Abstract
Objectives
To examine the accuracy and validity of self report of hip replacement (HR) for osteoarthritis.
Methods
We compared self-reported HR and the reason for surgery in elderly white women aged ≥ 65 years from the Study for Osteoporotic Fractures cohort to medical records and pelvis radiographs. Women, followed up for an average of 8 years at the fifth clinic visit were asked about any HRs since baseline.
Results
Among 7421 women attending the fifth clinic visit, 347 reported 387 HRs. Radiographs and/or medical records were available for 316 self-reported HRs. Participants accurately reported that HRs were for arthritis or fracture, with 94.5% and 97.2% of these self-reported diagnoses, respectively, confirmed from medical records. However, 1 in 8 self-reported HRs were not attributed by participants to either arthritis or a fracture; of these, medical records indicated that 88% were for osteoarthritis. Overall, 302 (95.6%) of self-reported HRs were confirmed as HRs (kappa for agreement with self-report = 0.95, 95% CI: 0.92–.96). Under-reporting of HRs compared to HRs seen on radiographs was minimal (0.28%).
Conclusion
Elderly women accurately report HRs and whether the surgery is for arthritis or a hip fracture, though a small number of HRs for arthritis are not attributed to this diagnosis by women. Since hip osteoarthritis and hip fracture have very different determinants, epidemiologic studies that use self-reported HR as an indicator for the presence of hip osteoarthritis or as an outcome of hip osteoarthritis should verify the underlying cause by asking about reason for surgery.
Self-report is an efficient method for obtaining information on medical diagnoses and interventions in large clinical and epidemiological studies. The need to use such self-report data is increasing along with the growing cost and difficulty of obtaining access to medical records. Studies have shown that the accuracy of self-report health data varies substantially by diagnosis and treatment [1–4], so validity needs to be documented for individual conditions and procedures. Hip replacement (HR) is a common and expensive treatment for end-stage hip osteoarthritis (OA) in older women. HR for hip OA ascertained from medical records has been widely used to study risk factors and outcomes of hip OA in epidemiological studies [5–7]. Because a high proportion of HR surgeries are for conditions other than OA, including hip fracture [8, 9] and bone necrosis [10], the validity of self-report of HR for hip OA needs to be thoroughly examined. Yet we have found only one study that assessed the accuracy of HR. Liu et al examined the accuracy of self-reported primary HR for any diagnosis in Scottish women aged 50 to 64 years, and found a greater than 99% agreement with hospital admission records [11]. However, this study did not distinguish between the different reasons for a HR, and hence the results cannot be generalized to HR specifically for OA, particularly in elderly populations where treatment of hip fracture with HR is common.
In this study we examined the accuracy of self-reports of HR during the previous 8 years, reason for surgery, and side and date of surgery compared with medical records and pelvis radiographs in a large cohort study of elderly women.
Materials and Methods
Subjects
Subjects were participants in the Study of Osteoporotic Fractures. Caucasian women 65 years or older were recruited from population based listings at four clinical centers in the United States [12]. All women were community dwelling and able to walk without the assistance of another person at the baseline examination. Women with bilateral hip replacements were excluded from the original cohort.
Baseline and follow up assessments
Participants completed baseline and follow-up mailed questionnaires and clinic examinations at 2 year intervals beginning in 1985. At the fifth clinic visit, an average of 8.3 years after the baseline visit, participants responded to a self-administered question asking “Since you first visited the clinic, about 8 years ago, have you had hip replacement surgery where part or all of your hip joint was replaced”. Those reporting a HR were asked whether the right, left or both hips were replaced and the reason for a HR, with response options of “arthritis”, “hip fracture” and “other”. Individuals were allowed to report more than one reason for the HR on the questionnaire. Those not attending follow-up visits were asked to complete the same self-administered questionnaires (SAQ). Similar questions about hip replacement were asked at previous follow-up visits, but we analyzed only the report from the fifth visit in order to assess the accuracy of long-term recall.
Covariates assessed at visit 5 include, age, self reported health status, self-reported history of a physician diagnosis OA in any joint, self-reported hip pain on most days of the month, body weight and height, cognitive function and physical disability. Cognitive function was measured using the modified Mini-Mental State Examination (MMSE), with higher scores on a scale of 0 to 30 representing better cognition [13]. An index of lower extremity function was assessed with a five item questionnaire [14]. Body weight and height were measured, and body mass index (BMI) was calculated as weight in kilograms divided by the square of height in meters. Other data only available at the baseline visit included years of education.
Radiographs and medical records
Supine pelvis radiographs of the hip were obtained at baseline in all subjects and in those who attended the fifth clinic visit, plus 461 subjects who did not come to the clinic but had a pelvis film using portable equipment at their place of residence. During the reading of paired baseline and follow-up radiographs for hip OA, the presence of a HR at baseline and new (first) HRs during follow-up were recorded.
For women who reported having a HR during follow-up for “arthritis” or “other”, after obtaining their consent, we requested medical records of the surgery, including a discharge summary and operative report. As part of a separate set of procedures for fracture ascertainment and adjudication in SOF, information on fractures was collected every four months when participants were requested to fill out postcards indicating if they had fractured any bone. For all reported hip fractures, after obtaining participant’s consent we requested a copy of the radiologist’s report and the preoperative radiograph, which were reviewed by a radiologist to confirm the occurrence of a hip fracture [15].
Confirmation of HR
Self-reported HRs were verified using the available medical records and/or pelvis radiographs. Self-report of a HR that occurred during follow-up was classified as “confirmed” when the medical records and/or reading of the pelvis radiographs for OA were available and identified a primary (first) HR that occurred during follow-up. A self-reported HR was classified as a “false positive” when the surgical medical and/or reading of the pelvis radiographs for OA were available and did not indicate that a HR had occurred during follow-up. If the medical record and radiograph reading were in conflict on whether a HR occurred, the pelvis radiographs were reviewed by an experienced rheumatologist (NEL) whose interpretation was accepted.
A self-reported HR for which we had neither medical records of the surgery nor follow up pelvis radiograph readings available was classified as an unconfirmed report. Hips with evidence of a HR on the baseline radiograph were excluded from this study since we were interested in self report of a first of HR since baseline.
Under-reporting of HR
We defined under-reporting of HR (false negatives) in those who reported no HR during follow-up as evidence of a new HR during follow-up on the pelvis radiograph.
Ascertainment and classification of reason for HR
The diagnosis associated with a confirmed HR was determined using the medical records obtained for HR surgery and/or for the adjudication of a self-reported hip fracture. The reason for a confirmed HR was classified as “OA” if the medical record was obtained and stated that a HR was performed for “osteoarthritis”, “degenerative arthritis” or “degenerative joint disease” of the hip and there was no mention of “osteonecrosis”, “hip fracture”, or a “failed prosthesis”. The reason for a confirmed HR was classified as “other” when the medical record indicated a diagnosis other than osteoarthritis or fracture. The reason for a confirmed HR was classified as “hip fracture” when a) the medical record was obtained for a reported HR and stated that the HR was for a hip fracture or b) the radiograph reading identified a new HR and the fracture adjudication data indicated that a hip fracture had occurred within one year prior to the self-reported date of a HR. One year or less criteria for confirming HR for fracture was used since there were very few HRs that occurred more than 3 months after the hip fracture (N=7). If a hip fracture occurred more than one year before the HR then the reason for HR was considered unknown. However, there were none of these. When medical records of the surgery were not available and the HR was confirmed by radiograph and there was no confirmed hip fracture, then the reason for HR was considered unknown. Similarly if there was a confirmed hip fracture but no medical records or radiographs to confirm the presence of HR, the reason for HR was considered unknown.
Analysis
We analyzed accuracy of self-report of HR in women who completed the fifth clinic visit SAQ. Hips were the unit of analysis for determining agreement between self-report and medical records or radiographs. Hips with a HR on the baseline radiograph were excluded. For self-reported HR that either had medical records or had radiograph data, we calculated the percent of reported HRs that were confirmed and the percent that were false positives. This was done for all HRs combined and for each self-reported reason for surgery. Unconfirmed reports of HR were not included in these calculations. The percent of false negatives was calculated as the number of persons with confirmed HRs based on pelvis radiograph readings but reported no HR divided by the total number of those who reported no HR.
For confirmed HR, we determined the accuracy of the reported diagnosis of HR calculated for each category assessed. Women who reported that a HR was for arthritis and “other” reasons were counted as reporting HR for arthritis. Similarly women who reported HR for both fracture and for “other” reasons were counted as reporting HR for fracture. Kappa statistics were calculated for the agreement between self-reported HR and confirmed HR for OA and fracture. In addition, we determined the accuracy of the side and date of the reported operation among women who reported a HR accurately. The accuracy of the reported side of HR was defined as the number of hips for which women reported the correct side of HR operation divided by the total number of hips confirmed for a HR. We compared the self-reported month and year of operation with the month and year of operation reported on the medical records to access accuracy of date of operation.
We compared visit 5 subject characteristics for false positive reports and unconfirmed HRs with confirmed HRs using analysis of variance for continuous variables and chi-square tests for categorical variables. All analyses were performed using the SAS statistical package version 9.1 (SAS Institute, Inc., Cary, NC).
Results
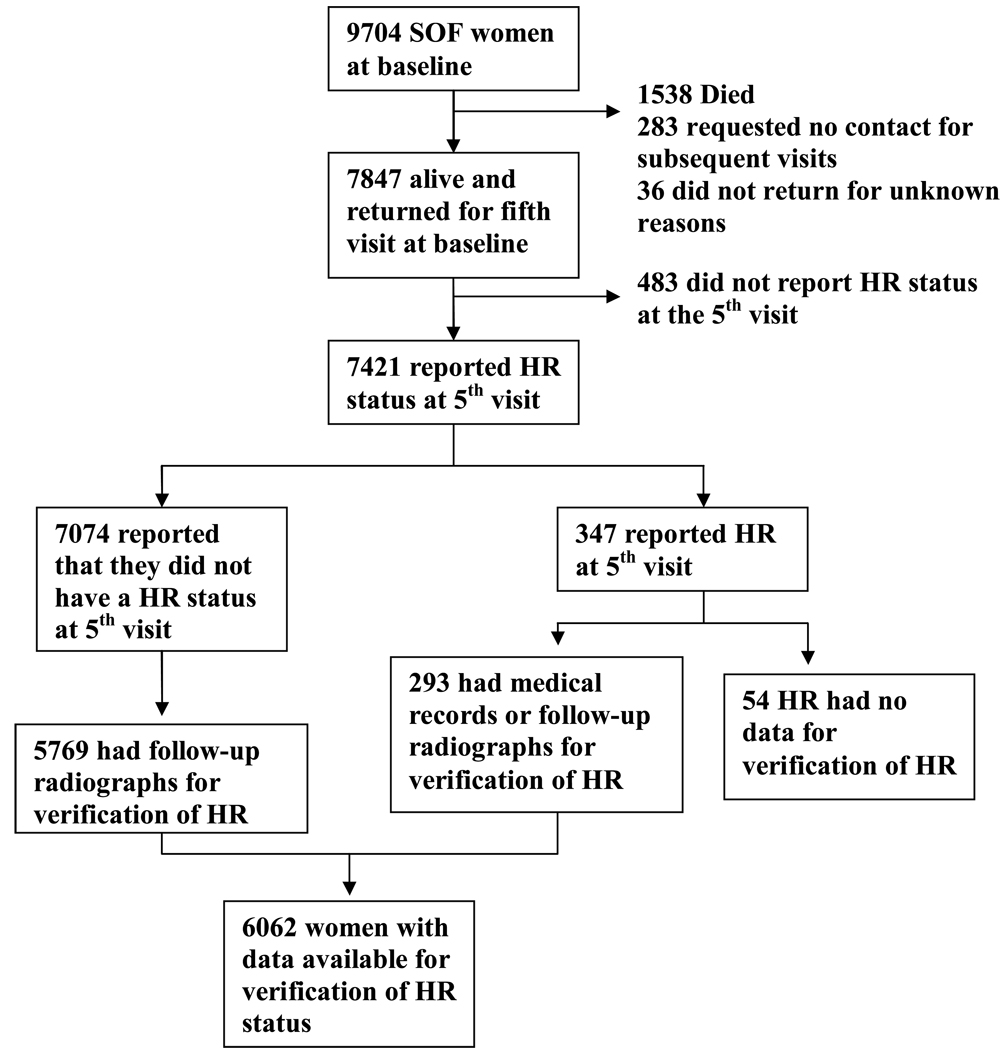
A flow chart of the participants included in the analysis for verification of HR status is presented in figure 1.
Figure 1.
Flow chart of SOF participants with available data to verify THR status: This figure shows selection of women for the study from women in the Study of Osteoporotic Fractures (SOF) cohort.
Overall there was excellent agreement between self reported HRs and confirmed HR with pelvis radiographs and or medical records (kappa= 0.95 CI 95% 0.92–0.96). Among the 6062 women with available medical records or radiographs for verification of their HR status, 293 women reported 316 HRs at visit 5. Of these 293 women, a HR was confirmed in 280 (95.6%) women reporting at least one confirmed HR (table 1). Of the 316 hips reported as having a HR, 302 (95.6%) were confirmed from medical records or radiographs (table 1). Of 206 HR reported for arthritis, data for HR confirmation was available in 183; 98.9% of these were confirmed as a HR (data not shown in tables). There were a total of 14 (4.3%) false positive reports in 13 women (table 1). Of these, 2 were reported by participants as being for arthritis and 12 were reported for hip fracture (of which 9 had a confirmed hip fracture and a surgically implanted pin but no HR), (data not shown in tables). The cumulative incidence in women between baseline and visit 5 of self reported HRs and of confirmed HRs was 4.8% (293/6062) and 4.3% (259/6062) respectively.
Table 1.
Characteristics of participants at fifth visit when their HR status was assessed: The Study of Osteoporotic Fractures 1995–1996
| Characteristics | Women not reporting HR (N=7074)a |
Overall (347 women)¥ |
Women reporting a HR | ||
|---|---|---|---|---|---|
| Confirmed (280 women)& |
‡False positives (13 women)†, |
‡Unconfirmed (54 women)¶, |
|||
| Current age, mean± std |
78.8 ± 4.8 | 80.0 ± 5.2 | 79.5±4.8 | *83.0 ± 6.1 | *82.2 ±6.3 |
|
bEducation ≥ 12 years, n (%) |
2751 (38.9) | 152 (43.9) | 130 (46.6) | 5 (38.5) | *17 (31.5) |
| Body Mass Index (kg/cm2), mean± std |
26.5 ± 4.8 | 26.6 ± 5.4 | 26.7 ± 5.5 | 25.8 ± 3.4 | 25.6 ± 3.7 |
| History of OA, n (%) |
1260 (17.8) | 119 (34.4) | 100 (35.7) | 4 (30.8) | 15 (28.3) |
| Good vs. poor Health, n (%) |
5493 (77.7) | 259 (74.6) | 214 (76.4) | 10 (76.9) | 35 (64.8) |
|
bHip Pain on most days of the month, n (%) |
2155 (30.7) | 199 (57.9) | 166 (59.7) | *4 (30.8) | 29 (54.7) |
| Lower limb disability (range 0– 15), mean ± std |
2.1 ± 3.5 | 4.1 ± 4.6 | 3.6 ± 4.2 | 3.2 ± 4.3 | **7.4 ± 5.7 |
| Mini Mental Status, mean ± std |
24.2 ± 2.2 | 24.0 ± 2.4 | 24.1± 2.2 | 23.73 ± 1.7 | 23 ± 4.5 |
| Live alone, n (%) | 3556 (50.7) | 186 (54.6) | 156 (56.5) | 6 (46.2) | 25 (46.3) |
| SAQ completed by Participant, n (%) |
6820 (96.5) | 328 (94.5) | 275 (97.5) | 14 (100) | *42 (77.8) |
| Relative, friend or staff, n (%) |
135 (1.9) | 13 (3.8) | 2 (0.7) | 0 | 11 (20.4) |
| Participant and other, n (%) |
115 (1.6) | 6 (1.7) | 5 (1.8) | 0 | 1 (1.9) |
p-values compared to women who reported a confirmed THR
p-value <0.05
p-values <0.0001
Includes 1305 women whose HR status could not be verified due to lack of medical records or pelvic x-rays.
assessed at baseline visit
387 hips reported as having HR of which 40 were bilateral HR reports.
301 hips with confirmed HRs of which 21 were bilateral. Also includes an additional 9 women who reported a bilateral HR of which 1 had only a unilateral HR and 8 who’s HR on the other side could not be verified due to lack of medical records or pelvic x-rays.
14 hips reported as having HR but were false positive reports of which 1 bilateral HR was reported but had no HR on either hip.
No data available for HR verification in 63 hips reporting a HR of which 9 were bilateral HR reports
Several characteristics of the 7421 women who provided self-report data on HR at the fifth clinic visit (1995–1996) are presented in table 1. Sixty three self-reported HRs in 54 women could not be verified or confirmed due to lack of medical records and radiographs. These women were significantly older, less educated and had higher lower limb disability compared to women who had a confirmed HR. Similarly women who falsely reported HR were older and reported less hip pain on most days of the month. Other subject characteristics were similar in each of the two groups for women compared to women with confirmed HR (table 1).
Underreporting of HRs
16 women reporting no HR in 18 hips were confirmed to have a HR from radiographs resulting in a false negative rate of 0.28% (data not shown in tables). 50% of the false negatives had a confirmed hip fracture one year prior to the HR. Medical records were lacking to determine the reason for the remaining 50% of the false negatives.
Accuracy of reported reason for HR
Table 2 shows the self-reported reason for surgery for all 387 HRs and for the 290 (76.7%) HRs with medical records for HR reported for arthritis and other and radiographs and hip fracture adjudication data available for HR reported for fracture. Overall, 69% of the confirmed HRs were for OA based on the medical records data, while slightly over a quarter were due to hip fractures. Only 2.9% were due to reasons other than OA or hip fracture.
Table 2.
Verification of self reported HR and the reported diagnoses
| Self-reported reason for hip replacement: |
aHRs with verification data available |
Confirmed | Confirmed for | ||
|---|---|---|---|---|---|
| hip fracture |
OA | other reason | |||
| N | 1 (1/N) |
2 (2/1) |
3 (3/1) |
4 ((1-(3+2)/1) |
|
| Arthritis | 166 | 165 | 4 | 156 | 5 |
| (N=206 ) | (80.6%) | (99.4%) | (2.4%) | (94.5%) | (3.0%) |
| Fracture | 81 | 72 | 70 | 2 | 0 |
| (N=130) | (62.3%) | (88.9%) | (97.2%) | (2.8%) | (0%) |
| Other | 34 | 34 | 3 | 30 | 1 |
| (N=42 ) | (81%) | (100%) | (8.8) | (88.2%) | (2.9%) |
| None given | 7 | 6 | 0 | 4 | 2 |
| (N=9) | (77.8%) | (85.7%) | (66.7%) | (50%) | |
| Total self reported | 290 | 277 | 77 | 192 | 8 |
| HRs (N=387) | (76.7%) | (95.5%) | (28.4%) | (69.3%) | (2.9%) |
For reported HR for fracture, had to have both pelvic radiograph and medical records. All others had to have medical records.
Evaluation of the self-reported reasons for the HR indicated a very high accuracy rate of 94.5% for HRs reported by the participant as due to arthritis. The remaining 2.4% reported for arthritis were confirmed as HR due to fracture and 3% for some other reason (1 for rheumatoid arthritis, 4 for aseptic necrosis). Seventy-two confirmed HRs were reported by participants as due to facture and had available data for verification of reason of HR; 70 (97.2%) were confirmed as for fracture and 2 (2.8%) were confirmed as for OA (table 2). Kappa for agreement between self-reported diagnosis of HR for arthritis and HR for fracture as the reason for surgery from medical records were 0.87 (95% CI: 0.83–0.90) and 0.88 (95% CI: 0.81–0.93), respectively.
Accuracy of reported side, bilateral HR and date of HR operation
Most women with unilateral HR accurately reported the side of the surgery. Among the 280 women with confirmed HR, 2 out of 250 women reporting a unilateral HR miss-reported the side of surgery for unilateral HR. Among the 30 women with a confirmed HR who reported a bilateral HR, 1 had HR confirmed on only one side while the remaining 8 had a HR confirmed on one side but there was no data for verification of the HR on the other side.
74.5% of women with confirmed HR and who reported date of surgery, accurately reported both the month and year of operation. 79% reported the year accurately.
Discussion
Our analyses found that the overall accuracy of self-report for HR was high in elderly women based on a comparison to medical records and radiographic findings. This confirms results from the Liu et al study on the accuracy of self-report of hip replacement. Approximately one in twenty self-reports of HR could not be confirmed when medical records or radiographs were available. False positive reports of HR were few in number and most were instances where a participant had a confirmed hip fracture with a surgically implanted pin in the fractured hip, suggesting a possible misinterpretation of surgical fracture repair as a HR. Underreporting of HR was minimal in this population, with less than 0.3% of the women not reporting a new HR who had evidence of one on the follow-up radiograph; at least half of these were HR for hip fracture.
To our knowledge, our study is unique in assessing the accuracy self-reported diagnosis of HR. We found that women accurately reported whether HR was for arthritis or a hip fracture, the two most common diagnoses associated with HR. This is noteworthy because the risk factors and determinants of hip osteoarthritis and hip fracture differ substantially [16, 17] and thus the conditions should not be combined in epidemiological studies using HR as an indicator for the presence of hip osteoarthritis or as a clinical outcome of hip osteoarthritis. In our study, more than one quarter of HRs were confirmed as being a treatment of hip fracture, so the potential for misclassification is substantial. Our results indicate that self-reported reason for surgery is adequate for making this distinction with a high degree of accuracy. 95% of confirmed HRs that were self-reported as being for arthritis had a diagnosis of osteoarthritis or degenerative arthritis in the medical record. The remainder had medical records diagnoses of aseptic necrosis and hip fracture, in equal proportions. This very low level of misclassification of reason for surgery should be acceptable in most epidemiological studies of hip osteoarthritis. A small proportion of women were unable to define the reason for their HR as either a fracture or arthritis. In the vast majority of cases, when medical records were available they identified these as HR for osteoarthritis. Thus assigning HR for which the participant is unable to attribute a cause as due to arthritis will result in only a small amount of misclassification.
We found that elder women were more likely to give a false positive report of HR compared to women who accurately reported HR. A few studies have shown that age and education status are related to accuracy of self report of certain common medical conditions [18–20]. We confirmed this result for older age but not for low education levels.
Finally we showed that women with unilateral HR were able to accurately report which hip was replaced. This is important for studies using self-report of HR as a clinical outcome of hip OA. Women reported the month and year of the operation relatively accurately indicating that time to event analysis is possible with self report dates.
This study has several limitations. Participants were volunteers who attended the clinic visit or completed a mailed questionnaire 8.3 years after the baseline visit. Twenty percent of women did not complete the fifth visit or complete a mailed questionnaire and are more likely to have had poor health and more prone to reporting errors. In addition, participants were elderly Caucasian women and hence the results may not be generalizable to other ethnic and gender groups. Some studies have shown that gender and race affect the accuracy of self reporting though the results are not always consistent. It is possible that the accuracy self-report of HR in our study may be higher compared to other populations [21] . We were unable to obtain the data needed to verify a self-report of a new HR in 16% of women who reported one; this could cause us to have underestimated false positive reports of HR in our study. In addition these women were older, less educated and had higher lower limb disability compared to women who had a confirmed HR and hence may be more likely to falsely report a HR. However, it is unlikely that the false positive rate in these women would have been high enough to substantially affect the accuracy rates for HR in our study, and assuming that all these women falsely reported a HR would give a biased estimate of the true rate. Participants only reported the month and year of operation and not the day of operation so we were unable to pinpoint the date of surgery more precisely than +/− one month.
About 4% of participants had help from someone else in completing the questionnaire. Studies suggest that proxy respondents may be less likely to give false-positive reports of medical events [15]. We assessed the accuracy of long term self report of HR in this study. Although HR status was also assessed at year 2 and 6, given that women’s long term recall of HR was highly accurate, it is unlikely that previous report of HR would significantly change the results of our study.
In conclusion, we found that older white women accurately reported hip replacements during the previous 8 years and, importantly also accurately reported whether the reason for the surgery was arthritis or hip fracture. In particular, when women reported a hip replacement for arthritis, 99% were confirmed as a hip replacement from medical records or radiographs and 95% had a confirmed diagnosis of osteoarthritis or degenerative arthritis. Thus, epidemiological and clinical studies in this demographic group can use self-report of a hip replacement for arthritis as a valid indicator of the presence of hip osteoarthritis and as a clinical outcome measure for osteoarthritis of the hip.
Acknowledgments
Investigators in the Study of Osteoporotic Fractures Research Group: San Francisco Coordinating Center (California Pacific Medical Center Research Institute and University of California San Francisco): SR Cummings (principal investigator), MC Nevitt (co-investigator), DC Bauer (co-investigator), DM Black (co-investigator), KL Stone (co-investigator), W Browner (co-investigator), R Benard, T Blackwell, PM Cawthon, L Concepcion, M Dockrell, S Ewing, M Farrell, C Fox, R Fullman, SL Harrison, M Jaime-Chavez, W Liu, L Lui, L Palermo, N Parimi, M Rahorst, D Kriesel, C Schambach, R Scott, J Ziarno. University of Maryland: MC Hochberg (principal investigator), R Nichols (clinic coordinator), S Link. University of Minnesota: KE Ensrud (principal investigator), S Diem (co-investigator), M Homan (co-investigator), P Van Coevering (program coordinator), S Fillhouer (clinic director), N Nelson (clinic coordinator), K Moen (assistant program coordinator), F Imker-Witte, K Jacobson, M Slindee, R Gran, M Forseth, R Andrews, C Bowie, N Muehlbauer, S Luthi, K Atchison. University of Pittsburgh: JA Cauley (principal investigator), LH Kuller (co-principal investigator), JM Zmuda (co-investigator), L Harper (project director), L Buck (clinic coordinator), M Danielson (project administrator), C Bashada, D Cusick, A Flaugh, M Gorecki, M Nasim, C Newman, N Watson. The Kaiser Permanente Center for Health Research, Portland, Oregon: T Hillier (principal investigator), K Vesco (co-investigator), K Pedula (co-investigator), J Van Marter (project director), M Summer (clinic coordinator), A MacFarlane, J Rizzo, K Snider, J Wallace.
The Study of Osteoporotic Fractures (SOF) is supported by National Institutes of Health funding. The National Institute on Aging (NIA) provides support under the following grant numbers: AG05407, AR35582, AG05394, AR35584, AR35583, R01 AG005407, R01 AG027576-22, 2 R01 AG005394-22A1, and 2 R01 AG027574-22A1.
Reference
- 1.Beckles GL, Williamson DF, Brown AF, Gregg EW, Karter AJ, Kim C, et al. Agreement between self-reports and medical records was only fair in a cross-sectional study of performance of annual eye examinations among adults with diabetes in managed care. Med Care. 2007;45:876–883. doi: 10.1097/MLR.0b013e3180ca95fa. [DOI] [PubMed] [Google Scholar]
- 2.Bush TL, Miller SR, Golden AL, Hale WE. Self-report and medical record report agreement of selected medical conditions in the elderly. Am J Public Health. 1989;79:1554–1556. doi: 10.2105/ajph.79.11.1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harlow SD, Linet MS. Agreement between questionnaire data and medical records. The evidence for accuracy of recall. Am J Epidemiol. 1989;129:233–248. doi: 10.1093/oxfordjournals.aje.a115129. [DOI] [PubMed] [Google Scholar]
- 4.Linet MS, Harlow SD, McLaughlin JK, McCaffrey LD. A comparison of interview data and medical records for previous medical conditions and surgery. J Clin Epidemiol. 1989;42:1207–1213. doi: 10.1016/0895-4356(89)90119-4. [DOI] [PubMed] [Google Scholar]
- 5.Gossec L, Tubach F, Baron G, Ravaud P, Logeart I, Dougados M. Predictive factors of total hip replacement due to primary osteoarthritis: a prospective 2 year study of 505 patients. Ann Rheum Dis. 2005;64:1028–1032. doi: 10.1136/ard.2004.029546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Karlson EW, Mandl LA, Aweh GN, Sangha O, Liang MH, Grodstein F. Total hip replacement due to osteoarthritis: the importance of age, obesity, and other modifiable risk factors. Am J Med. 2003;114:93–98. doi: 10.1016/s0002-9343(02)01447-x. [DOI] [PubMed] [Google Scholar]
- 7.Liu B, Balkwill A, Banks E, Cooper C, Green J, Beral V. Relationship of height, weight and body mass index to the risk of hip and knee replacements in middle-aged women. Rheumatology (Oxford) 2007;46:861–867. doi: 10.1093/rheumatology/kel434. [DOI] [PubMed] [Google Scholar]
- 8.Berend KR, Hanna J, Smith TM, Mallory TH, Lombardi AV. Acute hip arthroplasty for the treatment of intertrochanteric fractures in the elderly. J Surg Orthop Adv. 2005;14:185–189. [PubMed] [Google Scholar]
- 9.Waddell JP, Morton J, Schemitsch EH. The role of total hip replacement in intertrochanteric fractures of the femur. Clin Orthop Relat Res. 2004:49–53. doi: 10.1097/01.blo.0000150113.11866.48. [DOI] [PubMed] [Google Scholar]
- 10.Ortiguera CJ, Pulliam IT, Cabanela ME. Total hip arthroplasty for osteonecrosis: matched-pair analysis of 188 hips with long-term follow-up. J Arthroplasty. 1999;14:21–28. doi: 10.1016/s0883-5403(99)90197-3. [DOI] [PubMed] [Google Scholar]
- 11.Liu B, Sweetland S, Beral V, Green J, Balkwill A, Casabonne D. Self-reported information on joint replacement and cholecystectomy agrees well with that in medical records. J Clin Epidemiol. 2007;60:1190–1194. doi: 10.1016/j.jclinepi.2007.02.007. [DOI] [PubMed] [Google Scholar]
- 12.Cummings SR, Black DM, Nevitt MC, Browner WS, Cauley JA, Genant HK, et al. The Study of Osteoporotic Fractures Research Group. Appendicular bone density and age predict hip fracture in women. JAMA. 1990;263:665–668. [PubMed] [Google Scholar]
- 13.Teng EL, Chui HC. The Modified Mini-Mental State (3MS) examination. J Clin Psychiatry. 1987;48:314–318. [PubMed] [Google Scholar]
- 14.Lane NE, Nevitt MC, Hochberg MC, Hung YY, Palermo L. Progression of radiographic hip osteoarthritis over eight years in a community sample of elderly white women. Arthritis Rheum. 2004;50:1477–1486. doi: 10.1002/art.20213. [DOI] [PubMed] [Google Scholar]
- 15.Nevitt MC, Cummings SR, Browner WS, Seeley DG, Cauley JA, Vogt TM, et al. The accuracy of self-report of fractures in elderly women: evidence from a prospective study. Am J Epidemiol. 1992;135:490–499. doi: 10.1093/oxfordjournals.aje.a116315. [DOI] [PubMed] [Google Scholar]
- 16.Arden NK, Lane NE, Parimi N, Javaid KM, Lui LY, Hochberg MC, et al. Defining incident radiographic hip osteoarthritis for epidemiologic studies in women. Arthritis Rheum. 2009;60:1052–1059. doi: 10.1002/art.24382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE, et al. Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med. 1995;332:767–773. doi: 10.1056/NEJM199503233321202. [DOI] [PubMed] [Google Scholar]
- 18.Okura Y, Urban LH, Mahoney DW, Jacobsen SJ, Rodeheffer RJ. Agreement between self-report questionnaires and medical record data was substantial for diabetes, hypertension, myocardial infarction and stroke but not for heart failure. J Clin Epidemiol. 2004;57:1096–1103. doi: 10.1016/j.jclinepi.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 19.Simpson CF, Boyd CM, Carlson MC, Griswold ME, Guralnik JM, Fried LP. Agreement between self-report of disease diagnoses and medical record validation in disabled older women: factors that modify agreement. J Am Geriatr Soc. 2004;52:123–127. doi: 10.1111/j.1532-5415.2004.52021.x. [DOI] [PubMed] [Google Scholar]
- 20.Corser W, Sikorskii A, Olomu A, Stommel M, Proden C, Holmes-Rovner M. "Concordance between comorbidity data from patient self-report interviews and medical record documentation". BMC Health Serv Res. 2008;8:85. doi: 10.1186/1472-6963-8-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cooper-Patrick L, Gallo JJ, Gonzales JJ, Vu HT, Powe NR, Nelson C, et al. Race, gender, and partnership in the patient-physician relationship. JAMA. 1999;282:583–589. doi: 10.1001/jama.282.6.583. [DOI] [PubMed] [Google Scholar]