Abstract
Objectives
This study compares black and white caregivers of persons with Alzheimer’s disease (AD) on two general measures of negative and positive emotion (depressive symptoms, positive mood) and two caregiving specific measures of negative and positive emotion (caregiver burden, caregiver satisfaction). We hypothesized that black caregivers would exhibit lower levels of negative emotion and higher levels of positive emotion over time than whites.
Method
396 caregivers were recruited from the Rush Alzheimer’s Disease Center in Chicago, Illinois, as part of a longitudinal study of persons with AD. The analyses for this report are based on data from 307 caregivers who were interviewed quarterly over approximately four years from 1999–2002; an average of nine observations per person.
Results
The results showed that black caregivers reported fewer depressive symptoms over time than whites (β̂ = −0.14, p < 0.01) but this finding was only for those caregivers living with the care recipient with Alzheimer’s disease. No race differences were found for measures of positive emotion.
Conclusion
Our data add to the growing body of evidence that blacks have better emotional outcomes when exposed to the stress of providing informal care to a disabled family member.
Keywords: caregiver affect, psychological adjustment, race/ethnicity, Alzheimer’s disease
INTRODUCTION
The debilitating effects of Alzheimer’s disease (AD) and other late-life dementia syndromes eventually require assistance with most activities of daily living, supervision, and possible legal guardianship. These demands are sources of substantial chronic stress as indicated by the high rate of negative emotional states and psychiatric morbidity for family caregivers (Schulz et al., 1995). There is evidence that substantial racial differences may exist in caregiver adjustment with better adjustment for blacks. Despite a number of studies that have shown better psychological adjustments among black caregivers, it is not well understood what explains this apparent advantage.
Psychological adaptation to chronic stress has been modeled in persons providing care for a chronically disabled family member, particularly for disabilities produced by a late-life dementia syndrome. These observational studies have consistently shown that family dementia caregivers are likely to report clinically significant levels of negative emotion (Haley et al., 1995, 2004, Lawton et al., 1992; Miller et al., 1995; Schulz et al., 1995) and reduced frequency of positive emotion (Haley et al., 2004; Lawton et al., 1992; Roff et al., 2004; White et al., 2000).
Among basic demographic variables, race has emerged as an important predictor of caregiver psychological adaptation (Connell & Gibson, 1997). Blacks are less likely than whites to report symptoms of emotional distress in the context of providing daily care for a family member with dementia (Farran et al., 1997; Fredman et al., 1995; Haley et al., 1995, 1996, 2004; Lawton et al., 1992; Miller et al., 1995; Roth et al., 2001; White et al., 2000). Similarly, blacks are more likely than whites to report positive emotional experiences and perceptions of caregiving experiences (Haley et al., 2004; Lawton et al., 1992; Roff et al., 2004). Although the consistency of better psychological outcomes found in black caregivers is impressive, much of the evidence is based on cross-sectional studies.
In one of the few published longitudinal studies of dementia caregivers, Roth et al. (2001) found evidence of better psychological adaptation in blacks over time on measures of positive and negative emotional function, life satisfaction, and depressive symptoms; however, the temporal pattern varied between measures. Racial differences in life satisfaction increased over a two-year period, primarily due to a decline in scores for white caregivers. By contrast, depressive symptoms remained stable over time in both racial subgroups, with higher levels reported by white caregivers at each of three measurement points. Thus, positive emotion may provide a more sensitive indicator of racial differences in caregiver psychological adaptation.
To further evaluate racial differences in caregiver emotional adaptation, this report will present data from a four-year longitudinal study of family caregivers for persons with Alzheimer’s disease (AD). A major strength of the study design was that caregiver emotional function was measured at three-month intervals over approximately four years to characterize individual differences. Previous longitudinal studies of dementia caregivers have typically relied on 3–5 observation points to estimate rates of change, potentially limiting precision. AD symptom severity was also sequentially measured over the course of this study to characterize dementia-specific care-related stressors over time. Based on previous reports, black caregivers were expected to exhibit better emotional adaptation across study time than white caregivers.
A secondary objective of this report is to examine two hypotheses that have been postulated to account for racial differences in caregiver psychological adaptation – higher levels of religiosity and more supportive social environments in blacks than whites (Dilworth-Anderson et al., 2002). As secondary objectives, the present study will evaluate religiosity and three features of the social environment - living arrangements, quality of the past relationship between caregiver and AD participant, and quality of caregiver social support - as moderator variables with respect to any observed racial differences in caregiver emotional function.
METHODS
Participants
Caregivers in the present study were recruited as part of a longitudinal study of 396 persons with AD. This AD cohort was recruited from the Rush Alzheimer’s Disease Center (June, 1999, through April, 2002) and lived within the Chicago metropolitan area. Eligibility required that each participant complete a standardized clinical evaluation (Gilley et al., 2005), meet diagnostic criteria for possible or probable AD (McKhann et al., 1984), and reside in a community setting. Community residence encompassed a wide range of private and public housing arrangements, excluding only institutional facilities providing assisted living or nursing care. All data collection procedures were presented verbally by study representatives and specified in writing via consent documents. As an added precaution, AD participants and a responsible family member jointly signed consent documents. The Institutional Review Board of Rush University Medical Center approved consent procedures for AD and caregiver participants.
Caregiver participants included for the purpose of this current report met three criteria: (a) identified himself or herself as the primary family member responsible for the AD participant’s care; (b) was the adult child or spouse of the AD participant; and (c) completed three or more data collection interviews. Thirty-four caregivers who were not related by blood or marriage to the AD participant were excluded and 55 caregivers were excluded who had less than three data collection interviews primarily because of institutionalization (n = 26) or death (n = 15) of the AD participant. A total of 307 caregivers met the three criteria. Of the 307 caregiver participants, 234 lived with the AD participant, including 138 spouse and 96 adult child caregivers. The remaining 73 caregivers (all adult children) lived in the area, but not with the AD participant.
Measures
Caregiver Emotional Function
Four measures of emotional function were obtained using structured interviews, conducted either in-person or by telephone at baseline and at three-month intervals during the study. These measures crossed two content dimensions (general emotion, emotional appraisal of caregiver experiences) with two valence dimensions (positive, negative). General measures of emotion require caregivers to describe current levels of negative and positive emotion without reference to care-related stresses. The second set of measures covered negative and positive appraisals of caregiving-specific experiences and responsibilities. Because there is evidence in both the general and caregiver populations that negative- and positive-valence responses are largely independent patterns of emotion (Lawton et al., 1991; Watson & Tellegen, 1988), the valence dimension was systematically incorporated into the measurement design.
Negative Emotion
General negative emotion was assessed using a measure of depressive symptoms. Depressive symptoms have been widely used to document clinically significant levels of negative emotion in dementia caregivers (Schulz et al., 1995). For this study, we used the 10-item version of the Center for Epidemiologic Studies Depression scale (CES-D) (Kohout et al., 1993) to measure depressive symptoms. Items were rated as present or absent during the past week. Total scores range from 0 to 10, with higher scores indicating greater depressive symptoms. The internal consistency of the CES-D was examined in the total study population (Cronbach’s alpha = 0.75).
Negative emotion specific to caregiving experiences was measured using a 10-item measure of caregiver burden (Burden) (Lawton et al., 1991). This measure uses a 4-point ordinal response scale and asks the respondent to report how often in the past week they have felt a certain way (i.e., almost never, sometimes, often, almost always) for items that express some form of subjective distress linked to caregiving such as: “I feel isolated and alone as a result of caring for Mr(s) ______,” “I will be unable to care for Mr(s) ______ much longer,” and ”I have lost control of my life since Mr(s) ______’s illness. Total scores for Burden range from 10–40, with higher scores indicating greater caregiving burden. The internal consistency of Burden was tested in the total population (Cronbach’s alpha = 0.88).
Positive Emotion
General positive emotion was measured with a 10-item positive affect (PA) scale that has been widely used in emotion research (Watson et al., 1988). The PA uses a 4-point ordinal response scale and asks the respondent to report how often s/he has felt a certain way in the past week (e.g., interested, excited, strong, enthusiastic, etc.). Total scores for PA range from 10 to 40, with higher scores indicating more positive affect. The internal consistency of PA was tested in the total population (Cronbach’s alpha = 0.89).
Positive emotion specific to caregiving experiences was measured using a 5-item scale of caregiver satisfaction (Satisfaction) (Lawton et al., 1989). Caregiver satisfaction uses a 4-point ordinal response scale and asks the respondent to report the regularity (i.e., almost never, sometimes, often, almost always) of positive aspects of caregiving such as: “I really enjoy being with _______” and “_______ shows real appreciation of what I do for him/her.” Total scores for Satisfaction range from 5–20, with higher scores indicating greater caregiving satisfaction. The internal consistency of Satisfaction was tested in the total population (Cronbach’s alpha = 0.77).
Care-related Stressors
The following measures were assessed over the study to characterize the changes in stress intensity over time: AD participant disease severity; AD participant functional disability; years having provided care, and hours of care provided weekly.
AD Severity
Cognitive impairment is used as an index of dementia severity. For this study, the Mini-Mental State Examination (MMSE) (Folstein et al., 1975) was used to measure cognitive impairment of the AD participant. This brief performance test assesses orientation, memory, attention, language, and visuo-spatial abilities. The MMSE was conducted via face-to-face testing with the AD participant every six months. These interviews were conducted every six months because of the slow progression of the disease. Scores range from 0 to 30 based on the number of correct responses; thus, lower scores indicate greater severity of cognitive impairment.
Functional disability
Functional disability of the participant with AD was measured using six items from the Katz Adjustment Scale (KAS) (Cornoni-Huntley et al., 1986; Katz & Alporn, 1976). Items cover the ability to perform six self-care activities: bathing; dressing; walking across a small room; transferring from bed to a chair; using the toilet; and eating. KAS scores range from 0 to 6 based on the number of activities performed requiring assistance, with higher scores indicating greater functional disability. The KAS was conducted via telephone interview with the caregiver every three months. Items were rated on a two-point scale (“no help required,” “needs help/unable to perform”) with “the previous month” used as the time frame of reference.
Stress exposure
Two measures capture the temporal properties of stress exposure: 1) length of time (in years) providing care to the person with AD, assessed at baseline only, and 2) current amount of care provided per week (in hours per day).
Caregiver Social Resources
Various factors have been hypothesized to account for racial differences in caregiver adjustment (Connell & Gibson, 1997; Dilworth-Anderson et al., 2004; Li et al., 1999; Roth et al., 2001). We tested three social resource factors in our models - religiosity, social support, and quality of past relationship with the care recipient. Assessments were conducted with the caregivers via telephone every three months for a total of 15 assessments over approximately 48 months.
Religiosity
Caregivers were asked six questions about perceptions of their religiosity/spirituality (Fetzer Institute, 1999); for example, “How important is your religious faith or spirituality to you?” “To what extent do you consider yourself a religious or spiritual person?” and “How much is religion or spirituality a source of strength and comfort to you”? Response choices included: not at all, a little, some, quite a bit, and a great deal. The six questions were summed into a composite variable with a range of 6–30, with higher scores indicating greater religiosity/spirituality. The internal consistency of the religiosity scale was tested in the total population (Cronbach’s alpha = 0.92).
Social support
Caregivers’ social support was measured using the Multidimensional Scale of Perceived Social Support (Dahlem et al., 1991) which consists of 12 questions; for example: “There is a special person who is around when I am in need,” “My family really tries to help me,” and “I can talk about my problems with my friends.” The five Likert response choices ranged from strongly agree to strongly disagree, with a neutral middle choice. The 12 questions were summed into a composite variable with a range of 12–60, with higher scores indicating lower social support. The internal consistency of the social support scale was tested in the total population (Cronbach’s alpha of 0.91).
Relationship quality
Caregivers were also asked three questions about the quality of their past relationship with the care recipient; for example, “Before he/she had memory problems, to what extent did you enjoy the time the two of you spent together?” “How close did you feel to him/her at that time?” and “How much emotional support did he/she give to you”? The response choices were: not at all, a little, some, quite a bit, and a great deal. The three caregiver social resources questions were summed into a composite variable with a range of 3–15, with higher scores indicating a better past relationship. The internal consistency of the relationship quality scale was tested in the total population (Cronbach’s alpha = 0.83).
Analysis
We hypothesized that black caregivers would exhibit lower levels of negative emotion and higher levels of positive emotion over time than whites. Generalized linear regression models for the vector of measurements of scores over time were fit using the Generalized Estimating Equations (GEE) method (Diggle et al., 2002), which was implemented using the GENMOD® procedure in SAS® Version 9 (SAS Institute Inc., 2004). GEE procedures model the vector of scores from each person as a function of age, sex, time since baseline, race, and other predictor variables. GEE is particularly suitable for the analysis of these data, as it offers a choice of link functions to model the outcome variable and accounts for the within-person correlation across repeated measurements. Due the highly skewed distribution of the CES-D and burden scores, we specified a log link function with a Poisson error structure for analyses (Allison, 1999; SAS Institute Inc., 2004). We specified identity links with normal distributions for the analyses of both positive affect and satisfaction scale scores. The “working” within-person correlation was assumed to be identical for each pair of times of observation (exchangeable error structure); the estimates from GEE models are robust to the choice of working correlation matrix. All models were validated using both graphical techniques and tests of alternative structures.
All of the spouse caregivers and more than half (57%) of the adult child caregivers resided with their care recipients. It has been documented that caregiver experiences and depressive symptoms differ according to co-residence status (Li et al., 1997, 1999; Waite et al., 2004) and as such, we stratified our data based on caregiver and care recipient co-residence. We included a contrast term in our models to compare spouse and child caregivers.
We modeled each of the caregiver outcomes using the same set of core variables. The effects of age, gender, race, and education were entered into the models with coefficients representing the effect of the variable on the average outcome score over all observations. Study time (in years) was included to estimate the rate of change in the outcome over time. Interactions between the demographic variables and study time were also entered to evaluate the effect of each demographic variable on the rate of change of the outcome. MMSE, KAS, and time providing care (in hours) were entered as time-varying coefficients, and the baseline measure of length of time in years providing care was also entered. In a secondary set of analyses, baseline measures of religiosity, social support, and quality of past relationship with the care recipient were entered into the models as possible explanatory variables for the race differences in caregiver adjustment. We also calculated predicted outcome values for co-residing caregivers and non co-residing caregivers by race for graphic presentation.
A high rate of follow-up participation is needed to optimally model time-varying measurements of caregiver depression. In this study, participation rates across the 14 follow-up observations ranged from 76.1 to 90.8 percent, with a median of 80.8 percent. To be eligible for analysis, a participant had to have non-missing values for depressive symptoms, caregiver burden, positive affect, and caregiver satisfaction, at baseline and for at least two other time points. When a participant had a change in caregiver, only the data up until that change were retained; that is, analyzed data are only for the same caregiver for each participant over time. Furthermore, only observations up until date of nursing home placement, if applicable, were retained. During the course of this study, 79 of the 307 participants (25.7%) were placed in a nursing home; the placement rates did not differ by race.
RESULTS
As shown in Table 1, there were differences by race in key study variables at baseline. Compared to whites, black caregivers were younger, more likely to be female, had less education, and were more likely to be adult child caregivers than spouses. The majority of both blacks and whites co-resided with their care recipients (80% vs. 75%, respectively). Black care recipients also had greater cognitive impairment and functional disability than their white counterparts. Further, black caregivers reported providing more care per week, higher levels of religiosity, and less social support than their white counterparts.
Table 1.
Baseline study variables by race and by living arrangement, Mean (SD), unless otherwise indicated
| Blacks* (n = 74) | Whites (n =229) | p value | Co-residing (n = 234) | Not co- residing (n =73) | p value | |
|---|---|---|---|---|---|---|
| Caregiver characteristics, fixed effects | ||||||
| Age | 56.9 (13.3) | 61.2 (13.6) | .020 | 63.4 (13.7) | 50.2 (7.1) | <.001 |
| Female sex, # (%) | 57 (77.0) | 148 (64.6) | .048 | 154 (65.8) | 53 (72.6) | .280 |
| Black, # (%) | -- | -- | -- | 59 (25.5) | 15 (20.8) | .417 |
| Co-residing, # (%) | 59 (79.7) | 172 (75.1) | .417 | -- | -- | -- |
| Education | 13.7 (3.2) | 14.7 (2.8) | .033 | 14.1 (3.0) | 15.4 (2.3) | <.001 |
| Kinship relationship: | <.001 | -- | ||||
| Spouse, # (%) | 20 (27.0) | 116 (50.7) | 138 (59.0) | -- | ||
| Adult child, # (%) | 54 (73.0) | 113 (49.3) | 96 (41.0) | 73 (100%) | ||
| Care recipient characteristics | ||||||
| MMSE | 11.8 (7.1) | 14.9 (8.4) | .002 | 14.1 (8.3) | 14.5 (7.8) | .734 |
| Katz Activities Scale | 2.1 (2.1) | 1.7 (2.1) | .024 | 1.8 (2.1) | 1.7 (2.1) | .725 |
| Care-related characteristics | ||||||
| Amount of care provided per week (hours) | 60.6 (56.5) | 47.0 (56.5) | .005 | 59.2 (59.3) | 21.5 (33.9) | <.001 |
| Length of time providing care (years) | 4.1 (4.5) | 3.4 (3.1) | .139 | 3.5 (3.6) | 3.6 (3.2) | .841 |
| Religiosity | 24.3 (5.3) | 20.6 (6.9) | <.0001 | 21.2 (6.8) | 22.1 (6.7) | .375 |
| Social support | 27.8 (7.9) | 24.4 (7.7) | .004 | 26.0 (8.1) | 22.8 (6.5) | <.001 |
| Past relationship | 12.8 (2.7) | 12.8 (2.4) | .884 | 13.0 (2.3) | 12.1 (2.9) | .018 |
The difference between the race and co-residing sample sizes (303 vs. 307) is due to missing race values for 4 people.
Because we stratified our data based on caregiver and care recipient co-residence, we also show differences in Table 1 between the co-residers and non co-residers on key study variables at baseline. Compared to non co-residers, co-residers were older and had less education. All spouse caregivers co-resided with the AD participant, compared to approximately half of the adult child caregivers. Compared to non co-residers, co-residers reported spending nearly three times more hours per week (59 hours vs. 22 hours) caring for the recipient, indicated less social support, and reported having a better past relationship with the care recipient. Although the range for amount of care provided per week in hours includes 0, the data are substantially positively skewed; that is, no caregiver reported providing 0 hours of care per week. Finally, there were few blacks (n = 15) among the adult child caregivers not living with their affected parent. Because of these differences, hypotheses regarding race differences in caregiver emotion were primarily tested in the subgroup living with the AD participant.
Caregivers living with the AD participant
Measures of negative emotion
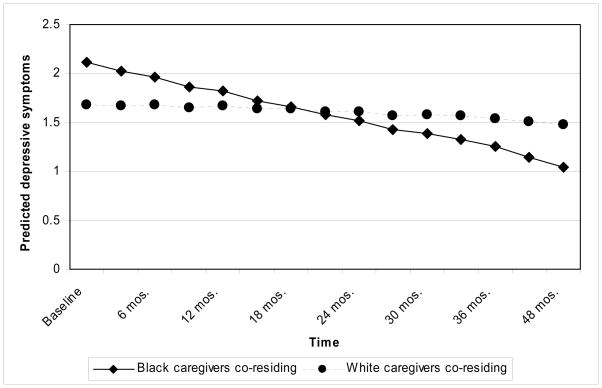
Table 2 summarizes the GEE regression models predicting caregiver depressive symptoms (CES-D scale) and perceived burden (Burden scale) in providing informal care. Models for the CES-D scale scores were fit using 2088 observations (M = 8.9 observations per person). After adjustment for other study variables, there was no significant intercept difference between white and black caregivers in CES-D scores. The interaction between race and study time indicates that CES-D scores were more likely to decrease over time in blacks than whites. This pattern is illustrated graphically in Figure 1. In addition to race, CES-D scores were correlated with levels of cognitive impairment (MMSE), functional disability (KAS), and hours of care provided over the course of the study. These time-varying covariates provide a crude metric of care-related stressors in relation to caregiver depressive symptoms. Finally, there was a gender difference, with higher CES-D scores for females. Note that the interaction between gender and study time was not significant, indicating that there was no gender difference in rates of change over the follow-up period.
Table 2.
Models predicting levels of negative emotion on the CES-D and Burden scales in caregivers living with the AD participant, Estimate (SE)
| Variable | CES-D | Burden |
|---|---|---|
| Intercept | 0.88 (0.17)*** | 2.70 (0.07)*** |
| Study time | −0.03 (0.03) | 0.01 (0.01) |
| Caregiver characteristics, fixed effects | ||
| Age (years) | −0.01 (0.01) | −0.01 (0.00)*** |
| Gender: male | −0.35 (0.13)** | −0.08 (0.04)* |
| Race: black | 0.23 (0.12) | 0.07 (0.05) |
| Education (years) | −0.04 (0.02) | 0.01 (0.01) |
| Kinship relationship: spouse | 0.19 (0.19) | 0.09 (0.06) |
| Caregiver characteristics, slope | ||
| Age × study time | −0.00 (0.00) | 0.00 (0.00) |
| Gender × study time | −0.08 (0.06) | −0.02 (0.02) |
| Education × study time | 0.01 (0.01) | −0.00 (0.00) |
| Race × study time | −0.14 (0.05)** | −0.05 (0.02)** |
| Care-related stress characteristics | ||
| MMSE | −0.01 (0.01)* | −0.01 (0.00)** |
| Katz Activities Scale | 0.01 (0.02) | 0.02 (0.01)*** |
| Care provided/week (hours) | 0.00 (0.00)** | 0.00 (0.00)*** |
| Time providing care (years) | 0.00 (0.02) | −0.00 (0.01) |
Notes. Study time is a linear function of time, measuring change since baseline;
p <= .05;
p <= .01;
p <= .001.
Figure 1.
Predicted values of CES-D, by race, based on the model for caregivers living with the AD participant (all other variables set to their average values).
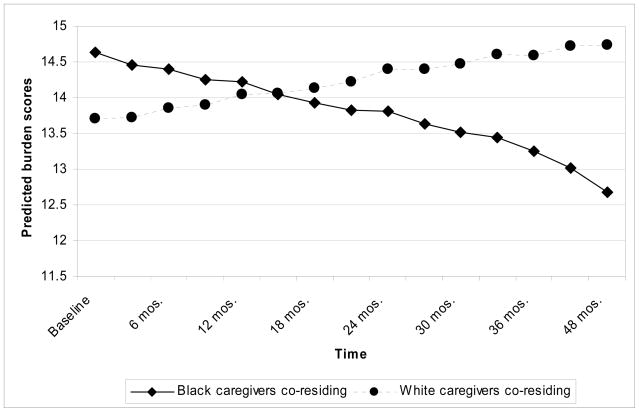
Models for the Burden scale scores were fit using 2050 observations (M = 8.8 observations per person). The pattern of effects for the Burden scale (see Table 2) closely parallels the effects for the CES-D scale. There were no race differences in the intercept (baseline), but blacks and whites exhibited different patterns of change over time. As shown in Figure 2, burden scores tended to decrease over time for black caregivers while increasing over time for white caregivers. Burden scores were also related to age, gender, dementia severity on the MMSE and KAS, and hours of care provided.
Figure 2.
Predicted values of Burden, by race, based on the model for caregivers living with the AD participant (all other variables set to their average values).
Non-linear changes were explored by examining study time and study time squared both alone in the models (i.e., without any covariates) and in the models with covariates. There was no apparent curvilinear time trend for the CES-D or burden scale scores. To examine whether the observed race differences in caregiver negative emotion can be accounted for by social factors, terms for caregiver religiosity, perceive social support, and quality of the past relationship between the caregiver and AD participant were added to the models predicting CES-D and burden scale scores. As shown in Table 3, the race by study time interaction term remained significant for both measures. Compared to the unadjusted models presented in Table 2, the race by study time coefficients were essentially unchanged with the addition of these social factors.
Table 3.
Models predicting levels of negative emotion on the CES-D and Burden scales in caregivers living with the AD participant, controlling for social factors, Estimate (SE)
| Variable | CES-D | Burden |
|---|---|---|
| Intercept | 1.29 (0.40)** | 2.87 (0.17)*** |
| Study time | −0.03 (0.03) | 0.01 (0.20) |
| Caregiver characteristics, fixed effects | ||
| Age (years) | −0.00 (0.01) | −0.01 (0.00)*** |
| Gender: male | −0.39 (0.13)** | −0.10 (0.04)* |
| Race: black | 0.24 (0.12)* | 0.08 (0.05) |
| Education (years) | −0.02 (0.02) | 0.01 (0.01)* |
| Kinship relationship: spouse | 0.29 (0.19) | −0.05 (0.02)** |
| Caregiver characteristics, slope | ||
| Age × study time | −0.00 (0.00) | 0.00 (0.00) |
| Gender × study time | −0.08 (0.06) | −0.02 (0.02) |
| Education × study time | 0.01 (0.01) | −0.00 (0.00) |
| Race × study time | −0.14 (0.05)** | −0.05 (0.02)** |
| Care-related stress characteristics | ||
| MMSE | −0.01 (0.01)** | −0.01 (0.00)** |
| Katz Activities Scale | 0.01 (0.02) | 0.02 (0.01)*** |
| Care provided/week (hours) | 0.00 (0.00)** | 0.00 (0.00)*** |
| Time providing care (years) | −0.00 (0.02) | −0.00 (0.01) |
| Social Factors | ||
| Religiosity | −0.01 (0.01) | −0.01 (0.00)* |
| Perceived Social Support | 0.02 (0.01)** | 0.00 (0.00) |
| Relationship Quality | −0.06 (0.02)* | −0.01 (0.01) |
Notes. Study time is a linear function of time, measuring change since baseline;
p <= .05;
p <= .01;
p <= .001.
Measures of positive emotion
Table 4 summarizes the GEE regression models predicting perceived satisfaction (Satisfaction scale) in providing informal care and caregiver positive mood (Positive Affect scale). Models for the Satisfaction scale were fit using 2045 observations (M = 8.7 observations per person). The pattern of effects for the Satisfaction scale is shown in Table 4. There was no evidence of race differences or non-linear trends in Satisfaction scores over time.
Table 4.
Models predicting levels of positive emotion on the Caregiver Satisfaction and Positive Affect scales in caregivers living with the AD participant, Estimate (SE)
| Variable | Satisfaction | Positive Affect |
|---|---|---|
| Intercept | 14.12 (0.72)*** | 26.07 (1.08)*** |
| Study time | 0.19 (0.14) | −0.45 (0.20)* |
| Caregiver characteristics, fixed effects | ||
| Age (years) | 0.04 (0.03) | −0.01 (0.04) |
| Gender: male | 1.86 (0.53)*** | −0.02 (0.69) |
| Race: black | −0.05 (0.61) | −0.04 (0.79) |
| Education (years) | −0.15 (0.09) | 0.12 (0.12) |
| Kinship relationship: spouse | −0.69 (0.86) | 0.64 (1.18) |
| Caregiver characteristics, slope | ||
| Age × study time | −0.00 (0.01) | −0.00 (0.01) |
| Gender × study time | 0.01 (0.17) | 0.78 (0.31)* |
| Education × study time | −0.01 (0.02) | −0.01 (0.04) |
| Race × study time | 0.12 (0.21) | −0.03 (0.30) |
| Care-related stress characteristics | ||
| MMSE | 0.07 (0.02)*** | 0.06 (0.03) |
| Katz Activities Scale | 0.02 (0.06) | −0.01 (0.10) |
| Care provided/week (hours) | −0.00 (0.00) | 0.00 (0.00) |
| Time providing care (years) | −0.02 (0.05) | 0.13 (0.09) |
Notes. Study time is a linear function of time, measuring change since baseline;
p <= .05;
p <= .01;
p <= .001.
Models for the Positive Affect scale were fit using 2050 observations (M = 8.8 observations per person). Contrary to study hypotheses, there was no relationship between race and Positive Affect scale scores. There was a significant gender difference, with a trend toward increasing Positive Affect scale scores over time for males. Measures of disease severity and care-related time demands were not related to Positive Affect scores. A non-linear trend in Positive Affect scores over time was found, but incorporating linear and non-linear temporal effects into the models did not reveal any effect for race, dementia severity, or care-related demands.
In the models among caregivers not co-residing with the AD participant (n=73), although we found higher levels of depressive symptoms in black caregivers at baseline, we found no changes in caregiver depressive symptoms by race, or differences in burden, caregiver satisfaction, or positive affect by race. The reader should note that the small number of black caregivers not co-residing with the AD participant (n = 15 [21%]) limits statistical power and hence our ability to make inferences about race differences among caregivers not living with their care recipients.
DISCUSSION
Data from this four-year longitudinal study provide further evidence of race differences in the emotional adaptation of family caregivers. Positive and negative emotional function was assessed at three-month intervals for caregivers of older adults with AD. Race differences in emotion were only found in caregivers living in the same household as the person with AD. In this subgroup, levels of negative emotion declined over time for black caregivers, while remaining unchanged or increased in whites. Irrespective of living arrangements, we did not find race differences in positive emotion. Care-related stresses (AD participant disease severity, AD participant functional disability, years providing care and hours of care provided per week) were also measured longitudinally in our study and included as model covariates, mitigating any confounding of race with AD severity. Finally, the social resources we measured (religiosity, perceived social support, and quality of the past relationship in our models) did not account for any of the race effects for caregivers co-residing with the AD participants.
Despite the protracted course of dementia syndromes, race differences in caregiver emotional adaptation have primarily been evaluated in cross-sectional studies (Connell & Gibson, 1997). It is, therefore, important to highlight the similarities and differences in the findings of our study and the longitudinal study reported by Roth et al. (2001). Both studies found race differences across repeated measurements of negative emotion, suggesting that black caregivers are better able than whites to emotionally adapt to the stresses of providing informal care for a family member with dementia. However, the temporal patterns in negative emotion for blacks and whites differed between our studies. We found a decline in two measures of negative emotion over time for black caregivers in conjunction with relatively stable levels for whites. By contrast, Roth et al. (2001) found that depressive symptoms increased in severity over time for white caregivers, while remaining stable for blacks. Second, we found that race differences were limited to caregivers living in the same household as the person with AD. Living arrangements were not examined as a factor in Roth et al. (2001). Finally, we were unable to replicate race differences in positive emotion found by Roth et al. (2001).
Race differences could arise from adaptive advantages in black caregivers or vulnerabilities in white caregivers. The pattern of temporal changes in caregiver emotional function provides valuable information about the relative likelihood of these two explanations. The decline in levels of negative emotion for black caregivers in our study suggests that blacks may have an adaptive advantage, with no clear deficit in whites. The prominent finding of Roth et al. (2001) suggests deteriorating emotional function in whites, which favors a vulnerability or deficit in the coping skills. A steady decline in emotional function has been described as a pattern resulting from the “wear and tear” of dementia-related stresses (Schulz et al., 1995) in caregivers with inadequate coping skills. Further research is needed to clarify if there is a consistent pattern of race differences in caregiver emotional function over time and disease progression.
There are three major differences in methodology between our study and Roth et al. (2001) that may have contributed to differences in results. One difference is in the number and spacing of repeated measurements. Estimates of change in emotional function in Roth et al. were based on a maximum of three observations at one-year intervals, with most participants completing only two observations. We measured emotional function and other key variables at three-month intervals for up to four years, with an average of 8.6 observations for each caregiver participant. The larger vector of observations may provide a more precise estimate of individual differences in change over time. The second difference is in sample characteristics. Caregivers in both studies were convenience samples identified through dementia clinics, but drawn from areas of different population density. Participants in Roth et al. (2001) were drawn from rural and smaller urban areas whereas our study primarily included caregivers living in a large urban area. Finally, different measures of positive emotion were used in the two studies.
Our finding that race differences in caregiver emotional adaptation were limited to caregivers living with their family member with AD has several possible explanations. Caregivers living in the same household are exposed to higher levels of dementia-related stress and more likely to be extensively engaged in providing care. High levels of caregiver stress may therefore be required to unmask individual differences in coping skills related to race. Caregivers not living in the same household as the person with AD will have less exposure to disease symptoms and fewer care-related demands, possibly making it difficult to detect race differences in emotional adaptation. Positive attitudes toward family care among blacks could also diminish the perceived “burden” of providing care for a family member, particularly when the need for care is substantial.
Social resources are thought to account for race differences in caregiver emotional adaptation (Dilworth-Anderson et al., 2002), most notably greater religiosity and availability of social support among blacks. Furthermore, contextual differences, such as caregiver financial burden and leisure time satisfaction, are oftentimes obscured by over-simplifying race differences (Williams, 2005). Although we did not examine caregiver financial burden or satisfaction with leisure time, we did evaluate the impact of caregiver social resources by including indicators of religiosity, perceived social support, and quality of the past relationship in our models. For caregivers living in the same household as the person with AD, none of these social resource variables accounted for the observed race effects. Further research is needed to determine if other social or contextual factors contribute to race differences in emotional adaptation of dementia caregivers. The sociocultural stress and coping model (Knight et al., 2000) enumerates how social forces can shape attitudes toward caregiving and the development of coping strategies via culturally-transmitted values and behaviors. Dilworth-Anderson and colleagues (2002) suggest that culture is essential to understanding how people justify their values and beliefs about caregiving; for example, norms of reciprocity, sense of duty, obligation, and expectation, role engulfment, and God’s will contribute to development of appropriate coping strategies (Dilworth-Anderson et al., 2002). Beyond cultural norms of filial responsibility, there are oftentimes intergenerational differences between caregivers’ expectations of providing care and care recipients’ expectations of receiving care (Peek et al., 1998). Clearly, understanding race differences in caregiving is complex and involves numerous micro and macro-level factors.
The present study has three major limitations. First, the study used a convenience sample of caregivers identified through a dementia specialty clinic. Selection biases related to medical service utilization may affect the distribution of caregiver and disease – stress characteristics. Thus, population-based studies are needed to further explore the effects of race and other factors associated with caregiver emotional adaptation. Population studies are also needed to identify comparable non-caregivers to more fully explicate the relationship between race and emotional adaptation.
The second limitation of our study was the small number of black caregivers not living with their family member with AD (n = 15). As a result, statistical power to detect race differences in emotional function is likely to be limited. Nonetheless, the subgroup of black caregivers living in the same household as the person with AD (n = 59) was large enough to detect race differences in levels and rates of change of negative emotion. In addition, we did not establish that the measurement properties of the metrics were invariant between blacks and whites.
Third, there are important limitations to the generalizeability of our results. The persons with AD in our sample tended to have moderate to severe disease. Thus, the longitudinal assessment of caregiver emotional function primarily captures temporal patterns of adaptation to the later stages of the disease. Caregivers with limited coping skills may be less likely to continue providing care as the disabling effects of a dementia syndrome become severe. Thus, it is difficult to rule out a “healthy survivor” bias in our results. Race differences in our study were limited to a comparison between black and white caregivers. Other race, ethnic, and cultural differences in caregiver emotional adaptation may exist and warrant further study. Finally, the restriction of the sample to caregivers for persons with AD limits the generality of the findings. Because of the prevalence, duration, and complexity of the care-related demands associated with dementia syndromes, the use of dementia caregivers to study the psychological effects of chronic stress has heuristic value; however, effect sizes cannot be readily extrapolated to other disabling conditions that require care.
Research on psychological adaptation of family dementia caregivers has several significant public health implications. Without substantial progress in prevention and treatment, the number of cases of late-life dementia in the United States could reach 13.5 million by the year 2050 (Brookmeyer et al., 1998; Hebert et al., 2003), exposing many older adults to care-related stress. High levels of negative emotion have been linked to a reduction in life expectancy for dementia caregivers (Schulz & Beach, 1999), indicating the potential for substantial physical “wear-and-tear” with long-term exposure to caregiver stress (Schulz et al., 1995). Furthermore, impaired caregiver psychological adaptation increases the risk for nursing home placement for the family member with a dementia syndrome (Gilley et al., 2005; Yaffe et al., 2002).
Modeling the emotional function of dementia caregivers provides information about the effects of chronic stress and factors that influence psychological adaptation. Our data add to the growing body of evidence that blacks have better emotional outcomes when exposed to the stress of providing informal care to a disabled family member. Research is needed to further explore the factors that contribute to this apparent advantage.
Acknowledgments
This study was supported by grants from the National Institute on Aging, National Institutes of Health (R01 AG09966, R01 AG10315). The authors thank study participants and their family members for commitment of time and energy to the project. We would like to acknowledge the significant contribution of Dr. David W. Gilley to the conceptualization, analytic interpretation, and portions of drafted text of this manuscript. We also thank Melinda Scheuer and her staff of research assistants for data collection activities, Todd Beck, M.S., for analytic programming, and George Dombrowski and his staff for data management.
References
- Allison PD. Logistic regression using the SAS® system: Theory and application. Cary, NC: SAS Institute Inc; 1999. [Google Scholar]
- Brookmeyer R, Gray S, Kawas C. Projections of Alzheimer’s disease in the United States and the public health impact of delaying disease onset. American Journal of Public Health. 1998;88:1337–1342. doi: 10.2105/ajph.88.9.1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connell CM, Gibson GD. Racial, ethnic, and cultural differences in dementia caregiving: Review and analysis. The Gerontologist. 1997;37:355–364. doi: 10.1093/geront/37.3.355. [DOI] [PubMed] [Google Scholar]
- Cornoni-Huntley J, Brock D, Ostfeld A, Taylor JO, Wallace RG, editors. Established populations for epidemiological studies of the elderly data book. Washington, DC: U.S. Government Printing Office; 1986. [Google Scholar]
- Dahlem NW, Zimet GD, Walker RR. The multidimensional scale of perceived social support: A confirmation study. Journal of Clinical Psychology. 1991;47:756–761. doi: 10.1002/1097-4679(199111)47:6<756::aid-jclp2270470605>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- Diggle PJ, Heagerty P, Liang KY, Zeger SL. Analysis of longitudinal data. 2. NY: Oxford University Press; 2002. [Google Scholar]
- Dilworth-Anderson P, Goodwin PY, Williams SW. Can culture help explain the physical health effects of caregiving over time among African American caregivers? Journal of Gerontology: Social Sciences. 2004;59:138–145. doi: 10.1093/geronb/59.3.s138. [DOI] [PubMed] [Google Scholar]
- Dilworth-Anderson P, Williams IC, Gibson BE. Issues of race, ethnicity, and culture in caregiving research: A 20-year review (1980–2000) The Gerontologist. 2002;42:237–272. doi: 10.1093/geront/42.2.237. [DOI] [PubMed] [Google Scholar]
- Farran CJ, Miller BH, Kaufman JE, Davis L. Race, finding meaning, and caregiver distress. Journal of Aging and Health. 1997;9:316–333. doi: 10.1177/089826439700900303. [DOI] [PubMed] [Google Scholar]
- Fetzer Institute. Multidimensional measurement of religiousness/spirituality for use in health research: A report of the Fetzer Institute/National Institute on Aging Working Group. Kalamazoo, MI: Health Research Program Area of the John E. Fetzer Institute; 1999. [Google Scholar]
- Folstein MF, Folstein S, McHugh PR. Mini-mental state: a practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Fredman L, Daly MP, Lazur AM. Burden among white and black caregivers to elderly adults. Journal of Gerontology: Social Sciences. 1995;50:110–118. doi: 10.1093/geronb/50b.2.s110. [DOI] [PubMed] [Google Scholar]
- Gilley DW, McCann JJ, Bienias JL, Evans DA. Caregiver psychological adjustment and institutionalization of persons with Alzheimer’s disease. Journal of Aging and Health. 2005;17:172–189. doi: 10.1177/0898264304274252. [DOI] [PubMed] [Google Scholar]
- Haley WE, Gitlin LN, Wisniewski SR, Mahoney DF, Coon DW, Winter L, et al. Well-being, appraisal, and coping in African American and Caucasian dementia caregivers: Findings from the REACH study. Aging & Mental Health. 2004;8:316–329. doi: 10.1080/13607860410001728998. [DOI] [PubMed] [Google Scholar]
- Haley WE, Roth DL, Coleton MI, Ford GR, West CA, Collins RP, et al. Appraisal, coping, and social support as mediators of well-being in Black and White family caregivers of patients with Alzheimer’s disease. Journal of Consulting and Clinical Psychology. 1996;64:121–129. doi: 10.1037//0022-006x.64.1.121. [DOI] [PubMed] [Google Scholar]
- Haley WE, West CA, Wadley VG, Ford GR, White FA, Barrett JJ, et al. Psychological, social, and health impact of caregiving: A comparison of Black and White dementia caregivers and noncaregivers. Psychology and Aging. 1995;10:540–552. [PubMed] [Google Scholar]
- Hebert LE, Scherr PA, Bienias JL, Bennett DA, Evans DA. Alzheimer’s disease in the U. S. population: Prevalence estimates using the 2000 census. Archives of Neurology. 2003;60:1119–1122. doi: 10.1001/archneur.60.8.1119. [DOI] [PubMed] [Google Scholar]
- Katz S, Alporn CA. A measure of primary sociological functions. International Journal of Health Services. 1976;6:493–508. doi: 10.2190/UURL-2RYU-WRYD-EY3K. [DOI] [PubMed] [Google Scholar]
- Knight BG, Silverstein M, McCallum TJ, Fox LS. A sociocultural stress and coping model for mental health outcomes among African American caregivers in southern California. Journal of Gerontology: Psychological Sciences. 2000;55:142–150. doi: 10.1093/geronb/55.3.p142. [DOI] [PubMed] [Google Scholar]
- Kohout FJ, Berkman LF, Evans DA, Cornoni-Huntley J. Two shorter forms of the CES-D depression symptoms index. Journal of Aging & Health. 1993;5:179–193. doi: 10.1177/089826439300500202. [DOI] [PubMed] [Google Scholar]
- Lawton MP, Kleban MH, Moss M, Rovine M, Glicksman A. Measuring caregiving appraisal. Journal of Gerontology: Psychological Sciences. 1989;44:61–71. doi: 10.1093/geronj/44.3.p61. [DOI] [PubMed] [Google Scholar]
- Lawton MP, Moss M, Kleban MH, Glicksman A, Rovine M. A 2-factor model of caregiving appraisal and psychological well-being. Journal of Gerontology: Psychological Sciences. 1991;46:181–189. doi: 10.1093/geronj/46.4.p181. [DOI] [PubMed] [Google Scholar]
- Lawton MP, Rajagopal D, Brody E, Kleban MH. The dynamics of caregiving for a demented elder among Black and White families. Journal of Gerontology: Psychological Sciences. 1992;47:156–164. doi: 10.1093/geronj/47.4.s156. [DOI] [PubMed] [Google Scholar]
- Li WL, Seltzer MM, Greenberg JS. Social support and depressive symptoms: Differential patterns in wife and daughter caregivers. Journal of Gerontology: Social Sciences. 1997;52:200–211. doi: 10.1093/geronb/52b.4.s200. [DOI] [PubMed] [Google Scholar]
- Li WL, Seltzer MM, Greenberg JS. Change in depressive symptoms among daughter caregivers: An 18-month longitudinal study. Psychology and Aging. 1999;14:206–219. doi: 10.1037//0882-7974.14.2.206. [DOI] [PubMed] [Google Scholar]
- McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer’s disease: Report of the NINCDS-ADRDA work group. Neurology. 1984;34:939–944. doi: 10.1212/wnl.34.7.939. [DOI] [PubMed] [Google Scholar]
- Miller B, Campbell RT, Farran CJ, Kaufman JE, Davis L. Race, control, mastery, and caregiver distress. Journal of Gerontology: Social Sciences. 1995;50:374–382. doi: 10.1093/geronb/50b.6.s374. [DOI] [PubMed] [Google Scholar]
- Peek MK, Coward RT, Peek CW, Lee GR. Are expectations for care related to the receipt of care? An analysis of parent care among disabled elders. Journal of Gerontology: Social Sciences. 1998;53:127–136. doi: 10.1093/geronb/53b.3.s127. [DOI] [PubMed] [Google Scholar]
- Roff LL, Burgio LD, Gitlin L, Nichols L, Chaplin W, Hardin JM. Positive aspects of Alzheimer’s caregiving: The role of race. Journal of Gerontology: Psychological Sciences. 2004;59:185–190. doi: 10.1093/geronb/59.4.p185. [DOI] [PubMed] [Google Scholar]
- Roth DL, Haley WE, Owen JE, Clay OJ, Goode KT. Latent growth models of the longitudinal effects of dementia caregiving: A comparison of African American and White family caregivers. Psychology and Aging. 2001;16:427–436. [PubMed] [Google Scholar]
- SAS Institute Inc. SAS Online Doc R 9.1.3. Cary, NC: SAS Institute Inc; 2004. [Google Scholar]
- Schulz R, Beach SR. Caregiving as a risk factor for mortality: The caregiver health effects study. Journal of the American Medical Association. 1999;282:2215–2219. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- Schulz R, O’Brien AT, Bookwala J, Fleissner K. Psychiatric and physical morbidity effects of dementia caregiving: prevalence, correlates, and causes. The Gerontologist. 1995;35:771–791. doi: 10.1093/geront/35.6.771. [DOI] [PubMed] [Google Scholar]
- Waite A, Bebbington P, Skelton-Robinson M, Orrell M. Social factors and depression in carers of people with dementia. International Journal of Geriatric Psychiatry. 2004;19:582–587. doi: 10.1002/gps.1136. [DOI] [PubMed] [Google Scholar]
- Watson D. Intraindividual and interindividual analyses of Positive and Negative Affect: Their relation to health complaints, perceived stress, and daily activities. Journal of Personality and Social Psychology. 1988;54:1020–1030. doi: 10.1037//0022-3514.54.6.1020. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- White TM, Townsend AL, Stephens MAP. Comparison of African American and White women in the parent care role. The Gerontologist. 2000;40:718–728. doi: 10.1093/geront/40.6.718. [DOI] [PubMed] [Google Scholar]
- Williams IC. Emotional health of black and white dementia caregivers: A contextual examination. Journal of Gerontology: Psychological Sciences. 2005;60:287–295. doi: 10.1093/geronb/60.6.p287. [DOI] [PubMed] [Google Scholar]
- Yaffee K, Fox P, Newcomer R, Sands L, Lindquist K, Dane K, et al. Patient and caregiver characteristics and nursing home placement in patients with dementia. Journal of the American Medical Association. 2002;287:2090–2097. doi: 10.1001/jama.287.16.2090. [DOI] [PubMed] [Google Scholar]