Abstract
BACKGROUND
Latino immigrants face a higher burden of colorectal cancer (CRC) and screening rates are low.
OBJECTIVE
To assess the effectiveness of a multilevel intervention in increasing the rate of CRC screening among Latino immigrants.
DESIGN
A randomized controlled trial, with randomization at the physician level.
PARTICIPANTS
Pairs of 65 primary care physicians and 65 Latino immigrant patients participated, 31 in the intervention and 34 in the control group.
INTERVENTION
CRC educational video in Spanish on a portable personal digital video display device accompanied by a brochure with key information for the patient, and a patient-delivered paper-based reminder for their physician.
MEASUREMENTS
Completed CRC screening, physician recommendation for CRC screening, and patient adherence to physician recommended CRC screening.
RESULTS
The overall rate of completed screening for CRC was 55% for the intervention and 18% for the control group (p = 0.002). Physicians recommended CRC screening for 61% of patients in the intervention group versus 41% in the control group (p = 0.08). Of those that received a recommendation, 90% in the intervention group adhered to it versus 26% in the control group (p = 0.007).
CONCLUSIONS
The intervention was successful in increasing rates of completed CRC screening primarily through increasing adherence after screening was recommended. Additional efforts should focus on developing new strategies to increase physician recommendation for CRC screening, while employing effective patient adherence interventions.
KEY WORDS: colorectal cancer, immigrant health, primary care, prevention, intervention
INTRODUCTION
Colorectal cancer (CRC) is the second most common cancer in the U.S.1,2 Latinos in the U.S. are more likely to be diagnosed with advanced stage CRC, have a lower survival probability, and lower CRC screening rates(29%) than the general population.1–3 Among eligible foreign-born U.S. Latinos, only 22% are screened for CRC with any of the recommended tests1.
One of the most important factors influencing CRC screening rates is clinician recommendation4,5. Interventions that target more than one level (patients, providers) often are more effective in increasing cancer screening.6 Guerra et al. found that physician recommendation is a powerful motivator for CRC screening in Latinos regardless of literacy level, and suggest that interventions to increase provider CRC screening recommendations may increase screening rates.7
This study tested the effectiveness of a culturally and linguistically sensitive, multi-level intervention to improve CRC screening rates in an urban, Latino immigrant population.
METHODS
Study Design and Setting
We conducted a randomized controlled trial in the primary care clinic of a large New York City teaching hospital caring for a large, diverse, underserved population.
Population and Randomization
Primary care physicians consented to study participation by signing a written consent, and completed a brief demographic questionnaire. We recruited attending/staff physicians two months prior to starting patient recruitment, and recruited rotating medicine residents during the first week of their ambulatory care rotation. To limit confounding by physician characteristics, we randomly allocated physicians to the intervention or control group within strata defined by physician gender, role (resident or attending), Spanish proficiency and place of birth. Randomization was performed by computer before patient recruitment.
From September 2006 to May 2007, a trained research assistant approached patients in the primary care clinic waiting area prior to their physician visit to assess study eligibility. All Latino immigrant Spanish-speaking patients, 50 years or older, who used the primary care facility as their regular source of care for at least the previous two years were asked to participate. We excluded patients current with CRC screening, those with gastrointestinal symptoms, a personal history of cancer, a family history of CRC, patients who had a visit with a physician with a patient already in the study , and those who did not consent to participate.
We recruited patients during the last two weeks of each month to minimize the possibility that the consent process would have an activating effect on the control group physicians. Patients were blind to their physician’s randomization. Patients of physicians randomly assigned to the intervention group received the intervention, while patients of physicians in the control group received usual care.
Intervention
Research assistants showed intervention patients a Spanish-language CRC educational video on a portable personal digital video device while they waited for their visits. The 11-minute video was developed by the National Alliance for Hispanic Health with CDC funding, through a needs assessment process with nationwide partnering community sites. The video was then evaluated through pre-post surveys and focus groups. It includes education about CRC screening modalities, prevention, and risk factors. The video was accompanied by a brochure in Spanish with key information from the video. Intervention patients were also given a one-page reminder to hand to their physicians notifying them of 1) their patients’ eligibility for CRC screening, and 2) their patients’ receipt of CRC education.
Outcome Assessment
A research assistant, not involved in patient recruitment and blind to the randomization assignment, reviewed electronic medical records 3 months after the index visit to determine the primary outcome, CRC screening completion, and the secondary outcomes, physician recommendation of any CRC screening test recommended in the guidelines and patient adherence to physician CRC screening recommendation.
Statistical Analysis
All analyses were performed using the intention to treat principle comparing patient screening outcomes among those seen by physicians randomized to the intervention versus control groups (using the patient as the unit of analysis). To compare physician and patient characteristics between the groups, we used contingency table analysis and Chi-square tests and T-tests. We conducted logistic regression analysis to assess the effect of the intervention adjusting for possible covariates. Odds Ratios were adjusted for potential confounding by patient variables (age, gender, education level, insurance status, acculturation level, and English proficiency) and physician variables (attending vs. resident, Spanish fluency).
RESULTS
Physician and Patient Characteristics
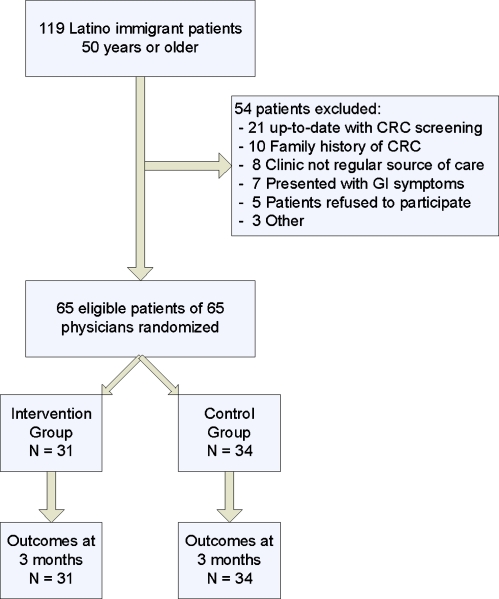
Eighty-two physicians worked in the clinic during the implementation of the study. Seventy-six were approached to participate (were available during the consent process predetermined time). 72 agreed to participate and were enrolled (88% of total physicians and 95% of all approached). Seven physicians did not have patients recruited into the study and were excluded. Study physicians and those excluded had similar personal characteristics. Physician characteristics were similar in the intervention and control groups. (Table 1) Sixty-five eligible patients were enrolled (Fig. 1). No patients were dropped after consenting to participate. Patient characteristics were similar in the intervention and control groups (Table 1).
Table 1.
Baseline Characteristics of Physicians and Patients in the Intervention (N = 31) and Control (N = 34) Groups
| Physician Characteristicsa | ||
| Intervention (n = 31) | Control (n = 34) | |
| Type of Provider | ||
| Staff Physician | 4 (13%) | 6 (18%) |
| Resident | 27 (87%) | 28 (82%) |
| Gender | ||
| Male | 15 (48%) | 18 (53%) |
| Primary language | ||
| English | 28 (90%) | 31 (91%) |
| Spanish | 2 (7%) | 2 (6%) |
| Other | 1 (3%) | 1 (3%) |
| Speak Spanish | ||
| Well-Very Well | 11 (35%) | 13 (38%) |
| Country of Birth | ||
| U.S. | 27 (87%) | 28 (82%) |
| Patient Characteristicsa | ||
| Intervention (n = 31) | Control (n = 34) | |
| Age | ||
| Mean (SD) | 57.6 (6.4) | 58.9 (7.05) |
| Gender | ||
| Male | 15 (48%) | 17 (50%) |
| Marital Status | ||
| Ever Married | 26 (84%) | 26 (76%) |
| Speak English | ||
| Well-Very Well | 9 (29%) | 11 (32%) |
| Education | ||
| 6th grade or less | 11 (35%) | 8 (24%) |
| 7th grade or more | 20 (65%) | 26 (76%) |
| Acculturation Levelb | ||
| Mean (SD) | 1.7 (0.63) | 1.8 (0.73) |
| Health Insurance | ||
| Insured | 21 (68%) | 19 (56%) |
| Years since migrated to the U.S. | ||
| Mean (SD) | 25 (14.4) | 26 (14.1) |
a No statistically significant differences between groups of physicians or patients were found at p < 0.05.
b Marín, G., Sabogal, F., VanOss Marín, B., Otero-Sabogal, F., Pérez-Stable, E. J. Development of a short acculturation scale for Hispanics. Hispanic Journal of Behavioral Sciences,1987; Vol. 9, pp. 183–205
Figure 1.
Flow chart of patient recruitment.
CRC Screening Rates
The overall screening completion rate three months following the intervention was significantly greater in the intervention group than in the control group (17 of 31 (55%) vs. 6 of 34 (18%), (p = 0.002). The absolute increase in completed screening rate was 37% (95% CI 15.5% to 58.9%) and the number needed to treat was 2.7 (95% CI 1.7 to 6.5) for each additional patient screened. Of the patients in the intervention group 19 (61%) received a recommendation for CRC screening compared with 14 (41%) of the patients in the control group (p = 0.08). Of the patients receiving a recommendation for screening, adherence was greater in the intervention group (17 of 19 (90%)) than in the control group (6 of 14 (43%)) (p = 0.007). The absolute increase in adherence was 47% (95% CI 17.25% to 75.98%). Adjusted odd ratios and their 95% confidence intervals for the relationship between intervention and outcomes are shown in Table 2.
Table 2.
Relationship Between Intervention and CRC Screening Outcomes
| Outcome | Intervention n (%) | Control n (%) | Adjusted ORa | 95% CI |
|---|---|---|---|---|
| Completed CRC screening | 17 (55%) | 6 (18%) | 5.4 | 1.6–18.5 |
| Physician recommendation for CRC screening | 19 (61%) | 14 (41%) | 2.0 | 0.70–5.86 |
| Adherence to CRC screening recommendation | 17 (90%) | 6 (43%) | 21.9 | 1.88–255.8 |
a Odds ratios adjusted for: Patient variables (age, gender, education level, insurance status, acculturation level, and English proficiency) and physician variables (attending vs. resident, Spanish fluency)
DISCUSSION
The intervention led to statistically significant and clinically important improvements in CRC screening rates by both increasing physician CRC screening recommendations and increasing patient adherence with the physician recommended screening.
Our study addresses the low CRC screening rates in a hard to reach, Latino immigrant population. Despite the improvements made by this intervention, the CRC screening completion rate (55%) in our study remained below national targets of 90%, but similar to current rates among eligible non-Hispanic whites.8,9 We found that even for those patients who overcame general health care system access barriers to seek primary care, their rate of CRC screening was well below optimal. This represents a missed opportunity in a population where the majority does not have a regular source of care and have low rates of preventive care.10–13
Several studies have shown the importance of activating providers to increase their preventive care recommendations14,15. Our intervention was associated with an increase in physician recommendations for CRC screening that fell shy of statistical significance. Our study showed that low rates of physician recommendation remain a major rate limiting factor for CRC screening.
There are several barriers that impede physicians from recommending CRC screening.16 Physicians cite lack of time to educate their patients as a barrier for screening.16–18 Interventions that use ancillary personnel to provide CRC screening recommendations might be more effective. These should be studied as a means to overcome this rate-limiting step.
Our sample is limited in size because the Latino immigrant population at the clinic was on average young (i.e. below the recommended age of CRC screening), and this limited size is reflected in the wide confidence intervals shown in Table 2 and may have accounted for the failure to detect a significant impact on physician recommendations for CRC screening. The majority of the physicians in the study were rotating residents, and although this could be a limitation, many immigrants depend upon resident physicians for their medical care.
In conclusion, our study demonstrates the feasibility of using a patient-directed approach to enhance CRC screening in a Latino immigrant population. Furthermore, we have demonstrated that the impact of this intervention is primarily mediated through greater adherence by patients to their physician’s recommendations for screening. These findings have substantial implications for the design and implementation of primary care interventions and policies that address the many barriers providers encounter to recommend CRC screening in a diverse patient population. Additional research with larger sample sizes is needed as well as with other underserved and hard to reach populations with the goal of developing clinical practices that will improve the quality of care provided in primary care clinics.
Acknowledgment
This work was done in collaboration with the National Alliance for Hispanic Health. This work was supported by Cooperative Agreement Number T01 CD000146 from Centers for Disease Control and Prevention (CDC). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the CDC.
Conflict of Interest None disclosed.
References
- 1.O'Brien K, Cokkinides V, Jemal A, et al. Cancer statistics for Hispanics, 2003 Cancer. Journal for Clinicians. 2003;53(4):208–26. doi: 10.3322/canjclin.53.4.208. [DOI] [PubMed] [Google Scholar]
- 2.American Cancer Society. Cancer Facts and Figures for Hispanic/Latinos 2009. Accessed January 05, 2010. http://www.cancer.org/docroot/stt/stt_0.asp?from=fast
- 3.Jemal A, Clegg LX, Ward E, et al. Annual report to the nation on the status of cancer. 1975–2001. With a special feature regarding survival. Cancer. 2004;101(1):3–27. doi: 10.1002/cncr.20288. [DOI] [PubMed] [Google Scholar]
- 4.Gilbert A, Kanarek N. Colorectal cancer screening: physician recommendation is influential advice to Marylanders. Prev Med. 2005;41(2):367–79. doi: 10.1016/j.ypmed.2005.01.008. [DOI] [PubMed] [Google Scholar]
- 5.Klabunde CN, Vernon SW, Nadel MR, Breen N, Seeff LC, Brown ML. Barriers to colorectal cancer screening: a comparison of reports from primary care physicians and average-risk adults. Medical Care. 2005;43(9):939–44. doi: 10.1097/01.mlr.0000173599.67470.ba. [DOI] [PubMed] [Google Scholar]
- 6.Zapka JG, Lemon SC. Interventions for patients, providers, and health care organizations. Cancer. 2004;101:1165–87. doi: 10.1002/cncr.20504. [DOI] [PubMed] [Google Scholar]
- 7.Guerra CE, Dominguez F, Shea JA. Literacy and knowledge, attitudes, and behavior about colorectal cancer screening. J Health Commun. 2005;10(7):651–63. doi: 10.1080/10810730500267720. [DOI] [PubMed] [Google Scholar]
- 8.National Commission on Prevention Priorities. Preventive Care: A National Profile on Use, Disparities, and Health Benefits. Partnership for Prevention, August 2007
- 9.Jemal A, Siegel R, Ward E, et al. Cancer Statistics, 2008. CA Cancer J Clin. 2008;58:71–96. doi: 10.3322/CA.2007.0010. [DOI] [PubMed] [Google Scholar]
- 10.Wallace LS, DeVoe JE, Rogers ES, Malagon-Rogers M, Fryer GE., Jr The medical dialogue: disentangling differences between Hispanic and non-Hispanic whites. J Gen Intern Med. 2007;22(11):1538–43. doi: 10.1007/s11606-007-0368-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.New York City Department of Health and Mental Hygiene. The Health of Immigrants In New York City, Report from the New York City Department of Health and Mental Hygiene, 2006. Accessed January 05, 2010. http://home2.nyc.gov/html/doh/downloads/pdf/episrv/episrv-immigrant-report.pdf
- 12.O'Malley AS, Forrest CB, Feng S, Mandelblatt J. Disparities despite coverage: gaps in colorectal cancer screening among Medicare beneficiaries. Arch Intern Med. 2005;165:2129–35. doi: 10.1001/archinte.165.18.2129. [DOI] [PubMed] [Google Scholar]
- 13.Sambamoorthi U, McAlpine DD. Racial, ethnic, socioeconomic, and access disparities in the use of preventive services among women. Prev Med. 2003;37:475–84. doi: 10.1016/S0091-7435(03)00172-5. [DOI] [PubMed] [Google Scholar]
- 14.Love RR, Baumann LC, Brown RL, Fontana SA, Clark CC, Sanner LA, Davis JE. Cancer prevention services and physician consensus in primary care group practices. Cancer Epidemiol Biomarkers Prev. 2004;13(6):958. [PubMed] [Google Scholar]
- 15.Lane DS, Messina CR, Cavanagh MF, Chen JJ. A provider intervention to improve colorectal cancer screening in county health centers. Medical Care. 2008;46:S109–16. doi: 10.1097/MLR.0b013e31817d3fcf. [DOI] [PubMed] [Google Scholar]
- 16.Guerra CE, Schwartz JS, Armstrong K, Brown JS, Halbert CH, Shea JA. Barriers of and facilitators to physician recommendation of colorectal cancer screening. J Gen Intern Med. 2007;22(12):1681–8. doi: 10.1007/s11606-007-0396-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.O'Malley AS, Rentería-Weitzman R, Huerta EE, Mandelblatt J. Patient and provider priorities for cancer prevention and control: a qualitative study in Mid-Atlantic Latinos. Ethn Dis. 2002;12(3):383–91. [PubMed] [Google Scholar]
- 18.Bajracharya SM. An assessment of the perceived barriers and strategies to promoting early detection of colorectal cancer: a practitioners' perspective. Int Q Community Health Educ. 2006–2007;26(1):23–44. doi: 10.2190/13R7-5177-G833-8V85. [DOI] [PubMed] [Google Scholar]