Abstract
Nearly 100% of patients experience trauma to the trigeminal nerve during orthognathic surgery, impairing sensation and sensory function on the face. In a recent randomized clinical trial, people who performed sensory re-training exercises reported less difficulty related to residual numbness and decreased lip sensitivity than those who performed standard opening exercises only. We hypothesized that re-training reduces the impaired performance on neurosensory tests of tactile function that is commonly observed post-surgically. We analyzed thresholds for contact detection, two-point discrimination, and two-point perception, obtained during the clinical trial before and at 1, 3, and 6 months after surgery, to assess tactile detection and discriminative sensitivities, and subjective interpretation of tactile stimulation, respectively. Post-surgery, the retrained persons exhibited less impairment, on average, than non-retrained persons only in two-point perception (P < 0.025), suggesting that retrained persons experienced or interpreted the tactile stimuli differently than did non-retrained persons.
Keywords: sensory impairment, orthognathic surgery, sensory thresholds, sensory re-training, trigeminal nerve injury
INTRODUCTION
During orthognathic surgery, nearly 100% of patients experience trauma to sensory branches of the trigeminal nerve (Westermark et al., 1998; Essick et al., 2001; Teerijoki-Oksa et al., 2003). With time, sensation and sensory function return in most people, although recovery may not be complete. Non-invasive treatments to expedite the time-course of recovery and its extent are not available. As part of our program to identify new therapies for the rehabilitation of these individuals, we recently conducted a multi-center clinical trial to assess the potential benefit of facial sensory re-training (Phillips et al., in press). Individuals were randomly assigned to sensory-re-training or ‘opening exercise only’ groups, and were assessed before surgery and at 1, 3, and 6 mos after surgery. The primary aim of the clinical trial was to determine whether the magnitude and duration of patient-reported burden from altered sensation are lessened when facial sensory re-training exercises are performed in conjunction with standard opening exercises, compared with when the opening exercises are performed alone. Burden was defined by the person’s reports of objectionable impressions of numb or unusual sensations, including pain, in the facial, peri-oral, and oral regions.
The re-training exercises initially increased, then lessened, the burden associated with the objectionable impression of negative altered sensations. By 6 mos post-surgery, the likelihood of a person reporting fewer problems or less interference with everyday life related to residual numbness or decreased lip sensitivity was significantly higher in the sensory-re-training group, approximately twice that of the ‘opening exercise only’ group. The difference between the two groups at each visit was not statistically significant for unusual sensations, although the trend was for the sensory-re-training group to have a higher likelihood of reporting less of a problem by 6 mos post-surgery. In contrast, the two exercise groups did not differ at any post-surgical time in the perceived problems associated with face or mouth pain, which decreased substantially from 1 to 6 mos post-surgery in both groups.
Based on these finding, we hypothesized that re-training reduces the impaired performance on neurosensory tests of tactile function that is commonly observed post-surgically. We undertook the analyses reported in this paper to evaluate this hypothesis and to investigate the mechanisms underlying the treatment benefit provided by sensory re-training. Using procedures that minimized response bias, we obtained thresholds for contact (touch) detection and two-point discrimination, to assess the individuals’ tactile and spatial discriminative sensitivities, respectively. We also obtained the two-point perception threshold, a response bias-prone measure of spatial sensitivity, to probe the persons’ subjective interpretation of tactile stimulation.
MATERIALS & METHODS
Participants
The data analyzed for this report came from 186 participants enrolled in a multi-center, double-blind, two-arm parallel group, stratified block-randomized controlled clinical trial (Table) (Phillips et al., in press). Sample size determination for the clinical trial was based on variability estimates of the individuals’ responses to questions regarding the burden of orofacial sensory alterations on daily life (Phillips and Bennett, 2000) and is described in Phillips et al. (in press). Consecutive patients were eligible for enrollment if scheduled after December 1, 2002, for bilateral sagittal split osteotomy (BSSO) to correct severe malocclusion and/or developmental disharmony. Half of the participants were randomized to receive instruction on standard opening exercises only after surgery. The other half were given, in addition, a progressive series of sensory re-training exercises during which the individual systematically touched or stroked the face with a cosmetic brush. Inclusion and exclusion criteria, as well as consent procedures, are described in Phillips et al. (in press). The two exercise groups were balanced with respect to number of jaws operated (mandible only vs. mandible and maxilla), and whether the person received a genioplasty, an additional surgical procedure on the chin. Written consent (or assent) was obtained in accordance with the policies of the University of North Carolina Biomedical Institutional Review Board.
Table.
Demographic and Surgical Characteristics for the Entire Sample and for Individuals Randomized to Each of the Exercise Groups*
| All Participants | Sensory Re-training (+ Opening Exercises), N = 92 | Opening Exercises Only, N = 94 | P-value | |
|---|---|---|---|---|
| Age | ||||
| Mean | 25.1 | 24.6 | 25.5 | 0.61 |
| Std | 11.8 | 12.1 | 11.5 | |
| % Female | 71 | 72 | 70 | 0.82 |
| % Caucasian | 94 | 95 | 93 | 0.58 |
| % Mandible only | 61 | 62 | 61 | 0.91 |
| % Genioplasty | 29 | 29 | 29 | 0.93 |
| % Center 1 | 49.5 | 48.9 | 50 | 0.88 |
Exercise Programs and Training
Three time-dependent levels of instruction for the sensory-retraining and opening-only exercise programs were given during training sessions held at 1 wk, 1 mo (4 to 6 wks), and 3 mos after surgery (Phillips et al., in press). The three levels were designed to challenge patients increasingly in a manner similar to that of the early and late phases of sensory education commonly used after injuries to the hand nerves (Dellon et al., 1974; Dellon, 1988; Waylett-Rendall, 1988; Gregg, 1992). Specifically, individuals learned to discriminate moving from non-moving touch, the orientation of moving touch, and the direction of moving touch, in turn. The opening-only exercise program was based on current clinical practice at our Institution.
Assessment of Sensory Impairment
Prior to surgery and at 1, 3, and 6 mos following surgery, participants were appointed for data collection visits. Sensory thresholds were estimated on the right and left sides of the chin, areas supplied by the inferior alveolar nerve.
Contact Detection
The contact detection threshold, the minimum force of contact against the skin that is felt, was measured with the use of nylon monofilaments (“Touch Test Sensory Evaluators”, Stoelting, 620 Wheat Lane, Wooddale, IL 60191, USA). During each trial, a filament was pressed against the skin during one interval, and no stimulus was applied during a second interval. Participants identified the interval (first or second) during which the filament was delivered. A computer program specified the random sequence of the site to be tested, the random sequence of the interval for stimulus application, the monofilament to be used for each of 30 trials for each site, and predicted the threshold force that would be detected in the correct interval on 75% of the trials (Harvey, 1986).
Two-point Discrimination
The two-point discrimination threshold, the minimum separation between 2 points for which a person discriminates 2 points from 1 point of contact, was measured by means of the hand-held Diskcriminator TM (Lafayette Instrument Company, PO Box 5729, 3700 Sagamore Parkway North, Lafayette, IN 47904-5729, USA). This instrument consists of 2 disks of miniature probes of 14 different separations between 2 and 15 mm. Two additional custom-built instruments provided separation of 20 and 25 mm. Testing was identical to that for contact detection, with the following exceptions. Two probes were pressed against the skin during 1 interval, and 1 probe during the other interval. Participants identified the interval (first or second) during which 2 probes were applied. The threshold-tracking algorithm specified the separation between the 2 probes to be used on each trial, and predicted the threshold separation that would be detected in the correct interval on 75% of the trials.
Two-point Perception
The two-point perception threshold is the minimum separation between 2 points of skin contact for which a participant perceives 2 rather than 1 point of contact. Testing proceeded as for two-point discrimination, but with the following exceptions: Fifteen trials instead of 30 were conducted at each test site. Each trial consisted of a single interval during which 2 points were pressed against the skin. Participants were instructed to report whether they felt 2 distinct points of contact. The tracking algorithm estimated the separation that was mathematically predicted to result in a two-point perception on 50% of the trials (Chen et al., 1995; Feldman et al., 1997).
Statistical Analysis
For each threshold measure at each post-surgery visit, we normalized the log-transformed threshold values of the right and left sides of the chin by subtracting the side-matched log-transformed pre-surgery value to obtain a side-specific impairment ratio. The maximum impairment ratio of the right and left sides at each visit for each of the threshold measures was used as the outcome variable.
A repeated-measures analysis of covariance with an unstructured covariance matrix was performed for each threshold measure, according to a general linear mixed model (Proc Mixed; SAS, 2004), where Yijk denotes the value of the threshold measured on participant i in group j at time k, where i = 1 to n; j = re-trained, non-re-trained; and k = 1 mo, 3 mos, 6 mos. The pre-surgery threshold value of the side used in calculation of the maximum impairment ratio served as a covariate. The model also accounted for whether the person received a genioplasty, an additional surgical procedure on the chin, and for whether a Le Fort I procedure (maxillary osteotomy) was performed in addition to the mandibular osteotomy. The level of significance was set at 0.05. The time by exercise group interaction was not statistically significant for any of the threshold measures (P > 0.35), and was removed from the final models. At each post-surgical visit, people in a given group were considered impaired, on average, if the 95% confidence intervals for the mean value did not include ‘0.0’.
RESULTS
Contact Detection
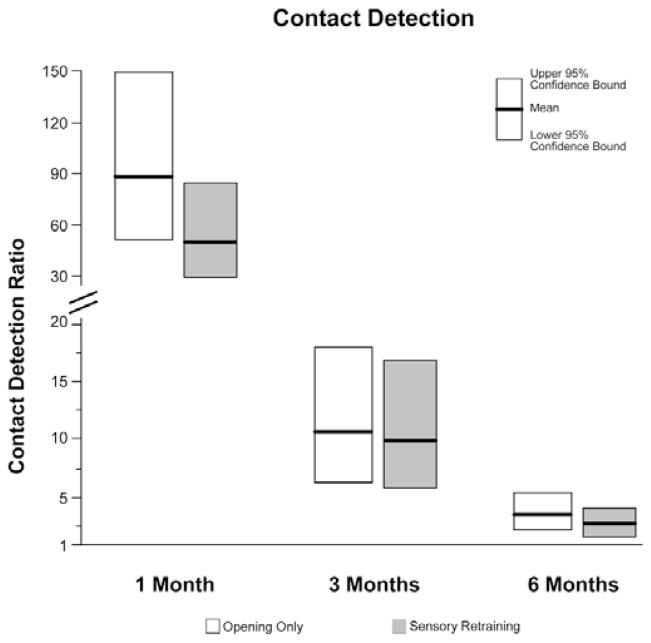
Impairment in contact detection decreased significantly over the six-month post-surgery period (P < 0.0001; Fig. 1), although persons in both groups remained impaired, on average, throughout the period. The average threshold values for persons at 1, 3, and 6 mos post-surgery were elevated 62.7, 10.2, and 3.4 times the pre-surgical values, respectively. The average impairment on the chin was 1.7 times higher in those who received maxillary surgery in addition to the mandibular surgery (P = 0.027), but was unaffected by the addition of a second mandibular procedure, genioplasty (P = 0.61). No significant differences were observed in the impairment of persons in the two exercise groups (P = 0.16).
Figure 1.
Impairment in contact (touch) detection on the chin. Shown are the geometric least-squares means of the impairment ratio with 95% confidence intervals at 1, 3, and 6 mos post-surgery. Sensory thresholds were obtained 1, 3, and 6 mos post-surgery on 89, 89, and 88 people in the sensory re-training group and on 89, 90, and 87 people in the ‘opening only’ group.
Two-point Discrimination
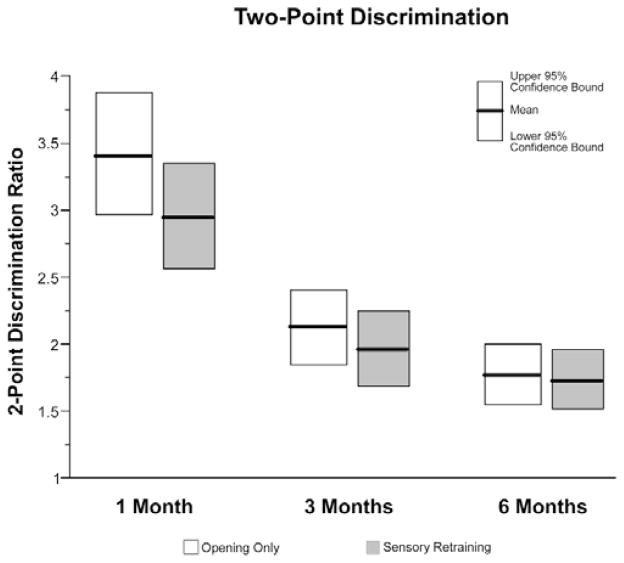
Similar to contact detection, impairment in two-point discrimination decreased over time (P < 0.0001; Fig. 2), but persons in both groups were still impaired at 6 mos, on average. The average threshold values for persons at 1, 3, and 6 mos post-surgery were elevated 3.0, 2.0, and 1.7 times the pre-surgical values, respectively. Average impairment on the chin was 1.31 times higher in those who received maxillary surgery in addition to the mandibular surgery (P < 0.0001), but was unaffected by the addition of a genioplasty procedure (P = 0.91). No significant differences were observed in the impairment of those in the two exercise groups (P = 0.34).
Figure 2.
Impairment in two-point discrimination on the chin. Shown are the geometric least-squares means of the impairment ratio with 95% confidence intervals at 1, 3, and 6 mos post-surgery. Sensory thresholds were obtained 1, 3, and 6 mos post-surgery on 89, 89, and 88 people in the sensory re-training group and on 90, 91, and 86 people in the ‘opening only’ group.
Two-point Perception
The average threshold values for persons at 1, 3, and 6 mos post-surgery were elevated 3.0, 1.8, and 1.4 times the pre-surgical values, respectively (Fig. 3). Elevation on the chin was 1.25 times higher, on average, in those who received maxillary surgery in addition to the mandibular surgery (P = 0.0023), but was unaffected by the addition of a genioplasty procedure (P = 0.90). In contrast to two-point perception and contact detection, a significant difference was observed for the two exercise groups (P = 0.025). The thresholds for those who performed opening exercises only were 1.17 times higher, on average, than those of persons who received facial sensory re-training.
Figure 3.
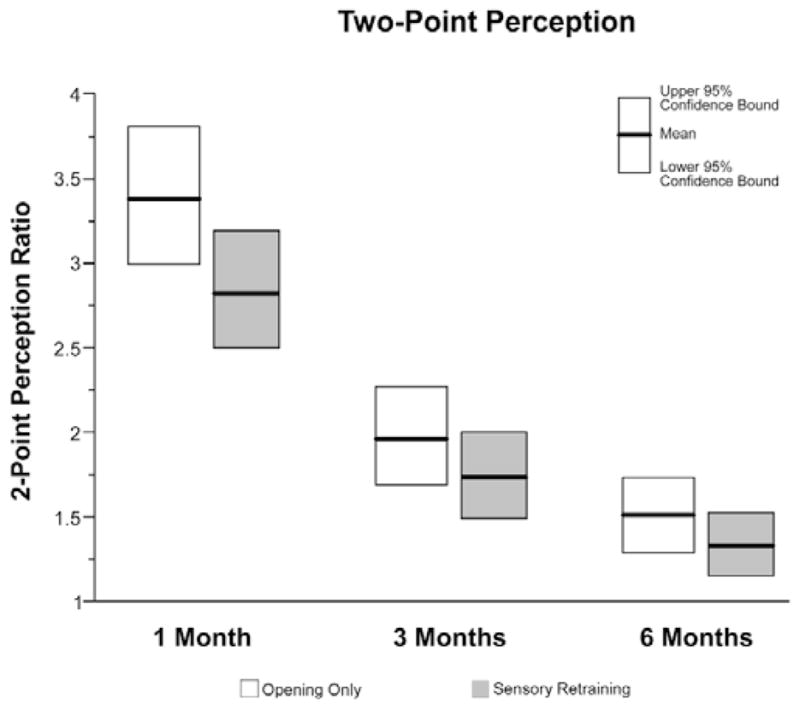
Impairment in two-point perception on the chin. Shown are the geometric least-squares means of the impairment ratio with 95% confidence intervals at 1, 3, and 6 mos post-surgery. Sensory thresholds were obtained 1, 3, and 6 mos post-surgery on 89, 89, and 88 people in the sensory re-training group and on 91, 92, and 86 people in the ‘opening only’ group.
DISCUSSION
Sensory re-training has been used extensively in the rehabilitation of persons with transected hand nerves after surgical repair (Dellon et al., 1974; Dellon, 1984, 1988; Imai et al., 1991; Callahan, 1995). Re-training alters central nervous system organization so that the most functionally useful information can be extracted from the impoverished and disordered nerve signals (Florence et al., 2001; Lundborg, 2003). The aim of such re-training has been to improve patients’ manual dexterity and use of the hand, to increase tactile awareness, and to lessen the objectionable impressions of hypoesthesic (numbness), paresthesic (tingling), and dysesthesic (uncomfortable or painful) sensations. Similar goals have been recommended for facial sensory re-training (Gregg, 1992; Meyer and Rath, 2001), with the caveats that branches of the trigeminal nerve are often crushed or stretched, but are rarely transected, during orthognathic surgery (Fridrich et al., 1995; Westermark et al., 1998), and that the face and palmar hand serve distinctly different functions (Trulsson and Essick, 1997).
Among the tests used to evaluate the effectiveness of sensory re-training of the hand has been two-point discrimination, particularly for point stimuli that are moved laterally across the skin (Dellon, 1988; Imai et al., 1991). However, statistical analyses of the data of the present study did not indicate that sensory re-training improved an individual’s ability to discriminate or to detect tactile stimulation on the face, although the mean levels of impairment of the sensory-retrained participants at each post-surgery visit were less than those of participants who were not re-trained. The lack of a significant difference in the two-point discrimination threshold between the two groups might be attributed to the less severe nature of the patients’ injuries: The topographic mapping between distinct skin sites and their central nervous system targets were less disrupted in these patients than in those with repaired, transecting injuries of the hand nerves, favoring less impairment of two-point discrimination in orthognathic surgery patients (Van Boven and Johnson, 1994a,b). Indeed, the thresholds were elevated less than two-fold by 6 mos post-surgery. The finding that contact detection was unaffected by facial sensory re-training is consistent with the hand literature, and with the assumption that the threshold reflects solely the anatomical connectivity of the peripheral innervation (Dellon, 1988; Bell-Krotoski et al., 1993).
Of particular relevance to the difference in re-trained and non-re-trained patients’ difficulty with numbness and loss of lip sensitivity (Phillips et al., in press) was the finding that retrained participants reported feeling 2 distinct points of skin contact at shorter separations than did non-re-trained participants, even at 1 mo post-surgery. This result indicates that the re-trained individuals experienced or interpreted the sensations evoked by the stimuli differently (Johnson et al., 1994), even though the individuals were no better at discriminating 2 points of contact from 1. One interpretation is that re-trained persons became more critical and introspective in their evaluation of altered sensation, which led to greater acceptance by 6 mos post-surgery. Consistent with this interpretation was the finding that re-trained patients viewed numbness and decreased sensitivity as more problematic early during recovery, but as less problematic later during recovery, than did non-re-trained patients (Phillips et al., in press).
The difference in the mean impairment in two-point perception between the re-trained and non-re-trained patients approximated in magnitude that observed for those who underwent mandibular and maxillary osteotomies vs. mandibular osteotomies only. However, only for the comparison of the two-jaw and ‘mandibular osteotomy only’ patients can the difference be attributed to their individual tactile discriminative abilities: Unlike the re-trained and non-retrained groups of patients, the two-jaw and one-jaw groups differed similarly, on average, in two-point discrimination and two-point perception thresholds. That is, those who underwent two-jaw surgery experienced greater sensory impairment in the lower face than those who underwent mandibular procedures only, based on measures of tactile discrimination as well as of tactile detection. To the authors’ knowledge, this result has not been reported previously. However, the inferior alveolar nerve might have experienced greater injury during the two-jaw surgery: The surgery, and thus hypotensive anesthesia, lasted longer, and the mandible underwent greater manipulation. In addition, the inferior alveolar nerve might have been traumatized during 2 separate stages of the two-jaw surgery. The mandibular osteotomy cuts were often completed before, but the mandibular osteotomy splits were performed after, the maxillary osteotomy. It is also possible that sensory function of the inferior alveolar nerve was impaired indirectly by the injury of the infra-orbital nerve during the two-jaw surgeries. For example, in animal studies, injury to the inferior alveolar nerve has been shown to alter the activity and excitability of the opposing infra-orbital nerve (Tsuboi et al., 2004). Moreover, those who undergo mandibular procedures only sometimes report altered sensations on the upper lip (Essick et al., 2001). Similar effects of injury to the infra-orbital nerve on the inferior alveolar nerve and on sensation on the lower lip are plausible.
Acknowledgments
The authors thank Atousa Safavi, Colleen Ellett Farmer, Harold Jennings, Debora Price, and Akshya Patel for their efforts in participant enrollment and data collection. This project was supported by NIH grant DE01367.
References
- Bell-Krotoski J, Weinstein S, Weinstein C. Testing sensibility, including touch-pressure, two point discrimination, point localization, and vibration. J Hand Ther. 1993;6:114–123. doi: 10.1016/s0894-1130(12)80292-4. [DOI] [PubMed] [Google Scholar]
- Callahan AD. Methods of compensation and re-education for sensory dysfunction. In: Hunter JM, Mackin EJ, Callahan AD, editors. Rehabilitation of the hand. St. Louis, MO: CV Mosby; 1995. pp. 701–714. [Google Scholar]
- Chen CC, Essick GK, Kelly DG, Young MG, Nestor JM, Masse B. Gender-, side- and site-dependent variations in perioral human spatial resolution. Arch Oral Biol. 1995;40:539–548. doi: 10.1016/0003-9969(94)00202-m. [DOI] [PubMed] [Google Scholar]
- Dellon AL. Functional sensation and its reeducation. Clin Plast Surg. 1984;11:95–99. [PubMed] [Google Scholar]
- Dellon AL. Re-education of sensation. In: Dellon AL, editor. Evaluation of sensibility and re-education of sensation in the hand. Baltimore, MD: John D. Lucas; 1988. pp. 203–246. [Google Scholar]
- Dellon AL, Curtis RM, Edgerton MT. Reeducation of sensation in the hand after nerve injury and repair. Plast Reconstr Surg. 1974;53:297–305. doi: 10.1097/00006534-197403000-00008. [DOI] [PubMed] [Google Scholar]
- Essick GK, Austin S, Phillips C, Kiyak A. Short-term sensory impairment following orthognathic surgery. Oral Maxillofac Surg Clin North Am. 2001;13:295–313. [Google Scholar]
- Feldman JA, Essick GK, Zuniga JR, Phillips C. Inter-examiner reliability of three subjective clinical neurosensory tests. Int J Adult Orthod Orthognath Surg. 1997;12:273–285. [Google Scholar]
- Florence SL, Boydston LA, Hackett TA, Lachoff HT, Strata F, Niblock MM. Sensory enrichment after peripheral nerve injury restores cortical, not thalamic, receptive field organization. Eur J Neurosci. 2001;13:1755–1766. doi: 10.1046/j.0953-816x.2001.01555.x. [DOI] [PubMed] [Google Scholar]
- Fridrich KL, Holton TJ, Pansegrau KJ, Buckley MJ. Neurosensory recovery following the mandibular bilateral sagittal split osteotomy. J Oral Maxillofac Surg. 1995;53:1300–1306. doi: 10.1016/0278-2391(95)90588-x. [DOI] [PubMed] [Google Scholar]
- Gregg JM. Nonsurgical management of traumatic trigeminal neuralgias and sensory neuropathies. Oral Maxillofac Surg Clin North Am. 1992;4:375–392. [Google Scholar]
- Harvey LO., Jr Efficient estimation of sensory thresholds. Behav Res Meth Instrum Comput. 1986;18:623–632. [Google Scholar]
- Imai H, Tajima T, Natsumi Y. Successful reeducation of functional sensibility after median nerve repair at the wrist. J Hand Surg [Am] 1991;16:60–65. doi: 10.1016/s0363-5023(10)80014-0. [DOI] [PubMed] [Google Scholar]
- Johnson KO, Van Boven RW, Hsiao SS. The perception of two points is not the spatial resolution threshold. In: Boivie J, Hansson P, Lindblom U, editors. Touch, temperature, and pain in health and disease: mechanisms and sssessments. Seattle, WA: IASP Press; 1994. pp. 389–404. [Google Scholar]
- Lundborg G. Richard P. Bunge memorial lecture. Nerve injury and repair–a challenge to the plastic brain. J Peripher Nerv Syst. 2003;8:209–226. doi: 10.1111/j.1085-9489.2003.03027.x. [DOI] [PubMed] [Google Scholar]
- Meyer RA, Rath EM. Sensory rehabilitation after trigeminal nerve injury or nerve repair. Oral Maxillofac Surg Clin North Am. 2001;13:365–376. [Google Scholar]
- Phillips C, Bennett E. Psychological ramifications of orthognathic surgery. In: Fonseca R, editor. Oral and naxillofacial surgery. Vol. 2. Philadelphia, PA: Saunders; 2000. pp. 506–534. [Google Scholar]
- Phillips C, Essick G, Preisser JS, Turvey TA, Tucker M, Lin D. Sensory retraining following orthognathic surgery: effect on patient perception of altered sensation. J Oral Maxillofac Surg. 2007 doi: 10.1016/j.joms.2006.09.035. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAS Institute Inc. SAS/STAT® 9.1 user’s guide. Cary, NC: The Institute; 2004. [Google Scholar]
- Teerijoki-Oksa T, Jääskeläinen S, Forssell K, Virtanen A, Forssell H. An evaluation of clinical and electrophysiologic tests in nerve injury diagnosis after mandibular sagittal split osteotomy. Int J Oral Maxillofac Surg. 2003;32:15–23. doi: 10.1054/ijom.2002.0325. [DOI] [PubMed] [Google Scholar]
- Trulsson M, Essick GK. Low-threshold mechanoreceptive afferents in the human lingual nerve. J Neurophysiol. 1997;77:737–748. doi: 10.1152/jn.1997.77.2.737. [DOI] [PubMed] [Google Scholar]
- Tsuboi Y, Takeda M, Tanimoto T, Ikeda M, Matsumoto S, Kitagawa J, et al. Alteration of the second branch of the trigeminal nerve activity following inferior alveolar nerve transaction in rats. Pain. 2004;111:323–324. doi: 10.1016/j.pain.2004.07.014. [DOI] [PubMed] [Google Scholar]
- Van Boven RW, Johnson KO. The limit of tactile spatial resolution in humans: grating orientation discrimination at the lip, tongue and finger. Neurology. 1994a;44:2361–2366. doi: 10.1212/wnl.44.12.2361. [DOI] [PubMed] [Google Scholar]
- Van Boven RW, Johnson KO. A psychophysical study of the mechanisms of sensory recovery following nerve injury in humans. Brain. 1994b;117:149–167. doi: 10.1093/brain/117.1.149. [DOI] [PubMed] [Google Scholar]
- Waylett-Rendall J. Sensibility evaluation and rehabilitation. Orthop Clin North Am. 1988;19:43–56. [PubMed] [Google Scholar]
- Westermark A, Bystedt H, von Konow L. Inferior alveolar nerve function after sagittal split osteotomy of the mandible: correlation with degree of intraoperative nerve encounter and other variables in 496 operations. Br J Oral Maxillofac Surg. 1998;36:429–433. doi: 10.1016/s0266-4356(98)90458-2. [DOI] [PubMed] [Google Scholar]