Abstract
BACKGROUND
In response to dramatic increases in obesity prevalence, clinical guidelines urge health care providers to prevent and treat obesity more aggressively.
OBJECTIVE
To describe the proportion of obese primary care patients receiving obesity care over a 5-year period and identify factors predicting receipt of care.
DESIGN
Retrospective cohort study utilizing VHA administrative data from 6 of 21 VA administrative regions.
PATIENTS
Veterans seen in primary care in FY2002 with a body mass index (BMI) ≥30 kg/m2 based on heights and weights recorded in the electronic medical record (EMR), survival through FY2006, and active care (1 or more visits in at least 3 follow-up years FY2003–2006).
MAIN MEASURES
Receipt of outpatient visits for individual or group education or instruction in nutrition, exercise, or weight management; receipt of prescriptions for any FDA-approved medications for weight reduction; and receipt of bariatric surgery.
KEY RESULTS
Of 933,084 (88.6%) of 1,053,228 primary care patients who had recorded heights and weights allowing calculation of BMI, 330,802 (35.5%) met criteria for obesity. Among obese patients who survived and received active care (N = 264,667), 53.5% had a recorded obesity diagnosis, 34.1% received at least one outpatient visit for obesity-related education or counseling, 0.4% received weight-loss medications, and 0.2% had bariatric surgery between FY2002–FY2006. In multivariable analysis, patients older than 65 years (OR = 0.62; 95% CI: 0.60–0.64) were less likely to receive obesity-related education, whereas those prescribed 5–7 or 8 or more medication classes (OR = 1.41; 1.38–1.45; OR = 1.94; 1.88–2.00, respectively) or diagnosed with obesity (OR = 4.0; 3.92–4.08) or diabetes (OR = 2.23; 2.18–2.27) were more likely to receive obesity-related education.
CONCLUSIONS
Substantial numbers of VHA primary care patients did not have sufficient height or weight data recorded to calculate BMI or have recorded obesity diagnoses when warranted. Receipt of obesity education varied by sociodemographic and clinical factors; providers may need to be cognizant of these when engaging patients in treatment.
KEY WORDS: obesity, diagnosis, patient education, health services research, veterans
INTRODUCTION
Obesity is associated with substantial morbidity and is a modifiable risk factor for a variety of chronic illnesses, including several leading causes of death.1 In response to dramatic increases in obesity rates, clinical practice guidelines have urged health care providers to prevent and treat obesity more aggressively.1–6 Most guidelines, however, are based on carefully controlled trials with highly motivated subjects. Little research has documented the extent to which obesity is routinely managed or the types of care that are provided to obese patients in clinical practice. Most previous studies have examined trends in bariatric surgery and anti-obesity medications.7–9 A few studies examining provider diagnosis of obesity and brief physician counseling in the private sector have found suboptimal performance.10,11
Given recent decisions by Medicare and some health care organizations to reimburse for obesity-related treatments and develop obesity-related performance measures, trends and variations in obesity-related practices are increasingly relevant to health care providers.12,13 The Veterans Health Administration (VHA) is an ideal setting to explore such practices because obesity is highly prevalent among VHA patients,14 and the VHA’s electronic medical record (EMR) allows identification of obese patients and the care they receive. Our study’s objectives were to describe, among obese VHA primary care patients, the proportion who received obesity care over a 5-year period and to identify patient-level factors that predict receipt of such care.
METHODS
Data Sources and Population
This retrospective study utilized sociodemographic, diagnostic, anthropometric, mortality, utilization, and pharmacy data from Fiscal Years (FY) 2002–2006 obtained from national VHA administrative and clinical databases including the National Patient Care Database, the Vital Status File, the Corporate Data Warehouse, and the Pharmacy Benefits Management Database.
We first identified patients who received most of their primary care in any of 6 of the VHA’s 21 regionally integrated care networks. The six networks are geographically diverse, representing the Northeast, Southeast, Southwest, Midwest, and Northwest regions of the country, and they reflected the variability of obesity care within the VA during the study period. In 2001–2002 administrative surveys, less than half of VHA medical centers who responded indicated that they provided weight management programs.15 The term “program” was widely interpreted and ranged from simple dietary referrals to more intensive, multidisciplinary programs. Fewer than half of VHA medical centers provided such programs in 2001–2002.15
Identification of Obese Cohort
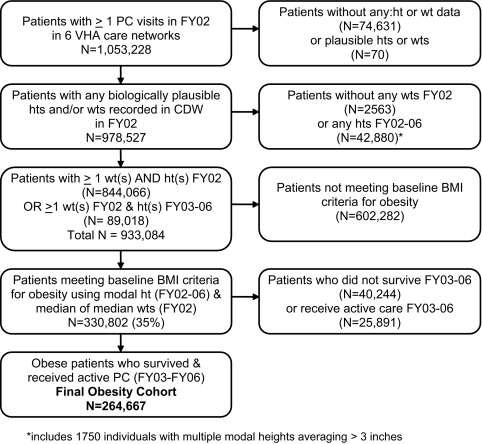
To identify our cohort, we used BMI derived from heights and weights obtained during routine clinical encounters and recorded in the EMR. The data are stored in facility information systems and uploaded into the Corporate Data Warehouse; validation work indicates that this database contains some height and weight values that reflect probable data entry errors.16 Therefore, we used an iterative process to eliminate or control for height and weight outliers while avoiding suspect BMI values. First, we removed biologically “implausible” values (i.e., weights ≤70 lbs or ≥700 lbs, and heights ≤48 inches or ≥84 inches).14 We divided the baseline year (FY2002) into quarters and determined the median weight (if available) for each quarter for every patient. Because heights are recorded less frequently than weights, we took the modal height for each patient among all heights recorded in FY2002–FY2006. When multiple modes were present, we averaged the modes if the difference between them was 3 or fewer inches. We defined the baseline BMI by using the median of the quarterly median weights for FY2002 and the modal height from FY2002–FY2006. Inclusion criteria were: one or more primary care visits in FY2002; BMI ≥30 mg/k2; survival through FY2006; and active care, defined as 1 or more visits in at least 3 of the 4 follow-up years (FY2003–FY2006; Fig. 1).
Figure 1.
Flowsheet of inclusion and exclusion criteria for obesity cohort. Asterisk denotes PC: primary care; VHA: Veterans Health Administration; ht: height; wt.: weight; CDW: Corporate Data Warehouse; FY: fiscal year.
Sociodemographic and Clinical Characteristics
Sociodemographic data included age, sex, ethnicity, and marital status. Data obtained from VHA administrative databases are generally accurate and complete. Race/ethnicity is the exception; rates of missing data have been high since 2003 due to a change in its manner of collection.17,18 We also collected VHA priority status, which consists of nine categories related to disability and income.19 We grouped patients as follows: patients with 50% or more service-connected disability and no co-payment requirement; patients with co-payment requirements for medications, and patients with co-payment requirements both for medical care and medications.
We also included distance from patients’ homes to their primary source of VA care as an indicator of geographic barrier to obesity care. Patients’ ZIP codes were obtained from their most frequently reported residence over the study period, while their facility’s ZIP code was based on their most frequently used health facility. Distance was calculated as the straight line distance between the patient and facility ZIP code centroids using the latitude and longitude coordinates for each.20,21
We assigned patients to obesity class I (30–34 kg/m2), II (35–39 kg/m2), or III (≥40 kg/m2) according to their baseline BMI. We used outpatient and inpatient ICD-9-CM codes21–25 from FY2002–FY2006 to assess the presence or absence of ten comorbidities that might enhance the probability of receiving treatment for obesity-related care, and seven psychiatric conditions that might pose barriers to obesity care (Table 1). We also included an indicator variable for cancer (excluding skin cancer). Although obesity is a risk factor for some cancers, patients with active cancer may not be suitable candidates for weight management treatment. To control for the overall chronic illness burden, we counted the number of medication classes used by each patient.26
Table 1.
Sociodemographic and Clinical Characteristics (N = 264,667)
| Male, N (%) | 249,589 (94.3) |
| Age in years, mean (SD) | 60.8 (12.2) |
| 55 years or younger, N (%) | 94,902 (35.9) |
| 56–65 years, N (%) | 64,060 (24.2) |
| 66–75 years, N (%) | 73,848 (27.9) |
| 76 years & older, N (%) | 31,857 (12.0) |
| Ethnicity | |
| White, N (%) | 171,385 (64.8) |
| African American, N (%) | 21,491 (8.1) |
| Hispanic, N (%) | 19,547 (7.4) |
| Other, N (%) | 2,090 (0.8) |
| Unknown, N (%) | 50,154 (19.0) |
| Married, N (%) | 173,182 (65.4) |
| Distance from most frequently used facility ≥30 miles, N (%)* | 100,304 (37.9) |
| Priority status | |
| 50% or more disability and no co-pays, N (%) | 61,051 (23.1) |
| Co-pays for pharmacy only, N (%) | 127,062 (48.0) |
| Co-pays for medical care and pharmacy, N (%) | 76,554 (28.9) |
| Number of obesity-related medical comorbidities FY2002–2006, mean (SD) | 4.0 (1.7) |
| Diagnosis of: | |
| Diabetes, N (%) | 120,189 (45.4) |
| Hypertension, N (%) | 221,903 (83.8) |
| Hyperlipidemia, N (%) | 206,474 (78.0) |
| Ischemic heart disease, N (%) | 106,569 (40.3) |
| Congestive heart failure, N (%) | 34,004 (12.9) |
| Cholelithiasis, N (%) | 6,151 (2.3) |
| Osteoarthritis, N (%) | 117,367 (44.4) |
| Low back pain, N (%) | 107,524 (40.6) |
| Gastroesophageal reflux disease, N (%) | 87,836 (33.2) |
| Obstructive sleep apnea, N (%) | 37,857 (14.3) |
| Cancer (excluding skin cancer), N (%) | 37,205 (14.1) |
| Number of psychiatric comorbidities FY2002–2006, mean (SD) | 0.9 (1.2) |
| Diagnosis of: | |
| Alcohol use disorder, N (%) | 23,191 (8.8) |
| Substance use disorder, N (%) | 10,126 (3.8) |
| Tobacco dependence, N (%) | 51,044 (19.3) |
| Depression, N (%) | 72,035 (27.2) |
| Post-traumatic stress disorder, N (%) | 30,631 (11.6) |
| Dementia, N (%) | 15,919 (6.0) |
| Serious mental illness, N (%) | 22,821 (8.6) |
| Number of medication classes FY2002–2006, mean (SD) | 5.8 (2.2) |
| 0–4, N (%) | 77,930 (29.4) |
| 5–7, N (%) | 123,470 (46.7) |
| 8 or more, N (%) | 63,267 (23.9) |
Obesity Care Practices
Using ICD-9-CM codes, we determined whether patients had received a clinician-assigned diagnosis of obesity: (1) in FY2002 and (2) at anytime during FY2002–2006. We also constructed a “monitoring” variable indicating whether patients had a weight recorded in each of the years (FY2003–2006) they received active care. We identified obesity-related counseling and education by two methods: (1) clinic stop codes, a categorization scheme used by VHA to classify the type of clinic in which each outpatient visit occurred, and (2) Healthcare Common Procedure Coding System (HCPCS) Level II codes, a uniform coding system maintained by the American Medical Association and Centers for Medicare and Medicaid Services,27 which is also used by the VHA to identify outpatient medical services and procedures. We included any codes related to visits at obesity-related clinics and/or visits for which obesity-related services were provided (e.g., education or counseling about weight control, nutrition counseling, or physical fitness/exercise). Because attendance at a single session of a comprehensive weight management class might be coded with both a clinic stop code and a HCPCS Level II code, only one obesity-related service or visit was counted per day. We then created the following variables to indicate the type and amount of obesity treatments received in FY2002–FY2006: (1) number of outpatient visits for individual or group education or instruction in nutrition, exercise, or weight management; (2) number of days prescribed any FDA-approved medications for weight reduction (e.g., sibutramine or orlistat); and (3) bariatric surgery, as determined from ICD-9A procedure codes from inpatient data and Current Procedural Terminology codes from outpatient data.
Analysis
We characterized cohort members and their obesity care by using descriptive statistics. Chi-square tests examined bivariate associations of baseline BMI class with receipt of obesity diagnosis and with receipt of obesity treatment. Two separate multivariable logistic regressions evaluated the influence of patient-level predictors on the likelihood of receiving a diagnosis of obesity and of receiving obesity education any time during FY2002–FY2006. Due to the high rate of missing ethnicity/race data, we conducted sensitivity analyses that determined that model results were similar whether those with missing data were included or race/ethnicity variables were included, and so we dropped race/ethnicity variables. Analyses were conducted using SAS version 9.2.20
RESULTS
Sociodemographic and Clinical Characteristics
Among 1,053,228 patients with one or more primary care visits in FY2002 in any of the six networks, 933,084 (88.6%) had at least one plausible weight and height recorded in FY2002 (N = 844,066; 80.1%), or at least one weight recorded in FY2002 and a height recorded during FY2003–FY2006 (N = 89,018, 8.5%; Fig. 1). Of these, 330,802 (35.5%) met BMI criteria for obesity. Among obese patients, 66,135 (19.9%) died or did not meet criteria for receiving active care in FY2003–2006, leaving a final cohort of 264,667 patients.
Most patients were male (249,589; 94.3%; Table 1). Their mean (SD) age was 60.8 (12.2) years; 105,705 (39.9%) were over age 65. Approximately 16% were racial/ethnic minorities, and for another 19%, race/ethnicity was not recorded. Most obese patients (164,264, 62.1%) lived within 30 miles of their most frequently used VA facility. Patients had on average 4.0 (1.7) of 10 possible obesity-related medical comorbidities and were prescribed an average of 5.8 (2.2) medications from different medication classes, suggesting a considerable burden of illness. Hypertension was the most frequently diagnosed medical comorbidity (83.8%), followed by hyperlipidemia (78%) and diabetes (45.4%). Patients also averaged 0.9 of 7 psychiatric comorbidities, most commonly depression (27.2%).
Body Mass Index and Recording of Obesity Diagnosis
The cohort’s mean (SD) baseline BMI was 34.5 (4.4) kg/m2. Among these patients, 67% had Class I, 23% had Class II, and 10% had Class III obesity (Table 2). Only 28%, however, had a clinician-recorded obesity diagnosis in FY2002. Furthermore, only 54% received a diagnosis of obesity during FY2002–FY2006. Patients with Class III obesity were significantly more likely to be diagnosed with obesity (87%), compared with those with Class II (68%) or Class I obesity (43%; p < 0.0001).
Table 2.
Baseline Body Mass Index and Obesity Care Practices Received (N = 264,667)
| Mean (SD) baseline BMI, kg/m2 | 34.5 (4.4) |
| Baseline BMI class | |
| Class I (BMI 30–34 kg/m2), N (%) | 175,977 (66.5) |
| Class II (BMI 35–39 kg/m2), N (%) | 61,399 (23.2) |
| Class III (BMI ≥40 kg/m2), N (%) | 27,291 (10.3) |
| Obesity diagnosis in FY2002, N (%) | 73,285 (27.7) |
| Obesity diagnosis in FY2002–2006, N (%) | 141,533 (53.5) |
| Weight monitored in FY2003–FY2006, N (%)a | 215,691 (81.5) |
| Visits for outpatient education or instruction in nutrition, exercise, or weight management in FY2002–FY2006 | |
| 0, N (%) | 174,428 (65.9) |
| 1, N (%) | 40,517 (15.3) |
| 2–5, N (%) | 37,172 (14.0) |
| 6 or more, N (%) | 12,550 (4.7) |
| Mean (SD) outpatient visits with education or instruction in nutrition, exercise, or weight management in FY2002–FY2006 (for those who had 1 or more visits) | 4.2 (17.9) |
| Prescribed weight loss medication in FY2002–FY2006, N(%) | 1,059 (0.4) |
| Mean (SD) number of days weight loss medication(s) prescribed | 271.5 (313.9) |
| Underwent bariatric surgery in FY2002–2006, N (%) | 407 (0.2) |
| Received any obesity treatment in FY2002–FY2006, N (%) | 90,546 (34.2) |
BMI: body mass index; FY: fiscal year
aHad to have at least one weight recorded in the same year that the patient received active care (at least 3 of 4 years in FY2003–FY2006)
Obesity Monitoring and Treatments
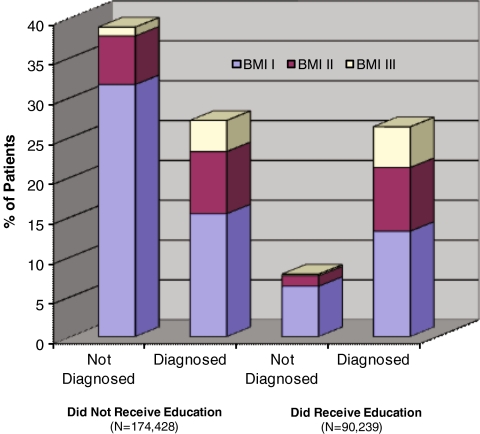
A total of 215,691 (81.5%) obese patients had one or more weights documented in the EMR every year they received active care. Only 34% received individual or group outpatient education or counseling in nutrition, exercise, or weight management between FY2002–FY2006. Patients receiving such instruction averaged 4.2 (17.9) visits, but almost half had only 1 visit. Only 1,059 (0.4%) received any weight loss medication, and 407 (0.2%) had bariatric surgery. Of the 90,239 patients who received obesity-related counseling, 51,605 (57.2%), 24,658 (27.3%), and 13,976 (15.5%) had Class 1, II, and III obesity, respectively, whereas 69,656 (77.2%) had a recorded diagnosis of obesity (Fig. 2).
Figure 2.
Proportion of obese patients with vs. without obesity diagnosis who did vs. did not receive obesity education by body mass index class (N = 264,667). BMI: body mass index.
Multivariable Analyses
In multivariable analyses (Table 3), the relative odds of being diagnosed with obesity were 6.68 [95% confidence interval (CI): 6.44, 6.94] and 2.52 (95% CI: 2.47, 2.57), respectively, in patients with Class III and Class II obesity compared with Class I obesity. Among the other medical and psychiatric diagnoses, sleep apnea (OR = 1.59; 95% CI: 1.55, 1.64) was most likely to be associated with an obesity diagnosis. The relative odds of receiving a diagnosis of obesity were lower for males (OR = 0.71; 95% CI: 0.69, 0.74) compared with females, and for patients 66–75 years old (OR = 0.74; 95% CI: 0.72, 0.77) and 76 or older (OR = 0.52; 95% CI: 0.51, 0.54) compared with patients age 55 or younger.
Table 3.
Factors Associated with Receipt of Obesity Diagnosis and Obesity-Related Education (N = 264,568)
| Obesity diagnosis (OR 95% CI) | Obesity education OR (95% CI) | |
|---|---|---|
| Male (vs. female) | 0.71 (0.69–0.74) | 0.93 (0.89–0.96) |
| Age (vs. 55 years or younger) | ||
| 56–65 years | 0.98 (0.96–1.00) | 0.87 (0.85–0.89) |
| 66–75 years | 0.74 (0.72–0.76) | 0.62 (0.60–0.64) |
| 76 years or older | 0.52 (0.51–0.54) | 0.50 (0.49–0.52) |
| Married (vs. not married) | 0.96 (0.94–0.98) | 0.86 (0.85–0.88) |
| Distance from most frequently used facility >30 miles (vs. ≤30 miles) | 1.12 (1.10–1.14) | 1.06 (1.04–1.08) |
| Priority status (vs. co-pays required for medical care and pharmacy) | ||
| 50% or more disability and no co-pays required | 1.00 (0.98–1.03) | 1.26 (1.22–1.29) |
| Co-pays required for pharmacy only | 1.14 (1.12–1.17) | 1.15 (1.12–1.17) |
| Medication class count (vs. 0–4 classes) | ||
| 5–7 medication classes | 1.08 (1.06–1.10) | 1.41 (1.38–1.45) |
| 8 or more medication classes | 1.27 (1.24–1.30) | 1.94 (1.88–2.00) |
| Baseline BMI (vs. Class I) | ||
| Class II | 2.52 (2.47–2.57) | 0.98 (0.96–1.00) |
| Class III | 6.68 (6.44–6.94) | 1.02 (0.99–1.06) |
| Diagnosis of: | ||
| Obesity | NA | 4.00 (3.92–4.08) |
| Diabetes | 1.33 (1.31–1.35) | 2.23 (2.18–2.27) |
| Hypertension | 1.30 (1.27–1.33) | 1.03 (1.00–1.05) |
| Hyperlipidemia | 1.37 (1.35–1.40) | 1.47 (1.43–1.50) |
| Ischemic heart disease | 0.88 (0.86–0.90) | 1.04 (1.02–1.06) |
| Congestive heart failure | 1.05 (1.02–1.08) | 1.10 (1.07–1.13) |
| Cholelithiasis | 1.24 (1.17–1.31) | 1.18 (1.12–1.25) |
| Osteoarthritis | 1.17 (1.15–1.19) | 1.11 (1.10–1.15) |
| Low back pain | 1.10 (1.08–1.12) | 1.12 (1.10–1.15) |
| Gastroesophageal reflux disease | 1.04 (1.02–1.05) | 1.01 (0.99–1.03) |
| Obstructive sleep apnea | 1.59 (1.55–1.64) | 1.29 (1.26–1.32) |
| Cancer (non-skin) | 1.36 (1.33–1.39) | 1.02 (0.99–1.05) |
| Alcohol use disorder | 1.08 (1.04–1.11) | 1.06 (1.02–1.09) |
| Substance use disorder | 0.78 (0.74–0.82) | 1.44 (1.37–1.51) |
| Tobacco dependence | 1.15 (1.13–1.18) | 0.95 (0.93–0.97) |
| Depression | 1.06 (1.04–1.09) | 1.06 (1.04–1.09) |
| Post-traumatic stress disorder | 0.99 (0.96–1.02) | 1.13 (1.10–1.17) |
| Dementia | 1.03 (0.99–1.07) | 1.14 (1.09–1.18) |
| Serious mental illness | 1.20 (1.16–1.24) | 1.10 (1.06–1.14) |
OR: odds ratio; BMI: body mass index; NA: not applicable
*Individual or group outpatient instruction or counseling for nutrition, exercise, or weight management
In multivariable analyses, clinician-diagnosed obesity was the strongest predictor for receiving obesity-related education (OR = 4.0; 95% CI: 3.92, 4.08), followed by diagnoses of diabetes (OR = 2.23; 95% CI: 2.18, 2.27) and hyperlipidemia (OR = 1.50; 95% CI: 1.46,1.53; Table 3). Patients prescribed 8 or more types of medication and patients prescribed 5–7 types of medication had a 1.94 and 1.41 greater odds of receiving obesity-related instruction, respectively, than were those prescribed 4 or fewer. The odds of receiving obesity-related education decreased with increasing age. Weak or null effects were noted for all of the other variables.
DISCUSSION
Despite the burgeoning epidemic of obesity in the VHA and the potential benefits of treating obesity, our findings indicate suboptimal rates of obesity care among our cohort of obese primary care patients. In FY2002 alone, 20% of primary care patients did not have sufficient height or weight data to calculate their BMI, and 72% of obese primary care patients did not have obesity diagnoses recorded when warranted. The rates we found in the VHA, however, are comparable or better than those recently reported in the private sector.28,29 The relatively higher rates of weight and height documentation within the VHA may be due to its EMR. Nevertheless, our findings suggest that a critical missing link occurs between the automatic calculation of BMI that occurs within the VHA’s EMR, if a height and weight are entered, and clinicians’ formal recognition and diagnosis of an obesity disorder. We found that an obesity diagnosis, and not BMI per se, was the strongest predictor of receiving obesity-related education. These findings suggest that a diagnosis of obesity may serve as a “marker” to reflect level of provider concern and/or patient interest in seeking obesity treatment, a finding consistent with previous reports that brief physician counseling for obesity occurs more frequently for obese patients who have an obesity diagnosis recorded.11
Periodic documentation of heights and weights is recommended for identifying obese patients and monitoring obesity’s course or response to treatment.1–6 Failure to record obesity diagnoses, heights, and weights could be caused by a number of factors, including perceptions of importance, time constraints, and competing clinical demands.10,11,30 Their omission from the medical record has implications for health services research and quality monitoring. Recent plans by health care institutions such as the VHA and National Committee for Quality Assurance to implement performance measures to assess how consistently physicians calculate BMI may improve documentation rates in the future.13,31,32 During the time period covered by this study, few VHA facilities had implemented clinical reminders that automatically prompt clinicians to record a diagnosis of obesity after a BMI is generated in the EMR, and there was no performance measure requiring screening for obesity; however, beginning in 2006 the VHA issued policies and provided facilities with tools to systematically identify obese patients and offer them treatment through the MOVE! Weight Management Program for Veterans.15
Our data indicate that only about 10–13% of obese veterans received individual or group outpatient education in nutrition, exercise, or weight management on an annual basis, and only about one-third received any obesity-related education over the 5-year study period. Obese patients who were older than 65 years, prescribed fewer types of medications, or lacking an EMR diagnosis of obesity or diabetes were less likely to have outpatient obesity-related education. We cannot determine whether this was due to patient preference or other factors, but our findings suggest that providers may need to be especially vigilant in offering obesity-related education and engaging such patients in treatment if they would benefit from treatment.
We also found limited utilization of weight loss medications and of bariatric surgery, which may be partially due to system barriers. National policies in place during the study period allowed VHA facilities to make anti-obesity medications available to eligible patients who met criteria for use through non-formulary drug requests, but despite this, facilities have varied widely in their use.31 The adverse effect profile of these medications, however, also makes them a poor choice for many veterans, who tend to be older and sicker than the population in which the medications were tested and approved. Compared with national rates reported for the general population (24 per 100,000 adults) in 2002,8 the bariatric surgery rates we found also appear lower (407 in FY2002–FY2006 and just 68 in FY2002 alone for our cohort). With only 12 approved VHA bariatric centers nationwide, however, access was limited.
Disease burden among these patients was great, especially considering that the final cohort excluded more than 40,000 obese patients who died during the 5-year study period. Patients were more likely to receive obesity-related instruction as their number of prescribed medication classes increased, suggesting that patients are less likely to receive counseling or education when their burden of illness is low. Obesity-related comorbidities were common and included those explicitly recommended by guidelines to trigger considering obesity treatment.1 A diagnosis of diabetes conferred the highest probability of receiving obesity-related education. Although psychiatric comorbidities were highly prevalent in our obesity cohort, they did not appear to pose a barrier to obesity education.
Controlling for other factors, obese males were less likely to be diagnosed with obesity than were obese females. In addition, older patients, especially those over 65, were considerably less likely to receive a diagnosis of obesity or obesity-related education. This may reflect uncertainty on the part of clinicians in identifying and treating obesity in older adults in whom the relationship between BMI and health risks is less clear and weight management goals may differ from younger adults. Because of the large number of patients with unknown ethnicity, we were not able to include this important factor in the multivariable analyses. Distance of home residence from most frequently used VA facility did not significantly impact access to obesity care.
Limitations
Limitations of this retrospective cohort study include its reliance on administrative height and weight data, which likely contain data entry errors.16 Although we may have misclassified some patients as obese/not obese, we believe that the approach used to control for outliers and define the cohort was conservative. Furthermore, it is clear that we identified more obese patients using heights and weights than would have been identified by relying on ICD-9-CM codes for obesity. Because clinicians’ notes are not captured in the VHA’s national administrative data, we were not able to identify any instances of brief physician counseling that may have occurred during routine visits. Other studies, however, using chart reviews suggest that obesity counseling by physicians is provided to only a minority of patients.11 Furthermore, although brief physician counseling may increase motivation to lose weight and result in greater weight loss in some patients, systematic reviews indicate that most obese patients require moderate-intensity counseling (defined as more than 1 visit per month for the first 3 months) to successfully lose weight and maintain weight loss.6 When we looked for this level of intensity in our cohort, we found only 1.6% received it, a negligible proportion. We were also unable to determine from our administrative data if additional patients may have been referred for obesity counseling, but failed to attend, or to ascertain patients’ level of motivation, which clearly plays an important role in determining whether patients receive treatment for obesity.
Although not representative of the entire VHA, our cohort was identified from a population of 1.5 million primary care patients served by six geographically diverse care networks, representing about 20% of the VHA’s 5.4 million patients. Large health care systems such as the VHA may be more likely to have dietitians, exercise counselors, or behavior specialists, and subspecialty clinicians to provide a comprehensive range of treatment options for obesity, but smaller clinics and independent providers can refer patients to specialists and community-based programs, or utilize an increasing array of Internet- and web-based options. In any case, the current study provides valuable information about the different types and amount of obesity care provided in routine clinical practice to a population of mostly male obese primary care patients, finding that the receipt of such care varied by patients’ sociodemographic and clinical factors. Future analyses will examine the influence of system-level factors on receipt of obesity care, including facility-level variability in the implementation of MOVE!, the VHA’s nationwide program for managing obesity.15
Acknowledgements
The research reported here was supported by the Department of Veteran Affairs, Veterans Health Administration, Health Services Research and Development Service (project no. IIR 05–121). Dr. Noël is a Research Psychologist at the South Texas Veterans Health Care System. The views expressed in this article are those of the author(s) and do not necessarily represent the views of the Department of Veterans Affairs.
Conflict of Interest The research reported here was supported by the Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service (project no. IIR 05–121). The funding agency provided support to conduct this study, including collection, management, analysis, and interpretation of the data, and preparation of the manuscript, but has not participated in manuscript development, and has not reviewed or approved this manuscript.The authors have no conflict of interests to declare. Sources of support for the authors for the past 3 years are listed below:Dept. of Veterans Affairs: Noël, Copeland, Pugh, Kahwati, Tsevat, Nelson, Wang, BollingerUT Health Science Center: Noël, Copeland, Pugh, Hazuda, WangUniversity of Cincinnati: TsevatUniversity of Washington: NelsonNIH: Noël, Copeland, Pugh, Wang, Nelson, TsevatCDC: PughEpilepsy Foundation: PughAbbott Laboratories: Pugh
Footnotes
The research reported here was supported by the Department of Veteran Affairs, Veterans Health Administration, Health Services Research and Development Service (project no. IIR 05–121). Dr. Noël is a Research Psychologist at the South Texas Veterans Health Care System. The views expressed in this article are those of the author(s) and do not necessarily represent the views of the Department of Veterans Affairs.
References
- 1.Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. Washington: National Institutes of Health; 1998. [PubMed] [Google Scholar]
- 2.National Task Force on the Prevention and Treatment of Obesity Overweight, obesity, and health risk. Arch Intern Med. 2000;160:898–904. doi: 10.1001/archinte.160.7.898. [DOI] [PubMed] [Google Scholar]
- 3.Nawaz H, Katz DL. American College of Preventive Medicine Practice policy statement. Weight management counseling of overweight adults. Am J Prev Med. 2001;21:73–8. doi: 10.1016/S0749-3797(01)00317-8. [DOI] [PubMed] [Google Scholar]
- 4.Lyznicki JM, Young DC, Riggs JA, Davis RM. Council on Scientific Affairs American Medical Association. Obesity: assessment and management in primary care. Am Fam Physician. 2001;63:2185–96. [PubMed] [Google Scholar]
- 5.National Task Force on the Prevention and Treatment of Obesity Medical care for obese patients: advice for health care professionals. Am Fam Physician. 2002;65:81–8. [PubMed] [Google Scholar]
- 6.McTigue KM, Harris R, Hemphill B, et al. Screening and interventions for obesity in adults: summary of the evidence for the US Preventive Services Task Force. Ann Intern Med. 2003;139:933–49. doi: 10.7326/0003-4819-139-11-200312020-00013. [DOI] [PubMed] [Google Scholar]
- 7.Mehrotra C, Serdula M, Naimi TS, Khan LK, Miller J, Dietz W. Population-based study of trends, costs, and complications of weight loss surgeries from 1990–2002. Obes Res. 2005;13(11):2029–34. doi: 10.1038/oby.2005.249. [DOI] [PubMed] [Google Scholar]
- 8.Davis MM, Slish K, Chao C, Cabana MD. National trends in bariatric surgery, 1996–2002. Arch Surg. 2006;141(1):71–4. doi: 10.1001/archsurg.141.1.71. [DOI] [PubMed] [Google Scholar]
- 9.Stafford RS, Radley DC. National trends in antiobesity medication use. Arch Intern Med. 2003;169(9):1046–50. doi: 10.1001/archinte.163.9.1046. [DOI] [PubMed] [Google Scholar]
- 10.Stafford RS, Farhat JH, Misra B, Schoenfeld DA. National patterns of physician activities related to obesity management. Arch Fam Med. 2000;9:631–8. doi: 10.1001/archfami.9.7.631. [DOI] [PubMed] [Google Scholar]
- 11.McAlpine DD, Wilson AR. Trends in obesity-related counseling in primary care: 1995–2004. Med Care. 2007;45:322–9. doi: 10.1097/01.mlr.0000254575.19543.01. [DOI] [PubMed] [Google Scholar]
- 12.United States. Department of Health and Human Services. HSS announces revised Medicare obesity coverage policy. News Release. Available from: URL: http://www.hhs.gov/news/press/2004pres/20040715.html. Accessed January 20, 2010.
- 13.National Committee for Quality Assurance. Proposed new measures for HEDIS 2009: Body Mass Index (BMI) Assessment (BAA) BMI Percentile Assessment and Counseling for Nutrition and Physical Activity (BCA). 2008; NCQA.
- 14.Das SR, Kinsinger LS, Yancy WS, Jr, Wang A, Ciesco E, Burdick M, et al. Obesity prevalence among veterans at Veterans Affairs medical facilities. Am J Prev Med. 2005;28:291–4. doi: 10.1016/j.amepre.2004.12.007. [DOI] [PubMed] [Google Scholar]
- 15.Kinsinger LK, Jones KR, Kahwati LK, Harvey R, Burdick M, Zele V, Yevich SJ. Design and dissemination of the MOVE! weight management program for veterans. Prev Chron Dis. 2009;6(3):1–6. [PMC free article] [PubMed] [Google Scholar]
- 16.Perrin R, Bates J, Noel PH, Copeland LA, Lancaster B. National Clinical Data for VA Research: the VA Corporate Data Warehouse. Workshop. February, 2008 National HSR&D Meeting, Baltimore, MD.
- 17.Sohn MW, Zhang H, Arnold N, Stroupe K, Taylor BC, Wilt TJ, Hynes DM. Transition to the new race/ethnicity data collection standards in the Department of Veterans Affairs. Popul Health Metr. 2006;4:7. doi: 10.1186/1478-7954-4-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Long JA, Bamba MI, Linq B, Shea JA. Missing race/ethnicity data in Veterans Health Administration based disparities research: a systematic review. J Health Care Poor Underserved. 2006;17(1):128–40. doi: 10.1353/hpu.2006.0029. [DOI] [PubMed] [Google Scholar]
- 19.Gao J, Wang Y, Engelhardt J. Logistic analysis of veterans’ eligibility-status changes. Health Serv Manag Res. 2005;18:175–85. doi: 10.1258/0951484054572493. [DOI] [PubMed] [Google Scholar]
- 20.U.S. Census Bureau. (2000). Population and housing profile, US census STF1. Generated from http://factfinder.census.gov/servlet/DTGeoSearchByListServlet?ds_name=DEC_2000_SF1_U&_lang=en&_ts=272882185413. Accessed October 6, 2009.
- 21.SAS Insitute Inc., SAS 9.2, Cary, NC: SAS Institute Inc., 2008.
- 22.World Health Organization. International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). American Medical Association Press, 2006}. [PubMed]
- 23.Kerr EA, Hofer TP, Hayward RA, Adams JL, Hogan MM, McGlynn EA, Asch SM. Quality by any other name?: A comparison of three profiling systems for assessing health care quality. Health Serv Res. 2007;42(5):2070–87. doi: 10.1111/j.1475-6773.2007.00730.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cornell J, Pugh JA, Williams JW, Jr, Kazis L, Lee A, Parchman M, Zeber J, Pederson T, Montgomery KA, Noël PH. Multimorbidity clusters: clustering binary data from a large administrative medical database. Applied Multivariate Research. 2008;12(3):163–82. [Google Scholar]
- 25.Zeber JE, Copeland LA, Amuan M, Cramer JA, Pugh MJV. The role of comorbid psychiatric conditions in health status in epilepsy. Epilepsy & Behavior. 2007;10:539–546. doi: 10.1016/j.yebeh.2007.02.008. [DOI] [PubMed] [Google Scholar]
- 26.Schneeweiss S, Seeger JD, Maclure M, Wang PS, Avorn J, Glynn RJ. Performance of comorbidity scores to control for confounding in epidemiologic studies using claims data. Am J Epidemiol. 2001;154(9):854–64. doi: 10.1093/aje/154.9.854. [DOI] [PubMed] [Google Scholar]
- 27.Buck CJ. Saunders 2008 ICD-9-CM, Volumes 1, 2, and 3, HCPCS Level II and CPT Professional Edition Package. 2007. St. Louis, Mo. Saunders.
- 28.Ma J, Xiao L, Stafford RS. Underdiagnosis of obesity in adults in US outpatient settings. Arch Intern Med. 2009;169(3):313–4. doi: 10.1001/archinternmed.2008.582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ma J, Xiao L, Stafford RS. Adult obesty and office-based quality of care in the United States. Obesity (Silver Spring) 2009 Feb 5. [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 30.Ruelaz AR, Diefenbach P, Simon B, Lanto A, Arterburn D, Shekelle PG. Perceived barriers to weight management in primary care-perspectives of patients and providers. JGIM. 2007;22:518–22. doi: 10.1007/s11606-007-0125-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Personal Communication. Leila C. Kahwati, MD MPH, VHA Deputy Chief Consultant for Preventive Medicine, summarizing findings from the MOVE! Weight Management Program for Veterans, Special Evaluation Report: Clinical Effectiveness, 2009.
- 32.National Committee for Quality Assurance. Proposed new measures for HEDIS 2009: Body Mass Index (BMI) Assessment (BAA) BMI Percentile Assessment and Counseling for Nutrition and Physical Activity (BCA). 2008; NCQA.