Abstract
Rapidly expanding evidence increasingly strengthens the evidence linking psychological factors to asthma and allergy expression. Parallel studies in animals and humans demonstrating the influence of prenatal maternal stress and early caregiving experiences on the disrupted regulation of defensive biological systems [eg, sympathetic and adrenomedullary (SAM) system and the hypothalamicpituitary-adrenocortical (HPA) axis] provide strong proof of concept for this line of research. The consequent altered neuroimmune responses may influence the expression of immune-mediated disorders such as asthma as well as enhance an individual's susceptibility to other environmental factors that may also contribute to asthma risk.
Keywords: asthma, childhood, interactions, prenatal, stress
Introduction
Efforts to understand the role of psychological stress in asthma expression and atopy are currently undergoing rapid expansion in the context of our increased understanding of both the neurobiology of stress and asthma pathophysiology, [1] as well as trying to determine why asthma remains a leading cause of health disparities largely unexplained by known physical environmental factors [2,3]. Notably, consensus statements by both the National Academy of Science and the National Institute of Environmental Health Sciences [4] support the position that examining disparities in environmental health requires attention to both environmental hazards and social conditions [5]. Although a number of theoretical models explaining health disparities have been proposed, a psychosocial stress model may offer the greatest promise [3,6,7].
With an estimated half of all cases diagnosed by age 3 years and two-thirds diagnosed by age 5 years, asthma is a developmental disease [8]. This developmental framework presupposes that adverse early-life experiences, including prenatal exposures, may negatively influence neuroendocrine and immune developmental processes relevant to asthma risk. Although studies of mechanisms by which perinatal stress may increase the risk of childhood asthma are only beginning to emerge, [9,10] proof of concept is provided by drawing from animal studies on the effects of early-life adversity on stress neurobiology and development and more recent human data that parallel the animal research. This overview provides a framework grounded in this theoretical rationale and may guide future studies that examine the mechanisms underlying the role of stress in asthma development in epidemiologic research.
Neurobiology of Stress
Psychological stressors have been associated with the activation of the sympathetic and adrenomedullary (SAM) system and the hypothalamic-pituitary-adrenocortical (HPA) axis (see Wright [1] for an extensive review). Negative emotional responses disturb the regulation of the HPA axis and the SAM systems; that is, in the face of stress, physiologic systems may operate at higher or lower levels than during normal homeostasis. The disturbed balance of these systems is relevant to disease. Immune, metabolic, and neural defensive biologic responses important for the short-term response to stress may produce long-term damage if not checked and eventually terminated [11]. The potential detrimental cost of such accommodation to stress has been conceptualized as allostatic load (ie, wear and tear from chronic under- or overactivity of the allostatic system). Hormones and neuropeptides released into the circulation when individuals experience stress are thought to be involved in regulating both immunomediated and neurogenic inflammatory processes. Studies in animals and humans have shown that prenatal maternal stress and disturbances in early caregiving may have lasting effects on the stress pathways discussed above [12-14].
Critical Developmental Periods
Prenatal Maternal Stress and Perinatal Physiologic Programming
Studies suggest that characteristics of the in utero environment, independent of genetic susceptibility, influence fetal development, including immune development. The concept that nongenetic factors act early in life to permanently organize or imprint physiologic systems is known as perinatal programming [15]. The HPA axis seems particularly susceptible to early-life programming. Both nonhuman primate and rodent models of prenatal stress and early adverse caregiving [13,14,16] have helped us understand the consequences of similar experiences in humans [17,18]. Maternal and fetal stress stimulates placental secretion of corticotropin-releasing hormone, which, in turn, is elevated in the neonatal circulation [19-22]. This may stimulate the fetal HPA axis to secrete glucocorticoids, amplifying fetal glucocorticoid excess. Although these in utero responses may be adaptive in the short term, being geared toward coping with anticipated environmental challenges, ultimately they may exact a toll in contributing to increased risk of disease in later life [15].
A well-known key characteristic of HPA axis functioning is the marked interindividual variability of responses to challenge, [23] and the understanding of the relevance of this neuroendocrine system in human pathophysiology (including that relevant to asthma) requires the identification of the determinants of this variability. Genetic factors, other in utero and postnatal environmental factors, and the timing of exposures likely impact the differentiation of this response. The notion that the influence of maternal stress on such physiologic programming may vary based on an individual's genetic background is supported by noted strain differences in hormonal and behavioural responses to stress in rats and mice [15]. Data suggest that fetoplacental 11β-hydroxysteroid dehydrogenase, type 2 (11β-HSD2), may play an important role in modulating the programming effects of prenatal endogenous glucocorticoid exposure [19,24]. The type 2 isoform inactivates cortisol to cortisone, plays a role in the ontogeny of the fetal pituitary-adrenal axis, and protects the developing fetus from the adverse effects of circulating maternal glucocorticoids [25]. Interestingly, 11β-HSD2 has been colocalized in human lung tissue and is expressed in human placenta [26,27]. Interperson and interstrain (mouse) variability in the expression and efficiency of 11β-HSD2 has been demonstrated, suggesting genetic variability [28]. Glucocorticoid receptors are also highly expressed in virtually all fetal tissues from midgestation or earlier [29]. Variants of the glucocorticoid receptor gene may contribute to interindividual variability in HPA axis activity and glucocorticoid sensitivity in response to stress as well [30].
The complexity of the measurement issues related to prenatal physiologic stress responses is beyond the scope of this overview. A number of recent reviews provide more detail [31,32]. Others highlight particular methodologic challenges and detail strategies for studying these processes prenatally [33,34].
Also central to consideration of the influence of antenatal maternal stress on the postnatal development of children are the putative effects of episodes of such stress on the fetus. These are beginning to be explored and documented [35]. Prenatal cortisol dysregulation in depressed pregnant women has been linked to prematurity and low birth weight [36] and postpartum depression [37]. Gestational exposure to maternal stress has been shown to alter the development of humoral immunocompetence in offspring, as well as their hormonal and immunologic responses to postnatal stress [38-41]. Evidence in rhesus monkeys suggests that stress experienced during pregnancy impacts the infant monkeys' response to antigens at birth [42].
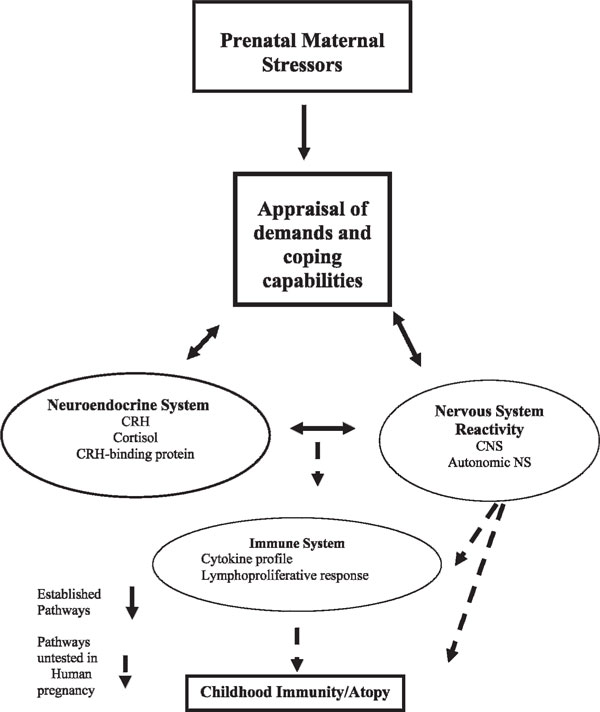
In this light, there is also evidence that the asthma phenotype could be programmed before birth. Both genetic and environmental factors affecting maturation of the immune system during pregnancy and early childhood set the stage for the inflammatory processes and altered reactivity to stimuli that are characteristic of chronic asthma. Studies have shown a positive association between maternal use of antibiotics during pregnancy and the development of childhood asthma and a negative association between maternal use of probiotics during pregnancy and the development of childhood asthma [43]. Others have considered the influence of maternal infections during gestation on asthma risk [44-48]. Some speculate that stress triggers hormones in early life, which influence T helper (Th)2 cell predominance, perhaps through a direct influence of stress hormones on cytokine production, [1,49] although this has not been studied directly to date. In particular, alterations in stress-induced maternal cortisol levels may influence the fetal immune system development and lead to an increased risk of atopic disorders, as conceptualized in Figure 1.
Figure 1.
Conceptual model linking prenatal maternal stress with childhood immunity. CNS = central nervous system; CRH = corticotropinreleasing hormone; NS = nervous system.
In preliminary analyses in our laboratory, we examined the relationship between diurnal salivary cortisol expression and total immunoglobulin E (IgE) among 89 pregnant mothers enrolled in the Asthma Coalition on Community, Environment, and Social Stress (ACCESS) project, a prospective cohort designed to study the effects of early-life stress on urban childhood asthma risk [50]. Salivary cortisol was collected five times per day over 3 consecutive days to assess basal awakening response, morning rise, diurnal slope, and area under the curve. Total IgE was dichotomized above or below the population mean (48.95 IU/mL). Repeated measures mixed models were run controlling for race, income, and weeks pregnant at the time of cortisol sampling. Higher levels of maternal total IgE were significantly associated with a flatter diurnal cortisol slope (p = .05). Examination of the cortisol curves showed that those with higher IgE demonstrated less of a decline during the evening. Thus, blunted HPA functioning in pregnant women was related to higher maternal total IgE expression. Other evidence suggests that elevated maternal IgE in utero may potentiate fetal sensitization to allergens and enhance atopic risk in infancy [51]. Stress-induced altered activity of the maternal HPA axis may have immunomodulatory effects that influence expression of IgE during pregnancy, which, in turn, may have implications for fetal sensitization and childhood allergy and asthma risk. These findings warrant further study.
Early Childhood Caregiving Experience
The early childhood environment and caregiving experience can also impact these processes [52-54]. Studies in both rodents and primates have shown that environmental manipulations that increase maternal stress result in elevated cortisol levels and dysfunctional behaviours in offspring that are evident later in life [55-57]. In parallel to the animal studies, evidence linking the social environment and social stress to regulation of the HPA axis during early development in humans is also growing [17]. Numerous retrospective studies in human HPA functioning suggest that increased reactivity of the HPA system is associated with early-life trauma [58-61] and severe deprivation [62]. Studies of infants and toddlers have linked maternal depression to dysregulation of the child's HPA axis in both cross-sectional [63] and longitudinal [64] studies. Other studies of preschoolers and older children suggest that children's cortisol levels are positively correlated with numerous social stresses [65-67] and to broader family characteristics known to be associated with higher stress levels (eg, low socio-economic status [SES]) [65]. Essex and colleagues examined the relationships of maternal stress beginning in infancy and concurrent stress on preschoolers' (aged 4.5 years) HPA activity and later mental health outcomes [68]. A cross-sectional analysis revealed that preschoolers exposed to high levels of concurrent maternal stress had elevated cortisol levels. Longitudinal analyses showed that concurrently stressed children with elevated cortisol also had a history of high maternal stress exposure in infancy. Importantly, children exposed only to high levels of concurrent or early stress had cortisol levels that did not significantly differ from those never exposed to stress. Also of note, further analysis of the specific components of stress indicated that maternal depression beginning in infancy was the most potent predictor of children's cortisol.
In this context, it is notable that our laboratory has also linked early-life caregiver stress to repeated wheeze [9] and dysregulation of immune function [10] in a birth cohort predisposed to atopy. Specifically, caregiver stress assessed during infancy predicted antigen-specific T-cell proliferative responses in children at approximately 2 years of age [10]. There is growing evidence that these cytokine patterns are already present in the first year of life [69] and may have their roots in utero [70].
Need to Consider Environmental Interactions with Stress
Another notion that we have explored in an ongoing Boston cohort is whether there is increased asthma risk in lower-income urban environments that can be explained, in part, by a combination of increased contaminant exposures and greater susceptibility to their effects. It has long been noted that air pollution, for instance, may be higher near major roadways, power plants, and industrial sites, where property values are lower and lower-income populations reside. Increased life stress among subgroups living in lower-income neighborhoods has also been proposed as a primary pathway through which socioecomic position (SEP) impacts health [7]. These observations suggest that chronic social stressors, such as violence, may be more prevalent or severe in the same communities where pollution is elevated, resulting in both greater exposures and greater susceptibility [71].
Traffic-related air pollution is linked to asthma exacerbation and respiratory outcomes [72,73]. In the United States and Europe, children living or attending school near truck routes and highways show increased asthma symptoms, [72] hospitalizations, [74] allergic rhinitis, [75] and reduced lung function [73]. Traffic-related pollutants may also influence etiology [76].
In parallel, chronic stress has been linked to asthma symptoms in cross-sectional population studies [77] and in prospective studies linking caretaker stress to infant wheeze [9] and IgE and immune mediator production [10]. Some evidence indicates that violent events may trigger asthma episodes [78]. Chronic stress may induce HPA axis and cortisol dysregulation, [79,80] glucocorticoid resistance, [81] SAM activation, catecholamine production, [82] immune mediator function, inflammation, [82] and cytokine production [10,83]. Finally, stress and pollution impact common physiologic systems, facilitating synergistic effects; earlychildhood environmental exposures and catecholamines affect Th1-Th2 balance [1]. For example, studies show that psychological stress, [84] diesel exhaust, cigarette smoke, and ozone affect oxidative stress, asthma, and chronic obstructive pulmonary disease [85].
Traffic-health relationships have been examined using many traffic indicators, [75,86] with no consensus on which best capture variability in traffic-related pollution or health outcomes in different settings. Previous studies have successfully extrapolated traffic-related exposures from sampling homes to larger cohorts using predictive land-use regression (LUR) models [73,86]. LUR shows strong predictive power for intraurban nitric oxide (NO2) variability, [87] using traffic and land use characteristics (ie, population density, major sources).
My research group investigated the potential for exposure to violence (ETV), as a chronic stressor, to increase pollution susceptibility [88]. We developed GIS- based models to retrospectively estimate residential exposures to traffic-related air pollution for 413 children in a community-based pregnancy cohort recruited in East Boston, Massachusetts, between 1987 and 1993, using monthly NO2 measurements for 13 sites collected over 18 years. Merging pollution estimates with questionnaire data on lifetime ETV (considered here as a chronic stressor) and prospectively collected repeated measures data on asthma onset in these urban children, we explored the hypothesis that stress may enhance the susceptibility to air pollution in childhood asthma etiology.
After correcting for potential confounders, including gender, SES, race/ethnicity, tobacco smoke exposure, and lower respiratory tract illnesses, we found an elevated risk of asthma with a 1 SD (4.3 ppb) increase in NO2 exposure solely among children with above-median violence exposures (odds ratio [OR] = 1.63; 95% confidence interval [CI] = 1.14-2.33; p = .03). Among children always living in the same community, with lesser measurement error, this association was magnified (OR = 2.40; 95% CI = 1.48-3.88; p = .0009).
Summary
Evidence from both animal and human studies supports the notion that HPA functioning and other stress pathways may be altered by in utero stress and early caregiving experiences. Both nonhuman primate and rodent models of early adverse caregiving [13,14,16] have helped us understand the consequences of similar experiences in humans [17,18]. Disturbed regulation of stress systems (eg, HPA axis and the SAM system) related to chronic stress suggests that immune function, which is modulated by these systems, may also be disrupted in these individuals. This, in turn, may have implications for asthma development [89]. Future studies that incorporate these strands of overlapping scholarship and strategies for studying stress reactivity during pregnancy, infancy, and early childhood are needed to continue to elucidate the mechanisms underlying the links between stress and asthma development. Specifically, these studies need to address how fetal exposure to stress may influence human immune and neuroendocrine development, whether such effects are independent of postnatal exposures, and how these pathways may, in turn, influence asthma development. The role of exposure timing and critical windows of development will need to be considered in these study designs. By so doing, we will be better able to translate this research into more effective intervention strategies and treatments.
Moreover, given the potential spatial covariance across exposures, and because stress and physical environmental factors (eg, pollution) may influence common physiologic pathways (ie, oxidative stress) and health outcomes (ie, respiratory disease), [1] stronger methods are needed to disentangle their effects and investigate synergies [3,7,90]. Similar hypotheses could be developed in relation to stress and tobacco exposure.
References
- Wright RJ. Stress and atopic disorders. J Allergy Clin Immunol. 2005;116:1301–6. doi: 10.1016/j.jaci.2005.09.050. [DOI] [PubMed] [Google Scholar]
- Gold DR, Wright RJ. Population disparities in asthma. Annu Rev Public Health. 2005;26:1–25. doi: 10.1146/annurev.publhealth.26.021304.144528. [DOI] [PubMed] [Google Scholar]
- Wright RJ, Fisher EB. In: Neighborhoods and health. Kawachi I, Berkman LF, editor. New York: Oxford University Press; 2003. Putting asthma into context: influences on risk, behavior, and intervention; pp. 233–62. full_text. [Google Scholar]
- Summary of the Symposium on Genetic Variation and Gene Environment Interaction in Human Health and Disease. National Institute of Environmental Health Sciences (NIEHS), National Human Genome Research Institute (NHGRI) and National Institute of Alcohol Abuse and Alcoholism (NIAAA) http://www.niehs.nih.gov/health/topics/science/gene-env/docs/gesymp03.pdf (accessed November 30, 2007).
- Hernandez LM, Blazer DG, editor. Committee on Assessing Interactions Among Social, Behavioral and Genetic Factors in Health. Genes, behavior, and the social environment: moving beyond the nature/nurture debate. Washington (DC): Institute of Medicine of the National Academies; 2006. pp. 109–31. [Google Scholar]
- Dressler WW, Oths KS, Gravlee CC. Race and ethnicity in public health research: models to explain health disparities. Annu Rev Anthropol. 2005;34:231–52. doi: 10.1146/annurev.anthro.34.081804.120505. [DOI] [Google Scholar]
- Gee GC, Payne-Sturges DC. Environmental health disparities: a framework integrating psychosocial and environmental concepts. Environ Health Perspect. 2004;112:1645–53. doi: 10.1289/ehp.7074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed CE. The natural history of asthma. J Allergy Clin Immunol. 2006;118:543–8. doi: 10.1016/j.jaci.2006.06.020. [DOI] [PubMed] [Google Scholar]
- Wright RJ, Cohen S, Carey V. Parental stress as a predictor of wheezing in infancy: a prospective birth-cohort study. Am J Respir Crit Care Med. 2002;165:358–65. doi: 10.1164/ajrccm.165.3.2102016. [DOI] [PubMed] [Google Scholar]
- Wright RJ, Finn PW, Contreras JP. Chronic caregiver stress and IgE expression, allergen-induced proliferation and cytokine profiles in a birth cohort predisposed to atopy. Am Acad Allergy Asthma Immunol. 2004;113:1051–7. doi: 10.1016/j.jaci.2004.03.032. [DOI] [PubMed] [Google Scholar]
- McEwen BS. Protective and damaging effects of stress mediators: the good and bad sides of the response to stress. Metab Clin Exp. 2002;51(6 Suppl 1):2–4. doi: 10.1053/meta.2002.33183. [DOI] [PubMed] [Google Scholar]
- Meaney MJ, Szyf M. Maternal care as a model for experiencedependent chromatin plasticity? Trends Neurosci. 2005;28:456–63. doi: 10.1016/j.tins.2005.07.006. [DOI] [PubMed] [Google Scholar]
- Sanchez MM, Ladd CO, Plotsky PM. Early adverse experience as a developmental risk factor for later psychopathology: evidence from rodent and primate models. Dev Psychopathol. 2001;13:419–49. doi: 10.1017/S0954579401003029. [DOI] [PubMed] [Google Scholar]
- Sanchez MM. The impact of early adverse care on HPA axis development: nonhuman primate models. Horm Behav. 2006;50:623–31. doi: 10.1016/j.yhbeh.2006.06.012. [DOI] [PubMed] [Google Scholar]
- Welberg L, Seckl J. Prenatal stress, glucocorticoids and the programming of the brain. J Neuroendocrinol. 2001;17:113–28. doi: 10.1046/j.1365-2826.2001.00601.x. [DOI] [PubMed] [Google Scholar]
- Sanchez MM, Noble PM, Lyon CK. Alterations in diurnal cortisol rhythm and acoustic startle response in nonhuman primates with adverse rearing. Biol Psychiatry. 2005;15:373–81. doi: 10.1016/j.biopsych.2004.11.032. [DOI] [PubMed] [Google Scholar]
- Gunnar MR, Donzella B. Social regulation of the cortisol levels in early human development. Psychoneuroendocrinology. 2002;27:199–220. doi: 10.1016/S0306-4530(01)00045-2. [DOI] [PubMed] [Google Scholar]
- Gunnar MR. Quality of early care and buffering of neuroendocrine stress reactions: potential effects on the developing human brain. Prev Med. 1998;27:208–11. doi: 10.1006/pmed.1998.0276. [DOI] [PubMed] [Google Scholar]
- Seckl J. Glucocorticoids, feto-plaental 11-beta-hydroxysteroid dehydrgenase type 2, and the early life origins of adult disease. Steroids. 1997;62:89–94. doi: 10.1016/S0039-128X(96)00165-1. [DOI] [PubMed] [Google Scholar]
- Seckl JR. Glucocorticoid programming of the fetus: adult phenotypes and molecular mechanisms. Mol Cell Endocrinol. 2001;185:61–71. doi: 10.1016/S0303-7207(01)00633-5. [DOI] [PubMed] [Google Scholar]
- Reinisch JM, Simon NG, Karwo WG. Prenatal exposure to prednisone in humans and animals retards intra-uterine growth. Science. 1978;202:436–8. doi: 10.1126/science.705336. [DOI] [PubMed] [Google Scholar]
- Goland RS, Jozak S, Warren WB. Elevated levels of umbilical cord plasma corticotropin-releasing hormone in growth-related fetuses. J Clin Endocrinol Metab. 1993;77:1174–9. doi: 10.1210/jc.77.5.1174. [DOI] [PubMed] [Google Scholar]
- Marsland AL, Manuck SB, Fazzari TV. Stability of individual differences in cellular immune responses to acute psychological stress. Psychosom Med. 1995;57:295–8. doi: 10.1097/00006842-199505000-00012. [DOI] [PubMed] [Google Scholar]
- Edwards C, Benediktsson R, Lindsay R, Seckl J. Dysfunction of placental glucocorticoid barrier--link between fetal environment and adult hypertension. Lancet. 1993;341:355–7. doi: 10.1016/0140-6736(93)90148-A. [DOI] [PubMed] [Google Scholar]
- Krozowski Z, Li KXZ, Koyama K. The type I and type II 11 beta-hydroxysteroid dehydrogenase enzymes. J Steroid Mol Biol. 1999;69:391–401. doi: 10.1016/S0960-0760(99)00074-6. [DOI] [PubMed] [Google Scholar]
- Brown RW, Diaz R, Robson A. The ontogeny of 11beta-hydroxysteroid dehydrogenase type 2 and mineralocorticoid receptor gene expression reveal intricate control of glucocorticoid action in development. Endocrinology. 1996;137:794–7. doi: 10.1210/en.137.2.794. [DOI] [PubMed] [Google Scholar]
- Hirasawa G, Sasano H, Takahashi K. Colocalization of 11beta-hydroxysteroid dehydrogenase type II and mineralocorticoid receptor in human epithelia. J Clin Endocrinol Metab. 1997;82:3859–63. doi: 10.1210/jc.82.11.3859. [DOI] [PubMed] [Google Scholar]
- Stewart P, Rogerson F, Mason J. Type 2, 11beta-hydroxysteroid dehydrogenase messenger RNA and activity in human placenta and fetal membranes: its relationship to birth weight and putative role in fetal steroidogenesis. J Clin Endocrinol Metab. 1995;80:885–90. doi: 10.1210/jc.80.3.885. [DOI] [PubMed] [Google Scholar]
- Diaz R, Brown RW, Seckl JR. Ontogeny of mRNAs encoding glucocorticoid and mineralocorticoid receptors and 11beta-deoxysteroid dehydrogenase in prenatal rat brain development reveal complex control of glucocorticoid action. J Neurosci. 1998;18:2570–80. doi: 10.1523/JNEUROSCI.18-07-02570.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wust S, Van Rossum EF, Federenko IS. Common polymorphisms in the glucocorticoid receptor gene are associated with adrenocortical responses to psychosocial stress. J Clin Endocrinol Metab. 2004;89:565–73. doi: 10.1210/jc.2003-031148. [DOI] [PubMed] [Google Scholar]
- de Weerth C, Buitelaar JK. Physiological stress reactivity in human pregnancy--a review. Neurosci Biobehav Rev. 2005;29:295–312. doi: 10.1016/j.neubiorev.2004.10.005. [DOI] [PubMed] [Google Scholar]
- Monk C, Myers MM, Sloan RP. Effects of women's stresselicited physiological activity and chronic anxiety on fetal heart rate. J Dev Behav Pediatr. 2003;24:32–8. doi: 10.1097/00004703-200302000-00008. [DOI] [PubMed] [Google Scholar]
- Harville EW, Savitz DA, Dole N. Patterns of salivary cortisol secretion in pregnancy and implications for assessment protocols. Biol Psychiatry. 2007;74:85–91. doi: 10.1016/j.biopsycho.2006.07.005. [DOI] [PubMed] [Google Scholar]
- Jones NM, Holzman CB, Zanella AJ. Assesing mid-trimester salivary cortisol levels across three consecutive days in pregnant women using an at-home collection protocol. Paediatr Perinatal Epidemiol. 2006;20:425–37. doi: 10.1111/j.1365-3016.2006.00744.x. [DOI] [PubMed] [Google Scholar]
- DiPietro JA, Cotigan KA, Gurewitsch ED. Fetal response to induced maternal stress. Early Hum Dev. 2003;74:125–38. doi: 10.1016/j.earlhumdev.2003.07.001. [DOI] [PubMed] [Google Scholar]
- Field T, Hernandez-Reif M, Diego M. Prenatal cortisol, prematurity and low birthweight. Infant Behav Dev. 2006;29:268–75. doi: 10.1016/j.infbeh.2005.12.010. [DOI] [PubMed] [Google Scholar]
- Nierop A, Bartsikas A, Zimmerman R, Ehlert U. Are stress-induced cortisol changes during pregnancy associated with postpartum depressive symptoms? Psychosom Med. 2006;68:931–7. doi: 10.1097/01.psy.0000244385.93141.3b. [DOI] [PubMed] [Google Scholar]
- Barker DJ. A new model for the origins of chronic disease. Med Health Care Philos. 2001;4:31–5. doi: 10.1023/A:1009934412988. [DOI] [PubMed] [Google Scholar]
- Hales CN, Barker DJP, Clark PMS. Fetal and infant growth and impaired glucose tolerance at age 64. BMJ. 1991;303:1019–22. doi: 10.1136/bmj.303.6809.1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levitt NS, Lindsay RS, Holmes MC, Seckl JR. Dexamethasone in the last week of pregnancy attenuates hippocampal glucocorticoid receptor gene expression and elevates blood pressure in the adult offspring in the rat. Neuroendocrinology. 1986;39:1299–305. doi: 10.1159/000127146. [DOI] [PubMed] [Google Scholar]
- Egliston K-A, McMahan C, Austin M-P. Stress in pregnancy and infant HPA axis function: conceptual and methodological issues relating to the use of salivary cortisol as an outcome measure. Psychoneuroendocrinology. 2007;32:1–13. doi: 10.1016/j.psyneuen.2006.10.003. [DOI] [PubMed] [Google Scholar]
- Coe CL, Lubach GR, Karaszewski JW. Prenatal stress and immune recognition of self and nonself in the primate neonate. Biol Neonate. 1999;76:301–10. doi: 10.1159/000014172. [DOI] [PubMed] [Google Scholar]
- Kalliomäki M, Salminen S, Arvilommi H. Probiotics in primary prevention of atopic disease: a randomized placebocontrolled trial. Lancet. 2001;357:1076–9. doi: 10.1016/S0140-6736(00)04259-8. [DOI] [PubMed] [Google Scholar]
- Hughes CH, Jones RC, Wright DE, Dobbs FF. A retrospective study of the relationship between childhood asthma and respiratory infection during gestation. Clin Exp Allergy. 1999;29:1378–81. doi: 10.1046/j.1365-2222.1999.00662.x. [DOI] [PubMed] [Google Scholar]
- Xu B, Pekkanen J, Jarvelin MR. Maternal infections in pregnancy and the development of asthma among offspring. Int J Epidemiol. 1999;28:723–7. doi: 10.1093/ije/28.4.723. [DOI] [PubMed] [Google Scholar]
- McKeever T, Lewis SA, Smith C, Hubbard R. The importance of prenatal exposures on the development of allergic disease: a birth cohort study using the West Midlands General Practice Database. Am J Respir Crit Care Med. 2002;166:827–32. doi: 10.1164/rccm.200202-158OC. [DOI] [PubMed] [Google Scholar]
- Calvani M, Alessandri C, Sopo SM. Infections and uterus related complications during pregnancy and development of atopic and nonatopic asthma in children. Allergy. 2004;59:99–106. doi: 10.1046/j.1398-9995.2003.00338.x. [DOI] [PubMed] [Google Scholar]
- Macaubas C, De Klerk NH, Holt BJ. Association between antenatal cytokine production and the development of atopy and asthma at age 6 years. Lancet. 2003;362:1192–7. doi: 10.1016/S0140-6736(03)14542-4. [DOI] [PubMed] [Google Scholar]
- von Hertzen LC. Maternal stress and T-cell differentiation of the developing immune system: possible implications for the development of asthma and atopy. J Allergy Clin Immunol. 2002;109:923–8. doi: 10.1067/mai.2002.124776. [DOI] [PubMed] [Google Scholar]
- Wright RJ, Franco-Suglia S, Staudenmayer JW. AJRCCM 2007. Blunted cortisol response predicts increased total IgE in pregnant mothers enrolled in an urban asthma birth-cohort: Project ACCESS. Presented at the International Conference of the American Thoracic Society; San Francisco, CA. 2007.
- Liu C-A, Wang C-L, Chuang H. Prenatal prediction of infant atopy by maternal but not paternal total IgE levels. J Allergy Clin Immunol. 2003;112:899–904. doi: 10.1016/j.jaci.2003.08.030. [DOI] [PubMed] [Google Scholar]
- Vallee M, Mayo W, Dellu F. Prenatal stress induces high anxiety and postnatal handling induces low anxiety in adult offspring: correlation with stress-induce corticosterone secretion. J Neurosci. 1997;17:626–36. doi: 10.1523/JNEUROSCI.17-07-02626.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu D, Diorio J, Tannenbaum B. Maternal care, hippocampal gluccocorticoid receptors, and hypothalamic-pituitary-adrenal response to stress. Science. 1997;277:1659–62. doi: 10.1126/science.277.5332.1659. [DOI] [PubMed] [Google Scholar]
- Anisman H, Zaharia MD, Meaney MJ, Merali Z. Do early-life events permanently alter behavioral and hormonal responses to stressors? Int J Dev Neurosci. 1998;16:149–64. doi: 10.1016/S0736-5748(98)00025-2. [DOI] [PubMed] [Google Scholar]
- Caldji C, Diorio J, Meaney MJ. Variations in maternal care in infancy regulate the development of stress reactivity. Biol Psychiatry. 2000;48:1164–74. doi: 10.1016/S0006-3223(00)01084-2. [DOI] [PubMed] [Google Scholar]
- Coplan J, Andrews MW, Rosenblum LA. Persistent elevations of cerebrospinal fluid concentrations of corticotropin-releasing factor in adult nonhuman primates exposed to early-life stressors: implications for the pathophysiology of mood and anxiety disorders. Proc Natl Acad Sci USA. 1996;93:1619–23. doi: 10.1073/pnas.93.4.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francis DD, Caldji C, Champagne F. The role of corticotropin-releasing factor-norepinephrine systems in mediating the efects of early experience on the development of behavioral and endocrine responses to stress. Biol Psychiatry. 1999;46:1153–66. doi: 10.1016/S0006-3223(99)00237-1. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA. Diverse patterns of neuroendocrine activity in maltreated children. Dev Psychopathol. 2001;13:677–93. doi: 10.1017/S0954579401003145. [DOI] [PubMed] [Google Scholar]
- DeBellis MD, Baum AS, Birmaher B. Developmental traumatology, part 1: biological stress systems. Biol Psychiatry. 1999;9:1259–70. doi: 10.1016/S0006-3223(99)00044-X. [DOI] [PubMed] [Google Scholar]
- Heim C, Newport DJ, Heit S. Pituitary-adrenal and autonomic responses to stress in women after sexual and physical abuse in childhood. JAMA. 2000;284:592–7. doi: 10.1001/jama.284.5.592. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Perel J. The corticotropin-releasing hormone challenge in depressed abused, depressed nonabused, and normal control children. Biol Psychiatry. 1997;42:669–79. doi: 10.1016/S0006-3223(96)00470-2. [DOI] [PubMed] [Google Scholar]
- Gunnar MR, Bruce J, Hickman SE. Salivary cortisol response to stress in children. Adv Psychosom Med. 2001;22:52–60. doi: 10.1159/000059275. full_text. [DOI] [PubMed] [Google Scholar]
- Field T. Monographs of the society for research in child development. The development of emotion regulation: Biological and behavioral considerations. 1994;59(21):208–227. [PubMed] [Google Scholar]
- Hessl D, Dawson G, Frey K. In: Advancing research on developmental plasticity: integrating the behavioral sciences and the neurosciences of mental health. Hann DM, Huffman LC, Lederhendler KK, Minecke D, editor. Bethesda (MD): National Institutes of Mental Health; 1998. A longitudinal study of children of depressed mothers: psychobiological findings related to stress. [Google Scholar]
- Lupien SJ, King S, Meaney MJ, McEwen BS. Child's stress hormone levels correlate with mother's socioeconomic status and depressive state. Biol Psychiatry. 2000;48:976–80. doi: 10.1016/S0006-3223(00)00965-3. [DOI] [PubMed] [Google Scholar]
- Schmidt LA, Fox NA, Rubin KH. Behavioral and neuroendocrine responses in shy children. Dev Psychobiol. 1997;30:127–40. doi: 10.1002/(SICI)1098-2302(199703)30:2<127::AID-DEV4>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- Tout K, de Haan M, Campbell EK, Gunnar MR. Social behavior correlates of cortisol activity in child care: gender differences and time-of-day effects. Child Dev. 1998;69:1247–62. doi: 10.2307/1132263. [DOI] [PubMed] [Google Scholar]
- Essex MJ, Klein MH, Cho E, Kalin NH. Maternal stress beginning in infancy may sensitize children to later stress exposure: effects on cortisol and behavior. Biol Psychiatry. 2002;52:776–84. doi: 10.1016/S0006-3223(02)01553-6. [DOI] [PubMed] [Google Scholar]
- Lemanske RF. Issues in understanding pediatric asthma: epidemiology and genetics. J Allergy Clin Immunol. 2002;109(Suppl):S521–4. doi: 10.1067/mai.2002.124564. [DOI] [PubMed] [Google Scholar]
- Miller RL, Ginger LC, Bell CA. Prenatal exposure, maternal sensitization, and sensitization in utero to indoor allergens in an inner-city cohort. Am J Respir Crit Care Med. 2001;164:995–1001. doi: 10.1164/ajrccm.164.6.2011107. [DOI] [PubMed] [Google Scholar]
- Wright RJ. Health effects of socially toxic neighborhoods: the violence and urban asthma paradigm. Clin Chest Med. 2006;27:413–21. doi: 10.1016/j.ccm.2006.04.003. [DOI] [PubMed] [Google Scholar]
- Brauer M, Hoek G, Van Vilet P. Air pollution from traffic and the development of respiratory infections and asthmatic and allergic symptoms in children. Am J Respir Crit Care Med. 2002;166:1092–8. doi: 10.1164/rccm.200108-007OC. [DOI] [PubMed] [Google Scholar]
- Brunekreef B, Janssen NA, Hartog J. Air pollution from truck traffic and lung function in children living near motorways. Epidemiology. 1997;8:298–303. doi: 10.1097/00001648-199705000-00012. [DOI] [PubMed] [Google Scholar]
- Lin M, Chen Y, Villeneuve P. Gaseous air pollutants and asthma hospitalization of children with low household income in Vancouver, British Columbia, Canada. Am J Epidemiol. pp. 294–303. [DOI] [PubMed]
- Duhme H, Weiland SK, Keil U. The association between selfreported symptoms of asthma and allergic rhinitis and selfreported traffic density on street of residence in adolescents. Epidemiology. 1996;76:578–82. doi: 10.1097/00001648-199611000-00003. [DOI] [PubMed] [Google Scholar]
- Gordian ME, Haneuse S, Wakefield J. An investigation of the association between traffic exposure and the diagnosis of asthma in children. J Exp Sci Environ Epidemiol. 2006;16:49–55. doi: 10.1038/sj.jea.7500436. [DOI] [PubMed] [Google Scholar]
- Oh Y-M, Kim YS, Yoo SH. Association between stress and asthma symptoms: a population-based study. Respirology. 2004;93:63–8. doi: 10.1111/j.1440-1843.2004.00609.x. [DOI] [PubMed] [Google Scholar]
- Wright R, Steinbach S. Violence: an unrecognized environmental exposure that may contribute to greater asthma morbidity in high risk inner-city populations. Environ Health Perspect. 2001;109:1085–9. doi: 10.2307/3454965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirschbaum C, Helhammer DH. Salivary cortisol in psychoneuroendocrine research: recent developments and applications. Psychoneuroendocrinology. 1994;19:313–33. doi: 10.1016/0306-4530(94)90013-2. [DOI] [PubMed] [Google Scholar]
- Seeman TE, McEwen BS. Impact of social environment characteristics on neuroendocrine regulation. Psychosom Med. 1996;58:459–71. doi: 10.1097/00006842-199609000-00008. [DOI] [PubMed] [Google Scholar]
- Miller GE, Ritchey AK, Cohen S. Chronic psychological stress and regulation of pro-inflammatory cytokines: a glucocorticoidresistance model. Health Psychol. 2002;21:531–41. doi: 10.1037/0278-6133.21.6.531. [DOI] [PubMed] [Google Scholar]
- Glaser R, Kiecolt-Glaser JK. Stress-induced immune dysfunction: implications for health. Nat Immunol. 2005;5:243–51. doi: 10.1038/nri1571. [DOI] [PubMed] [Google Scholar]
- Chen E, Fisher EB, Bacharier LB, Strunk RC. Socioeconomic status, stress, and immune markers in adolescents with asthma. Psychosom Med. 2003;65:984–92. doi: 10.1097/01.PSY.0000097340.54195.3C. [DOI] [PubMed] [Google Scholar]
- Epel E, Blackburn E, Lin J. Accelerated telomere shortening in response to life stress. Proc Natl Acad Sci USA. 2004;101(49):17312–5. doi: 10.1073/pnas.0407162101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman I, MacNee W. Oxidative stress and regulation of glutathione in lung inflammation. Eur Respir J. 2000;16:534–54. doi: 10.1034/j.1399-3003.2000.016003534.x. [DOI] [PubMed] [Google Scholar]
- Brauer M, Hoek G, van Vliet P. Estimating long-term average particulate air pollution concentrations: application of traffic indicators and geographic information systems. Epidemiology. 2003;14:228–39. doi: 10.1097/00001648-200303000-00019. [DOI] [PubMed] [Google Scholar]
- Hochadel M, Heinrich J, Gehring U. Predicting long-term average concentrations of traffic-related air pollutants using GIS-based information. Atmospheric Environment. 2006;40:542–53. doi: 10.1016/j.atmosenv.2005.09.067. [DOI] [Google Scholar]
- Clougherty J, Levy JI, Kubzansky LD. The effects of trafficrelated air pollution and exposure to violence on urban asthma etiology. Environ Health Perspect. 2007;115:1140–6. doi: 10.1289/ehp.9863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright RJ, Cohen RT, Cohen S. The impact of stress on the development and expression of atopy. Curr Opin Allergy Clin Immunol. 2004;5:23–9. doi: 10.1097/00130832-200502000-00006. [DOI] [PubMed] [Google Scholar]
- O'Neill MS, Jerrett M, Kawachi I. Health, wealth, and air pollution: advancing theory and methods. Environ Health Perspect. 2003;111:1861–70. doi: 10.1289/ehp.6334. [DOI] [PMC free article] [PubMed] [Google Scholar]