Abstract
Purpose
Following orthognathic surgery, patients use qualitatively different words to describe altered sensation on their face. These words indicate normal, hypoesthetic, paresthetic, or dysesthetic sensations and so reflect the intrusiveness of the altered sensation. The objective of this study was to examine the relationship between the intrusiveness of the altered sensation and the extent to which it and the associated impairment in facial function were perceived to be a problem in the lives of the patients.
Patients and Methods
One hundred forty-six patients who had a mandibular osteotomy with or without a maxillary procedure were included. Word choice data were obtained during patients’ assessment of spontaneous and evoked facial sensations before surgery and at 1 week, 1, 3, and 6 months after surgery and the difficulty or problem levels associated with the altered sensation itself (PAS) and facial functions or oral behaviors in every day life (PAF) were obtained from validated questionnaires. Stratified-by-subject repeated measures Mantel Haenszel correlation statistics were calculated to assess the associations between the intrusiveness of the altered sensation and the problem levels associated with the altered sensation and with the facial functions.
Results
On average, the perception of the difficulty with each of the PAS and PAF items decreased from 1 week to 6 months after surgery (all P values < .0001). Patients reported more difficulty in every day life related to the effect of the altered sensations than they did related to the effect on facial functions. The correlations of the intrusiveness of the altered sensation and problems with altered sensations (PAS) were stronger overall and at each visit than the correlations with problems of altered facial function (PAF). Although the correlation coefficients tended to increase in value from 1 week to 6 months postsurgery for the PAF items, the increase was proportionately greater for the PAS items.
Conclusions
The difficulties in everyday life perceived by patients following orthognathic surgery caused by altered sensations and, to a lesser extent, altered facial function are positively related to the type of altered sensation experienced. The extent of the difficulty follows the intrusiveness level: patients whose sensations are uncomfortable or painful report the most difficulty followed by those who experience nonpainful sensations that are not normally present (ie, positive symptoms), then those who experience only a simple loss in sensation (ie, negative symptoms). Subjective difficulty with altered sensation reflects, in part, its qualitative nature; whereas subjective difficulty with function may reflect the extent of loss in sensory innervation.
Virtually all patients experience some degree of neurosensory impairment after orthognathic surgery. The altered sensation often results in difficulty with everyday oral function, as reflected by drooling, difficulty in detecting food left on the chin, and an inability to accurately assess functionally relevant tactile stimuli on the face (eg, difficulty in shaving).1,2 Those patients who exhibit or report greater sensory alteration also tend to report more difficulty in eating and kissing3,4 and may be less satisfied with their treatment.5–7 In addition to its severity, the total area of the alteration over the face also affects patients’ perceptions. For example, patients who report altered sensation on both the upper lip and lower face report more problems related to their social interactions and the recovery of self-confidence than patients who report alteration on only one jaw or no alteration at all.8
In all previous reports, no clear distinction was made between patients who experienced simply a loss in sensation (negative signs and symptoms) and those who experienced active altered sensations (positive signs and symptoms) that are not normally present on the face, or those whose positive sensations were additionally uncomfortable or painful. Whether the quality of the altered sensation affected the patients’ overall recovery, or the extent to which they viewed the altered sensation or altered function to be a problem in their daily lives, has not been addressed.
In a recent study, a standardized word list was used by patients after bilateral sagittal split osteotomy (BSSO) to describe the altered sensation on their face. Based on their selection of words, sensation was classified as normal or abnormal. Abnormal sensations were ranked in increasing order of the intrusiveness of the sensation as hypoesthetic (diminished sensitivity, ie, negative symptoms such as numbness or dullness considered least intrusive), paresthetic (active sensations such as tingling or pins-and-needles considered as more intrusive than negative symptoms), or dysesthetic (active sensations with implied discomfort or pain considered most intrusive). Six months after surgery, almost two thirds of the patients reported experiencing active sensations during facial expressions or touch, not just a simple loss in sensation.9 Moreover, one third of patients reported that their sensations had actually worsened from those experienced 1 week after surgery. The objective of this study was to examine the relationship between the intrusiveness of the altered sensation reported by these patients and the extent to which the altered sensation and specific functional/oral behaviors were perceived to be a problem in everyday life and activities. The latter was assessed by the subjects’ responses on 2 patient perception questionnaires that were validated previously with a different group of patients undergoing orthognathic surgery.2
Methods
SUBJECTS
Potential subjects were screened at the Oral and Maxillofacial Clinic at the University of North Carolina at Chapel Hill (UNC) or at the University Oral Maxillofacial Surgery in Charlotte, NC, a community-based practice. A limited waiver of HIPAA (Health Insurance Portability and Accountability Act) authorization was requested and received from the Institutional Review Board. Consecutive patients with surgery dates after December 1, 2002, were eligible to be enrolled if they were scheduled for a bilateral sagittal split osteotomy to correct a severe malocclusion and/or a developmental disharmony. Inclusion and exclusion criteria are given in Table 1. Before a subject was enrolled, written consent (and assent if the subject was younger than 18 years) was obtained in accordance with the policies of the UNC School of Dentistry’s Institutional Review Board. Each subject enrolled and consented after April 14, 2003, signed an HIPAA consent form as well. Surgeries were performed by 5 attendings. Resident surgeons were present during all operations.
Table 1.
INCLUSION AND EXCLUSION CRITERIA FOR ENROLLMENT IN THE SENSORY RETRAINING CLINICAL TRIAL
| Inclusion criteria |
| Have a developmental dentofacial disharmony |
| Be 13 to 50 years of age |
| Be scheduled to receive a bilateral sagittal split either by mandibular surgery only or combined mandibular/maxillary surgery |
| Exclusion criteria |
| Have a congenital anomaly or acute trauma |
| Have had previous facial surgery |
| Are pregnant at baseline |
| Do not have the ability to follow written English instructions |
| Are unwilling to sign informed consent |
| Report a moderate level of discomfort or problem caused by altered sensation of numbness or unusual feeling on the face at baseline |
| Report no altered sensation at one week postsurgery |
| Have a medical condition associated with systemic neuropathy (diabetes, hypertension, kidney problems) |
All participants were enrolled in a multicenter, double blind, 2-arm parallel group, stratified block randomized controlled clinical trial (Table 2). The clinical trial was designed to evaluate sensory retraining, a rehabilitative therapy that offers significant potential for patients who experience impaired sensory function. Half of the subjects were randomized to receive instruction on standard opening exercises only after surgery, whereas the other half were also given a progressive series of sensory retraining exercises during which the patient systematically touched or stroked the face with a cosmetic brush. The altered sensation commonly following orthognathic surgery served as the experimental model. This report provides an exploratory analysis of the perception of the problem level or difficulty in everyday life or activities associated with altered sensation and associated altered facial function, and the relationship of these perceptions to the words chosen by the patients to describe the altered sensation.
Table 2.
DEMOGRAPHIC CHARACTERISTICS OF SUBJECTS ENROLLED IN THE SENSORY RETRAINING CLINICAL TRIAL FOR WHOM 6-MONTH DATA WERE AVAILABLE ON FEBRUARY 1, 2005
| Surgery Performed | n | Age |
% Female | % Caucasian | |
|---|---|---|---|---|---|
| Mean | SD | ||||
| Mandibular only + Genioplasty | 65 | 25.3 | 12.92 | 78.5 | 95.4 |
| 20 | 21.6 | 11.50 | 70.0 | 95.0 | |
| Mandibular and maxillary + Genioplasty | 38 | 25.1 | 9.56 | 60.5 | 89.5 |
| 23 | 28.5 | 12.42 | 82.6 | 100.0 | |
| 146 | 25.2 | 11.89 | 73.3 | 94.5 | |
PROCEDURES
Prior to surgery and at 1 week, 1 month, 3 months and 6 months after surgery, subjects were questioned about altered sensation at 4 extraoral locations: the hairy upper lip, upper vermillion, lower vermillion, and chin. Initially, the patient was instructed to keep the face at rest and not make any facial expression. Using a mirror to aid location of each site, the patient was asked whether any altered sensation was being experienced at that site (spontaneous alteration). If no altered sensation was reported, the site was categorized as normal. If altered sensation was present, the patient was then asked to choose at least 1 word from a standardized list to describe the altered sensation.1,9 More than 1 word could be selected for each site. The entire procedure was then repeated, but the patient was asked to make facial expressions and to touch or rub each test site with a finger before responding (evoked alteration). Patients who reported no altered sensation during either the spontaneous or the evoked assessment were categorized as having no altered sensation (normal sensation).
After consultation with 7 oral and maxillofacial surgeons, the words on the list were categorized as consistent with hypoesthetic, paresthetic, and dysesthetic sensations (Table 3).9 The categories were ordered and scored according to the level of the intrusiveness of the altered sensation (IAS): no alteration (value = 0) < hypoesthetic (value = 1) < paresthetic (value = 2) < dysesthetic (value = 3). Positive symptoms (paresthetic) were viewed as more intrusive than negative ones (hypoesthetic); and unpleasant or painful positive symptoms (dysesthetic) were viewed as more intrusive than nonpainful positive ones. The most intrusive category from which word(s) had been chosen during the spontaneous or the evoked assessments to describe any of the 4 sites was considered the maximum intrusiveness of altered sensation, IAS-max, over the subject’s face. The frequency of words chosen for each of the 4 facial sites has been reported previously.9
Table 3.
LIST OF WORDS GIVEN TO PATIENTS FOR SELECTION TO DESCRIBE ALTERED SENSATIONS, PRESENTED BY INTRUSIVENESS CATEGORY*
| No alteration |
| No words selected |
| Hypoesthetic |
| Numb |
| Warm |
| Wet |
| Rubbery |
| Wooden |
| Cool |
| Swollen |
| Stretched |
| Paresthetic |
| Tickling |
| Tingling |
| Twitching |
| Pulling |
| Crawling |
| Vibrating |
| Drawing |
| Itching |
| Dysesthetic |
| Prickling |
| Stinging |
| Electric |
| Painful |
| Cold |
| Hot |
| Tender |
| Excruciating |
| Sore |
| Burning |
| Shocking |
During each appointment, participants also completed 2 validated patient perception questionnaires: Postsurgical Perceptions and Problems with Facial Sensation.2 Responses to the items on Postsurgical Perceptions reflected the level of interference of post-surgery sensory alteration on the patient’s daily routine, health, and quality of life. Responses to the items on the Problems with Facial Sensation reflected the level of interference on different aspects of orofacial sensation and function. The individual items on both inventories were rated from “no problem” (1) to “serious problem” (7). For both questionnaires, subjects were instructed to report the magnitude of the problem during the past 2 weeks (during the past week for the 1-week postsurgery visit).
For this study, 2 sets of items were selected from the patient perception questionnaires (Table 4) to focus on the perception of the problem related to the altered sensation itself (Problems with Altered Facial Sensation, PAS) and on the perception of the problem related to facial function (Problems with Altered Facial Function, PAF) that could be linked to the intrusiveness of the altered sensation. In addition to analyses of the scores for the individual items, 2 summary measures were calculated for each visit: PASave and PAFave, the average of the scores for the 2 sets of items, respectively.
Table 4.
FORMAT OF THE PATIENT PERCEPTION QUESTIONNAIRES REGARDING SYMPTOMS AND PROBLEMS WITH FACIAL SENSATION AND FUNCTION
| Instructions: Doctors need to know when patients have problems after orthognathic surgery. Listed below are problems that some patients have mentioned as being a concern after orthognathic surgery. Choose the response that best describes how much of a problem in each area or function you have experienced in the past 2 weeks. Each item is rated from No Problem (1) to Serious Problem (7). |
| Problems with Altered Sensation (PAS) The 4 items from the 2 questionnaires that contributed to PAS included the following:
|
| Problems with Altered Function (PAF) The 4 items from the 2 questionnaires that contributed to PAF included the following:
|
STATISTICAL ANALYSIS
The purpose of the statistical analysis was 2-fold: 1) to assess the recovery pattern for the problem levels in everyday life and activities perceived to be associated with the altered sensation and oral function/behaviors. The recovery pattern for the problem levels associated with altered sensation (PAS) and facial function (PAF) was assessed by a stratified-by-subject repeated-measures Mantel-Haenszel correlation statistic between time and problem level separately for each item and summary measure. The recovery pattern for the word choice categories has been previously reported9 and 2) to assess the association between the intrusiveness of the altered sensation and the problem level experienced. For each of the 8 PAS and PAF items and each summary measure (PASave and PAFave), the null hypothesis was that there would be no association between the problem level reported (scored 1 to 7) and the intrusiveness of the word(s) chosen to describe the qualitative nature of the altered sensation (IASmax; scored 0 to 3). Because both IASmax and the questionnaire item responses were ordinally based, stratified-by-subject repeated measures Mantel-Haenszel correlation statistics were calculated to assess the associations between the intrusiveness of the altered sensation based on word choice and the reported problem levels associated with the altered sensation and facial functions.10 The null hypothesis for each PAS and PAF item score and summary measure, PASave and PAFave, was that the distribution of the scores, averaged over time, was interchangeable for all word categories, ie, levels of IASmax. A sensitivity analysis performed using modified ridits and different sets of scores (0,1,3,5) and (0,1,2,4) for the word categories indicated that the score assignment did not substantially change the conclusions. Because the stratified-by-subject analysis does not directly adjust for time changes in the choice of word categories or in the questionnaire item responses, confirmatory Spearman correlation coefficients were calculated to assess the association between word category intrusiveness and questionnaire item response separately at each of the 4 postsurgery visits. Level of significance was set at 0.05.
Results
The majority of the 146 participants was Caucasian and female (Table 2). All 146 patients underwent bilateral sagittal split surgery in close proximity to the inferior alveolar sensory nerves associated with the mandibular division of the trigeminal nerve, and 46 (32%) also had a genioplasty. Sixty-one (42%) underwent Le Fort surgery in close proximity to the infraorbital sensory nerves associated with the maxillary division of the trigeminal nerve as well.
Recovery of Sensation After Surgery
Prior to surgery, 96% of the patients reported no altered sensation at any of the 4 sites on the face during the spontaneous or evoked assessments of sensation. One week after surgery, all patients reported alteration of sensation; at 6 months after surgery, 15% reported no alteration in sensation at tested sites (Table 5). In contrast, at 1 week after surgery, 42% of the patients reported active sensations that were not painful (paresthetic), and an additional 51% selected words (“tender,” “sore,” “prickling,” or “burning”) indicating active sensations that were uncomfortable or painful (dysesthetic sensations). At 6 months, active sensations that were uncomfortable or painful were reported by fewer patients (23%) (Table 5).
Table 5.
PERCENTAGE OF PATIENTS CLASSIFIED ACCORDING TO THE MOST INTRUSIVE CATEGORY OF WORD(S) CHOSEN TO DESCRIBE ALTERED SENSATION ON THE FACE DURING THE SPONTANEOUS OR EVOKED ASSESSMENTS OF SENSATION
| Intrusiveness of Altered Sensation (IAS) | 1 Week % | 1 Month % | 3 Months % | 6 Months % |
|---|---|---|---|---|
| No alteration | 0 | 1 | 4 | 15 |
| Hypoesthetic | 7 | 11 | 16 | 19 |
| Paresthetic | 42 | 37 | 40 | 43 |
| Dysesthetic | 51 | 51 | 40 | 23 |
Reported Difficulty With Altered Sensations and Facial Functions
The percentages of patients who reported no trouble (1 of 7), a little to somewhat (2–4 of 7), and moderate to severe (5–7 of 7) trouble with each of the PAS and PAF items are given in Table 6. Also shown are the percentage of patients whose PASave and PAFave scores were in those categories. The perception of the difficulty with each of the PAS and PAF items and their average values decreased from 1 week to 6 months after surgery (P < .0001 for all PAS and PAF items and PASave and PAFave). Overall, the highest level of difficulty in everyday life was associated with numbness and the lowest level of difficulty with facial pain. The percentage of patients who reported moderate (5) to severe (7) difficulty ranged from 14% for problems with facial pain to 72% for problems with numbness at 1 week after surgery and from 2% to 12%, respectively, at 6 months after surgery.
Table 6.
PERCENTAGES OF PATIENTS WHO REPORTED NO DIFFICULTY (1),1 LITTLE TO SOMEWHAT (2–4),2 OR MODERATE TO SEVERE (5–7)3 DIFFICULTY OR PROBLEM EXPERIENCED IN THE PAST 2 WEEKS WITH ALTERED SENSATIONS (PAS ITEMS) OR WITH THE CONSEQUENCES OF ALTERED SENSATION ON FUNCTION (PAF ITEMS)
| 1 Week |
1 Month |
3 Months |
6 Months |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No1 | L/S2 | M/S3 | No | L/S | M/S | No | L/S | M/S | No | L/S | M/S | |
| PAS item | ||||||||||||
| Numbness | 2 | 26 | 72 | 5 | 44 | 51 | 17 | 64 | 19 | 27 | 61 | 12 |
| Unusual feelings | 9 | 49 | 42 | 20 | 56 | 24 | 35 | 55 | 10 | 53 | 43 | 4 |
| Less lip sensitivity | 14 | 43 | 43 | 23 | 47 | 30 | 38 | 45 | 17 | 45 | 47 | 8 |
| Facial pain | 19 | 67 | 14 | 52 | 41 | 7 | 73 | 24 | 3 | 80 | 18 | 2 |
| PASave | 1 | 48 | 51 | 5 | 66 | 29 | 22 | 66 | 12 | 33 | 62 | 5 |
| PAF item | ||||||||||||
| Drooling | 21 | 43 | 36 | 27 | 52 | 21 | 45 | 49 | 6 | 58 | 38 | 4 |
| Food particles | 4 | 54 | 42 | 11 | 58 | 31 | 34 | 54 | 12 | 46 | 52 | 2 |
| Not feeling smile | 26 | 49 | 25 | 44 | 45 | 11 | 71 | 27 | 2 | 81 | 18 | 1 |
| Speaking problems | 8 | 44 | 48 | 34 | 51 | 15 | 68 | 31 | 1 | 79 | 20 | 1 |
| PAFave | 2 | 55 | 43 | 12 | 70 | 18 | 35 | 61 | 4 | 49 | 51 | 0 |
PAFave PASave and were categorized as no difficulty (No) <1.5, little to somewhat (L/S) 1.5 to 4.25, moderate to severe (M/S) >4.25.
In general, patients reported less difficulty associated with facial function than they did with altered sensations. The percentage of patients who reported moderate (5) to severe (7) difficulty ranged from 25% for problems with facial expression (smiling) to 48% for problems with speaking at 1 week after surgery. By 6 months, however, less than 5% of the subjects reported moderate to severe difficulty related to facial function.
Although less than 12% of patients experienced moderate to severe difficulty at 6 months for any symptom or function related to altered sensation, most subjects had not fully recovered and the quality of their life was still affected. For example, subjects continued to report some problem related to altered sensation (20% for facial pain to 73% for numbness) and to altered facial function (19% for the sensation of facial expression/smiling to 54% for food particles).
Effect of the Intrusiveness of Altered Sensation on the Reported Difficulty With Altered Sensations
The Mantel-Haenszel correlation analyses, stratified by subject, indicated that the maximum intrusiveness of the words chosen to describe altered sensation was associated with subjects’ perception of the difficulty with the PAS items and the average score (P < .001). The relationship between PAS scores and the rankings of the maximum intrusiveness of the words chosen was confirmed by time-specific analyses (see Methods). In general, the associations strengthened over time with the strongest correlations observed at 6 months (Table 7): the intrusiveness of the sensory alteration explained 25% of the variability in the PASave score at 6 months.
Table 7.
SPEARMAN CORRELATION COEFFICIENTS CALCULATED AT EACH APPOINTMENT TIME BETWEEN EACH OF THE PROBLEMS-WITH-ALTERED SENSATION (PAS) AND PROBLEMS WITH ALTERED FUNCTION (PAF) ITEMS AND THE PATIENT RANKINGS BASED ON THE MAXIMUM INTRUSIVENESS OF THE WORDS CHOSEN TO DESCRIBE THEIR ALTERED FACIAL SENSATION
| Intrusiveness of Altered Sensation (IAS) | ||||
|---|---|---|---|---|
| PAS item/time | 1 Week | 1 Month | 3 Months | 6 Months |
| Numbness | 0.01 | 0.27 | 0.29 | 0.43 |
| Unusual feelings | 0.24 | 0.25 | 0.44 | 0.45 |
| Less lip sensitivity | 0.28 | 0.32 | 0.37 | 0.42 |
| Facial pain | 0.31 | 0.18 | 0.34 | 0.27 |
| PASave | 0.25 | 0.34 | 0.42 | 0.51 |
| PAF item | ||||
| Drooling | −0.04 | 0.04 | 0.11 | 0.10 |
| Food particles | 0.12 | 0.21 | 0.27 | 0.27 |
| Not feeling smile | 0.06 | 0.15 | 0.27 | 0.17 |
| Speaking problems | 0.16 | 0.10 | 0.23 | 0.19 |
| PAFave | 0.11 | 0.17 | 0.29 | 0.23 |
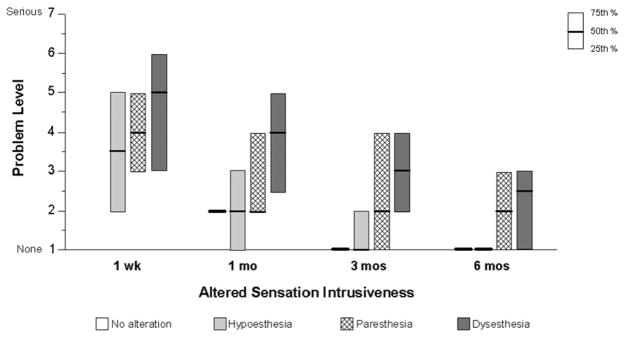
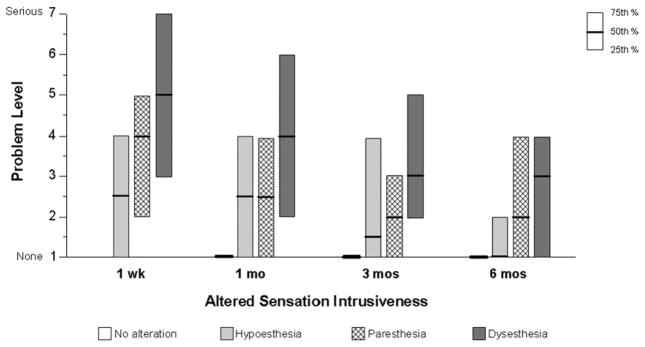
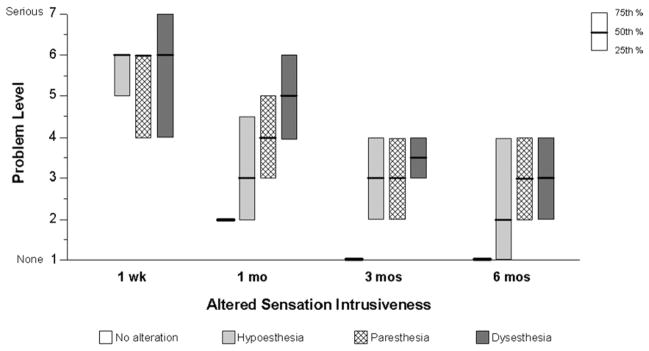
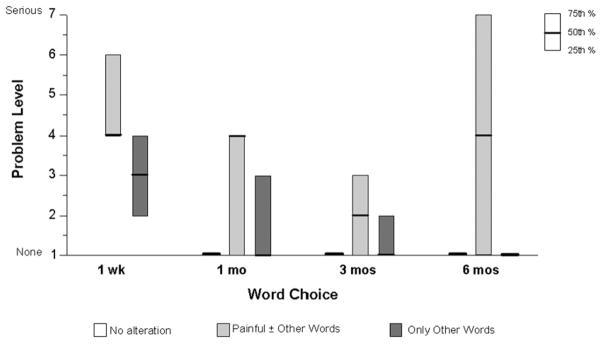
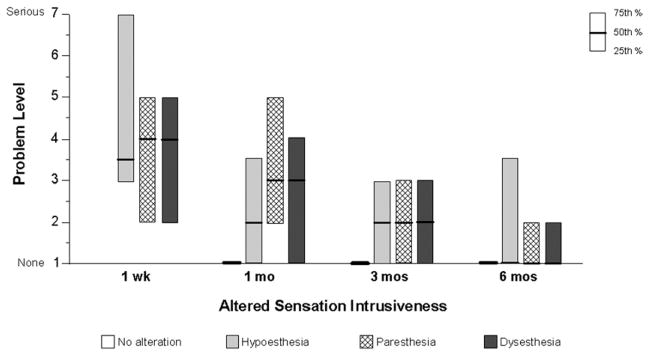
The relationship is displayed in Figure 1 for the PAS item “Unusual Feelings,” as qualitatively different altered sensations are nevertheless all unusual sensations. Patients who experienced dysesthetic sensations reported the greatest problems with unusual sensations, followed by patients who experienced, at worst, paresthesia, hypoesthesia, and no alteration in sensation, in turn. This trend was observed at all times after surgery. A very similar trend is observed for the PAS item “Less Lip Sensitivity” (Fig 2). In general, patients selecting at least 1 dysesthesia word for at least 1 site on the face reported higher levels of difficulty related to the alteration even when the PAS item explicitly referred to aspects of sensation unrelated to pain or discomfort, such as an unusual sensation (Fig 1), less sensitivity in the lips (Fig 2), and even numbness (Fig 3).
FIGURE 1.
The extent of difficulty or problem level associated with unusual feelings in the face or mouth reported by subjects in each of the intrusiveness categories from 1 week to 6 months.
FIGURE 2.
The extent of difficulty or problem level associated with less sensitivity to touch in the lips reported by subjects in each of the intrusiveness categories from 1 week to 6 months.
FIGURE 3.
The extent of difficulty or problem level associated with “numbness” reported by subjects in each of the intrusiveness categories from 1 week to 6 months.
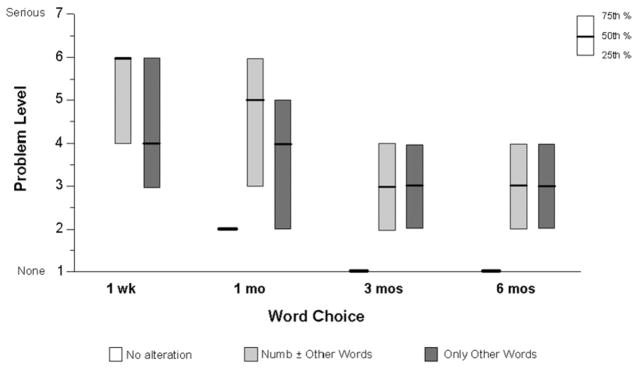
Patients who selected the word “numb” with or without other words reported a higher level of difficulty associated with numbness at the early postsurgical visits than did patients who did not select “numb.” However, at 6 months the distributions of the perception of the difficulty associated with numbness were identical (Fig 4). It is plausible that patients who did not specifically choose “numb” interpreted numbness more generally to include other aspects of hypoesthesia and paresthesia as well. In contrast, at every appointment, patients who selected the word “painful” with or without other words, reported substantially greater difficulty in everyday life related to facial pain than did patients who selected other words or no alteration to describe their facial sensation (Fig 5). Pain in the facial area caused a mild or moderate level of problems for most patients who indicated “painful” to describe their altered sensation; whereas patients who did not choose “painful” reported only negligible levels of difficulty with facial pain. An exception is observed at 1 week after surgery when mild to moderate difficulty with pain was common to all patients who reported altered sensation regardless of the quality of the alteration.
FIGURE 4.
The extent of difficulty or problem level from 1 week to 6 months associated with “numbness” reported by subjects who chose “numb” to describe the quality of their altered sensation, those who chose words other than “numb,” and those who reported no alteration.
FIGURE 5.
The extent of difficulty or problem level from 1 week to 6 months associated with “facial pain” reported by subjects who chose “painful” to describe the quality of their altered sensation, those who chose words other than “painful,” and those who reported no alteration.
Effect of the Intrusiveness of Altered Sensation on the Reported Difficulty With Altered Facial Function
The associations between the intrusiveness of altered sensation and the perception of the difficulty related to facial function were also statistically significant when the Mantel-Haenszel correlation analyses were performed stratified by subject (P < .001 for all individual PAF items and PAFave). The strength of the associations between the intrusiveness of the word choice and the PAF items was substantially less in general than with the PAS items, and the Spearman correlation values increased only slightly over time (Table 7). At 6 months, the word choice quality accounted for, at most, only 5% of the variability of the average altered function measure. An example of the average difficulty for altered function, drooling, is displayed in Figure 6. Note that about the same difficulty level was associated with drooling regardless of the intrusiveness level of the altered sensations reported by 3 months.
FIGURE 6.
The extent of difficulty or problem level associated with “drooling” reported by subjects in each of the intrusiveness categories from 1 week to 6 months.
Discussion
Although there is dissenting opinion,11,12 the literature suggests that the degree of return of normal sensation after orthognathic surgery is a critical determinant of patient satisfaction with treatment.5–7 Additionally, preliminary analysis of psychosocial data from our work has shown associations between impairment and satisfaction.8 For example, generalized neurosensory impairment, as defined by patients’ reports of abnormal spontaneous and evoked sensations, was found to negatively affect patients’ perception of recovery from unwanted symptoms and recovery of social and self-confidence. Moreover, patients who experienced altered sensations on both upper lip and lower face reported that their function, intraoral sensation, symptom recovery, and interactions socially were more of a problem than those who experienced altered sensation in only one area of the face or not at all.
Patients with altered sensation are faced not only with unfamiliar sensory experiences on their lips, chin, and mouth, but also with the strong possibility of bothersome problems with facial function,1,2 particularly those patients with more severe sensory impairments. Problems with function that are frequently cited include 1) drooling, 2) undetected food particles remaining on the lip and chin, 3) errors in speech articulation, particularly with fatigue, 4) dysesthesias or pain upon touching the gingiva, often resulting in poor oral hygiene habits, 5) cheek biting, and 6) pain upon exposure to cold food and drink.1,2,13 Difficulty with eating and kissing are also reported, although the relative contributions of motor, sensory, and psychological dysfunction in these situations remain unclear.3,4,14 Lemke et al4 reported that about 3 times as many patients with hypoesthesia, compared to those without, experienced serious problems with 1 or more of 9 aspects of oral function 6 months after surgery, chewing, and kissing cited most often.
The current study was motivated by the findings above and evidence that suggests that 1) patients vary in the characterizations they provide of the altered sensation on their face and mouth,9,15–17 2) patients who report greater discomfort with altered sensation tend to report positive symptoms such as paresthesias and pain,13 and 3) these latter patients are more likely to exhibit problems with aspects of facial function. Using questionnaire methods, Sandstedt and Sorensen13 obtained information from 226 patients who had received compensation because of damage to the trigeminal nerve at least 3 years earlier, most often from third molar extraction. Patients who reported slight discomfort via a visual analog scale were more likely to indicate “impaired sensitivity in the affected area” (interpreted as hypoesthesia); whereas patients who reported moderate or severe discomfort were more likely to indicate “complete loss of sensation” (interpreted as anesthesia). Patients who reported more severe discomfort were also more likely to indicate “itching, tingling, and a prickly sensation” (interpreted as paresthesia) and pain, and to indicate problems associated with eating (including drooling and increased need for use of handkerchief), interpersonal relationships (including kissing), and self-confidence.
The current study differs from that of Sandstedt and Sorensen13 in that the patients’ sensory dysfunctions in the current study all resulted from elective orthognathic surgery, which overall led to a positive clinical outcome. A few previous studies have asked patients after orthognathic surgery to describe their altered sensation by selecting from a list of words containing fewer words than in the present study.13,15,16 However, no previous study with orthognathic surgery patients has both used a word list recommended for the subjective assessment of altered sensations after orofacial nerve injury1 and tracked the characterization longitudinally. As shown in this article, the latter allows one to assess the time-dependent changes in the relationship between the qualitative nature of the altered sensation and problems related to the altered sensation and with oral function.
Eighty-five percent of the patients in this study reported a residual alteration in sensation at 6 months after surgery (Table 5). This is slightly higher than the 73% reported by Cunningham et al,16 but in their study patients who reported a burning, electric, or other “dysesthetic” facial sensation were not categorized as having a neurosensory deficit for the purpose of the analyses. As would be expected, the percentage of patients who reported moderate to severe difficulty or problems related to altered sensations after orthognathic surgery dropped dramatically from 1 week to 6 months postsurgery. Most patients did report mild problems or difficulty. Seventy-three percent of our patients reported at least mild difficulty in their everyday life related to numbness, 55% difficulty caused by the lips being less sensitive, 47% difficulty related to unusual sensations, and 20% problems related to facial pain (Table 6).
The correlations between the quality of altered sensation and the difficulty the alteration posed increased from 1 week to 6 months even though the intrusiveness of the words chosen and the difficulty levels reported both decreased, on average. It is plausible that patients, particularly those who are still experiencing positive sensations, have a heightened awareness of the residual alteration when the effects of confounding factors such as edema, bruising, and inflammation have subsided. The highest correlations between the quality of the altered sensation and the difficulty it posed were observed for the PAS item “problems with unusual feelings,” confirming that dysesthetic sensations are more problematic than other altered sensations, but also that paresthesias are perceived to be more problematic than losses in sensation or numbness. Sixty-six percent of patients used words that described positive symptoms, ie, paresthesic or dysesthesic sensations, at 6 months (Table 5). Patients who report dysesthetic sensations may have experienced greater sensory deficits than those who did not. However, we recently showed that subjects with trigeminal nerve injury with and without neuropathic pain perform similarly on many sensory tests of tactile and thermal sensibility.18
It is likely that most, if not all, patients who experience dysesthetic and paresthesic sensations also experience numbness and that the combination of both positive and negative symptoms contributed to the relatively high percentage of patients who reported a problem caused by 3 of the 4 PAS items in the present study. Patients selected very specific words to describe their altered sensation (eg, tingling and prickling); but it is possible that when asked about the difficulty caused by numbness, patients viewed “numbness” in a more general context. Even in the dental office, numbness is often equated with a tingling or prickling sensation. In contrast, “painful” has a more limited and uniformly understood meaning, which would explain why difficulty with facial pain was limited to those patients who selected that specific word.
Both the average degree of difficulty and the percentages of patients reporting at least a mild problem were lower at 6 months for the altered function (PAF) items: 54% reported some difficulty with food particles remaining on their face, 42% with drooling, and about 20% reported some difficulty feeling their face during smiling and with speaking (Table 6). These percentages appear higher than those reported by Lemke et al.4 However, in their study, the responses “no problem” and “mild problem” were not differentiated, thereby lowering the estimates. The reported difficulty with the oral function items (PAF) was correlated less strongly with the intrusiveness of the patients’ altered sensation, and the correlations were relatively stable over the 6-month period after surgery. Although the basis for the distinction merits further investigation, it is plausible that the functions evaluated were more dependent on the integrity of the sensory innervation rather than the qualitative nature of the altered sensation produced. This was certainly suggested by the problems with drooling data depicted in Figure 6. Patients were equally likely to report difficulty with drooling regardless of the qualitative nature of the altered sensation.
In all the analyses reported in this article, no account was taken of the type or number of surgical procedures that the patient underwent. Emphasis was focused on determining whether general relationships, across all patient subgroups, could be identified between the problem levels that were reported and the intrusiveness of the patients’ altered sensation. It is possible that the strength of the relationships is different for patients who underwent both maxillary and mandibular surgery, compared with mandibular surgery only, and for patients who received a genioplasty procedure compared with those who did not. For example, patients who experienced altered sensations on both the upper lip and lower face reported greater difficulty with altered sensation and function than those who experienced altered sensation on the lower face only.8 However, it was observed that the maximum intrusiveness category for most patients was determined by words selected for altered sensation on the lower lip or chin.9 As such, for patients who underwent 2-jaw surgery, altered sensation on the upper lip likely contributed to the measured level of difficulty, but did not contribute substantially to the assigned level of intrusiveness. Similarly, it is plausible that patients who underwent a genioplasty procedure might have had more difficulty with altered sensation and function than patients who did not. However, the distributions of intrusiveness scores were found to be very similar by 6 months for patients who did and did not have a genioplasty procedure.9 Subsequent analyses of larger samples of patients from the clinical trial are planned to explore these issues and to determine whether different relationships between the intrusiveness of altered sensation and the difficulty it poses are observed for patients who undergo different types of surgery.
Acknowledgments
Funded in part by NIH grant DE01367.
The authors wish to thank Atousa Safavi, Colleen Ellett Farmer, Harold Jennings, Debora Price, and Akshya Patel for their efforts in patient enrollment and data collection.
References
- 1.Zuniga JR, Essick GK. A contemporary approach to the clinical evaluation of trigeminal nerve injuries. Oral Maxillofac Surg Clin North Am. 1992;4:353. [Google Scholar]
- 2.Phillips C, Bennett ME. Psychological ramifications of orthognathic surgery. In: Fonseca R, editor. Oral & Maxillofacial Surgery. Vol. 1. Philadelphia, PA: W.B. Saunders; 2000. pp. 506–534. [Google Scholar]
- 3.Bothur S, Blomqvist JE. Patient perception of neurosensory deficit after sagittal split osteotomy in the mandible. Plast Reconstr Surg. 2003;111:373. doi: 10.1097/01.PRS.0000036049.37768.37. [DOI] [PubMed] [Google Scholar]
- 4.Lemke RR, Clark GM, Bays RA, et al. Effects of hypesthesia on oral behaviors of the orthognathic surgery patient. J Oral Maxillofac Surg. 1998;56:153. doi: 10.1016/s0278-2391(98)90856-4. [DOI] [PubMed] [Google Scholar]
- 5.Forssell H, Finne K, Forssell K, et al. Expectations and perceptions regarding treatment: A prospective study of patients undergoing orthognathic surgery. Int J Adult Orthodon Orthognath Surg. 1998;13:107. [PubMed] [Google Scholar]
- 6.Westermark A, Bystedt H, von Konow L. Patients’ evaluation of the final result of sagittal split osteotomy: Is it influenced by impaired sensitivity of the lower lip and chin? Int J Adult Orthodon Orthognath Surg. 1999;14:135. [PubMed] [Google Scholar]
- 7.Chen B, Zhang Z, Wang X. Factors influencing postoperative satisfaction of orthognathic surgery patients. Int J Adult Orthodon Orthognath Surg. 2002;17:217. [PubMed] [Google Scholar]
- 8.Harvey WS, Phillips CL, Essick GK. Neurosensory impairment and patient perception of recovery following orthognathic surgery. J Dent Res. 2001;80(Special Issue):187. [Google Scholar]
- 9.Phillips C, Essick G, Zuniga J, et al. Qualitative descriptors used by patients following orthognathic surgery to portray altered sensation. J Oral Maxillofac Surg. 2006;64:1751. doi: 10.1016/j.joms.2005.11.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Landis JR, Sharp TJ, Kuritz SF, et al. Mantel-Haenszel methods. Encyclopedia of Biostatistics. 1988:2378–2391. [Google Scholar]
- 11.Kiyak A. Psychological aspects of orthognathic surgery. Psychol Health. 1993;8:197. [Google Scholar]
- 12.Al-Bishri A, Dahlberg G, Barghash Z, et al. Incidence of neurosensory disturbance after sagittal split osteotomy alone or combined with genioplasty. Br J Oral Maxillofac Surg. 2004;42:105. doi: 10.1016/j.bjoms.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 13.Sandstedt P, Sorensen S. Neurosensory disturbances of the trigeminal nerve: A long-term follow-up of traumatic injuries. J Oral Maxillofac Surg. 1995;53:498. doi: 10.1016/0278-2391(95)90055-1. [DOI] [PubMed] [Google Scholar]
- 14.Essick GK. Invited discussion of: Effects of hypesthesia on oral behaviors of the orthognathic surgery patient (Lemke RR, Clark GM, Bays RA, Tiner BD, Rugh JD) J Oral Maxillofac Surg. 1998;56:158. doi: 10.1016/s0278-2391(98)90856-4. [DOI] [PubMed] [Google Scholar]
- 15.Upton LG, Rajvanakarn M, Hayward JR. Evaluation of the regenerative capacity of the inferior alveolar nerve following surgical trauma. J Oral Maxillofac Surg. 1987;45:212. doi: 10.1016/0278-2391(87)90117-0. [DOI] [PubMed] [Google Scholar]
- 16.Cunningham LL, Tiner BD, Clark GM, et al. A comparison of questionnaire versus monofilament assessment of neurosensory deficit. J Oral Maxillofac Surg. 1996;54:454. doi: 10.1016/s0278-2391(96)90120-2. [DOI] [PubMed] [Google Scholar]
- 17.Essick GK, Patel S, Trulsson M. Mechano- and thermosensory changes across the border of impaired sensitivity to pinprick after mandibular nerve injury. J Oral Maxillofac Surg. 2002;60:1250. doi: 10.1053/joms.2002.35721. [DOI] [PubMed] [Google Scholar]
- 18.Essick GK. Psychophysical assessment of patients with post-traumatic neuropathic trigeminal pain. J Orofac Pain. 2004;8:345. [PubMed] [Google Scholar]