Abstract
BACKGROUND
The inaccurate recording of medicines on admission to hospital is an important cause of medication error. Medication reconciliation has been used to identify and correct these errors.
OBJECTIVE
To determine if a multimodal intervention involving medication reconciliation with real-time feedback and education would reduce the number of errors made by medical staff when recording medicines at the time of admission to hospital.
DESIGN
Observational study.
PARTICIPANTS
Patients admitted to the general medical wards of a teaching hospital were studied prospectively. Patients ≥75 years of age and on ≥5 medications were identified as the ‘target group.’
INTERVENTION
After admission, a second medication history was taken, and discrepancies were identified and communicated to the medical teams. An educational intervention to encourage prescribers to obtain accurate medication histories was conducted at the same time.
MEASUREMENTS
The discrepancy rate was measured before and after the intervention.
MAIN RESULTS
There were 470 admissions in the ‘target group.’ Three hundred and thirty-eight of the admissions (71.9%) had one or more unintentional discrepancies. Although many discrepancies had little potential to cause harm, 33% were rated as clinically significant. During the study the discrepancy rate (prior to reconciliation) fell from 2.6 (SD 2.6) to 1.0 (SD 1.1) per admission (p < 0.0001). This decline in discrepancy rate remained significant (p = 0.001) even when only clinically important discrepancies were included. The proportion of admissions with one or more clinically important discrepancies also decreased during the study from 46% to 24% (p = 0.023).
CONCLUSIONS
Errors in the recording of medicines at the time of hospital admission are common. Combining the feedback provided by medication reconciliation with prescriber education reduced the error rate. This approach may be useful when the resources are not available to perform medication reconciliation for all patients admitted to hospital.
KEY WORDS: medical education, medical errors, medical record system
INTRODUCTION
Medication errors are an important cause of adverse events in hospital patients. Over half of the medication errors in hospital occur at the interfaces of care1–3 with many attributable to poor communication on admission and at other transition points in care1,3. A recent systematic review reported errors on admission in up to 67% of admissions, with many having the potential to cause harm4. Medication reconciliation is defined as a formal process of obtaining a complete and accurate list of each patient’s current home medications and comparing the physician’s admission and/or discharge orders to that list5. It has been shown to be effective in reducing errors2. The Institute for Healthcare Improvement identified medication reconciliation as one of the key interventions for improving patient safety5 in the 100,000 lives campaign and the subsequent 5 million lives campaign6. The Joint Commission on Accreditation of Healthcare Organizations (JCAHO) also identified medication reconciliation as an important national patient safety goal7.
A number of studies have investigated the rates of medication error at interfaces of care1,3,8–11, but little research has been conducted on interventions to prevent these errors occurring in the first place. In particular, our study utilised real-time feedback in addition to medication reconciliation, which is novel as other studies have only provided retrospective feedback, rather than on a case-by-case basis in real-time. The primary objective of this study was to investigate whether an education campaign, aimed at changing prescriber behaviour, would reduce error rates before medication reconciliation took place. This study also determined medication error rates on admission to Auckland City Hospital.
METHODS
Participants
This was a prospective study conducted at a 690-bed teaching hospital in Auckland, New Zealand. The primary aim was to determine whether adding education to medication reconciliation would result in a change in discrepancy rate. The majority of acute medical admissions to the hospital are cared for by the General Medical Service with smaller numbers admitted to other services such as Cardiology, Neurology and Renal Medicine. Patients admitted to the four General Medical wards, between 29 November 2006 and 30 March 2007, were eligible for inclusion. Ethics approval was not obtained as the regional ethics committee did not require approval since the study was an audit of a clinical service. Medication reconciliation was performed by a multidisciplinary team consisting of a final year pharmacy student (AC), nurse (EG), and clinical pharmacology resident (NT). On each weekday, all new general medical admissions were identified and patients included if they were admitted within the last 24 to 48 h and were likely to stay for at least 24 h before discharge. Patients who were 75 years old or older and using five or more medications prior to admission were identified as a group with a higher risk of having a discrepancy1,12 and were the “target group” for medication reconciliation. Patients living in residential care were given a lower priority for medication reconciliation. Patients admitted during the weekend or public holiday were reviewed on the first working day following admission, if they were still in hospital. Patients were still included if they were unable to communicate or cognitively impaired. Patients receiving palliative care were excluded if their regular medications had been discontinued because of expected death.
Data Collection
The name, route, dosage and frequency of all the medications the patient was taking prior to admission were recorded using a standardised data collection form. Both prescription and over-the-counter (OTC) medications were recorded including vitamin preparations, as were dietary supplements and herbal or homeopathic products, but these were not included in the analysis of discrepancies, as most of these are not supplied in hospital. Medications used on an as-required basis were included if used by the patient in the 3 weeks prior to admission. The medications were categorised by active ingredient using the Monthly Index of Medical Specialties (MIMS) listing13 of pharmacological class. Brief details concerning the reason for admission, past medical history, age, sex and allergies were obtained from the hospital notes. The grade of the admitting doctor (medical student, intern or resident) who took the initial medication history was noted.
The hospital notes and medication chart of eligible patients were reviewed within 24 h of admission where possible. This was followed by an interview with the patient to obtain information on their medication usage before hospitalisation. The interview was conducted at the bedside and had a standardised format. The information obtained was confirmed by checking with additional sources, which included two or more of the following: the referral letter from the primary care physician, a family member or caregiver, the medications brought to hospital by the patient, previous discharge summaries or direct verbal communication with the community pharmacy, primary care physician, nursing home or other institution providing residential care. Additional sources were checked until there was confidence the medication history was as accurate and complete as possible.
The medicines recorded on the medication chart on admission were compared with the history obtained from the patient (the ‘pre-admission medicines’). Differences between the ‘pre-admission’ and ‘admission’ medication lists were regarded as a discrepancy, unless the medication was deliberately started or discontinued on admission, as indicated in the notes.
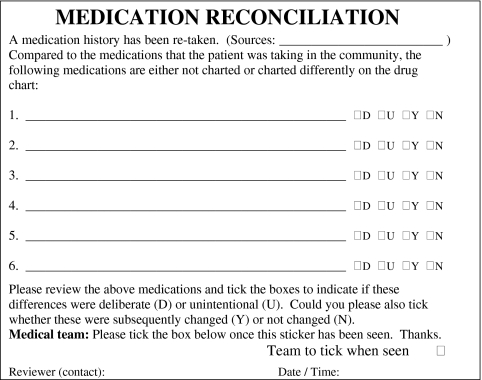
The types of discrepancy encountered included omission or addition of a medication, change in dose, frequency or time of administration and substitution with another agent of the same class. These discrepancies were communicated to the team using a standardised sticker (Fig. 1), which was placed into the clinical notes for review and completion by the medical team. The prescriber was able to note whether the discrepancy was deliberate or unintentional and record whether any changes were made to the chart as a result. Only unintentional discrepancies were considered as errors and included in the analyses. Where discrepancies were considered to have the potential to cause moderate discomfort or clinical deterioration, a text message was also sent to the medical team. If the discrepancy was thought to have the potential to cause severe discomfort or serious deterioration, the medical team was spoken to directly.
Figure 1.
Sticker placed into the hospital notes to provide feedback to the medical team and allow review of discrepancies.
Before the study, pharmacists took medication histories as part of their normal duties, but due to time limitations, this was done for only a small proportion of the patients. The pharmacists were able to continue their usual practice during the study. Any patients seen by the pharmacist were briefly reviewed by a member of the medication reconciliation team. The information collected by the pharmacist was recorded as part of the study, and if appropriate a sticker was placed in the notes.
Follow-up
Each patient was followed up at three time points: at 24 and 48 h, and after discharge. If a discrepancy was marked on the sticker as ‘deliberate’ or a reason for the difference was recorded in the notes, it was not included in the discrepancy count. A discrepancy was considered as ‘reconciled’ if the medication chart was changed within that time or the medical staff made it clear on the sticker or in the notes that they did not wish to make a change. If the medical staff did not comment on the discrepancy on the sticker or in the notes, it was recorded as ‘not reconciled’.
Multimodal Intervention to Improve Medication Documentation
An educational campaign targeted at junior medical staff was implemented to encourage accurate medication histories on admission and raise awareness about medication reconciliation. The campaign consisted of didactic teaching at the beginning, followed by posters and insertion of reminders into the hospital notes. The key message was the importance of taking an accurate medication history and of encourage prescribers to always check with the patient first. The teaching was conducted by a clinical pharmacologist (PB). An introduction to medication reconciliation was presented at one of the handover meetings, followed by a talk at an intern teaching session and one at medical grand round. The teaching emphasised the importance of taking accurate histories using multiple sources and gave examples of errors that had occurred. These presentations were done in the first few weeks and were not repeated. Posters were then placed in the admitting unit and the general medical wards, and served to remind staff to take an accurate medication history. Reminders (similar to the posters) were inserted in the back of the hospital notes folder at the time the patient was admitted. Unfortunately, we were not allowed to insert the reminders in the front of the notes. Although this would have reduced the impact of the reminders, we hoped that some prescribers would be prompted by them. These reminders and posters were introduced a few weeks into the campaign and left for the remainder of the study. The hospital pharmacy publishes a medicines information bulletin every few months that is circulated to all medical staff. One of these also discussed medication reconciliation and was circulated at the beginning of the campaign. The stickers and discussions between the junior medical staff and medication reconciliation team also provided “real-time” feedback to the prescribers. It is estimated that “face-to-face” interactions with the medical staff occurred about once a week for each intern and resident.
Severity Rating
A team consisting of a senior physician (PB), resident (NT), pharmacy student (AC) and nurse (EG) discussed and rated each discrepancy for its potential to cause discomfort or clinical deterioration. A 3-point scale, based on that used by Cornish et al.1, was used to classify the discrepancies. Decisions were reached by discussion until consensus was obtained. A record of the rating of each discrepancy was kept to maintain consistency. Class 1 discrepancies were defined as unlikely to cause patient discomfort or clinical deterioration. An example of this would be the omission of multivitamin tablets. Class 2 discrepancies had the potential to cause mild to moderate discomfort or clinical deterioration. An example would be unintentionally not charting lorazepam 1 mg twice daily when it had been taken regularly and stopping it abruptly could lead to withdrawal symptoms. Class 3 discrepancies were those which had the potential to result in severe discomfort, clinical deterioration, prolonged length of hospital stay or re-admission1. Such an example would be a patient who had severe congestive heart failure but unintentionally did not have their furosemide charted. Class 2 and 3 discrepancies were considered to be clinically important, and a separate analysis of the primary endpoints was conducted on these, with class 1 discrepancies excluded.
Study Endpoints
All analyses were performed for the target group only, i.e., those aged 75 years or older and on five or more medications. Because the main objective was to determine if adding an educational intervention to medication reconciliation would reduce the number of discrepancies, the primary endpoints were the change in mean number of discrepancies per admission per 2-week period and the change in the proportion of admissions with one or more discrepancies per 2-week period over the course of the study. This analysis was repeated with all class 1 discrepancies excluded. Secondary endpoints were discrepancy rates according to the class of medicine, route of administration, patient gender and grade of prescriber along with the change in the number of clinically important discrepancies over the course of the study.
Statistical Analysis
Poisson regression14 was used to analyse the primary endpoints to determine the change in mean number of discrepancies per admission per 2-week period and change in the proportion of admissions with one or more discrepancies per 2-week period over time. A Poisson regression was chosen instead of linear regression as most patients had no discrepancies, thereby skewing the discrepancy rate away from a normal distribution. This analysis was performed using the Statistical Analysis Software (SAS) v. 9.1. Other endpoints were analysed using the Statistical Package for Social Sciences (SPSS) v.14.0 for Windows. Means were compared using analysis of variance (ANOVA) and associations made using Pearson correlations. Differences in primary and secondary endpoints were considered to be statistically significant if the p-value was less than 0.013 (equivalent to a p-value of 0.05 with Bonferroni correction applied).
RESULTS
Medication reconciliation was conducted on 580 patients with a total of 633 admissions. This represented 25.6% of all general medical admissions during the study period. Reconciled patients had a mean age of 82 years (SD 9.9), and 57% were female. A total of 5,486 medications were recorded with a mean of 8.7 (SD 4.0) medications per patient.
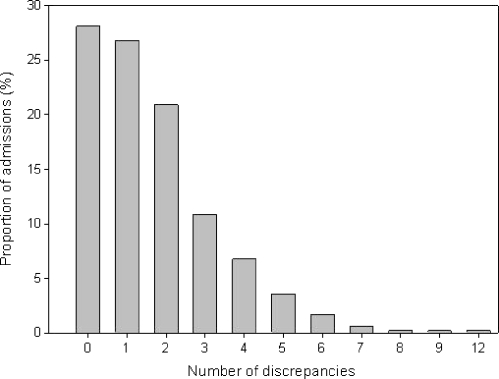
Four hundred and seventy (74%) admissions were in the target group, who were 75 years or older and on 5 or more medications. During the study, 338 (71.9%) of the admissions in this target group had at least one unintentional discrepancy (Fig. 2). Most patients had one to two discrepancies, but some had higher rates with a maximum of 12 discrepancies per admission.
Figure 2.
Distribution of the number of medication discrepancies per admission as a proportion of all patient admissions in the target population.
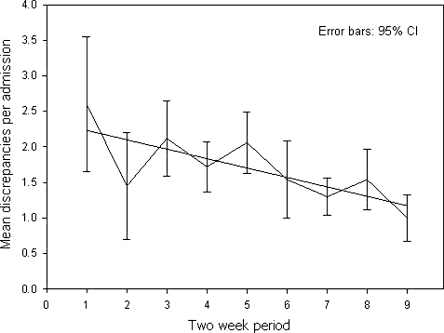
The mean number of discrepancies per admission in each 2-week period declined over the study period (p < 0.0001) (Fig. 3). In the first 2 weeks, the mean discrepancy rate was 2.6 (SD 2.6) discrepancies per admission, falling to 1.0 (SD 1.1) discrepancy per admission by the end of the study. When all class 1 discrepancies were excluded from the analysis, leaving only clinically important discrepancies (Class 2 and 3), a significant decline in the discrepancy rate over time was still observed (p = 0.001). There was a reduction in the proportion of admissions with one or more discrepancies from 83.3% to 56.3% between the first and last 2 weeks of the study, although this was not statistically significant (p = 0.28). When class 1 discrepancies were excluded, the decline seen in the proportion of admissions with one or more discrepancies were of borderline significance, reducing from 46% in the first 2 weeks to 24% in the last 2 weeks (p = 0.023).
Figure 3.
Effect of the intervention on the mean number of discrepancies per admission for each 2-week period of the intervention in the target population.
There were differences in discrepancy rates between medication classes (p < 0.0001) as shown in Table 1. Post-hoc testing showed that the discrepancy rate for the ‘ear, nose, oropharynx and eye’, ‘skin’, and ‘vitamins and minerals’ classes were higher than for other classes (p < 0.0001). There were also differences in discrepancy rates for each route of administration (p < 0.0001) with rates for inhaled and topical routes higher than for the oral route (Table 2; p < 0.0001). No difference in discrepancy rates was found for male as opposed to female patients or whether the admitting doctor was an intern or resident. Medical students were not included in the analysis as only a small percentage (<5%) of prescribing was done by students.
Table 1.
Percentage of Medications with Discrepancies in Each Medication Class
| Medication class | Number of discrepancies | Discrepancies as % of medications charted in each class (95% confidence interval) |
|---|---|---|
| Skin | 48 | 66 (55–77) |
| Eye, ear, nose and oropharynx | 52 | 50 (40–60) |
| Vitamins and minerals | 140 | 30 (26–34) |
| Genitourinary system | 15 | 30 (17–43) |
| Respiratory system | 68 | 27 (22–33) |
| Endocrine & metabolic disorders | 65 | 20 (16–24) |
| Central nervous system | 65 | 19 (15–23) |
| Alimentary system | 93 | 17 (13–20) |
| Musculoskeletal system | 15 | 16 (8–23) |
| Nutrition | 12 | 16 (8–24) |
| Infections and infestations | 5 | 15 (2–28) |
| Cardiovascular system | 160 | 9 (8–11) |
| Analgesia | 37 | 9 (6–12) |
| Other* | 11 | 24 (11–38) |
*Other includes the following medication classes: allergic disorders (14); immunology (2); neoplastic disorders (16); poisoning, toxicity and drug dependence (5); and other remedies (8).
Table 2.
Percentage of Medications with Discrepancies for Each Route of Administration
| Route of administration | Number of medications for each route | % with discrepancies (95% confidence interval) |
|---|---|---|
| Intramuscular | 33 | 30 (14–47) |
| Inhaled | 255 | 28 (22–33) |
| Oral | 3950 | 15 (13–16) |
| Rectal | 4 | 50 (42–142) |
| Subcutaneous | 41 | 20 (7–32) |
| Sublingual | 90 | 21 (13–30) |
| Topical | 170 | 58 (51–66) |
| Transdermal | 3 | 0 (–) |
| Vaginal | 3 | 100 (–) |
Of the 786 discrepancies identified in the target group, 525 (66.8%) were class 1, 249 (31.7%) were class 2 and 12 (1.5%) were class 3 in severity. Seven out of the 12 class 3 discrepancies were with cardiovascular medicines.
In the first 2 weeks of data collection, 85% (95% confidence interval, 76%–93%) of identified discrepancies were reconciled by discharge. This figure rose to 100% in the third 2-week period and remained at this level or close to it throughout the rest of the study.
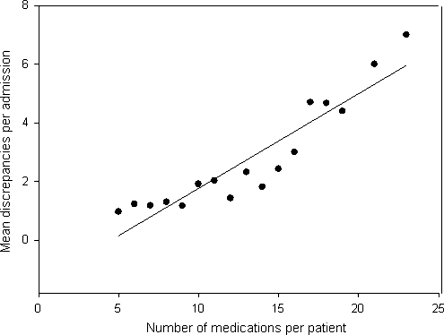
Patients who were taking a greater number of medications prior to admission were observed to have a greater number of discrepancies (p < 0.001). Figure 4 shows the number of discrepancies per admission increases with the number of medications taken by the patient prior to admission. There was no correlation between the number of discrepancies and age of the patient.
Figure 4.
The mean number of discrepancies per admission according to the number of medicines taken by the patient prior to admission.
DISCUSSION
This study reports a successful intervention to reduce medication errors on admission to a large tertiary hospital in New Zealand. Although there are many studies that report the effectiveness of pharmacist involvement and medication reconciliation on reducing discrepancy rates15,16, the novel feature of this study is that it incorporated both an educational intervention and real-time feedback to the medical staff aimed at changing prescriber behaviour.
Most previous studies have reported discrepancy rates but have not measured the effect of interventions to reduce discrepancies, in particular prior to medication reconciliation taking place1,3,8–11. An exception is a recent study from Boston that examined the effect of a web-based application that provided staff with information about the patient’s medicines prior to admission using electronic sources. This approach reduced discrepancies from 1.44 to 1.05 per patient17. This strategy differs from the approach in our study where we focused on the effect of education including providing feedback via a sticker in the notes. Another recent study that also utilised written feedback resulted in a reduction in discrepancy rate from 0.5 to 0 per patient16; however, their feedback occurred only at weekly intervals; hence, there was a time lapse between the discrepancy occurring and feedback, whereas our intervention involved both real-time feedback via a novel sticker system and proactive education. Our intervention was successful, and there was a pronounced decline in error rate during the study. With the exception of the dip observed in the second 2-week period, there appears to have been a consistent decrease over time. The dip observed coincides with Christmas and New Year when very few admissions were reconciled. There was a parallel, statistically significant reduction in the number of clinically important discrepancies over time.
We have also confirmed the findings of previous studies1,11 that show a large number of errors in the recording of medicines on admission to hospital. The error rate in this study was a little higher than most other studies1,18, with over 70% of admissions having one or more discrepancies. This may reflect the characteristics of our study population where the patients were on more medications compared to previous studies1,18. About one-third of admissions had clinically important discrepancies; a figure similar to those reported in other studies1,18,19.
We observed anecdotally that the admitting doctor often use patients’ previous discharge summaries as sources of medication histories rather than talking to the patient. This may have contributed to errors. Many doctors are unaware that past records are often out of date and may not accurately reflect the medications that the patient was taking. In addition, a significant proportion of admissions occur outside of normal working hours, and medication histories cannot be checked with the patient’s general practitioner or community pharmacy until the next working day.
Not surprisingly, the medications most commonly implicated in discrepancies were those that did not use the oral route. This may be because medications that are not taken orally are not thought to be important by the patient and doctor, and therefore are more likely to be omitted. The largest number of clinically important errors occurred in the cardiovascular class, with 7 out of the 12 Class 3 errors occurring within this class; 49% of all the errors in the cardiovascular class were considered clinically important compared to an average rate of 33% in other medication classes. Cardiovascular medications such as anticoagulants and anti-arrhythmics are more likely to result in an adverse outcome than other medication classes12, and extra vigilance needs to be taken when charting these medications.
A positive association between the number of medications that a patient was taking prior to admission and number of discrepancies was also noted. This is in contrast to the findings reported in the study by Cornish et al.1, which reported no association between number of medications and number of discrepancies observed. This may be because they only compared patients with fewer than eight medications to those with eight or more medications rather than looking at this as a continuous variable. Our findings suggest that if the resources are not available to perform medication reconciliation on all admissions, it may be appropriate to target patients on a higher number of medications.
A potential criticism of this study is that this was not a randomised controlled trial, but it is unlikely that an improvement to this extent would have occurred by chance. It is less clear what the most important components were, and our study design means that we cannot be certain about the relative importance of the different parts of the intervention. A number of different modalities were used. “Real-time” feedback was provided using the sticker. Weekly discussion with junior medical staff reminded staff of the ongoing programme. Posters were displayed throughout the study period. General education sessions where held periodically during the trial. In particular, we believe that the “real-time” feedback was important, because it continued throughout the study and helped illustrate to staff how often important discrepancies can occur. Many prescribers commented that they were surprised by the high discrepancy rate. We suspect that the posters and inserts in the hospital notes may have been less important because of their location and because prescribers may well have become desensitised. Having said this, previous studies suggest that interventions to modify the behaviour of prescribers are more successful when the educational message is delivered in a number of different ways17,20,21. We anticipate that if the benefit of medication reconciliation is to be sustained, we will need to repeat our education campaign at regular intervals.
Our findings suggest that the addition of education and feedback to medication reconciliation in the way that we have described here improves the recording of medicines on admission. The intervention is likely to be particularly useful when there are not enough resources for medication reconciliation to be performed for every admission. We have since adopted this approach in our organisation where we have increased the number of pharmacists who perform medication reconciliation but where we are still not able to perform medication reconciliation on every patient admitted to hospital.
Acknowledgements
Amy Chan was supported by a summer studentship from the Maurice and Phyllis Paykel Trust. The project was funded by the Auckland District Health Board. The results of this study were presented at the meeting of the Australasian Society of Clinical and Experimental Pharmacology in Auckland, New Zealand, on 31 August 2007
We would like to dedicate this study to the late Professor Peter Black who originally formulated the idea of this project. We would like to thank all the medical staff, pharmacists and nurses involved in this project. We are particularly grateful to Paul Gelber, Rob Ticehurst, Lynne Byers (Pharmacy); John Henley, David Spriggs, Matt Dawes (General Medicine); Lisa Noonan (Pharmacology) and to Greg Gamble, Department of Medicine, University of Auckland, for assistance with the statistical analysis.
Conflict of Interest None disclosed.
References
- 1.Cornish PL, Knowles SR, Marchesano R, et al. Unintended medication discrepancies at the time of hospital admission. Arch Intern Med. 2005;165:424–9. doi: 10.1001/archinte.165.4.424. [DOI] [PubMed] [Google Scholar]
- 2.Rozich JD, Resar RK. Medication safety: one organization’s approach to the challenge. J Clin Outcomes Manage. 2001;8:27–34. [Google Scholar]
- 3.Sullivan C, Gleason KM, Rooney D, Groszek JM, Barnard C. Medication reconciliation in the acute care setting: opportunity and challenge for nursing. J Nurs Care Qual. 2005;20:95–8. doi: 10.1097/00001786-200504000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Tam VC, Knowles SR, Cornish PL, Fine N, Marchesano R, Etchells EE. Frequency, type and clinical importance of medication history errors at admission to hospital: a systematic review. CMAJ. 2005;173:510–5. doi: 10.1503/cmaj.045311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Manno MS, Hayes DD. Best-Practice Interventions: How medication reconciliation saves lives. Nursing. 2006;36:63–64. doi: 10.1097/00152193-200603000-00045. [DOI] [PubMed] [Google Scholar]
- 6.Institute for Healthcare Improvement. Overview of the 5 Million Lives Campaign. Available at: http://www.ihi.org/IHI/Programs/Campaign/Campaign.htm?TabId=1. Accessed 14 February, 2010.
- 7.Thompson, C. A. JCAHO views medication reconciliation as adverse-event prevention. Am J Health Syst Pharm. 2005;62:1528,1530,1532. [DOI] [PubMed]
- 8.Boockvar KS, Carlson LaCorte H, Giambanco V, Fridman B, Siu A. Medication reconciliation for reducing drug-discrepancy adverse events. Am J Geriatr Pharmacother. 2006;4:236–43. doi: 10.1016/j.amjopharm.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 9.Collins D, Nickless G, Green C. Medication histories: does anyone know what medicines a patient should be taking? Int J Pharm Pract. 2004;12:173–8. doi: 10.1211/0022357044454. [DOI] [Google Scholar]
- 10.Pronovost P, Weast B, Schwarz M, et al. Medication reconciliation: a practical tool to reduce the risk of medication errors. J Crit Care. 2003;18:201–5. doi: 10.1016/j.jcrc.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 11.Slee A, Farrar K, Hughes D, Constable S. Optimising medical treatment—how pharmacist-acquired medication histories have a positive impact on patient care. Pharmaceut J. 2006;277:737–9. [Google Scholar]
- 12.Budnitz DS, Pollock DA, Weidenbach KN, Mendelsohn AB, Schroeder TJ, Annest JL. National surveillance of emergency department visits for outpatient adverse drug events. JAMA. 2006;296:1858–66. doi: 10.1001/jama.296.15.1858. [DOI] [PubMed] [Google Scholar]
- 13.Donohoo, E., Hoa, V., Jarvis, J., Keen, S., Morgan, E, eds. MIMS New ethicals—Issue 4. Auckland: CMPMedica (NZ) Ltd; 2005.
- 14.Fisher LD, Belle G. Biostatistics: A Methodology for the Health Sciences. New York: John Wiley and Sons; 1993. [Google Scholar]
- 15.Fertleman M, Barnett N, Patel T. Improving medication management for patients: the effect of a pharmacist on post-admission ward rounds. Qual Safe Health Care. 2005;14:207–11. doi: 10.1136/qshc.2004.011759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Varkey P, Cunningham J, O’meara J, et al. Multidisciplinary approach to inpatient medication reconciliation in an academic setting. Am J Health Syst Pharm. 2007;64:1–12. doi: 10.2146/ajhp060314. [DOI] [PubMed] [Google Scholar]
- 17.Schnipper JL, Liang CL, Bhan I, Labonville SA, Broverman CA. Effect of an electronic medication reconciliation application and process redesign on potential adverse drug events: a cluster-randomized trial. Arch Intern Med. 2009;169:771–80. doi: 10.1001/archinternmed.2009.51. [DOI] [PubMed] [Google Scholar]
- 18.Lau HS, Florax C, Porsius AJ, Boer A. The completeness of medication histories in hospital medical records of patients admitted to general internal medicine wards. Br J Clin Pharmacol. 2000;49:597–603. doi: 10.1046/j.1365-2125.2000.00204.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cohen J, Wilson C, Ward F. Improve drug history taking. Pharm Pract. 1998;8:13–6. [Google Scholar]
- 20.Grimshaw JM, Shirran L, Thomas R, et al. Changing provider behavior: an overview of systematic reviews of interventions. Med Care. 2001;39:2–45. doi: 10.1097/00005650-200108002-00002. [DOI] [PubMed] [Google Scholar]
- 21.Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients' care. Lancet. 2003;362:1225–30. doi: 10.1016/S0140-6736(03)14546-1. [DOI] [PubMed] [Google Scholar]