Abstract
Background
Findings have shown that single-incision laparoscopic cholecystectomy (SILC) is feasible and reproducible. The authors have pioneered a two-trocar SILC technique at the University of Texas Southwestern. Their results for 100 patients are presented.
Methods
From January 2008 to March 2009, 100 patients with symptomatic gallbladder disease underwent SILC through a 1.5- to 2-cm umbilical incision using a two-port (5-mm) technique. For nearly all the patients, a 30° angled scope was used. The gallbladder was retracted, with two or three sutures placed along the gallbladder. These sutures were either fixated internally or placed through the abdominal wall to obtain a critical view of Calot’s triangle. The SILC procedure was performed using standard technique with 5-mm reticulating or conventional laparoscopic instruments. The cystic duct and artery were well visualized, clipped, and divided. Cholecystectomy was completed with electrocautery, and the specimen was retrieved through the umbilical incision.
Results
In this series, 80 women (85%) and 15 men (15%) with an average age of 33.8 years (range, 17–66 years) underwent SILC. Their mean BMI was 29.8 kg/m2 (range, 17–42.5 kg/m2), and 39% of these patients had undergone previous abdominal surgery. The mean operative time was 50.8 min (range, 23–120 min). The mean estimated blood loss was 22.3 ml (range, 5–125 ml), and 5% of the patients had an intraoperative cholangiogram. There were no conversions of the SILC technique. A two-trocar technique was feasible for 87% of the patients. For the remaining patients, either a three-channel port or three individual trocars were required. A SILC technique was used for 5% of the patients to manage acute cholecystitis or gallstone pancreatitis.
Conclusion
The SILC technique with a two-trocar technique is safe, feasible, and reproducible. The operating times are reasonable and can be lessened with experience. Even complex cases can be managed with this technique. Excellent exposure of the critical view was obtained in all cases. The SILC procedure is becoming the standard of care for most of the authors’ elective patients with gallbladder disease. Clinical trials are warranted before the SILC technique is adopted universally.
Keywords: Cholecystectomy, Laparoscopic, LESS, NOTES, SILC, SILS, Single incision
Since the late 1980s, surgeons throughout the world have adopted minimal access surgical techniques, and most intraabdominal operations have been replicated successfully, or at least attempted, with the use of laparoscopy. A universal and continuous goal is to decrease more and more the degree of invasion needed to perform such procedures. Laparoscopy itself has become such a disruptive technology and such an evolution of surgery that it perhaps could even compare with such advances as the use of anesthesia or sterile techniques in medicine surgery [1–4].
Laparoscopy has promoted even more innovation with the development of numerous surgical instruments, technological solutions, and novel surgical platforms. Such solutions have come not only from university centers and medical device corporations, but also from individual surgeons with very innovative and entrepreneurial mindsets. However, despite this global vision of lessening the size and number of surgical incisions and thereby the degree of invasion, not much has truly changed during the past two decades.
One major trend during the past few years has been the proposal of natural orifice translumenal endoscopic surgery (NOTES). This concept has promised to give access to the peritoneal cavity through natural orifices such as the mouth, vagina, and the like without violating the abdominal wall. Surgical procedures then would be replicated with this approach. Theoretically, this would result in a painless and scarless surgical procedure [5–10].
Extensive capital and scientific investment together with multidisciplinary efforts have been expended throughout the world to implement such a technique. Unfortunately, most efforts have resulted in very little return of investment, at least not a measurable one in terms of clinical outcomes. Also, NOTES has proved very difficult to reproduce widely, and only a few centers have been successful in performing NOTES safely without violating the true concept of no incisions [11].
On the other hand, NOTES research has resulted in many novel and more advanced surgical technologies that could be adopted currently in minimal access surgery. Also, it has helped to change the mindset of surgeons, pushing them to find ways to lessen even more the size and number of incisions for a given laparoscopic procedure. The result has been a resurgence of single-incision laparoscopic surgical techniques, which had been described even a decade ago [12–15]. Increasingly more surgeons together with the industry have been trying to develop and implement new techniques and technologies that could follow such a concept.
During the latter part of 2007, our team evaluated the feasibility of performing such techniques on animal models mainly with single-incision laparoscopic cholecystectomy and placement of adjustable gastric banding, among others [16–18]. Our results were quite positive, motivating us to translate this technique to the human. In this article, we describe our experience using single-incision laparoscopic cholecystectomy with a large series of 100 patients, which currently represents one of the largest series reported from a single-center.
Methods
From January 2009 to March 2009, and following an initial institutional review board, patients with symptomatic gallbladder disease were recruited for this study. Patients were evaluated before and after surgery at the clinics of University of Texas, Southwestern hospitals and Parkland Memorial Hospital. Initially, our inclusion criteria were limited mainly to patients who would be acceptable candidates to undergo a laparoscopic cholecystectomy at an ambulatory surgery center. This represented patients in overall good health without complex biliary disease (including choledocolithiasis) or extensive previous abdominal surgery and with a body mass index lower than 35 kg/m2.
All the patients consented to a laparoscopic cholecystectomy. They were informed in great detail about the operative strategy of having a single incision in the abdomen with a possibility of several more incisions or a conversion to an open technique. No patients declined to undergo such a technique.
Our evaluation is a retrospective examination of prospectively collected data. As our experience with this technique improved, more complex patients were included, as described in the following discussion. For all the patients, the main author (HR) was part of the operating crew, and the operative technique was standardized.
Surgical technique
Following routine perioperative care and anesthesia, patients were placed in a supine position with both upper extremities abducted. The surgeon stood on the left side of the patient unless he or she was left-handed. The umbilicus then could be everted by pulling the deepest point of the umbilical scar (inner ring) out of its inward position (Fig. 1). A 1.5- to 2-cm transumbilical incision then was performed in a vertical fashion without extension of this incision beyond the outer limits of the umbilical folds (Fig. 2). By incising the umbilical stalk, we obtained direct access into the abdomen because the main author favors conventional laparoscopy (Fig. 3). Through that opening, a low-profile, 5-mm trocar (Dexide; Covidien, North Haven, CT) was placed under direct vision without the need for an introducer or previous pneumoperitoneum. Only for cases in which the entry site into the abdomen was not readily identified after the stalk had been incised was pneumoperitoneum obtained with the use of a Veress needle.
Fig. 1.
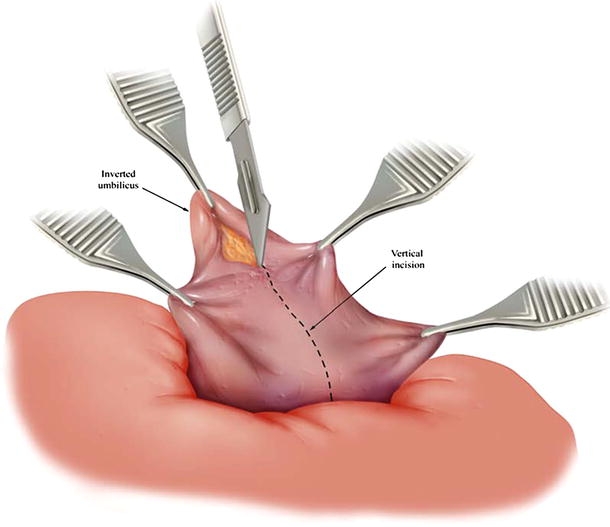
Eversion of the umbilicus and transumbilical incision within the umbilical folds giving adequate access and excellent aesthetic results. Copyright © 2009 Covidien. All rights reserved. Used with the permission of Covidien
Fig. 2.
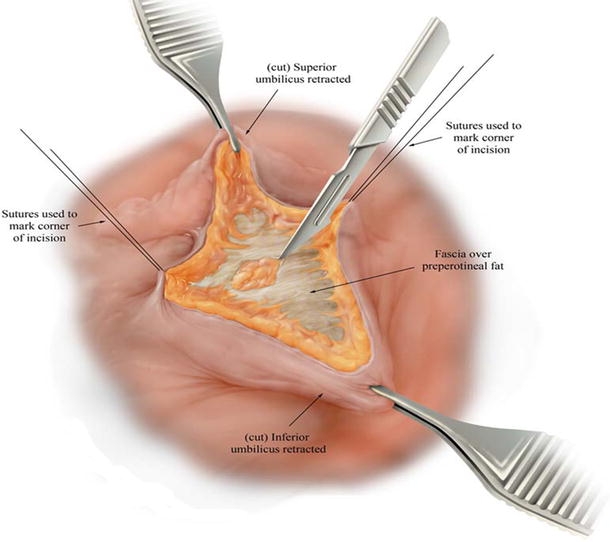
Open abdominal entry through the umbilical stalk. Copyright © 2009 Covidien. All rights reserved. Used with the permission of Covidien
Fig. 3.
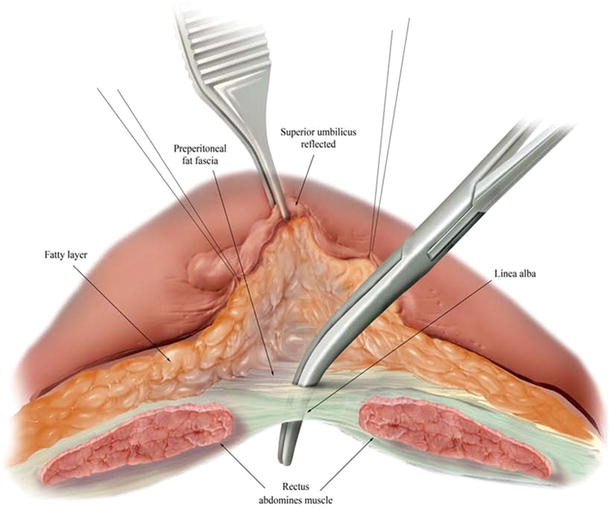
Adequate entry into the abdomen confirmed with placement of a blunt instrument through the incised umbilical stalk. Copyright © 2009 Covidien. All rights reserved. Used with the permission of Covidien
After adequate pneumoperitoneum had been obtained, a second 5-mm port was placed through the same skin incision, but approximately 5 mm above the first port. Only if needed was an additional 5-mm trocar placed inferiorly or laterally through the same skin incision but at a different fascial site. The use of three different fascial incisions could become a problem with a gas leak, yet we avoided this by not making such openings too near each other (at least 2 mm apart). Use of a third trocar was required mainly for cases involving a great degree of visceral fat (making exposure a bit more challenging) or a dome-down technique (n = 3).
For 10 patients, we chose to place a multichannel port device (TriPort [n = 7] Advanced Surgical Concepts or SILS Port [n = 3] by Covidien). The decision to use one of these multichannel devices was based mainly on its availability. This is quite evident considering the paucity of cases managed with such devices because during most of our experience, they were not yet available for clinical use.
For our first patient, a flexible-tip endoscope was used (EndoEYE Olympus, Tokyo, Japan). For all the remaining 99 patients, a 30º angled rigid laparoscope (Hopkins; Storz, Tuttlingen, Germany) was used. This decision was based purely on the limited availability of a special laparoscope in our operating room. As we evolved with this technique, we preferred to use an extra-long (50 cm) 30º rigid bronchoscope with a 90º adaptor for the light source (Hopkins; Storz).
After adjustment of the surgical table to a reverse Trendelemburg position with a slight rotation to the patient’s left side, the gallbladder was identified and then retracted cephalad and lateral with two or three interrupted sutures placed in the gallbladder fundus, body, and Hartmann’s pouch, imitating retraction from conventional technique (Figs. 4, 5, 6). These sutures were either internally fixated (using an extracorporeal suturing technique requiring a single instrument only) or placed through the abdominal wall to obtain a critical view of Calot’s triangle structures (Fig. 7). Laparoscopic cholecystectomy then was performed by standard technique with a single 5-mm Roticulator dissector (Covidien), conventional laparoscopic instruments, or both.
Fig. 4.
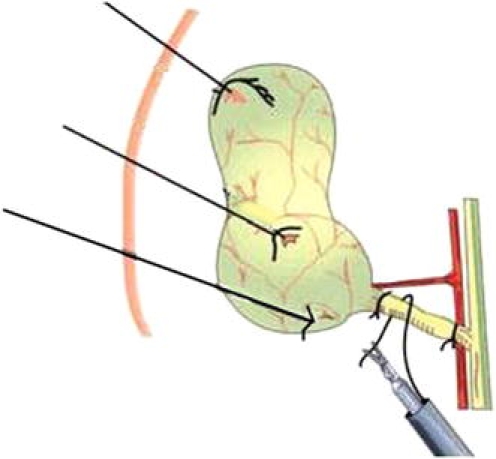
Two to three sutures used to retract the gallbladder. Modified with permission from Dávila F: Surgery without a trace. UNAM/AMCE Ed, 2002, First edition, México
Fig. 5.
Cephalad suture retraction at the dome of the gallbladder
Fig. 6.
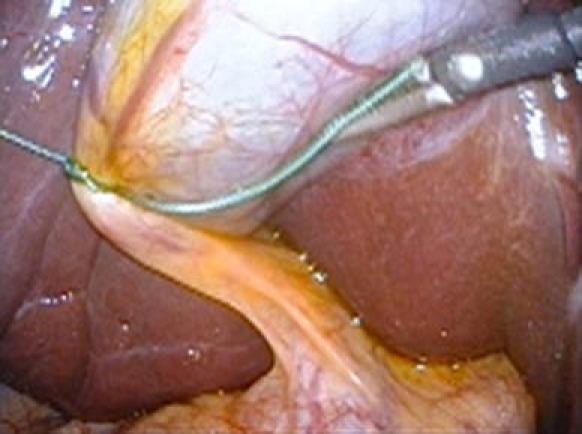
Lateral suture retraction at the level of the neck of the gallbladder
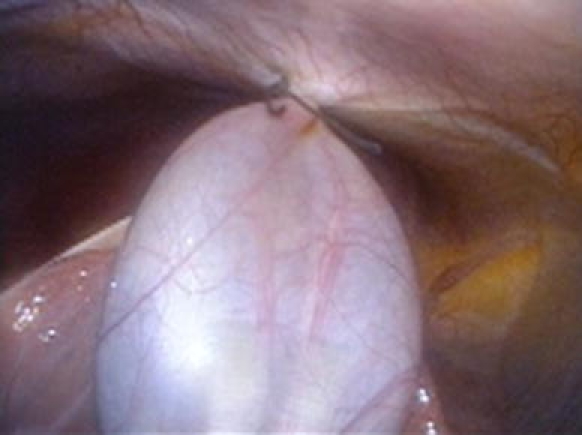
Fig. 7.
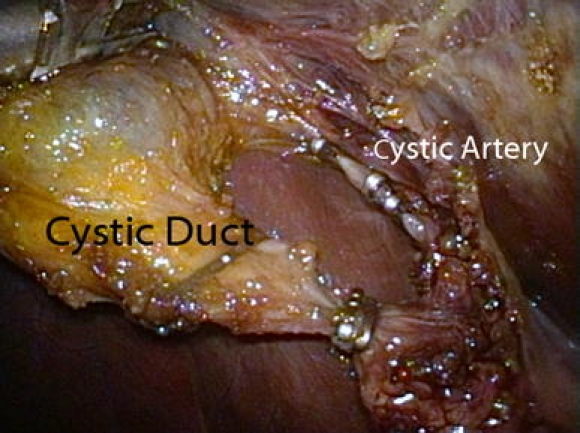
Critical view of structures at the triangle of Calot
For cases in which three ports or the multichannel ports were used (n = 13), a Roticulator grasper (Covidien) was used to improve exposure by lateral retraction of the gallbladder or retraction of omental fat in patients with increased intraabdominal and visceral fat. Critical exposure of the triangle of Calot was always obtained, and the cystic duct and artery were divided with a 5-mm clip applier. Cholecystectomy then was completed with the use of monopolar electrocautery (Fig. 8).
Fig. 8.

View of distended gallbladder hanging by retracting sutures from the abdominal wall
Next, one of the 5-mm trocars was exchanged for a 10-mm trocar to allow the use of a specimen retrieval bag. Then the fascial incisions were connected, followed by removal of the bag and specimen through the umbilical incision. Finally, the fascial opening and skin were closed with absorbable sutures.
A modified dome-down technique was performed by preserving the utmost superior attachment of the gallbladder to the liver bed and then dissecting down toward the hilum of the gallbladder. By keeping this attachment and using a third instrument, this technique was feasible for three patients.
Results
In this series, 80 woman (85%) and 15 men (15%) with an average age of 33.8 years (range, 17–66 years) underwent SILC. The mean body mass index (BMI) of the patients was 29.8 kg/m2 (range, 17–42.5 kg/m2), and 39% of them had undergone previous abdominal surgery. The mean operative time was 50.8 min (range, 23–120 min), and the mean estimated blood loss was 22.3 ml (range, 5–125 ml). An intraoperative cholangiogram was obtained for 5% of the patients. No conversions of the SILC technique occurred. A two-trocar technique was feasible for 87% of the patients. For the remaining 13% of the cases, either a three-channel device or three individual trocars were required. No conversions to conventional laparoscopy or open surgery occurred, and 5% of the patients underwent a SILC technique for acute cholecystitis or gallstone pancreatitis. Three patients had marked chronic cholecystitis, requiring a dome-down technique. For two of these patients, the gallbladder had to be ligated at the level of the neck with endoloops.
A review of our operative times showed a noticeable drop in time, from 73 min (range, 35–120 min) to 45.1 min (range, 23–90 min) (Table 1). Certainly, attaining a learning curve improved our times considerably to times comparable with those for conventional laparoscopic surgery at our institution. Additionally, as we progressed in our experience, an increasing number of complex patients were included in our study. Of the 39 patients who had previous surgery, 2 had undergone a laparoscopic Roux-Y-Gastric bypass. The remaining patients had lower abdominal procedures mainly for gynecologic and obstetric reasons. One patient was found to have Child’s A liver cirrhosis, confirmed with simultaneous liver biopsy. No intraoperative complications occurred.
Table 1.
Demographics and operative outcomes of our first 100 single incision laparoscopic cholecystectomies
| First 50 patients n (range) | Second 50 patients n (range) | Average 100 cases N (range) | |
|---|---|---|---|
| Age | 36.1 (21–66) | 31.84 (17–56) | 33.8 (17–66) |
| OR time (min) | 73 (35–120) | 45.1 (23–90) | 50.8 (23–120) |
| EBL (ml) | 32 (10–125) | 12.1 (5–50) | 22.3 (5–125) |
| F/M ratio (%/%) | 82/18 | 88/12 | 85/15 |
| BMI kg/m2 | 28 (17.4–41) | 28.94 (17–42.5) | 29.8 (17–42.5) |
OR operating room, EBL estimated blood loss, F female, M male, BMI body mass index
All the patients were evaluated in the clinic within 1 month after surgery. Three patients were evaluated in the emergency room before their scheduled appointment. Two of these patients were readmitted. The first patient had abdominal pain from an unknown source. For this patient, extensive evaluation with computed tomography (CT) scan of the abdomen, ultrasound of the liver, HIDA scan, and liver function tests were normal. The patient’s pain was self-limited, and he was discharged almost pain free within 72 h from the time of his readmission.
The second patient was one of those who had required a dome-down technique for severe chronic cholecystitis, and for whom a more proximal ligation to the neck and Hartmann’s pouch had been performed with endoloops. This patient was readmitted with symptomatic retained stones requiring uneventful endoscopic retrograde cholangiopancreatography (ERCP) and sphincterotomy. She was discharged home 24 h after her ERCP.
The final patient seen in the emergency room had been experiencing abdominal pain that was self-limited within hours. This patient also had a normal CT scan of the abdomen. No wound infections, biliary duct injuries, or postoperative hernias were reported. The most dramatic result undoubtedly was the absence of a visible scar in most cases (Figs. 9, 10).
Fig. 9.

Excellent aesthetic results 3 weeks after single-incision laparoscopic cholecystectomy
Fig. 10.

Excellent aesthetic results 6 months after single-incision laparoscopic cholecystectomy
Patients of all ages and the health care providers who evaluated them after surgery were very impressed and found value in the single-incision laparoscopic approach. It was noted that patients with morbid obesity and a large fatty liver were more challenging and perhaps not worth the time and potential additional risk of this technique. Subjectively, it was observed that older men posed a technically greater challenge for this technique mainly because of increased visceral fat.
Discussion
Any innovation, especially in medicine, may succeed only if it proves to be safe, reproducible, and cost effective, among several other factors. After 20 years, laparoscopic techniques in general surgery and in other specialties have shown most of those attributes. However, some techniques have not been as reproducible (e.g., laparoscopic inguinal hernia repair, laparoscopic hysterectomy, laparoscopic pancreatic resections). These procedures have become more controversial and thus have not been adopted widely as a gold standard.
A few years ago, NOTES was introduced as a new surgical concept that would share the same benefits conferred by conventional minimally invasive surgery but without scars and perhaps with considerably minimal pain to none at all [5–10]. All these theoretical advantages have spurred widespread research and investigation forward, with extensive financial and scientific investment allocated to NOTES. Since then, a broad array of mixed results has been reported. Most may argue that the return for the investment has been modest at its best because very few people have been successful in clinically replicating even basic surgical procedures using NOTES [11]. On the other hand, it is quite evident that this movement has resulted in the development of numerous technological advancements that can potentially be applied to a great extent in current clinical practice.
Parallel to this development has been a global interest and resurgence in laparoscopic surgery performed through a single incision without any visible scars. Several groups, including ours, have pioneered and mastered new techniques based on this concept [16–29], which by this time has received a very extensive nomenclature (Table 2).
Table 2.
Proposed nomenclature for single incision laparoscopic surgery
| Nomenclature |
|---|
| Single Incision Laparoscopic Surgery |
| TUES (Trans Umbilical Endoscopic Surgery) |
| SILS™ |
| LESS™ (Laparo Endoscopic Single-site Surgery) |
| SPA™ Single Portal Access |
| E-NOTES (Embryologic Natural Orifice Translumenal Endoscopic Surgery) |
| SAS (Single Access Surgery) |
| S3 (Single Site Surgery) |
| Single Port Surgery |
| CL1P (Cirugía Laparoscópica de 1 puerto, One-port laparoscopic surgery) |
| NOTUS (Natural Orifice Trans Umbilical Surgery) |
| SAVES (Single Access Video Endoscopic Surgery) |
Performing laparoscopic surgery through a single incision seems more intuitive than NOTES, especially for surgeons who routinely perform laparoscopic surgery and may not have the sophisticated infrastructure that NOTES may require. Also, the infrastructure needed to replicate surgical procedures with a single-incision laparoscopic platform appears to be quite straightforward and attainable by most practices, especially with the current availability of multiple technological solutions from the industry and from academic centers.
A single-incision laparoscopic cholecystectomy can be performed with a combination of conventional laparoscopic instrumentation and novel devices especially designed for this technique. Whether to use two rather than three instruments, trocars, or a multichannel device will be a decision based on the expertise of each surgical team and on the availability of these devices. Also, cost-containment decisions will determine the direction that might be taken. It is our observation that anytime a third instrument is required, a roticulating or articulating instrument will be almost mandatory to overcome the constant clashing of instruments. The use of a multichannel device promises a more streamlined process, with the benefits of a bimanual performance by the surgeon, yet with a potential increase in cost and the size of the fascial defect. This last hypothesis merits further investigation. Also smaller and more efficient multichannel devices (with 2, 3, or 4 channels) are being evaluated.
This surgical concept of laparoscopy through a single incision seems itself a bridge to NOTES because it promises the absence of a visible scar and potentially less pain than conventional laparoscopy [28, 29]. Both approaches have a single site of surgical entry. However, the two approaches are very different in nature.
Some clinicians, including our group, are already implementing hybrid techniques with single-incision laparoscopy and NOTES [30]. It is hypothesized that pain with single-incision laparoscopy may be less because muscle trauma to the abdominal wall is minimal if not absent altogether, especially with a transumbilical approach. Optimizing aesthetic results also makes the umbilicus the ideal incision of access. The skill sets necessary for single-incision laparoscopic cholecystectomy are greatly leveraged on the economies of scale and scope that most surgeons have already attained during the last 20 years, with laparoscopic cholecystectomy one among many procedures.
In the same way, once great experience with laparoscopy through a single incision is attained, it may lend itself very conducive to safe and successful implementation of NOTES (e.g., use of flexible endoscopy with one-wound laparoscopy, use of magnetic anchored devices) [23, 28, 31].
Once the basic concepts of this emergent technique are understood, especially its inherent challenges and potential solutions, its learning curve may be considerably shortened (Table 3). Actually, we believe that one of its greatest challenges, and consequently also that of NOTES, may be to change the mindset of surgeons, as was experienced during the late 1980s with the wide adoption of laparoscopy [2–4, 32]. It is our observation that once the fundamentals of the technique are understood and ideally put into practice on dry or animal models, a learning curve of 20 to 25 cases may be considered a conservative estimate for safe adoption of the procedure in clinical practice. This hypothesis should be subjected to detailed evaluation in further studies.
Table 3.
Common challenges and solutions during single incision laparoscopic surgery
| Challenges |
| Clashing of instruments |
| Lack of ideal operative ports |
| Interference and deflection of laparoscope’s light source by operating instruments |
| Interference of wires or tubing that connect perpendicularly to instruments (i.e., cautery) |
| Difficulty with retraction of organs or structures |
| Change of surgeon’s mindset |
| Lack of time and patience to learn |
| Loss of propioception due to crossed instrument |
| Solutions |
| Use of curved, reticulating, or flexible instruments |
| Use of very-low-profile trocars |
| Staggering heights and heads of trocars |
| Use of novel multichannel ports |
| Use of a laparoscope with a light source on the back of the camera |
| Use of a flexible-tip endoscope |
| Use of an extra-long 5-mm angled laparoscope (50 cm) |
| Use of a 90º adaptor for the light source (for sharp change in its direction parallel to the laparoscope) |
| Use of instruments that connect at their distal ends any necessary wires or tubing (i.e., cautery) |
| Use of extra-long bariatric size instruments |
| Use of retracting sutures |
| Continuous medical education |
| Potential solutions |
| Design of innovative retracting platforms |
| Implementation of magnetically anchored instruments deployed though a single incision |
| Implementation of robotic platforms |
| Design of sigmoid-shaped instruments |
| Additional basic surgical principles |
| Sound surgical judgment |
| Maintenance of equivalent operative exposure |
| Low threshold for use of additional ports at the initial incision site or prompt conversion to conventional laparoscopy or to open surgery |
Of paramount importance, as with any emergent technique, it only makes sense to practice a very careful patient selection, especially at the beginning of one’s experience, using strict criteria to find ideal patients. Once great expertise is achieved, these criteria can be relaxed. As a matter of fact, single-incision laparoscopic surgery may represent only another alternative. At some point, it will become more common to hear that a surgery started with a single-incision technique (one trocar), and that at placement of the camera and evaluation of the abdominal cavity, it was decided to proceed in this manner (using more than one trocar in the same incision) instead of using multiple trocars in different incisions. In both circumstances, the surgery would be performed laparoscopically. Using this approach clinicians may identify suitable candidates for this single incision laparoscopic technique. This could be adopted as an initial strategy when this technique used. We certainly took this approach.
Any innovative or disruptive technique or technology is conducive to mass adoption only if it is found to be safe in prospective clinical trials. Furthermore, crossing the chasm of innovation from early adopters to mass implementation is possible only if the technique, in addition to being safe, is reproducible and makes economic sense [33].
Based in our initial experience with one of the largest series reported from a single institution to date, single-incision laparoscopic cholecystectomy appears to have all the aforementioned attributes essential to successful innovation for its universal adoption. The surgical community must adopt this new technique only in a responsible way, with evaluation of results from series such as ours, in addition to proper continuous medical education and transparent communication to patients about its experience and outcomes. Surgeons who may consider implementing this technique will benefit the most from creating specialized teams, even with other health care providers from different specialties (e.g., gynecology, pediatric surgery, bariatric surgery) who have a common interest in this technique, as has been done in the past with NOTES and laparoscopy itself. Also, implementation of robotic platforms in single-incision laparoscopy has great potential because this may facilitate the performance of more complex operative procedures, making this technique even more reproducible [34].
Conclusions
Single-incision laparoscopic cholecystectomy is safe, feasible, and quite reproducible in experienced hands. This technique can be applied for the management of patients in outpatient surgery centers because most of them may not have very complex disease. Furthermore, with progressive experience, more complex patients may be suitable candidates for this technique. The outcomes seem comparable with those for conventional endoscopic techniques, with similar minimal morbidity and no mortality in our series. The operating times are reasonable and can be lessened to times comparable with those for the conventional endoscopic approach [35–37], especially when basic concepts regarding the challenges of this technique are better understood and solutions are being implemented.
We have observed that surgeons in training and experienced laparoscopic surgeons may not need to undergo a steep learning curve. After our initial experience with 100 patients, single-incision laparoscopic cholecystectomy is becoming the standard of care for most of our elective patients with gallbladder disease. Clinical trials still are warranted before this procedure is adopted universally. Wide adoption of this technique should be carefully implemented, with continuous medical education in theory and with simulator or animal models. Transparent communication with patients regarding experience and outcomes during the implementation phase for this procedure in clinical practice is not only mandatory but also ethical.
Acknowledgments
Disclosures
Dr. Homero Rivas is a consultant and speaker for Covidien, receiving honoraria and reimbursed travel for any activities that may involve either role. Dr. Rivas has no stock ownership, equity interests, patent-licensing arrangements, or the like that might pose a conflict of interest in connection with the submitted article. Dr. Rivas detailed that disclosures have not influenced in any way, shape, or form this scientific work and its publication. Dr. Esteban Varela is a research consultant for Ethicon Endosurgery, receiving honoraria and reimbursed travel for any activities that may involve this consulting role. Dr. Varela has no stock ownership, equity interests, patent-licensing arrangements, or the like that might pose a conflict of interest in connection with the submitted article. Dr. Varela’s detailed disclosures have not influenced in any way, shape, or form this scientific work and its publication. Dr. Daniel Scott has a licensing agreement with Ethicon Endosurgery regarding Magnetic Anchoring and Guidance Systems (MAGS). Also he has research grants with Ethicon Endosurgery. Dr. Scott is a speaker for Covidien and has research grants as well with this company. Dr. Scott is a speaker for Allergan. He has research and equipment grants with Storz and is a consultant for Accelerated Technologies Incorporated. Dr. Scott receives honoraria and reimbursed travel for any activities that may involve any role previously described. He has no stock ownership, equity interests, patent-licensing arrangements, or the like that might pose a conflict of interest in connection with the submitted article. Dr. Scott’s detailed disclosures have not influenced in any way, shape, or form this scientific work and its publication.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Cuschieri A (2005) Laparoscopic surgery: current status, issues, and future developments. Surgeon 3:125–130, 132–133, 135–138 [DOI] [PubMed]
- 2.Cuschieri A. Minimal access surgery: the birth of a new era. J R Coll Surg Edinb. 1990;35:345–347. [PubMed] [Google Scholar]
- 3.Soper NJ. Laparoscopic cholecystectomy. Curr Probl Surg. 1991;28:581–655. doi: 10.1016/0011-3840(91)90041-M. [DOI] [PubMed] [Google Scholar]
- 4.Nagy AG, Poulin EC, Girotti MJ, Litwin DE, Mamazza J. History of laparoscopic surgery. Can J Surg. 1992;35:271–274. [PubMed] [Google Scholar]
- 5.Rattner D. Introduction to NOTES White Paper. Surg Endosc. 2006;20:185. doi: 10.1007/s00464-005-3007-z. [DOI] [PubMed] [Google Scholar]
- 6.The NOSCAR Joint Committee on NOTES whose members are Hawes RH, Rattner DW, Fleischer D, Gostout CJ, Kalloo A, Kochman M, Marohn M, Ponsky J, Rothstein R, Schwaitzberg S, Smith CD, Swanstrom L, Talamini M, Thompson CC (2008) NOTES trademark: where have we been and where are we going? Gastrointest Endosc 67:779–780 [DOI] [PubMed]
- 7.Rattner D, Kalloo A, ASGE/SAGES Working Group ASGE/SAGES Working Group on Natural Orifice Translumenal Endoscopic Surgery, October 2005. Surg Endosc. 2006;20:329–333. doi: 10.1007/s00464-005-3006-0. [DOI] [PubMed] [Google Scholar]
- 8.Swain P. Nephrectomy and natural orifice translumenal endoscopy (NOTES): transvaginal, transgastric, transrectal, and transvesical approaches. J Endourol. 2008;22:811–818. doi: 10.1089/end.2007.9831. [DOI] [PubMed] [Google Scholar]
- 9.Zorron R, Maggioni LC, Pombo L, Oliveira AL, Carvalho GL, Filgueiras M. NOTES transvaginal cholecystectomy: preliminary clinical application. Surg Endosc. 2008;22:542–547. doi: 10.1007/s00464-007-9646-5. [DOI] [PubMed] [Google Scholar]
- 10.Pai RD, Fong DG, Bundga ME, Odze RD, Rattner DW, Thompson CC. Transcolonic endoscopic cholecystectomy: a NOTES survival study in a porcine model (with video) Gastrointest Endosc. 2006;64:428–434. doi: 10.1016/j.gie.2006.06.079. [DOI] [PubMed] [Google Scholar]
- 11.Boni L, Dionigi G, Rovera F. Natural orifices transluminal endoscopic surgery (NOTES) and other allied “ultra” minimally invasive procedures: are we loosing the plot? Surg Endosc. 2009;23:927–929. doi: 10.1007/s00464-009-0353-2. [DOI] [PubMed] [Google Scholar]
- 12.Navarra G, Pozza E, Occhionorelli S, Carcoforo P, Donini I. One-wound laparoscopic cholecystectomy. Br J Surg. 1997;84:695. doi: 10.1002/bjs.1800840536. [DOI] [PubMed] [Google Scholar]
- 13.Dávila F, Weber A, Dávila U, Lemus J, López J, Reyes G, Domínguez V (1999) Laparoscopic cholecystectomy with only one port (with no trace): a new technique. Society of Gastrointestinal Endoscopic Surgeons 1999 Annual Congress, San Antonio, TX
- 14.Kosumi T, Kubota A, Usui N, Yamauchi K, Yamasaki M, Oyanagi H. Laparoscopic ovarian cystectomy using a single umbilical puncture method. Surg Laparosc Endosc Percutan Tech. 2001;11:63–65. [PubMed] [Google Scholar]
- 15.Kubota A, Okuyama H, Oue T, Ikegami R, Kamiyama M, Yagi M, Kosumi T, Yamauchi K, Nogami T, Usui N (2001) Application of single-puncture technique to laparoscopy-assisted surgery in children. Pediatr Endosurg Innovative Tech 5:385–388
- 16.Rivas H, Varela E, Scott D (2008) Single-incision laparoscopic cholecystectomy in an animal model. Society of Gastrointestinal Endoscopic Surgeons, 2008 Annual Congress, Emerging Technologies, Philadelphia, PA
- 17.Rivas H, Varela E, Scott D (2008) Single-incision laparoscopic surgery for placement of adjustable gastric banding in an animal model. Society of Gastrointestinal Endoscopic Surgeons, 2008 Annual Congress, Emerging Technologies, Philadelphia, PA
- 18.Raman JD, Bensalah K, Bagrodia A, Stern JM, Cadeddu JA. Laboratory and clinical development of single keyhole umbilical nephrectomy. Urology. 2007;70:1039–1042. doi: 10.1016/j.urology.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 19.Rivas H, Varela E, Scott D (2008) As smooth as SILC: single-incision laparoscopic cholecystectomy. Society of Gastrointestinal Endoscopic Surgeons, 2008 Annual Congress, Emerging Technologies, Philadelphia, PA
- 20.Rivas H, Rivas R, Vargas R, Rivas H (2008) Single-umbilical-incision totally laparoscopic hysterectomy. Society of Gastrointestinal Endoscopic Surgeons, 2008 Annual Congress, Emerging Technologies, Philadelphia, PA
- 21.Castellucci SA, Curcillo PG, Ginsberg PC, Saba SC, Jaffe JS, Harmon JD. Single-port access adrenalectomy. J Endourol. 2008;22:1573–1576. doi: 10.1089/end.2008.0100. [DOI] [PubMed] [Google Scholar]
- 22.Cuesta MA, Berends F, Veenhof AA. The invisible cholecystectomy: a transumbilical laparoscopic operation without a scar. Surg Endosc. 2008;22:1211–1213. doi: 10.1007/s00464-007-9588-y. [DOI] [PubMed] [Google Scholar]
- 23.Afthinos JN, Forrester GJ, Binenbaum SJ, Harvey EJ, Kim GJ, Teixeira JA (2009) Single-incision laparoscopic cholecystectomy using flexible endoscopy: saline infiltration gallbladder fossa dissection technique. Surg Endosc. Epub ahead of print March 19 [DOI] [PubMed]
- 24.Tacchino R, Greco F, Matera D. Single-incision laparoscopic cholecystectomy: surgery without a visible scar. Surg Endosc. 2009;23:896–899. doi: 10.1007/s00464-008-0147-y. [DOI] [PubMed] [Google Scholar]
- 25.Tracy CR, Raman JD, Cadeddu JA, Rane A. Laparoendoscopic single-site surgery in urology: where have we been and where are we heading? Nat Clin Pract Urol. 2008;5:561–568. doi: 10.1038/ncpuro1215. [DOI] [PubMed] [Google Scholar]
- 26.Hodgett SE, Hernandez JM, Morton CA, Ross SB, Albrink M, Rosemurgy AS. Laparoendoscopic single site (LESS) cholecystectomy. J Gastrointest Surg. 2009;13:188–192. doi: 10.1007/s11605-008-0735-0. [DOI] [PubMed] [Google Scholar]
- 27.Zhu JF. Scarless endoscopic surgery: NOTES or TUES. Surg Endosc. 2007;21:1898–1899. doi: 10.1007/s00464-007-9551-y. [DOI] [PubMed] [Google Scholar]
- 28.Elazary R, Khalaileh A, Zamir G, Har-Lev M, Almogy G, Rivkind AI, Mintz Y. Single-trocar cholecystectomy using a flexible endoscope and articulating laparoscopic instruments: a bridge to NOTES or the final form? Surg Endosc. 2009;23:969–972. doi: 10.1007/s00464-008-0289-y. [DOI] [PubMed] [Google Scholar]
- 29.Abe N, Takeuchi H, Ueki H, Yanagida O, Masaki T, Mori T, Sugiyama M, Atomi Y (2009) Single-port endoscopic cholecystectomy: a bridge between laparoscopic and translumenal endoscopic surgery. J Hepatobiliary Pancreat Surg. Epub ahead of print April 17 [DOI] [PubMed]
- 30.Zornig C, Mofid H, Emmermann A, Alm M, von Waldenfels HA, Felixmüller C. Scarless cholecystectomy with combined transvaginal and transumbilical approach in a series of 20 patients. Surg Endosc. 2008;22:1427–1429. doi: 10.1007/s00464-008-9891-2. [DOI] [PubMed] [Google Scholar]
- 31.Scott DJ, Tang SJ, Fernandez R, Bergs R, Goova MT, Zeltser I, Kehdy FJ, Cadeddu JA. Completely transvaginal NOTES cholecystectomy using magnetically anchored instruments. Surg Endosc. 2007;21:2308–2316. doi: 10.1007/s00464-007-9498-z. [DOI] [PubMed] [Google Scholar]
- 32.Cuschieri A. The laparoscopic revolution: walk carefully before we run. J R Coll Surg Edinb. 1989;34:295. [PubMed] [Google Scholar]
- 33.Moore GA (2002, August 20) Crossing the chasm. Rev ed. Collins Business ed. USA
- 34.Rané A, Tan GY, Tewari AK (2009) Laparoendoscopic single-site surgery in urology: is robotics the missing link? BJU Int. Epub ahead of print March 4 [DOI] [PubMed]
- 35.Del Pin CA, Arthur KS, Honig C, Silverman EM. Laparoscopic cholecystectomy: relationship of pathology and operative time. JSLS. 2002;6:149–154. [PMC free article] [PubMed] [Google Scholar]
- 36.Berber E, Engle KL, Garland A, String A, Foroutani A, Pearl JM, Siperstein AE. A critical analysis of intraoperative time utilization in laparoscopic cholecystectomy. Surg Endosc. 2001;15:161–165. doi: 10.1007/s004640000329. [DOI] [PubMed] [Google Scholar]
- 37.Wang WN, Melkonian MG, Marshall R, Haluck RS. Postgraduate year does not influence operating time in laparoscopic cholecystectomy. J Surg Res. 2001;101:1–3. doi: 10.1006/jsre.2001.6252. [DOI] [PubMed] [Google Scholar]


