Abstract
Background
Neurofibrillary tangles and β-amyloid plaques have been observed in the amygdala in Alzheimer disease. A disproportionate abundance of this abnormality in the amygdala may cause behavioral symptoms similar to Klüver-Bucy syndrome.
Objectives
To describe an atypical behavioral presentation of Alzheimer disease and to review the literature on the subject.
Design
Case study.
Setting
Outpatient specialty clinic.
Patient
A 70-year-old man with progressive behavioral symptoms of hyperorality, hypersexuality, hypermetamorphosis, visual agnosia, hyperphagia, and apathy who died at age 77 of asphyxiation on a foreign object.
Main Outcome Measures
Clinical symptomatology, brain imaging, and neuropathology.
Results
The pathologic diagnosis was Alzheimer disease with abundant tangles and plaques in the lateral amygdala.
Conclusions
This case represents a variant of Alzheimer disease with prominent amygdala abnormalities and a Klüver-Bucy phenotype that was misdiagnosed as frontotemporal dementia. Clinical and imaging findings that may aid in accurate diagnosis are reviewed.
Alzheimer disease (AD) is characterized by memory dysfunction and a typical neuropathologic distribution pattern, particularly involving the entorhinal cortices and hippocampi.1 There is also a less appreciated body of literature that describes neurofibrillary tangles and amyloid plaques in the amygdalae,2–5 which may be linked to behavioral presentations of AD similar to Klüver-Bucy (KB) syndrome. We describe a patient with symptoms of KB syndrome pathologically confirmed to have AD with an atypically abundant amount of neurofibrillary tangles and neuritic plaques in the amygdala.
REPORT OF A CASE
A 70-year-old man had a 7-year history of mild memory difficulty and behavioral changes of insidious onset. He complained of poor memory but compensated with notes; it was noted that this was a factor in his decision to retire early (age 63) from his job as a school administrator. His wife was concerned about his progressive behavioral changes, specifically, sexual inappropriateness. For example, he flirtatiously approached a female parishioner and proceeded to hug and repeatedly kiss her. He lacked insight and said to the woman, “Why don’t we do it again?” Becoming increasingly suspicious, he thought his wife was stealing money. He was described as uncharacteristically “mean” and verbally aggressive. He remained functionally independent except for some problems handling finances, but he refused assistance. Although he was still driving, he was getting lost when in unfamiliar areas.
His medical history included asthma, hypertension, gout, and sleep apnea. He had no psychiatric history. His medications were albuterol, ipratropium bromide, cromolyn sodium, triamcinolone, theophylline, allopurinol, and indomethacin. There was no history of alcohol, tobacco, or other substance use. His sister and father had unspecified late-onset dementia.
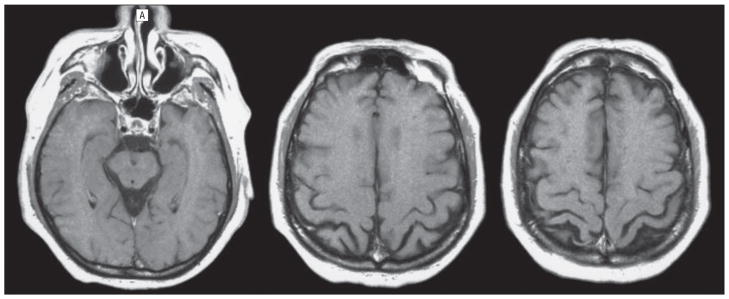
On examination, he was observed to be obese (107.55 kg, 167.64 cm tall) and “jocular and inappropriate.” His Mini-Mental State Examination score was 30 of 30. Results of his neurologic examination were normal except for symmetrical hyporeflexia, marginally impaired graphesthesia, and a right palmomental sign. Neuropsychological testing revealed impairment in object naming and mild impairment in acquisition, with otherwise normal scores (Table). Basic chemistries, complete blood cell count, thyrotropin level, vitamin B12 level, and microhemagglutination Treponema pallidum level were normal. Brain magnetic resonance imaging revealed a 0.7 × 2-cm meningioma adjacent to the left sylvian fissure and very mild subcortical punctate white matter changes; otherwise, the results were interpreted as normal. Retrospective review of these images suggested bilateral parietal atrophy (Figure 1). The initial clinical impression was mild frontotemporal dementia (FTD).
Table.
Neuropsychological Test Results for the Patient at Ages 70 to 74 Yearsa
| Neuropsychological Test | Patient Ages, y |
||||
|---|---|---|---|---|---|
| 70 | 71 | 72 | 73 | 74 | |
| MMSE score | 30 | 29 | 28 | 27 | 18 |
| Attention | |||||
| Digit Span score | 13 (97) | 14 (101) | 13 (97) | 9 (82) | 9 (82) |
| Language | |||||
| Boston Naming Test score | 39 (55) | 39 (55) | 31 (<55) | 23 (<55) | 16 (<55) |
| Memory score | |||||
| Logical Memory I | 16 (89) | 9 (76) | 7 (71) | 4 (65) | 3 (63) |
| Logical Memory II | 11 (97) | 7 (87) | 0 | 0 | NA |
| Visuoperception | |||||
| Block design score | 20 (105) | 27 (115) | 20 (105) | 12 (90) | 16 (100) |
Abbreviations: MMSE, Mini-Mental State Examination; NA, not applicable.
Standard scores are given in parentheses (mean [SD], 100 [15]).
Figure 1.
Brain magnetic resonance images of the patient at age 72 years showing slightly enlarged biparietal sulci and the absence of frontal or temporal lobar atrophy.
During the next 2 years, he reported that he began having more prominent sexual fantasies about other women while also becoming increasingly suspicious that his wife was cheating on him; he was prescribed paroxetine mesylate. His Mini-Mental State Examination score remained at 28 of 30; however, the neuropsychological studies began to show clear deficits in delayed recall and language with spared visuoperceptive ability (Table). Positron emission tomography (PET) demonstrated hypometabolism in the bilateral parietal and anterotemporal regions (Figure 2). The possibility of AD was considered, but the leading diagnosis remained FTD. From the ages of 74 to 77 years, he had a substantial decline in cognitive function, and his Mini-Mental State Examination score declined to 7. He displayed increasing hyperorality, and his wife noted that he would put “any” object in his mouth, including dog food, candles, adhesive bandages, and his wedding ring. His appetite seemed insatiable. He would reach into the toilet to manipulate fecal matter. When asked by his wife to get a rake, he brought a screwdriver. He became progressively withdrawn and apathetic. During the last year of his life, he required assistance with most activities of daily living. He died at age 77 years of asphyxiation on several adhesive bandages.
Figure 2.
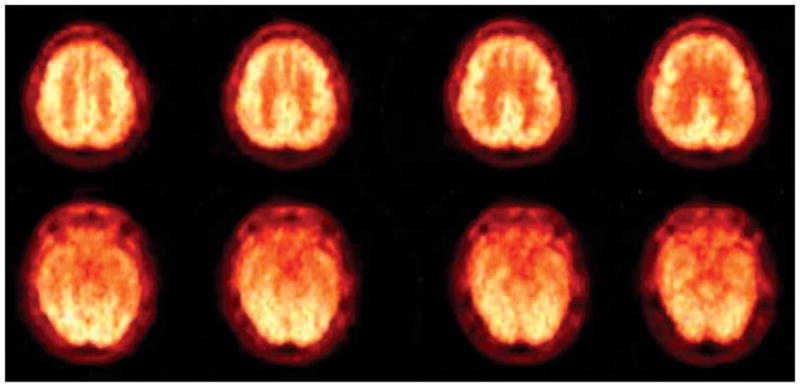
Positron emission tomography with radiolabeled fluorodeoxyglucose in the patient at age 73 years showing hypometabolism in the bilateral parietal and anterotemporal regions.
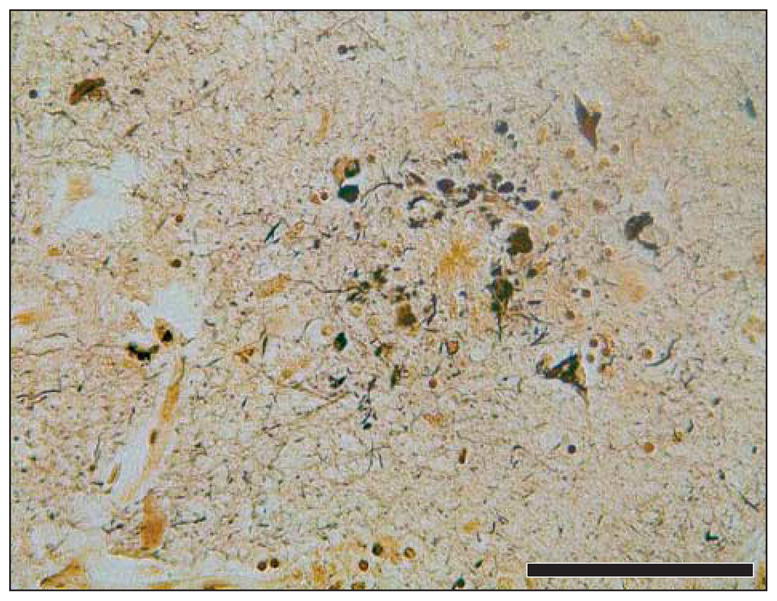
The pathologic diagnosis was AD with abundant neurofibrillary tangles and moderate neuritic plaques throughout the brain (Braak and Braak stage VI and a CERAD [Consortium to Establish a Registry for Alzheimer’s Disease] rating of “frequent”). The brain weight was 1400 g. The distribution of tangles and plaques was similar to that encountered in sporadic AD with this staging; however, the degree of amygdala abnormality was atypical. Neurofibrillary tangles were abundant in the lateral amygdala (approximately 150 per 1.6 mm2) (Figure 3 and Figure 4). This number of tangles is greater than 4+ (>50 tangles per 1.6 mm2) using the Kromer Vogt rating system for tangles in the amygdala in AD.2 There were neuritic plaques in the lateral, laterobasal, and accessory basal amygdala ranging from approximately 10 to 20 per 1.6 mm2 (Figure 5); 2+ Kromer Vogt rating for plaques in the amygdala.2 The amygdala showed moderate neuronal depletion and gliosis. There was also evidence of grade II cerebral amyloid angiopathy. Genetic testing showed that the patient had apolipoprotein E 3/3; presenilin genotyping was not performed.
Figure 3.
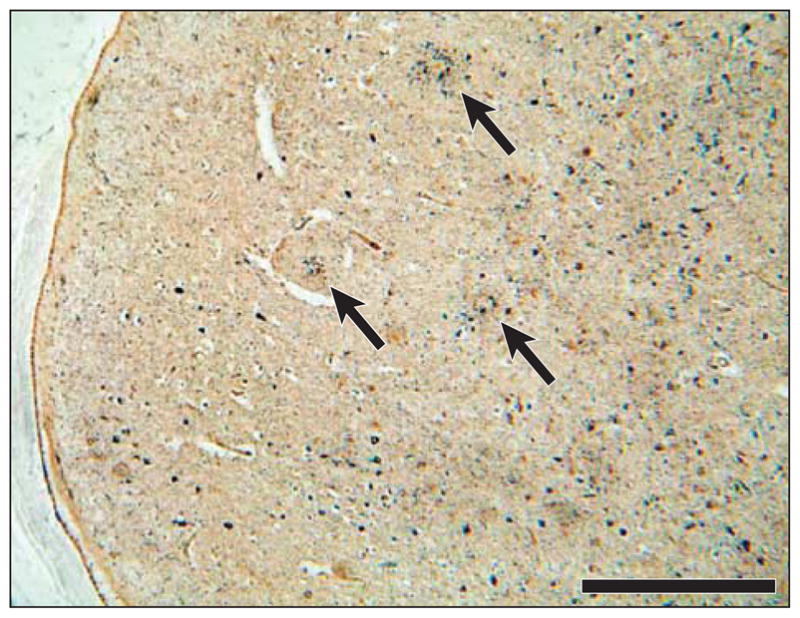
Bielschowsky silver impregnation staining showing an overview of large neuritic plaques (arrows) and smaller neurofibrillary tangles in the lateral amygdala adjacent to the inferior horn of the lateral ventricle. Bar=0.5 mm.
Figure 4.
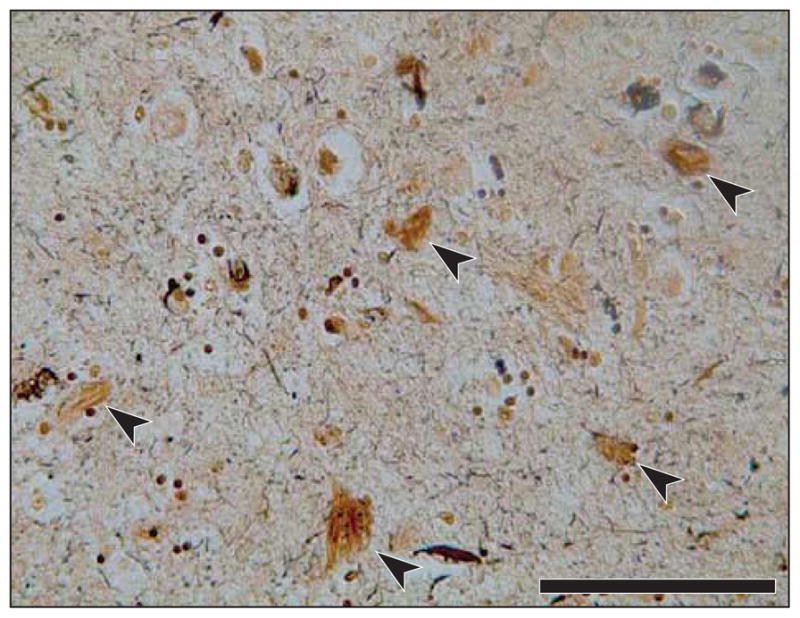
Bielschowsky silver impregnation staining showing a higher-power view of neurofibrillary tangles (arrowheads) in the lateral amygdala (approximately 150 tangles per 1.6 mm2). Bar=0.1 mm.
Figure 5.
Bielschowsky silver impregnation staining showing a higher-power view of neuritic plaques, amyloid core, and surrounding tangles (approximately 10–20 neuritic plaques per 1.6 mm2). Bar=0.1 mm.
COMMENT
Described by Klüver and Bucy in the late 1930s, this behavioral syndrome is associated with bilateral amygdala lesions and is characterized by the following cluster of symptoms: hypersexuality, hyperorality, hypermetamorphosis (excessive exploration of visual stimuli), visual agnosia, apathy, and withdrawal.6 The amygdala processes sensory information for emotional valence; therefore, amygdala lesions cause abnormal emotional responses, resulting in aggressiveness, fearlessness, or apathy.7 Lesion studies8 in rats demonstrate that efferent projections from the posterodorsal amygdala to the hypothalamus lead to hyperphagia, obesity, and sexual dysregulation. Projections between the visual cortex and the amygdala have been mapped in nonhuman primates.9 Injury to these projections likely underlies the visual agnosia and hypermetamorphosis observed in patients with amygdala lesions.
Sourander and Sjogren10 described KB syndrome symptoms in patients with AD. Morris et al11 suggested that excessive eating in some patients with dementia may be a form of KB syndrome. Burns and colleagues12 examined 178 patients with AD to quantify the number of KB syndrome symptoms: 29.3% had 1, 24.7% had 2, 17.2% had 3, 8.6% had 4, and 0.6% had all the KB syndrome symptoms.
Neuronal loss in the medial, central, and cortical nuclei of the amygdala has been observed in AD.13,14 Amyloid plaques and neurofibrillary tangles are consistently present in the amygdala in AD.3–5 The present patient had 150 tangles per 1.6 mm2 in the lateral amygdala. By comparison, 14 other AD brains with Braak and Braak stage VI were studied and were found to have 5 to 90 tangles per 1.6 mm2 in the amygdala. Kromer Vogt et al2 investigated the amygdala abnormalities of 20 patients with AD and demonstrated a significant amount of tangles and neuritic plaques in the cortical nucleus and accessory basal nucleus of the amygdala, which have projections with the hippocampus; however, the lateral nuclei of the amygdala were relatively spared (1 patient had a 4+ tangle score and 1 had a 3+ plaque score). Compared with patients with typical AD described by Kromer Vogt et al,2 the patient described herein had significant tangle and plaque density in the lateral amygdala. Hayman and colleagues15 also described a patient with KB syndrome after lateral amygdala lesions.
This is the first published study of this amygdaloid variant of AD with serial neuropsychological testing, magnetic resonance imaging, PET, and pathologic analysis. A frontal variant of AD with prominent behavioral symptoms has been described.16 The frontal variant is characterized by an atypical distribution of AD abnormalities in the frontal lobes that may be more difficult to distinguish from FTD. In contrast, PET of this patient revealed the typical pattern of posterior hypometabolism. This tool might be a useful diagnostic aid. Behavioral variants of AD are primarily a diagnostic challenge because several of the symptoms overlap with FTD.17 Cognitive-behavioral symptoms in AD often respond to acetylcholinesterase inhibitors, and misdiagnosis of FTD might preclude this intervention and other potential disease-modifying agents for AD that are currently being investigated. Also, FTD has more rapid progression, with mean survival of 4.2 years from initial evaluation compared with 6 years for AD.18
This patient’s prominent behavioral symptoms led to the incorrect diagnosis of FTD. There were, however, a variety of noteworthy signs and imaging clues that pointed toward the correct diagnosis of AD. The patient noted memory dysfunction, and delayed memory scores were very poor relatively early in the illness. Age at presentation was late, and the course was relatively slow. Magnetic resonance imaging showed evidence of biparietal atrophy. The PET demonstrated biparietal hypometabolism consistent with AD. The specificity and sensitivity of PET, used to differentiate between AD and FTD, were recently shown to be superior to those of clinical assessment alone.19 Furthermore, the positive finding of temporoparietal hypometabolism is strongly associated with AD abnormalities even in the presence of atypical features.20
Acknowledgments
Funding/Support: This work was funded by grant P30 AG10129 from the National Institutes of Health.
Footnotes
Financial Disclosure: None reported.
Author Contributions: All authors had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Kile, Olichney, and DeCarli. Acquisition of data: Kile, Ellis, and Farias. Analysis and interpretation of data: Kile, Olichney, and Farias. Drafting of the manuscript: Kile and Farias. Critical revision of the manuscript for important intellectual content: Kile, Ellis, Olichney, and DeCarli. Administrative, technical, and material support: Kile and Farias. Study supervision: Ellis, Olichney, Farias, and DeCarli.
Additional Contributions: We thank the subject volunteers and their caregivers for their generous contributions.
References
- 1.Braak H, Braak E. Staging of Alzheimer’s disease-related neurofibrillary changes. Neurobiol Aging. 1995;16(3):271–278. doi: 10.1016/0197-4580(95)00021-6. [DOI] [PubMed] [Google Scholar]
- 2.Kromer Vogt LJ, Hyman BT, Van Hoesen GW, Damasio AR. Pathological alterations in the amygdala in Alzheimer’s disease. Neuroscience. 1990;37(2):377–385. doi: 10.1016/0306-4522(90)90408-v. [DOI] [PubMed] [Google Scholar]
- 3.Hedreen JC, Broadhead JC, Price DL. Senile plaques in the amygdala in Alzheimer’s disease. Neurology. 1988;38(2 suppl 1):227. [Google Scholar]
- 4.Brady DR, Mufson EJ. Amygdaloid pathology in Alzheimer’s disease: qualitative and quantitative analysis. Dementia. 1990;1:5–17. [Google Scholar]
- 5.Unger JW, Lapham LW, McNeill TH, Eskin TA, Hamill RW. The amygdala in Alzheimer’s disease: neuropathology and Alz 50 immunoreactivity. Neurobiol Aging. 1991;12(5):389–399. doi: 10.1016/0197-4580(91)90063-p. [DOI] [PubMed] [Google Scholar]
- 6.Kluver H, Bucy PC. Preliminary analysis of the temporal lobes in monkeys. Arch Neurol Psychiat. 1939;42:979–1000. doi: 10.1176/jnp.9.4.606. [DOI] [PubMed] [Google Scholar]
- 7.Mesulam MM. Principles of Behavioral and Cognitive Neurology. 2. New York, NY: Oxford University Press; 2000. Behavioral neuroanatomy: large-scale networks, association cortex, frontal syndrome, the limbic system, and hemispheric specializations; pp. 56–59. [Google Scholar]
- 8.King BM. Amygdaloid lesion-induced obesity: relation to sexual behavior, olfaction, and the ventromedial hypothalamus. Am J Physiol Regul Integr Comp Physiol. 2006;291(5):R1201–R1214. doi: 10.1152/ajpregu.00199.2006. [DOI] [PubMed] [Google Scholar]
- 9.Freese JL, Amaral DG. The organization of projections from the amygdala to visual cortical areas TE and V1 in the macaque monkey. J Comp Neurol. 2005;486(4):295–317. doi: 10.1002/cne.20520. [DOI] [PubMed] [Google Scholar]
- 10.Sourander P, Sjogren H. The concept of Alzheimer’s disease and its clinical implications. In: Wolstenholme GEW, O’Connor M, editors. Alzheimer’s Disease and Related Conditions. London, England: Churchill Livingstone; 1970. pp. 11–36. [Google Scholar]
- 11.Morris CH, Hope RA, Fairburn CG. Eating habits in dementia: a descriptive study. Br J Psychiatry. 1989;154:801–806. doi: 10.1192/bjp.154.6.801. [DOI] [PubMed] [Google Scholar]
- 12.Burns A, Jacoby R, Levy R. Psychiatric phenomena in Alzheimer’s disease, IV: disorders of behaviour. Br J Psychiatry. 1990;157:86–94. doi: 10.1192/bjp.157.1.86. [DOI] [PubMed] [Google Scholar]
- 13.Scott SA, DeKosky ST, Sparks DL, Knox CA, Scheff SW. Amygdala cell loss and atrophy in Alzheimer’s disease. Ann Neurol. 1992;32(4):555–563. doi: 10.1002/ana.410320412. [DOI] [PubMed] [Google Scholar]
- 14.Herzog AG, Kemper TL. Amygdaloid changes in aging and dementia. Arch Neurol. 1980;37(10):625–629. doi: 10.1001/archneur.1980.00500590049006. [DOI] [PubMed] [Google Scholar]
- 15.Hayman LA, Rexer JL, Pavol MA, Strite D, Meyers CA. Klüver-Bucy syndrome after bilateral selective damage of amygdala and its cortical connections. J Neuropsychiatry Clin Neurosci. 1998;10(3):354–358. doi: 10.1176/jnp.10.3.354. [DOI] [PubMed] [Google Scholar]
- 16.Johnson JK, Head E, Kim R, Starr A, Cotman CW. Clinical and pathological evidence for a frontal variant of Alzheimer disease. Arch Neurol. 1999;56(10):1233–1239. doi: 10.1001/archneur.56.10.1233. [DOI] [PubMed] [Google Scholar]
- 17.Neary D, Snowden JS, Gustafson L, et al. Frontotemporal lobar degeneration: a consensus on clinical diagnostic criteria. Neurology. 1998;51(6):1546–1554. doi: 10.1212/wnl.51.6.1546. [DOI] [PubMed] [Google Scholar]
- 18.Rascovsky K, Salmon DP, Lipton AM, et al. Rate of progression differs in frontotemporal dementia and Alzheimer disease. Neurology. 2005;65(3):397–403. doi: 10.1212/01.wnl.0000171343.43314.6e. [DOI] [PubMed] [Google Scholar]
- 19.Foster NL, Heidebrink JL, Clark CM, et al. FDG-PET improves accuracy in distinguishing frontotemporal dementia and Alzheimer’s disease. Brain. 2007;130(pt 10):2616–2635. doi: 10.1093/brain/awm177. [DOI] [PubMed] [Google Scholar]
- 20.Jagust W, Reed B, Mungas D, Ellis W, DeCarli C. What does fluorodeoxyglucose PET imaging add to a clinical diagnosis of dementia? Neurology. 2007;69(9):871–877. doi: 10.1212/01.wnl.0000269790.05105.16. [DOI] [PubMed] [Google Scholar]