders.
INTRODUCTION
The study of the early manifestations of Bipolar Disorder in youth, particularly during early childhood is of prime importance because of the severe impact that this condition has on the normal psychosocial development of children, their families, and society in general.1–3
The single largest risk factor for the development of Bipolar Disorder is a positive family history of the disorder.3 Therefore, one way to try to identify the prodromal and earliest clinical manifestations of Bipolar Disorder is the study of the offspring of adults with this disorder. This information is critical for developing early interventions that may prevent the onset of pediatric Bipolar Disorder as well as promote the normal psychosocial development of the child. 3, 4
The existent high-risk studies of pediatric Bipolar Disorder have shown that offspring ages 6 to 18 years old of parents with Bipolar Disorder are at increased risk of developing early-onset Bipolar as well as other psychiatric disorders.3, 5–11 The largest of these studies is the Pittsburgh Bipolar Offspring Study (BIOS). 5 The BIOS study showed that school-age offspring of parents with Bipolar Disorder had significantly higher rates of Any Axis-I disorders, Bipolar Spectrum (mostly Not-Otherwise-Specified), Major Depressive, Anxiety, Disruptive Behavior, and Attention Deficit Hyperactive Disorders (ADHD). However, after adjusting for both biological parents’ non-Bipolar psychopathology, the differences in the rates of Major Depressive, Disruptive Behavior, and ADHD disorders were no longer significant.
The above-noted studies were conducted with offspring aged 6 years and older. However, parents with either personal or family history of Bipolar Disorder often question if their preschool children’s behavioral and emotional problems are due to a Bipolar diathesis, since some of these problems are reminiscent of their own or their relatives’ problems during childhood. The few studies of preschool offspring of parents with Bipolar Disorder suggest that in comparison with offspring of control parents (mainly healthy controls), these children have higher rates of observed behavioral disinhibition, disruptive and depressive symptoms, fidgetiness, hyperactivity, disproportionate levels of aggression, and difficulty managing anger and hostile impulses during observed interactions with peers and unknown adults.12–16 Some of these problems (disruptive behaviors) persisted and even increased (e.g., depression) over time. 14 However, further studies are needed because these studies included very small samples of children and parents with Bipolar Disorder and had other methodological limitations delineated elsewhere.5, 7
Epidemiological as well as clinical studies have shown that clinically relevant symptoms and psychiatric disorders are reliably diagnosed in preschool children as young as 2 years old. 17–20 Symptoms of Major Depressive Disorder are also reliably ascertained in this population and are associated with significant psychosocial impairment and high rates of mood disorders in their family members. 18, 19, 21, 22 Although several case reports 23–27 and a recent study 24 showed that preschoolers can be diagnosed with Diagnostic and Statistical Manual-version IV (DSM-IV) 28 Bipolar Disorder, the diagnosis of mania in young children remains controversial and further longitudinal studies are warranted.
The primary goal of this paper is to evaluate whether preschool offspring of parents with Bipolar Disorder had significantly more lifetime DSM-IV Axis-I disorders than a demographically matched sample of preschool offspring of community parents (with and without non-Bipolar psychopathology). In addition to categorical diagnoses, since subthreshold mood symptomatology may precede the onset of full-blown mood disorders, the presence and severity of mood symptoms at intake were explored. Based on the available literature, it was hypothesized that offspring of parents with Bipolar Disorder will have higher rates of ADHD, disruptive behavior, anxiety and mood disorders, and higher ratings on depressive and manic symptom scales when compared with the offspring of control parents.
METHODS
Subjects
Parents (probands)
As part of BIOS, parents with DSM-IV Bipolar-I/II who had preschool children were recruited through advertisement (60%), adult Bipolar studies (9%) and adult outpatient clinics (31%). There were no differences in Bipolar subtype, age of Bipolar-onset, or rates of non-Bipolar Disorders on basis of recruitment source. Exclusion criteria included current or lifetime diagnoses of schizophrenia, mental retardation, and mood disorders secondary to substance abuse, medical conditions, or medications.
Control parents, grouped-matched by age, sex, and neighborhood using the area code and the first 3 digits of the telephone number and the ZIP code of the parents with Bipolar Disorder, were recruited from the community via phone using random dialing by the University Center for Social and Urban Research of the University of Pittsburgh. The exclusion criteria for the control parents were the same as those for the parents with Bipolar Disorder, with the additional requirements that neither of the biological parents could have Bipolar Disorder and they could not have a first-degree relative with Bipolar Disorder. However they could have other psychiatric disorders or be healthy.
Offspring of Bipolar and control parents
Except for children with a condition that impeded their participation in the study (e.g., mental retardation), all offspring ages 2–5 years old from each family were included.
Procedures
The study was approved by the University of Pittsburgh Institutional Review Board. Informed consent was obtained from all parents.
For all parents who participated as probands and 46% (68/148) of the biological co-parents, psychiatric disorders were ascertained face-to-face using the Structured Clinical Interview-DSM-IV (SCID).29 Lifetime ADHD, Disruptive Behavior, and Separation Anxiety Disorders were ascertained using the respective items from the DSM-IV. The SCID kappas were ≥ 0.8.
The Family History-Research Diagnostic Criteria method 30 (plus ADHD, separation, and disruptive behavior disorders items from the Schedule for Affective Disorders and Schizophrenia for School-Age Children, Present and Lifetime Version-K-SADS-PL)31 was used to ascertain psychiatric history from biological co-parents not seen for face-to-face interviews, as well as for siblings, and second-degree relatives.
Parents were interviewed about their children for the presence of lifetime psychiatric disorders using the K-SADS-PL. In addition, the severity of the worst past and current (a month preceding the interview) manic/hypomanic and depressive symptoms were assessed using the Kiddie Mania Rating Scale (K-MRS) 32, 33 and the depression section of K-SADS-Present Episode version (K-DEP) 34 (for these instruments see www.wpic.pitt.edu/research under “assessments”). Individual symptom items are rated on a 5 or 6 point Likert scale (“not present” to “severe” or “extreme”). The sum of 13 manic symptom items (MRS-13, range 0–64: for the scoring instructions see 32), the 5 manic items that do not overlap with ADHD symptoms and that were shown to separate preschool children with Bipolar Disorder from children with and without non-BP psychopathology (MRS-5; range 0–25), 24 and 12-depression items (DEP-12) from the K-DEP that correspond to the DSM symptoms of Major Depressive Disorder (DEP-12; range 0–60) 34 were analyzed (see Table 3 for a list of the symptoms included in the above-noted scales). Pervasive Developmental Disorders were ascertained using a DSM-IV symptom check list (alpha=.9).
Table 3.
Comparisons of the Total Current Depression and Manic Scores and the Caregivers/Teachers Scores between Offspring of Parents with Bipolar Disoder and Offspring of Community Control Parents
| Instrument | Offspring of Parents with Bipolar Disorder | Offspring of Control Parents | Analysis | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| statistic | df | p | Effect size | |||||||
| N | Mean | SD | N | Mean | SD | |||||
| Mania Rating Scale (MRS-13) | 97 | 3.23 | 6.4 | 79 | 0.53 | 1.5 | t=4 | 107.8 | <.001 | 0.58 |
| Mania Rating Scale (MRS-5) | 97 | 0.6 | 1.84 | 79 | 0.05 | 0.27 | t=2.9 | 101.1 | 0.004 | 0.42 |
| Depression Scale-12 (DEP-12) | 99 | 1.63 | 2.7 | 79 | 0.59 | 1.4 | t=3.3 | 152.4 | 0.001 | 0.52 |
| Caregiver/Teacher Report | ||||||||||
| Total Scores | 22 | 51.1 | 9.5 | 29 | 51.9 | 8.3 | t=−0.3 | 49 | .75 | −0.09 |
| Externalizing Scores | 22 | 53.4 | 9.4 | 29 | 52.4 | 7.8 | t=0.4 | 49 | .68 | 0.12 |
| Internalizing Scores | 22 | 48.9 | 9.3 | 29 | 50.3 | 9.6 | t=−0.5 | 49 | .62 | −0.15 |
MRS-13: Elation; irritability; grandiosity; decreased need for sleep; accelerated/pressured of speech; flight of ideas; distractibility; increased activity/hyperactivity; poor judgment; unusual energy; hallucinations; delusions; mood lability.
MRS-5: Elation; grandiosity; accelerated/pressured of speech; flight of ideas; hypersexuality
Depression Scale 12: Depressive mood; excessive or inappropriate guilt; anhedonia/lack of interest/low motivation; fatigue/lack of energy/tiredness; difficulty concentrating/inattention; psychomotor agitation; psychomotor retardation; insomnia; hypersomnia; lack of appetite; increased appetite; suicidal ideation/attempts.
The K-SADS-PL has adequate psychometric properties for evaluating psychiatric disorders in preschool children. 8, 35–37 Details regarding the procedures to use the K-SADS-PL in preschoolers and its psychometrics and limitations as compared with other instruments for preschool children are described in detail elsewhere.37 Briefly, the K-SADS-PL was administered by experienced bachelor’s or master’s level interviewers who were instructed on how to ask developmentally appropriate questions to parents regarding their children’s psychopathology. For example, a normal child is expected to be elated in certain situations and express exaggerated concepts about his abilities and these mood and cognitions cannot be misinterpreted as pathological elation or grandiose ideations. 24 Mood symptoms that are common in other psychiatric disorders (e.g., irritability, agitation) were not rated as present in the mood sections unless they intensified with the onset of abnormal mood. Comorbid diagnoses were not assigned if they occurred exclusively during a mood episode. Results of the interview were always presented to child psychiatrists who were ultimately responsible for all diagnoses. Only children with clinically relevant and persistent symptomatology that affected their psychosocial functioning were diagnosed with a psychiatric disorder.
All diagnoses were made using the DSM-IV criteria. However, operationalized criteria for Bipolar Not-Otherwise-Specified were utilized.38 Children and adolescents with this subtype of Bipolar Disorder have been shown to have similar, but less severe clinical picture, comorbid disorders, family history, and longitudinal outcome compared to youth with Bipolar Disorder-I. 38 Moreover, approximately 40% of youth with Bipolar Not-Otherwise-Specified, especially those with elevated family history for Bipolar Disorder, converted into Bipolar-I or II.39 With the exception of Bipolar, Major Depression, and Pervasive Developmental Disorders in children and Bipolar Disorder - Not-Otherwise-Specified in biological co-parents, no other Not-Otherwise-Specified disorders were included in this paper. As described in further detail elsewhere, kappas for all disorders ranged between .80 and .90. 37
Caregiver-Teacher Report Forms 40 were requested from all caregivers of children who were attending day care or preschool programs.
Approximately 75% of the assessments were carried out in the subjects’ homes. To ensure blindness to parental diagnoses, interviewers that assessed parental psychopathology were different from the interviewers who assessed their children’s psychopathology, and the child psychiatrists were blind to parental diagnoses. Interviewers were asked to complete a “guess form” reporting whether the parents were Bipolar Disorder or controls. They guessed correctly in 74% of the cases. Of the ones guessed correctly, 59% were “not at all certain” and 33% “somewhat certain” about their guess. In addition, in 8 % of the cases they were “definitely certain” or the blind was broken by the parent. The psychiatrists remained blind to parental status in all cases.
All parent, child, and relatives’ diagnoses were made according to the best estimate procedure. 41
Socio-economic status was ascertained using the Hollingshead scale. 42
Statistical Analyses
The differences in demographic and clinical characteristics between the groups were evaluated using t-, χ2, and Fisher-exact tests as appropriate. Since both biological parents’ non-Bipolar psychopathology may affect the risk for psychiatric disorders in their offspring and more than one child from each family was included (“within family-correlations”), the effects of these variables were analyzed using mixed logistic and mixed-effects nominal logistic regressions, respectively.
Effect sizes for continuous and categorical variables (d and h, respectively) were calculated as described by Cohen. 43 All p-values are based on two-tailed tests.
RESULTS
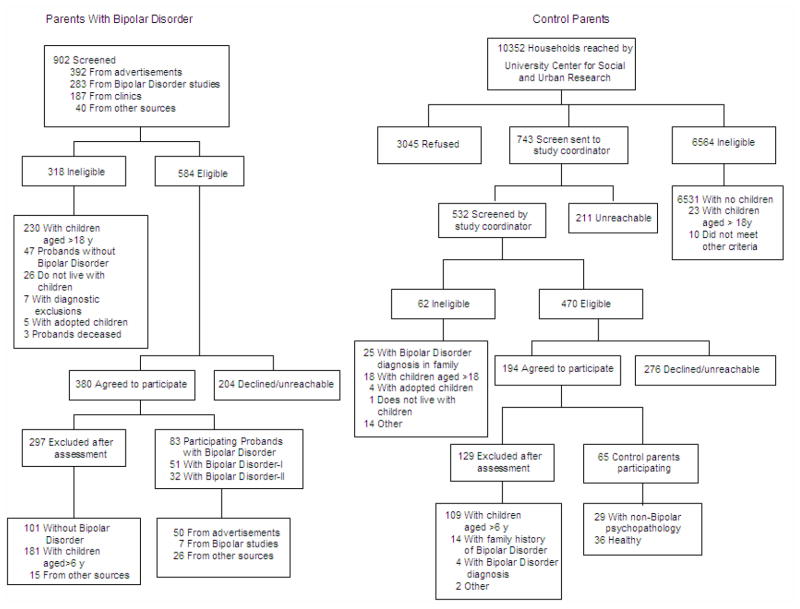
Parents
The recruitment flow of parents with Bipolar Disorder and controls has been described in detail elsewhere5 and is shown in Figure 1. Since the initial screening was done over the telephone and prior to obtaining subjects’ consent, the Institutional Review Board did not permit the recording of demographic information. Thus, comparisons between subjects who declined participation during the screen process and those who agreed to further participation are not available.
Figure 1.
Recruitment of Parents with Bipolar Disorder and Community Control Parents
Eighty-three parents (80.7%, 67/83 female) with Bipolar Disorder (I=51, II=32) and 65 community control parents (29 with non-Bipolar psychiatric disorders and 36 without any psychopathology) who had offspring 2–5 years old were recruited. Only two families had both parents with Bipolar Disorder. About 80% of parents with Bipolar Disorder reported that their initial DSM mood episode started when they were ≤ 22 years old and 30% before they were ≤13 years old.
The control parents had no first- or second-degree family history of Bipolar Disorder.
Demographic comparisons (Table 1)
Table 1.
Comparison of Demographics and Lifetime Axis-I Psychiatric Disorders between Proband Parents with Bipolar Disorder (BP) and Community Control Proband Parents
| Characteristic | Parents with Bipolar Disorder (N=83) | Controls (N= 65) | Analysis |
|||||
|---|---|---|---|---|---|---|---|---|
| Statistic | df | p | Effect size | |||||
| Mean | SD | Mean | SD | |||||
| Age (years) | 32.9 | 5.7 | 34.9 | 7.65 | t=−1.14 | 114.56 | 0.26 | |
| Socio-Economical Status | 35.9 | 14.4 | 38.4 | 15 | t=−1.02 | 146 | 0.31 | |
| Number of offspring | 2.4 | 1.1 | 2.3 | 1.03 | t=0.17 | 146 | 0.86 | |
| N | % | N | % | |||||
| Female | 75 | 90.4 | 48 | 73.8 | X2 =7.1 | 1 | 0.008 | 0.45 |
| Caucasian | 67 | 80.7 | 51 | 78.5 | X2=0.12 | 1 | 0.7 | |
| Married at Intake | 51 | 61.4 | 42 | 64.6 | X2=2.91 | 1 | 0.57 | |
| Any Axis I disorder | 83 | 100 | 29 | 44.6 | X2=60.74 | 1 | <.001 | 1.68 |
| Bipolar-I | 51 | 61.4 | 0 | 0.0 | Fisher’s exact test | - | <.001 | |
| Bipolar-II | 32 | 38.6 | 0 | 0.0 | Fisher’s exact test | - | <.001 | |
| Major Depressive Disorder | 0 | 0.0 | 13 | 20 | Fisher’s exact test | - | <.001 | |
| Dysthymic Disorder | 2 | 2.4 | 3 | 4.6 | Fisher’s exact test | - | 0.65 | |
| Any Anxiety | 58 | 69.9 | 13 | 20 | X2=36.3 | 1 | <.001 | 1.15 |
| Generalized Anxiety | 24 | 28.9 | 2 | 3.1 | X2=16.8 | 1 | <.001 | 0.78 |
| Separation Anxiety | 10 | 12 | 4 | 6.2 | X2=1.5 | 1 | 0.22 | |
| Panic | 24 | 28.9 | 3 | 4.6 | X2=14.3 | 1 | <.001 | 0.66 |
| Social Phobia | 19 | 22.9 | 3 | 4.6 | X2=9.6 | 1 | 0.002 | 0.53 |
| Obsessive-Compulsive | 18 | 21.7 | 0 | 0.0 | Fisher’s exact test | - | <.001 | |
| Post-Traumatic Stress | 28 | 33.7 | 7 | 10.8 | X2=10.65 | 1 | 0.001 | 0.56 |
| Attention Deficit Hyperactive Disorder | 19 | 22.9 | 3 | 4.6 | X2=9.62 | 1 | 0.002 | 0.53 |
| Disruptive Behavior Disorders | 35 | 42.2 | 7 | 10.8 | X2=17.7 | 1 | <.001 | 0.82 |
| Oppositional Defiant | 29 | 34.9 | 3 | 4.6 | X2=19.8 | 1 | <.001 | 0.79 |
| Conduct Disorder | 21 | 25.3 | 5 | 7.7 | X2=7.8 | 1 | .005 | 0.47 |
| Substance Use Disorders | 50 | 60.2 | 19 | 29.2 | X2=14.1 | 1 | <.001 | 0.65 |
| Alcohol | 38 | 45.8 | 15 | 23.1 | X2=8.2 | 1 | .004 | 0.49 |
| Drugs | 30 | 36.1 | 12 | 18.5 | X2=5.6 | 1 | .02 | 0.4 |
| Eating Disorders | 8 | 9.6 | 1 | 1.5 | X2=3.4 | 1 | .04 | 0.31 |
| Anorexia or Bulimia | 6 | 7.2 | 0 | 0.0 | Fisher’s exact test | - | <.001 | |
| Binge eating disorder | 3 | 3.6 | 1 | 1.5 | X2=.6 | 1 | .4 | 0.12 |
Except for parents with Bipolar Disorder being more likely to be Caucasian than the control parents there were no other between group demographic differences. On average, both groups of parents included two children in the study.
Axis-I disorders in Probands (Table 1)
With the exception of similar prevalence for Separation Anxiety, Dysthymic, and Eating Disorders, all other psychiatric disorders were present in higher rates in the parents with Bipolar Disorder when compared with the controls (p-values ≤ 0.04; Effect Sizes (ES):0.31–1.68). Within the parents with Bipolar Disorder, there were no significant differences in the rates of psychopathology between those recruited through advertisement vs. other means.
Axis I disorders in the biological co-parents
There was no difference in the proportion of direct assessments used to obtain the non-proband biological parent’s psychiatric disorders between parents with Bipolar Disorder (56%) and controls (44%). The biological co-parents of the offspring of parents with Bipolar Disorder showed higher rates of any Axis-I psychiatric disorders than the biological co-parents of the offspring of the controls (40.9% vs. 24.7%, p=.02). In addition, they had higher rates of Bipolar Disorder (3.2% vs. 0%), substance abuse (26% vs. 16%), and Disruptive Behavior Disorders (3.2% vs. 1.2%), but these comparisons did not reach statistical significance (p-values ≥.4).
Offspring
Demographic comparisons (Table 2)
Table 2.
Comparison of Demographic and Clinical Characteristics between Offspring of Bipolar Parents and Offspring of Community Control Parents
| Characteristic | Offspring of Parents with Bipolar Disorder (N= 121) | Offspring of Control Parents (N= 102) | Analysis |
|||||
|---|---|---|---|---|---|---|---|---|
| Statistic | df | p | Effect size | |||||
| Mean | SD | Mean | SD | |||||
| Age (years) | 3.8 | 1.3 | 3.8 | 1.3 | t=0.014 | 221 | 0.99 | |
| N | % | N | % | |||||
| Female | 62 | 51.2 | 45 | 44.1 | X2=1.13 | 1 | 0.29 | |
| Caucasian | 99 | 81.8 | 79 | 77.5 | X2=0.65 | 1 | 0.4 | |
| Living with both natural parents | 80 | 66.1 | 77 | 75.5 | X2=2.33 | 1 | 0.13 | |
| Any Axis I disorder* | 32 | 26.4 | 10 | 9.8 | X2=10.03 | 1 | 0.002 | 0.44 |
| Any Mood | 3 | 2.5 | 0 | 0.0 | Fisher’s exact test | - | 0.25 | |
| Bipolar Not-Otherwise-Specified | 2 | 1.7 | 0 | 0.0 | Fisher’s exact test | - | .5 | |
| Any Depression | 1 | .8 | 0 | 0.0 | Fisher’s exact test | - | >.9 | |
| Any Anxiety | 13 | 10.7 | 5 | 4.9 | X2=2.55 | 1 | 0.1 | |
| Generalized Anxiety | 2 | 1.7 | 0 | 0.0 | Fisher’s exact test | 1 | <.001 | |
| Separation Anxiety | 6 | 5 | 3 | 2.9 | Fisher’s exact test | 1 | 0.5 | |
| Social Phobia | 3 | 2.5 | 1 | 1.0 | Fisher’s exact test | 1 | 0.6 | |
| Specific phobia | 4 | 3.3 | 0 | 0.0 | Fisher’s exact test | 1 | 0.13 | |
| Obsessive-Compulsive | 0 | 0.0 | 0 | 0.0 | - | - | - | |
| Post-Traumatic Stress | 0 | 0.0 | 0 | 0.0 | - | - | - | |
| Attention Deficit Hyperactive Disorder | 19 | 15.7 | 2 | 2.0 | X2=12.3 | 1 | <.001 | 0.48 |
| Disruptive Behavior Disorder | 15 | 12.4 | 5 | 4.9 | X2=3.8 | 1 | 0.05 | |
| Oppositional Defiant | 14 | 11.6 | 5 | 4.9 | X2=3.2 | 1 | 0.07 | 0.24 |
| Conduct Disorder | 2 | 1.7 | 0 | 0.0 | Fisher’s exact | - | 0.5 | |
| Pervasive Developmental Disorder | 4 | 3.3 | 1 | 1.0 | Fisher’s exact | - | 0.4 | |
| Autism | 2 | 1.7 | 1 | 1.0 | Fisher’s exact | - | >.9 | |
| PDD-NOS | 2 | 1.7 | 0 | 0.0 | Fisher’s exact | - | .5 | |
| Adjustment Disorders | 2 | 1.7 | 1 | 1.0 | Fisher’s exact | - | >.9 | |
| Adjustment Depression | 1 | 0.8 | 0 | 0.0 | Fisher’s exact | - | >.9 | |
| Adjustment Anxiety | 0 | 0.0 | 1 | 1.0 | Fisher’s exact | - | >.9 | |
| Adjustment Mixed | 1 | 0.8 | 0 | 0.0 | Fisher’s exact | - | >.9 | |
| Elimination Disorders | 8 | 6.7 | 7 | 6.9 | X2=0.003 | 1 | .9 | |
| Enuresis | 7 | 5.8 | 3 | 2.9 | Fisher’s exact test | - | 0.3 | |
| Encopresis | 2 | 1.7 | 4 | 3.9 | Fisher’s exact test | - | 0.3 | |
| ** Other Psychiatric disorders | 6 | 5.0 | 3 | 2.9 | X2=.58 | 1 | 0.45 | |
| Sleep disorders | 3 | 2.5 | 3 | 2.9 | X2=.045 | 1 | 0.8 | |
| More than two disorders | 21 | 17.4 | 7 | 6.9 | X2=5.55 | 1 | .02 | 0.32 |
does not include elimination disorders
sleep disorder, phonological disorder, communication and development disorder, trichotillomania
121 offspring of parents with Bipolar Disorder and 102 offspring of control parents (58 from parents with at least one parent with non-BP psychopathology and 44 from healthy parents) were recruited. There were no between-group demographic differences. As expected, the mother was the reporter for most (78.9%) children. At intake, 5 children of the parents with Bipolar Disorder were taking psychotropic medications, mainly stimulants. None of the children of the control parents were taking medications.
Axis –I disorders (Table 2)
In comparison with the offspring of the control parents, the offspring of parents with Bipolar Disorder showed significantly greater lifetime prevalence of any Axis-I, Disruptive Behavior, ADHD, and two or more disorders (all p-values ≤0.05; ES: 0.24–0.48), and a trend for more Oppositional Defiant Disorder. Two offspring of parents with Bipolar Disorder had Bipolar Disorder Not-Otherwise-Specified (because they did not meet the DSM-IV duration criteria), one had Depressive Disorder Not-Otherwise-Specified, and one had Adjustment Disorder with Depressed Mood. The offspring of the controls did not have mood disorders.
Except for Oppositional Defiant Disorder that was equally diagnosed in children younger and older than 4 years old, about 80% of other disorders occurred in children older than 4 years old.
There were no differences in the rates of psychiatric disorders between the offspring of parents with Bipolar-I and the offspring of parents with Bipolar-II (p-values ≥.1). Parental age of onset of mood disorder was not significantly associated with increased rate of any Axis-I disorders in the offspring (p> .12). Within the offspring of parents with Bipolar Disorder, any Axis-I disorders was not significantly associated with mothers’ lifetime Bipolar diagnosis or any active Axis-I disorder at the time of assessment.
There were no between-group differences in the rates of psychiatric disorders between the offspring of parents that the interviewers “correctly guessed” had Bipolar Disorder and the children of parents that the interviewers “incorrectly guessed”. The same results were obtained within the offspring of parents with Bipolar Disorder (all p-values >.1).
Mixed effects logistic regressions
Adjusting for both biological parents non-Bipolar psychopathology and within-family correlations showed that when compared with the offspring of control parents the offspring of parents with Bipolar Disorder showed significantly higher risk for ADHD (Odds Ratio:8.17, 95%CI:1.3–52.6) and having ≥ 2 disorders (Odds Ratio:6.4, 95%CI:1.1–40). Comparisons for Disruptive Behavior Disorders (p=.4) and any Axis-I disorders (p=.2) were not significant.
Severity of manic and depressive symptoms
As depicted in Table 3, the total MRS-13, MRS-5, and DEP-12 scores were significantly higher in the offspring of the parents with Disorder when compared with the offspring of the controls. Adjusting for age, sex, parental diagnoses, and child’s Oppositional Defiant and ADHD diagnoses did not change the results. However, there were significant interactions with offspring with ADHD or Oppositional Defiant and a parent with Bipolar Disorder showing higher scores on the MRS (5 and 13 items) and DEP-12 (p-values <.04, effect sizes: 0.3–.5).
Children with high scores on the MRS-5 and 13 had high scores in the DEP-12 (rho= .46, p<.001; rho=.62 p<.001, respectively).
Exploratory analyses showed that with the exception of grandiosity and psychotic symptoms, all other manic symptoms (for a list of all manic symptoms see footnote in Table 3) were significantly higher in the offspring of parents with Bipolar Disorder (p-values ≤ .04, effect sizes between 0.35 and 0.63). After Bonferroni corrections, elation, irritability/anger, unusual energy, and mood lability remained statistically significant. For the depressive symptoms, between group differences were due mainly to the severity of irritability, difficulty concentrating, inattention, slow thinking, psychomotor agitation and insomnia (p-values ≤ .05, effect sizes between 0.26 and 0.36). After Bonferroni corrections, above-noted differences became non-significant. About 96% of the severity scores of individual manic and depressive symptoms were classified as mild or less.
Caregivers/Teachers Reports
Caregiver-Teacher Report Forms 40 were available for 56/105 (53.3%) of the preschoolers who attended day care. Five reports were incomplete for a total of 51 Caregiver-reports (22 offspring of parents with Bipolar Disorder and 29 offspring of controls). There were no demographic or clinical differences between the children whose caregivers completed or did not complete the Caregiver-Teacher Forms.
Pearson correlations for the Total, Internalizing, and Externalizing scores of the parent’s Child Behavior Checklist 37, 40 and Caregivers’ Forms ranged between .31 to .38 (p-values ≤ .02).
There were no differences in the Total, Internalizing and Externalizing Caregiver scores between offspring of parents with Bipolar Disorder and offspring of control parents. However, only 5/22 offspring of parents with Bipolar Disorder and 3/29 of the controls who had Caregiver reports had ADHD and/or Oppositional Defiant Disorder. Combining the children with ADHD and/or Oppositional Defiant Disorder (n=8) showed that they had significantly higher Caregiver’s Attention scores when compared with those without these disorders (p =.01).
DISCUSSION
When compared to the preschool offspring of the control parents and after adjusting for both biological parents’ non-Bipolar Disorders, and within family correlations, the offspring of parents with Bipolar Disorder showed an 8-fold increase in ADHD and significantly higher rates of ≥ 2 psychiatric disorders. There were no differences in the rates of psychiatric disorders between offspring of parents with Bipolar-I and -II. While only 3 offspring of parents with Bipolar Disorder had mood disorders, offspring of parents with Bipolar Disorder, especially those with ADHD and Oppositional Defiant Disorder, had significantly more severe current manic and depressive symptomatology than the offspring of the controls. In a subset of children, caregivers/teachers reported significantly more psychopathology in children with ADHD and Oppositional Defiant ghDisorder than those without these disorders.
Before discussing the above-noted findings, the limitations of the study deserve comment. First, as in any pediatric study, and especially for preschoolers, the main informant for both the Bipolar and controls groups were the mothers. In addition, in about half of the cases, the psychopathology in the biological co-parents was ascertained by interviewing the main informant. However, there were no between-group differences in rates of mothers serving as main informants and no differences in the proportion of direct and indirect interviews of co-biological parents of the Bipolar and control parents. Second, the children’s psychopathology was ascertained through parents and parental psychiatric illnesses and could have inflated the rates of the reported psychopathology in the offspring. However, the literature regarding this issue is controversial, and it appears that if there is any effect, it is small;44–46 similar biases existed for both groups of parents because about 50% of the control parents had Axis-I disorders and rates of psychiatric disorders in the offspring of parents with Bipolar Disorder was not associated with their mothers’ lifetime diagnosis of Bipolar Disorder and acute mood symptomatology at intake. In contrast to the above arguments, there were no between group differences in the Caregiver scores between offspring of parents with Bipolar Disorder and offspring of control parents. Nevertheless, very few offspring who had Caregiver reports had ADHD and/or Oppositional Defiant Disorder and the rest of the sample was healthy. To help clarify the above issues, more confirmatory work that utilizes parent report in tandem with measures less influenced by bias than parent ratings, and particular direct observation measurements, is needed. Third, the nature of the study could have attracted parents with more severe disorders. Nevertheless, the rates of psychiatric disorders in the parents with Bipolar Disorder were similar to those reported in the adult Bipolar literature. 47, 48 Also, even though BIOS is not an epidemiological study, the lifetime prevalence of psychiatric disorders found in the control parents was similar to that reported in a recent large epidemiological study in the United States. 49 Fourth, no direct observations of the preschoolers were available. Finally, although behavioral and mood disorders are identifiable in preschoolers, more studies are necessary regarding the way these disorders, particularly mania, are manifested in preschoolers and to determine the most appropriate methods and instruments to assess these conditions in this population.
Both biological parents of the offspring of parents with Bipolar Disorder showed higher rates of psychopathology than the control parents. Therefore, it is not surprising that the offspring of the parents with Bipolar Disorder showed significantly more psychopathology than the offspring of the controls. In fact, after taking into account both biological parents’ psychopathology, between-group differences in any Axis-I disorders and Disruptive Behavior Disorders were no longer significant. However, rates of ADHD remained significantly higher in the offspring of the parents with Bipolar Disorder. Other studies of preschool offspring of parents with Bipolar Disorder that evaluated dimensional symptomatology rather than categorical disorders have also shown that these children have symptoms frequently observed in children with ADHD (e.g., behavioral disinhibition, hyperactivity, and difficulty managing anger and hostile impulses).15, 17, 19
It is not yet clear why the results of the BIOS preschool-age study contrast with the results of the BIOS and other school-age high-risk studies (i.e., high prevalence of mood and anxiety disorders). 14,50–52 It is possible that the K-SADS-PL was not sensitive enough to detect mood and anxiety disorders in preschoolers. However, despite that BIOS is not an epidemiological study, rates of disorders ascertained through the K-SADS-PL are similar to those found in epidemiological studies 19, 37 and one epidemiological study using an unmodified K-SADS-PL, 53 diagnosed mood and anxiety disorders in preschoolers at rates similar to the Preschool Age Psychiatric Assessment.19 It is also probable that in comparison with older children, non-specific symptomatology such as irritability, hyperactivity, inattention, and impulsivity are ubiquitous manifestations of externalizing as well as internalizing psychopathology in preschool children. 9, 14, 54–57 In contrast, due to their emotional and cognitive developmental level, more specific manic symptoms such as grandiosity and elation or depressive symptoms such as hopelessness and severe melancholia are not yet evident, or if present, they are more difficult to ascertain.24 Thus, in BIOS although these non-specific externalizing symptoms may indeed be accounted for by early childhood ADHD, it is also possible that these symptoms, especially when accompanied by mood symptomatology and family history for mood disorders, are prodromal or subthreshold symptoms of mood disorders. 8, 9, 14, 16, 55, 58–61 In fact, in BIOS, preschool children of parents with Bipolar Disorder with externalizing disorders had significantly more manic and depressive symptoms than offspring of parents with Bipolar Disorder without these disorders, and the offspring of the control parents. As reported in the literature, these children are at high risk to develop mood disorders. 62–66
Only 3 preschool offspring of the parents with Bipolar Disorder had subthreshold mood disorders. However, these children have not reached the age of highest risk to develop Bipolar and Major Depressive Disorders and it has been consistently shown that the rate of these disorders is likely to increase with age. 5, 8, 9, 67, 68 Despite the above findings, the preschool offspring of parents with Bipolar Disorder and especially those with externalizing disorders, had significantly more severe manic (including elation) and depressive symptoms when compared with the offspring of the controls. However, it is important to note that in general, the severity of individual manic symptoms was sub-clinical. Furthermore, additional studies are needed to define the boundaries between Bipolar symptoms (e.g., elation, grandiosity, irritability, and mood episodicity) and the expected broad mood fluctuations and normal fantasies about special powers and abilities and appropriately increased self-concept commonly observed in preschool children. 24, 69
Since BIOS is prospectively following all children, we will be able to address the above issues and delineate types and severity of symptoms that predict subsequent conversion into Bipolar Disorder. In addition, because approximately 70% of the preschool offspring of parents with Bipolar Disorder did not have any diagnosable psychiatric illness and very few had subthreshold mood disorders, there is a window of opportunity for primary prevention in this high-risk population. Thus, psychosocial interventions aimed at helping preschool children to regulate their mood, interventions that have been found to be efficacious for preschoolers with Disruptive Behavior Disorders and older children with subthreshold mood disorders, and effective treatment of parental psychopathology may diminish the severity and perhaps delay or prevent the new onset of psychopathology in preschool offspring of parents with Bipolar Disorder.4, 24, 70–73
Acknowledgments
This work was supported by NIMH grant MH60952 (PI: Boris Birmaher, MD). The opinions and assertions contained in this report are the private views of the authors, and are not to be construed as official or as reflecting the views of the National Institute of Mental Health, the National Institutes of Health, or the Department of Health and Human Services.
The authors would like to thank Carol Kostek and Mary Kay Gill, MSN for their assistance with manuscript preparation, UCSUR staff, BIOS interviewers (Ryan Brown BA, Nick Curcio BS, Ronna Currie BS, Gail Oterson BS, Elizabeth Picard BS, and Lindsay Virgin BA), and Scott Turkin MD and the Dubois Regional Medical Center (DRMC) Behavioral Health Services staff for their collaboration. In addition, the authors would like to thanks Drs. Shelli Avenevoli and Editha Nottelmann and from NIMH for their support.
Footnotes
Disclosures: Dr. Birmaher discloses: Participated in forums sponsored by Forest Laboratories (11/2008), Shire Pharmaceuticals (7/2008), JAZZ Pharmaceuticals (1/2008), and royalties from Random House, Inc. and Lippincott Williams & Wilkins. Dr. Kupfer discloses: Advisor Boards for Pfizer, Inc, Eli Lilly & Company, Forest Pharmaceuticals, Inc., Solvay/Wyeth Pharmaceuticals and consultant for Servier Amerique. Drs. Axelson, Goldstein, Iyengar, Brent and Diler and Ms. Monk, Kalas, Obreja, Hickey and Mr. Shamseddeen have no financial disclosures.
References
- 1.Geller B, Tillman R, Bolhofner K, Zimerman B. Child Bipolar I Disorder: Prospective Continuity With Adult Bipolar I Disorder; Characteristics of Second and Third Episodes; Predictors of 8-Year Outcome. Arch Gen Psychiatry. 2008;65(10):1125–33. doi: 10.1001/archpsyc.65.10.1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.DelBello MP, Hanseman D, Adler CM, Fleck DE, Strakowski SM. Twelve-month outcome of adolescents with bipolar disorder following first hospitalization for a manic or mixed episode. Am J Psychiatry. 2007;164(4):582–90. doi: 10.1176/ajp.2007.164.4.582. [see comment] [DOI] [PubMed] [Google Scholar]
- 3.Pavuluri MN, Birmaher B, Naylor MW. Pediatric bipolar disorder: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 2005;44:846–71. doi: 10.1097/01.chi.0000170554.23422.c1. [DOI] [PubMed] [Google Scholar]
- 4.Miklowitz DJ, Chang KD. Prevention of bipolar disorder in at-risk children: theoretical assumptions and empirical foundations. Dev Psychopathol. 2008;20(3):881–97. doi: 10.1017/S0954579408000424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Birmaher B, Axelson D, Monk K, Kalas C, Goldstein B, Hickey MB, Obreja M, Ehmann M, Iyengar S, Shamseddeen W, Kupfer D, Brent D, Birmaher B, Axelson D, Monk K, Kalas C, Goldstein B, Hickey MB, Obreja M, Ehmann M, Iyengar S, Shamseddeen W, Kupfer D, Brent D. Lifetime psychiatric disorders in school-aged offspring of parents with bipolar disorder: the Pittsburgh Bipolar Offspring study. Arch Gen Psychiatry. 2009;66(3):287–96. doi: 10.1001/archgenpsychiatry.2008.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reichart CG, Wals M, Hillegers MHJ, Ormel J, Nolen WA, Verhulst FC. Psychopathology in the adolescent offspring of bipolar parents. J Affect Disord. 2004;78(1):67–71. doi: 10.1016/s0165-0327(02)00178-7. [DOI] [PubMed] [Google Scholar]
- 7.DelBello MP, Geller B. Review of studies of child and adolescent offspring of bipolar parents. Bipolar Disorders. 2001;3(6):325–34. doi: 10.1034/j.1399-5618.2001.30607.x. [DOI] [PubMed] [Google Scholar]
- 8.Henin A, Biederman J, Mick E, Sachs GS, Hirshfeld-Becker DR, Siegel RS, McMurrich S, Grandin L, Nierenberg AA. Psychopathology in the offspring of parents with bipolar disorder: a controlled study. Biol Psychiatry. 2005;58(7):554–61. doi: 10.1016/j.biopsych.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 9.Duffy A, Alda M, Crawford L, Milin R, Grof P. The early manifestations of bipolar disorder: a longitudinal prospective study of the offspring of bipolar parents. Bipolar Disorders. 2007;9(8):828–38. doi: 10.1111/j.1399-5618.2007.00421.x. [DOI] [PubMed] [Google Scholar]
- 10.Chang K, Steiner H, Ketter T, Chang K, Steiner H, Ketter T. Studies of offspring of parents with bipolar disorder. American Journal of Medical Genetics Part C, Seminars in Medical Genetics. 2003;123C(1):26–35. doi: 10.1002/ajmg.c.20011. [DOI] [PubMed] [Google Scholar]
- 11.Hirshfeld-Becker DR, Biederman J, Henin A, Faraone SV, Dowd ST, De Petrillo LA, Markowitz SM, Rosenbaum JF. Psychopathology in the young offspring of parents with bipolar disorder: a controlled pilot study. Psychiatry Res. 2006;145(2–3):155–67. doi: 10.1016/j.psychres.2005.08.026. [DOI] [PubMed] [Google Scholar]
- 12.Zahn-Waxler C, Mayfield A, Radke-Yarrow M, McKnew DH, Cytryn L, Davenport YB. A follow-up investigation of offspring of parents with bipolar disorder. Am J Psychiatry. 1988;145(4):506–9. doi: 10.1176/ajp.145.4.506. [DOI] [PubMed] [Google Scholar]
- 13.Zahn-Waxler C, Chapman M, Cummings EM. Cognitive and social development in infants and toddlers with a bipolar parent. Child Psychiatry Hum Dev. 1984;15(2):75–85. doi: 10.1007/BF00706165. [DOI] [PubMed] [Google Scholar]
- 14.Radke-Yarrow M, Nottelmann E, Martinez P, Fox MB, Belmont B. Young children of affectively ill parents: a longitudinal study of psychosocial development. J Am Acad Child Adolesc Psychiatry. 1992;31(1):68–77. doi: 10.1097/00004583-199201000-00011. [DOI] [PubMed] [Google Scholar]
- 15.Cytryn L, McKnew DH, Zahn-Waxler C, Radke-Yarrow M, Gaensbauer TJ, Harmon RJ, Lamour M. A developmental view of affective disturbances in the children of affectively ill parents. Am J Psychiatry. 1984;141(2):219–22. doi: 10.1176/ajp.141.2.219. [DOI] [PubMed] [Google Scholar]
- 16.Hirshfeld-Becker DR, Biederman J, Henin A, Faraone SV, Cayton GA, Rosenbaum JF. Laboratory-observed behavioral disinhibition in the young offspring of parents with bipolar disorder: a high-risk pilot study. Am J Psychiatry. 2006;163(2):265–71. doi: 10.1176/appi.ajp.163.2.265. [DOI] [PubMed] [Google Scholar]
- 17.Romano E, Tremblay RE, Farhat A, Cote S, Romano E, Tremblay RE, Farhat A, Cote S. Development and prediction of hyperactive symptoms from 2 to 7 years in a population-based sample. Pediatrics. 2006;117(6):2101–10. doi: 10.1542/peds.2005-0651. [DOI] [PubMed] [Google Scholar]
- 18.Sterba S, Egger HL, Angold A. Diagnostic specificity and nonspecificity in the dimensions of preschool psychopathology. J Child Psychol Psychiatry. 2007;48(10):1005–13. doi: 10.1111/j.1469-7610.2007.01770.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Egger HL, Angold A. Common emotional and behavioral disorders in preschool children: presentation, nosology, and epidemiology. J Child Psychol Psychiatry. 2006;47(3–4):313–37. doi: 10.1111/j.1469-7610.2006.01618.x. [DOI] [PubMed] [Google Scholar]
- 20.Angold A, Egger HL. Preschool psychopathology: lessons for the lifespan. J Child Psychol Psychiatry. 2007;48(10):961–6. doi: 10.1111/j.1469-7610.2007.01832.x. [DOI] [PubMed] [Google Scholar]
- 21.Luby JL, Si X, Belden AC, Tandon M, Spitznagel E. Preschool Depression: Homotypic Continuity and Course Over 24 Months. Arch Gen Psychiatry. 2009;66(8):897–905. doi: 10.1001/archgenpsychiatry.2009.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stalets MM, Luby JL. Preschool depression. Child Adolesc Psychiatr Clin N Am. 15(4):899–917. doi: 10.1016/j.chc.2006.05.011. [DOI] [PubMed] [Google Scholar]
- 23.Luby J, Tandon M, Nicol G. Three clinical cases of DSM-IV mania symptoms in preschoolers. J Child Adolesc Psychopharmacol. 2007;17(2):237–43. doi: 10.1089/cap.2007.0131. [DOI] [PubMed] [Google Scholar]
- 24.Luby J, Belden A. Defining and validating bipolar disorder in the preschool period. Dev Psychopathol. 2006;18(4):971–88. doi: 10.1017/S0954579406060482. [DOI] [PubMed] [Google Scholar]
- 25.Tumuluru RV, Weller EB, Fristad MA, Weller RA. Mania in six preschool children. J Child Adolesc Psychopharmacol. 2003;13(4):489–94. doi: 10.1089/104454603322724878. [DOI] [PubMed] [Google Scholar]
- 26.Mota-Castillo M, Torruella A, Engels B, Perez J, Dedrick C, Gluckman M. Valproate in very young children: an open case series with a brief follow-up. J Affect Disord. 2001;67(1–3):193–7. doi: 10.1016/s0165-0327(01)00431-1. [DOI] [PubMed] [Google Scholar]
- 27.Dilsaver SC, Akiskal HS. Preschool-onset mania: incidence, phenomenology and family history. J Affect Disord. 2004;82 (Suppl 1):S35–43. doi: 10.1016/j.jad.2004.05.018. [DOI] [PubMed] [Google Scholar]
- 28.APA. Diagnostic and statistical manual of mental disorders 4th edition (DSM-IV) 4. Washington DC: American Psychiatric Association; 2004. [Google Scholar]
- 29.Spitzer RL, Williams JB, Gibbon M, First MB. The Structured Clinical Interview for DSM-III-R (SCID). I: History, rationale, and description. Arch Gen Psychiatry. 1992;49(8):624–9. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- 30.Andreasen NC, Endicott J, Spitzer RL, Winokur G. The family history method using diagnostic criteria. Reliability and validity. Arch Gen Psychiatry. 1977;34(10):1229–35. doi: 10.1001/archpsyc.1977.01770220111013. [DOI] [PubMed] [Google Scholar]
- 31.Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. Journal of the American Academy of Child & Adolescent Psychiatry. 1997 Jul;36(7):980–8. doi: 10.1097/00004583-199707000-00021. [see comment] [DOI] [PubMed] [Google Scholar]
- 32.Axelson D, Birmaher BJ, Brent D, Wassick S, Hoover C, Bridge J, Ryan N. A preliminary study of the Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children mania rating scale for children and adolescents. J Child Adolesc Psychopharmacol. 2003;13:463–70. doi: 10.1089/104454603322724850. [DOI] [PubMed] [Google Scholar]
- 33.Frazier TW, Demeter CA, Youngstrom EA, Calabrese JR, Stansbrey RJ, McNamara NK, Findling RL. Evaluation and Comparison of Psychometric Instruments for Pediatric Bipolar Spectrum Disorders in Four Age Groups. J Child Adolesc Psychopharmacol. 2007;17(6):853–66. doi: 10.1089/cap.2007.0057. [DOI] [PubMed] [Google Scholar]
- 34.Chambers WJ, Puig-Antich J, Hirsch M, Paez P, Ambrosini PJ, Tabrizi MA, Davies M. The assessment of affective disorders in children and adolescents by semistructured interview. Test-retest reliability of the schedule for affective disorders and schizophrenia for school-age children, present episode version. Archives of General Psychiatry. 1985;42(7):696–702. doi: 10.1001/archpsyc.1985.01790300064008. [DOI] [PubMed] [Google Scholar]
- 35.Keenan K, Wakschlag LS. Are oppositional defiant and conduct disorder symptoms normative behaviors in preschoolers? A comparison of referred and nonreferred children. Am J Psychiatry. 2004;161(2):356–8. doi: 10.1176/appi.ajp.161.2.356. [DOI] [PubMed] [Google Scholar]
- 36.Kashani JH, Allan WD, Beck NC, Jr, Bledsoe Y, Reid JC. Dysthymic disorder in clinically referred preschool children. J Am Acad Child Adolesc Psychiatry. 1997;36(10):1426–33. doi: 10.1097/00004583-199710000-00025. [DOI] [PubMed] [Google Scholar]
- 37.Birmaher B, Ehmann M, Axelson DA, Goldstein BI, Monk K, Kalas C, Kupfer D, Gill MK, Leibenluft E, Bridge J, Guyer A, Egger HL, Brent DA, Birmaher B, Ehmann M, Axelson DA, Goldstein BI, Monk K, Kalas C, Kupfer D, Gill MK, Leibenluft E, Bridge J, Guyer A, Egger HL, Brent DA. Schedule for affective disorders and schizophrenia for school-age children (K-SADS-PL) for the assessment of preschool children--a preliminary psychometric study. J Psychiatr Res. 2009;43(7):680–6. doi: 10.1016/j.jpsychires.2008.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Axelson D, Birmaher B, Strober M, Gill MK, Valeri S, Chiappetta L, Ryan N, Leonard H, Hunt J, Iyengar S, Bridge J, Keller M. Phenomenology of children and adolescents with bipolar spectrum disorders. Arch Gen Psychiatry. 2006;63:1139–48. doi: 10.1001/archpsyc.63.10.1139. [DOI] [PubMed] [Google Scholar]
- 39.Birmaher BAD, Goldstein B, Strober M, Gill MK, Hunt J, Houck P, Iyengar S, Kim E, Yen S, Esposito C, Goldstein T, Ryan N, Keller M. Four-Year Longitudinal Course of Pediatric Bipolar Spectrum Disorder-The Course and Outcome of Bipolar Youth (COBY) Study. Am J Psychiatry. 2009;166:795–804. doi: 10.1176/appi.ajp.2009.08101569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Achenbach T, Rescorla LA. Manual for the ASEBA preschool froms and profiles. 2000. [Google Scholar]
- 41.Leckman JF, Sholomskas D, Thompson WD, Belanger A, Weissman MM. Best estimate of lifetime psychiatric diagnosis: a methodological study. Arch Gen Psychiatry. 1982;39(8):879–83. doi: 10.1001/archpsyc.1982.04290080001001. [DOI] [PubMed] [Google Scholar]
- 42.Hollingshead AB. Index of Social Status. In: Mangen DJ, Peterson WA, editors. Research instruments in social gerontology: Vol. 2. Social roles and social participation. Minneapolis, MN: University of Minnesota Press; 1982. [Google Scholar]
- 43.Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Lawrence A Erlbaum Associates; 1988. [Google Scholar]
- 44.Najman JM, Williams GM, Nikles J, Spence S, Bor W, O’Callaghan M, Le Brocque R, Andersen MJ. Mothers’ mental illness and child behavior problems: cause-effect association or observation bias? J Am Acad Child Adolesc Psychiatry. 2000;39(5):592–602. doi: 10.1097/00004583-200005000-00013. [DOI] [PubMed] [Google Scholar]
- 45.Youngstrom E, Loeber R, Stouthamer-Loeber M. Patterns and correlates of agreement between parent, teacher, and male adolescent ratings of externalizing and internalizing problems. J Consult Clin Psychol. 2000;68(6):1038–50. doi: 10.1037//0022-006x.68.6.1038. [DOI] [PubMed] [Google Scholar]
- 46.Low NCP, Cui L, Merikangas KR. Community versus clinic sampling: effect on the familial aggregation of anxiety disorders. Biol Psychiatry. 2008;63(9):884–90. doi: 10.1016/j.biopsych.2007.08.011. [DOI] [PubMed] [Google Scholar]
- 47.Kessler RC, Merikangas KR, Wang PS. Prevalence, comorbidity, and service utilization for mood disorders in the United States at the beginning of the twenty-first century. Annual Review of Clinical Psychology. 2007;3:137–58. doi: 10.1146/annurev.clinpsy.3.022806.091444. [DOI] [PubMed] [Google Scholar]
- 48.Merikangas KR, Herrell R, Swendsen J, Rossler W, Ajdacic-Gross V, Angst J. Specificity of bipolar spectrum conditions in the comorbidity of mood and substance use disorders: results from the Zurich cohort study. Arch Gen Psychiatry. 2008;65(1):47–52. doi: 10.1001/archgenpsychiatry.2007.18. [DOI] [PubMed] [Google Scholar]
- 49.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 50.Chang KD, Steiner H, Ketter TA. Psychiatric phenomenology of child and adolescent bipolar offspring. J Am Acad Child Adolesc Psychiatry. 2000;39(4):453–60. doi: 10.1097/00004583-200004000-00014. [DOI] [PubMed] [Google Scholar]
- 51.Duffy A, Alda M, Hajek T, Sherry SB, Grof P. Early stages in the development of bipolar disorder. Journal of Affective Disorders. doi: 10.1016/j.jad.2009.05.022. In Press. [DOI] [PubMed] [Google Scholar]
- 52.Johnson JG, Cohen P, Brook JS. Associations between bipolar disorder and other psychiatric disorders during adolescence and early adulthood: a community-based longitudinal investigation. Am J Psychiatry. 2000;157(10):1679–81. doi: 10.1176/appi.ajp.157.10.1679. [DOI] [PubMed] [Google Scholar]
- 53.Keenan K, Shaw DS, Walsh B, Delliquadri E, Giovannelli J. DSM-III-R disorders in preschool children from low-income families. J Am Acad Child Adolesc Psychiatry. 1997;36(5):620–7. doi: 10.1097/00004583-199705000-00012. [DOI] [PubMed] [Google Scholar]
- 54.West AE, Schenkel LS, Pavuluri MN, West AE, Schenkel LS, Pavuluri MN. Early childhood temperament in pediatric bipolar disorder and attention deficit hyperactivity disorder. J Clin Psychol. 2008;64(4):402–21. doi: 10.1002/jclp.20471. [DOI] [PubMed] [Google Scholar]
- 55.Hirshfeld-Becker DR, Biederman J, Henin A, Faraone SV, Micco JA, van Grondelle A, Henry B, Rosenbaum JF, Hirshfeld-Becker DR, Biederman J, Henin A, Faraone SV, Micco JA, van Grondelle A, Henry B, Rosenbaum JF. Clinical outcomes of laboratory-observed preschool behavioral disinhibition at five-year follow-up. Biol Psychiatry. 2007;62(6):565–72. doi: 10.1016/j.biopsych.2006.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Carlson GA, Carlson GA. Who are the children with severe mood dysregulation, a.k.a. “rages”? Am J Psychiatry. 2007;164(8):1140–2. doi: 10.1176/appi.ajp.2007.07050830. [comment] [DOI] [PubMed] [Google Scholar]
- 57.Zahn-Waxler C, McKnew DH, Cummings EM, Davenport YB, Radke-Yarrow M. Problem behaviors and peer interactions of young children with a manic-depressive parent. Am J Psychiatry. 1984;141(2):236–40. doi: 10.1176/ajp.141.2.236. [DOI] [PubMed] [Google Scholar]
- 58.Egeland JA, Shaw JA, Endicott J, Pauls DL, Allen CR, Hostetter AM, Sussex JN. Prospective study of prodromal features for bipolarity in well Amish children. J Am Acad Child Adolesc Psychiatry. 2003;42(7):786–96. doi: 10.1097/01.CHI.0000046878.27264.12. [see comment] [DOI] [PubMed] [Google Scholar]
- 59.Carlson GA, Meyer SE. Phenomenology and diagnosis of bipolar disorder in children, adolescents, and adults: complexities and developmental issues. Dev Psychopathol. 2006;18:939–69. doi: 10.1017/S0954579406060470. [DOI] [PubMed] [Google Scholar]
- 60.Kovacs M, Pollock M. Bipolar disorder and comorbid conduct disorder in childhood and adolescence. J Am Acad Child Adolesc Psychiatry. 1995;34(6):715–23. doi: 10.1097/00004583-199506000-00011. [DOI] [PubMed] [Google Scholar]
- 61.Shaw JA, Egeland JA, Endicott J, Allen CR, Hostetter AM, Shaw JA, Egeland JA, Endicott J, Allen CR, Hostetter AM. A 10-year prospective study of prodromal patterns for bipolar disorder among Amish youth. Journal of the American Academy of Child & Adolescent Psychiatry. 2005;44(11):1104–11. doi: 10.1097/01.chi.0000177052.26476.e5. [DOI] [PubMed] [Google Scholar]
- 62.Tillman R, Geller B. Controlled study of switching from attention-deficit/hyperactivity disorder to a prepubertal and early adolescent bipolar I disorder phenotype during 6-year prospective follow-up: rate, risk, and predictors. Development & Psychopathology. 2006;18(4):1037–53. doi: 10.1017/S0954579406060512. [DOI] [PubMed] [Google Scholar]
- 63.Burke JD, Loeber R, Lahey BB, Rathouz PJ. Developmental transitions among affective and behavioral disorders in adolescent boys. J Child Psychol Psychiatry. 2005;46(11):1200–10. doi: 10.1111/j.1469-7610.2005.00422.x. [DOI] [PubMed] [Google Scholar]
- 64.Boylan K, Vaillancourt T, Boyle M, Szatmari P. Comorbidity of internalizing disorders in children with oppositional defiant disorder. Eur Child Adolesc Psychiatry. 2007;16(8):484–94. doi: 10.1007/s00787-007-0624-1. [DOI] [PubMed] [Google Scholar]
- 65.Tillman R, Geller B, Bolhofner K, Craney JL, Williams M, Zimerman B. Ages of onset and rates of syndromal and subsyndromal comorbid DSM-IV diagnoses in a prepubertal and early adolescent bipolar disorder phenotype. Journal of the American Academy of Child & Adolescent Psychiatry. 2003;42(12):1486–93. doi: 10.1097/00004583-200312000-00016. [DOI] [PubMed] [Google Scholar]
- 66.Leibenluft E, Cohen P, Gorrindo T, Brook JS, Pine DS. Chronic versus episodic irritability in youth: a community-based, longitudinal study of clinical and diagnostic associations. J Child Adolesc Psychopharmacol. 2006;16:456–66. doi: 10.1089/cap.2006.16.456. [DOI] [PubMed] [Google Scholar]
- 67.Hillegers MH, Reichart CG, Wals M, Verhulst FC, Ormel J, Nolen WA. Five-year prospective outcome of psychopathology in the adolescent offspring of bipolar parents. Bipolar Disorders. 2005;7(4):344–50. doi: 10.1111/j.1399-5618.2005.00215.x. [DOI] [PubMed] [Google Scholar]
- 68.Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry. 2003;60(8):837–44. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- 69.Carlson GA. Mania and ADHD: comorbidity or confusion. J Affect Disord. 1998;51(2):177–87. doi: 10.1016/s0165-0327(98)00179-7. [DOI] [PubMed] [Google Scholar]
- 70.Weissman MM, Pilowsky DJ, Wickramaratne PJ, Talati A, Wisniewski SR, Fava M, Hughes CW, Garber J, Malloy E, King CA, Cerda G, Sood AB, Alpert JE, Trivedi MH, Rush AJ Team STD-C. Remissions in maternal depression and child psychopathology: a STAR*D-child report. JAMA. 2006;295(12):1389–98. doi: 10.1001/jama.295.12.1389. [DOI] [PubMed] [Google Scholar]
- 71.Horowitz JL, Garber J. The prevention of depressive symptoms in children and adolescents: A meta-analytic review. J Consult Clin Psychol. 2006;74(3):401–15. doi: 10.1037/0022-006X.74.3.401. [see comment] [DOI] [PubMed] [Google Scholar]
- 72.Beardslee WRVE, Van de Velde P, Swatling S, Hoke H. Preventing depression in children through resiliency promotion: the prevention intervention project. In: McMahon RJDPR, editor. The Effects of Parental Dysfunction on Children. New York: Kluwer Academic/Plenum; 2003. pp. 71–86. [Google Scholar]
- 73.Chang K, Howe M, Gallelli K, Miklowitz D. Prevention of pediatric bipolar disorder: integration of neurobiological and psychosocial processes. Ann N Y Acad Sci. 2006;1094:235–47. doi: 10.1196/annals.1376.026. [DOI] [PubMed] [Google Scholar]