SUMMARY
We evaluated the association between typhoid fever and Helicobacter pylori infection, as the latter microorganism may influence gastric acid secretion and consequently increase susceptibility to Salmonella typhi infection. Anti-H. pylori IgG and IgA antibody titres (ELISA) and gastrin concentration (RIA) were determined in the plasma of 87 blood culture-confirmed typhoid fever cases (collected after clinical recovery) and 232 random healthy controls without a history of typhoid fever, in the Jatinegara district, Jakarta. Patients with typhoid fever more often than controls were seropositive for H. pylori IgG (67% vs. 50%, P<0·008), when antibody titres were dichotomized around median titres observed in controls. H. pylori IgA seropositivity was not associated with typhoid fever. Plasma gastrin concentrations indicative of hypochlorhydria (i.e. gastrin ⩾25 or ⩾100 ng/l) were not significantly elevated in typhoid fever cases compared to controls (P=0·54 and P=0·27 respectively). In a multivariate analysis, typhoid fever was independently associated with young age (<33 years, median age of the controls) [odds ratio (OR) 7·93, 95% confidence interval (CI) 3·90–16·10], and H. pylori IgG seropositivity (OR 1·93, 95% CI 1·10–3·40). Typhoid fever was independently associated with H. pylori IgG seropositivity, but not with elevated gastrin concentration. Therefore, the association suggests a common risk of environmental exposure to both bacteria, e.g. poor hygiene, rather than a causal relationship via reduced gastric acid production.
INTRODUCTION
Typhoid fever is a serious systemic illness that each year affects over 20 million people, predominantly in developing countries [1]. Infection with Salmonella typhi is transmitted by the faecal–oral route and in several epidemiological studies risk factors were identified that suggested either waterborne transmission [2–6] or foodborne transmission [2, 7–9]. The determination of the relative contribution of distinct environmental risk factors for transmission of disease is essential to focus local control strategies. Also host-related risk factors for infection have been examined, identifying both genetic factors [10, 11] as well as concurrent Helicobacter pylori infection, that was interpreted as a cause of a reduced gastric acid barrier[8].
A high incidence of salmonellosis has been observed in individuals with surgically induced or other types of achlorhydria (pernicious anaemia and chronic atrophic gastritis) [12–14]. Also H. pylori infection may exert an effect on the secretion of gastric acid. Approximately 50% of the world's population is infected with H. pylori [15], and even higher prevalences have been reported in developing countries [16], where acquisition occurs at a younger age than in the developed world [17, 18]. Active infection with H. pylori is associated with a transient hypochlorhydria that may be present for several months [19]. Furthermore, H. pylori-induced chronic gastritis of the body of the stomach reduces acid secretion and persistent hypochlorhydria constitutes a risk for the development of gastric cancer [20, 21]. In the absence of the acid-mediated inhibition of gastric gastrin release, the serum gastrin concentration increases. In contrast, antral-predominant, body-sparing gastritis due to H. pylori increases gastric acid secretion, resulting in duodenal ulcer disease [21–23]. The localization of gastritis depends on the pre-morbid acid secretory status of a subject, dietary, genetic and bacterial factors [22, 24], and the age of acquisition of H. pylori infection [18].
Consequently, the association between H. pylori infection as an indicator of hypochlorhydria and the susceptibility to other gastrointestinal infections is ambiguous. An increased susceptibility to enteric infections in H. pylori-infected individuals, as measured by anti-H. pylori IgG response, was documented for cholera [25, 26] and typhoid fever [8]. However, the evidence for the association of H. pylori infection and diarrhoea is conflicting [27–32] and even a protective effect of H. pylori infection was demonstrated [33, 34].
To examine the association of H. pylori infection and typhoid fever, we determined the anti-H. pylori antibody titres and plasma gastrin in patients who had just recovered from typhoid fever and healthy controls in a case-control study in Jakarta, Indonesia.
MATERIAL AND METHODS
Study design
From June 2001 to October 2003 we identified patients with typhoid fever (S. typhi infections) in a passive community-based surveillance study among individuals with three or more days of fever in the Jatinegara district, Jakarta, Indonesia, as previously described [35]. In addition, six patients with typhoid fever were enrolled in the Medistra Hospital in Central Jakarta. Patients were interviewed using a standardized questionnaire and blood samples were collected during a household visit, conducted within 1 month after making the diagnosis by blood culture, at a time when the patient had recovered from typhoid fever.
During the study period healthy controls were randomly selected in a random household in every third rukun tetangga (RT) of a total of 1140 RTs in Jatinegara; RT being the smallest administrative unit comprising of 40–60 households. Controls were enrolled in a ratio of cases to controls of 1:4 to maximize statistical power of the analysis. The selection of controls was non-matched for age or sex to prevent over-matching. When a control reported any type of fever in the 30 days preceding the interview or refused participation, the house on alternating sides of the initially selected household was approached. From 378 healthy controls 291 (77%) allowed collection of a blood sample. Fifty-nine (20%) of these 291 controls were excluded from the analysis because they reported a history of typhoid fever (defined as an episode of three or more days of fever, requiring antibiotics prescribed by a physician who had made a diagnosis of typhoid fever). If cases or controls were <13 years of age, the mother or guardian was interviewed.
This study was approved by the Indonesian National Institute of Health Research and Development (Litbangkes) and the provincial authorities. From all participants a written informed consent was obtained at the household visit or during hospitalization.
Laboratory diagnosis of typhoid fever
The diagnosis of typhoid fever required confirmation by blood culture. To this end, blood was collected from febrile patients (dependent on the age, 5–10 ml), inoculated in aerobic bottles (Bactec, Becton Dickinson, Franklin Lakes, NJ, USA) and incubated. The identification of cultured microorganisms was done by biochemical tests and agglutination, as previously described [35].
Samples in patients and controls
In the household visits blood samples were collected from non-fasting cases and controls in EDTA tubes. Following centrifugation, plasma was separated and frozen at −70°C.
Measurement of anti-H. pylori IgA and IgG antibodies by ELISA
The ELISA technique for determination of IgG and IgA antibodies against H. pylori as well as information on the intra- and inter-assay variability of the results obtained by this ELISA have been described in detail elsewhere [36, 37]. The antigen is a mixture of sonicates of six different H. pylori strains; these had been obtained by sonicating whole bacteria for 6 min on a Branson sonifier (Danbury, CT, USA) (stage 4; 30 000 cycles/s), and adjusting the suspension to a protein concentration of 3 mg/ml. Optimum concentrations of reagents were determined by checker board titration as previously described [36]. ELISA results are expressed as the absorbance index (AI):
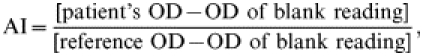 |
where OD is the optical density. Samples were assayed in blinded fashion in one run.
Measurements of gastrin concentrations
Plasma gastrin concentration was measured using a previously validated radioimmune assay (RIA) as previously described [38]. Samples were assayed in blinded fashion in one run.
Statistical methods
Data from the questionnaires were entered twice using Epi-Info 6.04b software (CDC, Atlanta, GA, USA), validated and imported in SPSS version 11.5 (SPSS Inc., Chicago, IL, USA) for further analysis. Unpaired t tests for normally distributed variables or Mann–Whitney U tests for not-normally distributed variables were used to test numerical variables. Correlation between numerical variables was tested by linear regression and the Pearson correlation coefficient (R) was provided. For the comparison of proportions the χ2 test or Fisher's exact test was used. To correct for age strata the Mantel–Haenszel statistic was applied. Measures of association were expressed as odds ratios with their respective confidence limits [OR (95% CI)] when categorical exposures were evaluated. To control for confounding a multivariate analysis was performed by the use of logistic regression.
RESULTS
Demographic characteristics
Plasma samples were available for 87 typhoid fever cases, and were collected at home following clinical recovery of the patient 22 days [median, IQR 20–27] after the confirmatory blood culture. Thirteen patients had been hospitalized and 74 patients were included in local health outpatient facilities. During the same period blood samples were obtained from 232 healthy controls. The median age of all subjects was 27 years (IQR 17–45). Patients with typhoid fever had a median age of 20 years (IQR 13–27), and were significantly younger than the controls [median age 33 years (IQR 19–50); P<0·001 by Mann Whitney U test]. The sex ratio did not differ between the typhoid fever group and controls, i.e. 53% and 59% were females respectively (P=0·29, χ2).
Concentration of IgG and IgA antibodies against H. pylori
Taking all subjects together, the median titre of anti-H. pylori IgG amounted to AI=0·126 (IQR 0·084–0·186) and for IgA to AI=0·094 (IQR 0·057–0·170). In a linear regression model IgG and IgA were significantly correlated, although not strongly considering the correlation coefficient (P<0·001, R=0·23).
In individuals who had suffered from typhoid fever in the preceding month the anti-H. pylori IgG titres [median 0·146 (IQR 0·092–0·190)] were higher than those in controls [median 0·119 (IQR 0·082–0·185)], but the difference did not reach a level of significance (P=0·24, by Mann–Whitney U test). Also the IgA titres did not differ significantly (P>0·50) between typhoid fever cases [median 0·098 (IQR 0·060–0·156)] and controls [median 0·092 (IQR 0·054–0·178)].
In typhoid fever patients and controls alike, IgG and IgA against H. pylori increased with age (Table 1), and in a linear regression model IgG titres and age were significantly correlated (P=0·005, R=0·16) as were IgA AI and age (P<0·001, R=0·30). In all age cohorts higher rates of IgG seropositivity were observed in the group of individuals with typhoid fever, and in the age cohort of 15–29 years this difference reached a level of significance (P=0·02).
Table 1.
H. pylori serology of typhoid fever cases and controls
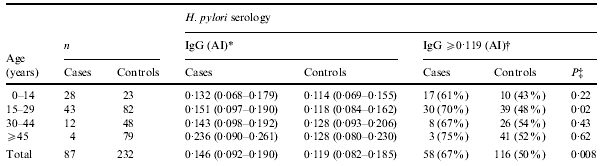
Median absorbance index (25–75% range).
Median antibody AI in total number of healthy controls.
χ2 test (Fisher's exact test if cells contained less than five subjects).
Next, the median AI of IgG and IgA in the healthy controls were used to dichotomize the data to obtain a cut-off level of H. pylori seropositivity (IgG⩾0·119 and IgA⩾0·092 respectively) comparable to the study procedures of Bhan et al. [8]. The percentage of individuals with typhoid fever who had an IgG titre above this level (n=58; 67%) was significantly higher (P=0·008) than that in the controls (n=116; 50%) (Table 1). No significant difference of IgA seropositivity between individuals with typhoid fever and controls was observed; i.e. 46 (53%) vs. 116 (50%) respectively (P=0·65). In a stratified analysis for all individuals correcting for age group by use of the Mantel–Haenszel statistic, IgG seropositivity remained significantly associated with typhoid fever (P=0·007), whereas IgA seropositivity reached borderline significance (P=0·05).
Gastrin concentration
Taking all subjects together, plasma gastrin concentration (ng/l) ranged from 6 to 1253 ng/l, with a median concentration of 54 ng/l (IQR 36–85). On average, gastrin concentrations did not change with age (P>0·50, R=0·004). The gastrin concentration in individuals with typhoid fever [median 53 ng/l (IQR 37–85)] did not differ significantly from that in controls [median 54 ng/l (IQR 36–85)] (P=0·74, Mann–Whitney U test).
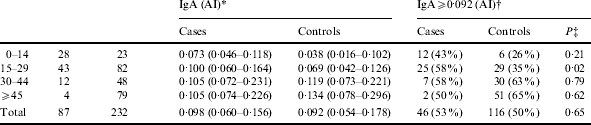
Gastrin concentrations of ⩾25 ng/l and ⩾100 ng/l have been evaluated as markers of hypochlorhydria as a condition of chronic atrophic gastritis [39]. In the analysis of the total group, i.e. both cases and controls, anti-H. pylori antibody indices were higher in the group of individuals with gastrin ⩾25 ng/l than in those with a lower plasma gastrin, reaching significance for IgA AI (P=0·02, Mann–Whitney U test) and borderline significance for IgG AI (P=0·06). The IgG and IgA AI of individuals with gastrin <100 ng/l did not differ significantly from those with gastrin ⩾100 ng/l (P=0·44 and P>0·50 respectively). Accordingly, IgG seropositivity (AI ⩾0·119) was significantly more often encountered in individuals with gastrin ⩾25 ng/l (P=0·03), but not so in the group with gastrin ⩾100 ng/l (P=0·29) (Table 2).
Table 2.
H. pylori IgG seropositivity and gastrin concentrations in all subjects
AI, Absorbance index.
P=0·03 (χ2 test).
P=0·29 (χ2 test).
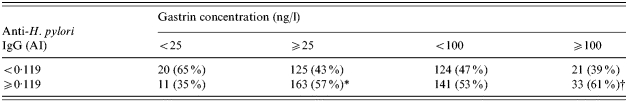
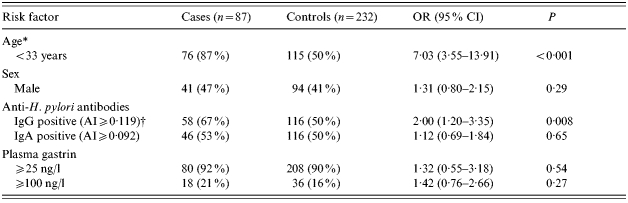
However, the proportions of typhoid fever cases and controls that had gastrin ⩾25 ng/l did not differ significantly (P=0·54) (Table 3). Similarly, in the group of typhoid fever patients, 18 (21%) individuals had a gastrin concentration ⩾100 ng/l, compared to 36 (16%) in the control group (P=0·27).
Table 3.
Univariate analysis: associations with typhoid fever
OR, Odds ratio, CI, confidence interval; AI, absorbance index.
Independently associated in multivariate analysis (OR 7·93, 95% CI 3·90–16·10).
Independently associated in multivariate analysis (OR 1·93, 95% CI 1·10–3·40).
Univariate and multivariate analysis
H. pylori IgG and IgA seropositivity and plasma gastrin concentrations in cases and controls were evaluated by univariate analysis (Table 3). Significantly associated with typhoid fever were: young age (dichotomized at 33 years, the median age of the controls); (OR 7·03, 95% CI 3·55–13·91), and H. pylori IgG seropositivity (OR 2·00, 95% CI 1·20–3·35). Neither H. pylori IgA seropositivity nor elevated plasma gastrin concentrations were significantly associated with typhoid fever.
In a multivariate analysis using multiple logistic regression the occurrence of typhoid fever was independently associated with H. pylori IgG seropositivity (OR 1·93, 95% CI 1·10–3·40), and young age (<33 years) (OR 7·93, 95% CI 3·90–16·10).
DISCUSSION
The main finding of this case-control study in Jakarta is that the prevalence of H. pylori IgG seropositivity was higher in individuals who had recently recovered from blood culture-confirmed typhoid fever than in healthy controls without a history of typhoid fever. However, we did not find an association between typhoid fever and an elevated plasma gastrin concentration indicative of hypochlorhydria or achlorhydria. Furthermore, typhoid fever was independently associated with young age, which suggests that either exposure to S. typhi or the proportion of those exposed that develop symptomatic infection (e.g. due to absence of a previously acquired immune response) is greater among young people.
A reduced secretion of bactericidal gastric acid due to acute or chronic H. pylori infection [22] may increase susceptibility to infection with enteric pathogens. This hypothesis was supported by case-control studies that examined anti-H. pylori IgG antibody concentrations in patients with typhoid fever and cholera, and observed a higher prevalence of H. pylori seropositivity among the cases than controls [8, 25, 26]. To this end, seropositivity was defined as an antibody concentration above the median antibody level of the controls [8], a method we applied in order to compare our results and also to confirm the demonstrated association of typhoid fever and H. pylori infection.
Although the anti-H. pylori IgG response reliably indicates prior infection with H. pylori, H. pylori colonization in the majority of adult typhoid fever cases and controls most likely occurred at a much younger age, i.e. in early childhood [17], than the acquisition of typhoid fever in our study. Moreover, the infection itself may exert different effects on the gastric acid secretion and is, therefore, not one-dimensionally associated with hypochlorhydria as a predisposing condition for enteric infections [21]. In addition, the evidence for a correlation between anti-H. pylori IgG-antibody levels and the severity of gastritis or H. pylori density remains conflicting [40–43], thereby diminishing the likelihood of a more severe gastritis in typhoid fever cases compared to controls. Further, anti-H. pylori antibodies may be a sensitive marker of chronic atrophic gastritis as a cause of hypochlorhydria, although not being a very specific marker [39], which can explain the higher antibody titres and more frequent anti-H. pylori IgG seropositivity in the individuals with gastrin levels of ⩾25 ng/l in our study. However, we did not find evidence for a higher prevalence of chronic atrophic gastritis, as determined by elevated concentrations of plasma gastrin, among cases of typhoid fever compared with healthy controls.
A more likely explanation of the association of increased anti-H. pylori IgG antibodies and typhoid fever might be a higher susceptibility to colonization by and re-exposure to H. pylori as a consequence of low hygienic standards and shared risk factors for both infections, than a supposedly decreased gastric acid secretion in typhoid fever cases. Since re-infection with H. pylori after eradication is common in developing countries [44] signifying continuous exposure, the association of typhoid fever and H. pylori IgG seropositivity may be confounded by poor hygiene.
Some issues related to the outcome of our study need consideration. We did not find an association between H. pylori IgA seropositivity and typhoid fever, probably due to the fact that the anti-H. pylori IgA serological response is a less sensitive marker for H. pylori infection than anti-H. pylori IgG [45–47]. We assume that H. pylori infection as determined by the anti-H. pylori antibody response preceded typhoid fever infection, because it takes 1–3 months after H. pylori infection to develop anti-H. pylori IgG antibodies and typhoid fever cases were visited within 1 month after blood-culture confirmation of S. typhi infection [48]. Moreover, in some cases the antibiotic treatment of typhoid fever might have interfered with the quantitative anti-H. pylori IgA antibody response, because in H. pylori eradication studies IgA titres decreased faster than IgG 6 weeks after antibiotic treatment, but even then IgA (and IgG) titres will remain elevated during 6–12 months after eradication [37, 44, 47, 49]. Furthermore, samples for determination of plasma gastrin were obtained from non-fasting subjects, but the gastrin concentrations in our study showed little elevation compared to concentrations in a population sample in Mexico, where samples were taking in a fasting state and median serum gastrin amounted to 35 ng/l (IQR 26–52) [39]. Finally, we assume that the association of H. pylori infection as defined by anti-H. pylori IgG response and typhoid fever may be the result of shared risk factors for exposure to both bacteria. Infection with H. pylori occurs in early childhood within families [17, 20]. Several risk factors for H. pylori infection have been identified without determination of the exact source of infection, but most are associated with poor hygiene and sanitation within households, and could coincide with the intra-household risk factors for typhoid fever in Jakarta [17, 35]. The improvement of hygiene within households might, therefore, reduce the risk of exposure to both bacteria. Continuous exposure may also explain the correlation of age and the anti-H. pylori antibody AI in our study, similar to findings of Chen et al. [40].
In conclusion, our findings demonstrated that typhoid fever was associated with H. pylori IgG seropositivity, whereas the gastrin concentrations were not significantly higher in typhoid fever cases compared with healthy controls. The findings do not support the hypothesis that the association points to H. pylori-induced hypochlorhydria as a risk factor for typhoid fever, but suggest that the epidemiological association is probably confounded by shared risk factors for infection with both bacteria.
ACKNOWLEDGEMENTS
Financial support was provided by the Royal Netherlands Academy of Arts and Sciences (KNAW). We thank the physicians, nurses and technicians of the participating health centres in Jakarta for their cooperation: Mitra International Hospital and Microbiology Laboratory, Budhi Asih, St Carolus, Medistra and Persahabatan Hospital, all puskesmas in Jatinegara and the local private practitioners. We thank Wim van Duijn, Izäk Biemond and Johan van der Reijden, and Adriette de Visser from the LUMC Laboratory of Gastroenterology–Hepatology, and Infectious Diseases respectively. This study could not have been conducted without our research assistants in Jakarta.
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Crump JA, Luby SP, Mintz ED. The global burden of typhoid fever. Bull World Health Organ. 2004;82:346–353. [PMC free article] [PubMed] [Google Scholar]
- 2.Luby SP, Faizan MK, Fisher-Hoch SP et al. Risk factors for typhoid fever in an endemic setting, Karachi, Pakistan. Epidemiol Infect. 1998;120:129–138. doi: 10.1017/s0950268897008558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Swaddiwudhipong W, Kanlayanaphotporn J. A common-source water-borne outbreak of multidrug-resistant typhoid fever in a rural Thai community. J Med Assoc Thai. 2001;84:1513–1517. [PubMed] [Google Scholar]
- 4.King CC, Chen CJ, You SL, Chuang YC, Huang HH, Tsai WC. Community-wide epidemiological investigation of a typhoid outbreak in a rural township in Taiwan, Republic of China. Int J Epidemiol. 1989;18:254–260. doi: 10.1093/ije/18.1.254. [DOI] [PubMed] [Google Scholar]
- 5.Gasem MH, Dolmans WM, Keuter MM, Djokomoeljanto RR. Poor food hygiene and housing as risk factors for typhoid fever in Semarang, Indonesia. Trop Med Int Health. 2001;6:484–490. doi: 10.1046/j.1365-3156.2001.00734.x. [DOI] [PubMed] [Google Scholar]
- 6.Mermin JH, Villar R, Carpenter J et al. A massive epidemic of multidrug-resistant typhoid fever in Tajikistan associated with consumption of municipal water. J Infect Dis. 1999;179:1416–1422. doi: 10.1086/314766. [DOI] [PubMed] [Google Scholar]
- 7.Velema JP, van Wijnen G, Bult P, van Naerssen T, Jota S. Typhoid fever in Ujung Pandang, Indonesia-high-risk groups and high-risk behaviours. Trop Med Int Health. 1997;2:1088–1094. doi: 10.1046/j.1365-3156.1997.d01-179.x. [DOI] [PubMed] [Google Scholar]
- 8.Bhan MK, Bahl R, Sazawal S et al. Association between Helicobacter pylori infection and increased risk of typhoid fever. J Infect Dis. 2002;186:1857–1860. doi: 10.1086/345762. [DOI] [PubMed] [Google Scholar]
- 9.Black RE, Cisneros L, Levine MM, Banfi A, Lobos H, Rodriguez H. Case-control study to identify risk factors for paediatric endemic typhoid fever in Santiago, Chile. Bull World Health Organ. 1985;63:899–904. [PMC free article] [PubMed] [Google Scholar]
- 10.Dunstan SJ, Stephens HA, Blackwell JM et al. Genes of the class II and class III major histocompatibility complex are associated with typhoid fever in Vietnam. J Infect Dis. 2001;183:261–268. doi: 10.1086/317940. [DOI] [PubMed] [Google Scholar]
- 11.Dharmana E, Joosten I, Tijssen HJ et al. HLA-DRB1*12 is associated with protection against complicated typhoid fever, independent of tumour necrosis factor alpha. Eur J Immunogenet. 2002;29:297–300. doi: 10.1046/j.1365-2370.2002.00318.x. [DOI] [PubMed] [Google Scholar]
- 12.Kunz LJ, Waddell WR. Association of Salmonella enteritis with operations on the stomach. N Engl J Med. 1956;255:555–559. doi: 10.1056/NEJM195609202551203. [DOI] [PubMed] [Google Scholar]
- 13.Gianella RA, Broitman SA, Zamcheck N. Influence of gastric acidity on bacterial and parasitic enteric infections: a perspective. Ann Intern Med. 1973;78:271–276. doi: 10.7326/0003-4819-78-2-271. [DOI] [PubMed] [Google Scholar]
- 14.Gianella RA, Broitman SA, Zamcheck N. The gastric barrier to microorganisms in man: in vivo and in vitro studies. Gut. 1972;13:251–256. doi: 10.1136/gut.13.4.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Torres J, Perez-Perez G, Goodman KJ et al. A comprehensive review of the natural history of Helicobacter pylori infection in children. Arch Med Res. 2000;31:431–469. doi: 10.1016/s0188-4409(00)00099-0. [DOI] [PubMed] [Google Scholar]
- 16.Bardhan PK. Epidemiological features of Helicobacter pylori infection in developing countries. Clin Infect Dis. 1997;25:973–978. doi: 10.1086/516067. [DOI] [PubMed] [Google Scholar]
- 17.Frenck RW, Jr, Clemens J. Helicobacter in the developing world. Microbes Infect. 2003;5:705–713. doi: 10.1016/s1286-4579(03)00112-6. [DOI] [PubMed] [Google Scholar]
- 18.Blaser MJ. Hypothesis: the changing relationships of Helicobacter pylori and humans: implications for health and disease. J Infect Dis. 1999;179:1523–1530. doi: 10.1086/314785. [DOI] [PubMed] [Google Scholar]
- 19.Harford WV, Barnett C, Lee E, Perez-Perez G, Blaser MJ, Peterson WL. Acute gastritis with hypochlorhydria: report of 35 cases with long term follow up. Gut. 2000;47:467–472. doi: 10.1136/gut.47.4.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Suerbaum S, Michetti P. Helicobacter pylori infection. N Engl J Med. 2002;347:1175–1186. doi: 10.1056/NEJMra020542. [DOI] [PubMed] [Google Scholar]
- 21.El Omar EM, Carrington M, Chow WH et al. Interleukin-1 polymorphisms associated with increased risk of gastric cancer. Nature. 2000;404:398–402. doi: 10.1038/35006081. [DOI] [PubMed] [Google Scholar]
- 22.El Omar EM, Oien K, El Nujumi A et al. Helicobacter pylori infection and chronic gastric acid hyposecretion. Gastroenterology. 1997;113:15–24. doi: 10.1016/s0016-5085(97)70075-1. [DOI] [PubMed] [Google Scholar]
- 23.Gillen D, El Omar EM, Wirz AA, Ardill JE, McColl KE. The acid response to gastrin distinguishes duodenal ulcer patients from Helicobacter pylori-infected healthy subjects. Gastroenterology. 1998;114:50–57. doi: 10.1016/s0016-5085(98)70632-8. [DOI] [PubMed] [Google Scholar]
- 24.McColl KE, Gillen D, el Omar E. The role of gastrin in ulcer pathogenesis. Baillieres Best Pract Res Clin Gastroenterol. 2000;14:13–26. doi: 10.1053/bega.1999.0056. [DOI] [PubMed] [Google Scholar]
- 25.Shahinian ML, Passaro DJ, Swerdlow DL, Mintz ED, Rodriguez M, Parsonnel J. Helicobacter pylori and epidemic Vibrio cholerae O1 infection in Peru. Lancet. 2000;355:377–378. doi: 10.1016/s0140-6736(99)05143-0. [DOI] [PubMed] [Google Scholar]
- 26.Clemens J, Albert MJ, Rao M et al. Impact of infection by Helicobacter pylori on the risk and severity of endemic cholera. J Infect Dis. 1995;171:1653–1656. doi: 10.1093/infdis/171.6.1653. [DOI] [PubMed] [Google Scholar]
- 27.Sullivan PB, Thomas JE, Wight DG et al. Helicobacter pylori in Gambian children with chronic diarrhoea and malnutrition. Arch Dis Child. 1990;65:189–191. doi: 10.1136/adc.65.2.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rahman MM, Mahalanabis D, Sarker SA et al. Helicobacter pylori colonization in infants and young children is not necessarily associated with diarrhoea. J Trop Pediatr. 1998;44:283–287. doi: 10.1093/tropej/44.5.283. [DOI] [PubMed] [Google Scholar]
- 29.Kehrt R, Becker M, Brosicke H, Kruger N, Helge H. Prevalence of Helicobacter pylori infection in Nicaraguan children with persistent diarrhea, diagnosed by the 13C-urea breath test. J Pediatr Gastroenterol Nutr. 1997;25:84–88. doi: 10.1097/00005176-199707000-00014. [DOI] [PubMed] [Google Scholar]
- 30.Passaro DJ, Taylor DN, Meza R, Cabrera L, Gilman RH, Parsonnet J. Acute Helicobacter pylori infection is followed by an increase in diarrheal disease among Peruvian children. Pediatrics. 2001;108:E87. doi: 10.1542/peds.108.5.e87. [DOI] [PubMed] [Google Scholar]
- 31.Weaver LT. Royal Society of Tropical Medicine and Hygiene Meeting at Manson House, London, 16 February 1995. Aspects of Helicobacter pylori infection in the developing and developed world. Helicobacter pylori infection, nutrition and growth of West African infants. Trans R Soc Trop Med Hyg. 1995;89:347–350. doi: 10.1016/0035-9203(95)90002-0. [DOI] [PubMed] [Google Scholar]
- 32.Dale A, Thomas JE, Darboe MK, Coward WA, Harding M, Weaver LT. Helicobacter pylori infection, gastric acid secretion, and infant growth. J Pediatr Gastroenterol Nutr. 1998;26:393–397. doi: 10.1097/00005176-199804000-00006. [DOI] [PubMed] [Google Scholar]
- 33.Rothenbacher D, Blaser MJ, Bode G, Brenner H. Inverse relationship between gastric colonization of Helicobacter pylori and diarrheal illnesses in children: results of a population-based cross-sectional study. J Infect Dis. 2000;182:1446–1449. doi: 10.1086/315887. [DOI] [PubMed] [Google Scholar]
- 34.Perry S, Sanchez L, Yang S, Haggerty TD, Hurst P, Parsonnet J. Helicobacter pylori and risk of gastroenteritis. J Infect Dis. 2004;190:303–310. doi: 10.1086/421705. [DOI] [PubMed] [Google Scholar]
- 35.Vollaard AM, Ali S, van Asten HAGH et al. Risk factors for typhoid and paratyphoid fever in Jakarta, Indonesia. J Am Med Assoc. 2004;291:2607–2615. doi: 10.1001/jama.291.21.2607. [DOI] [PubMed] [Google Scholar]
- 36.Pena AS, Endtz HP, Offerhaus GJ et al. Value of serology (ELISA and immunoblotting) for the diagnosis of Campylobacter pylori infection. Digestion. 1989;44:131–141. doi: 10.1159/000199902. [DOI] [PubMed] [Google Scholar]
- 37.Veenendaal RA, Pena AS, Meijer JL et al. Long term serological surveillance after treatment of Helicobacter pylori infection. Gut. 1991;32:1291–1294. doi: 10.1136/gut.32.11.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jansen JB, Lamers CB. Effect of changes in serum calcium on secretin-stimulated serum gastrin in patients with Zollinger–Ellison syndrome. Gastroenterology. 1982;83:173–178. [PubMed] [Google Scholar]
- 39.Ley C, Mohar A, Guarner J et al. Screening markers for chronic atrophic gastritis in Chiapas, Mexico. Cancer Epidemiol Biomarkers Prev. 2001;10:107–112. [PubMed] [Google Scholar]
- 40.Chen TS, Li FY, Chang FY, Lee SD. Immunoglobulin G antibody against Helicobacter pylori: clinical implications of levels found in serum. Clin Diagn Lab Immunol. 2002;9:1044–1048. doi: 10.1128/CDLI.9.5.1044-1048.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hsu PI, Lai KH, Tseng HH et al. Correlation of serum immunoglobulin G Helicobacter pylori antibody titers with histologic and endoscopic findings in patients with dyspepsia. J Clin Gastroenterol. 1997;25:587–591. doi: 10.1097/00004836-199712000-00007. [DOI] [PubMed] [Google Scholar]
- 42.Kreuning J, Lindeman J, Biemond I, Lamers CB. Relation between IgG and IgA antibody titres against Helicobacter pylori in serum and severity of gastritis in asymptomatic subjects. J Clin Pathol. 1994;47:227–231. doi: 10.1136/jcp.47.3.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yamamoto I, Fukuda Y, Mizuta T, Fukada M, Nishigami T, Shimoyama T. Serum anti-Helicobacter pylori antibodies and gastritis. J Clin Gastroenterol. 1995;21:S164–S168. (Suppl 1): [PubMed] [Google Scholar]
- 44.Soto G, Bautista CT, Roth DE et al. Helicobacter pylori reinfection is common in Peruvian adults after antibiotic eradication therapy. J Infect Dis. 2003;188:1263–1275. doi: 10.1086/379046. [DOI] [PubMed] [Google Scholar]
- 45.Karvar S, Karch H, Frosch M, Burghardt W, Gross U. Use of serum-specific immunoglobulins A and G for detection of Helicobacter pylori infection in patients with chronic gastritis by immunoblot analysis. J Clin Microbiol. 1997;35:3058–3061. doi: 10.1128/jcm.35.12.3058-3061.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kolho KL, Korhonen J, Verkasalo M, Lindahl H, Savilahti E, Rautelin H. Helicobacter pylori serology at diagnosis and follow-up of biopsy-verified infection in children. Scand J Infect Dis. 2002;34:177–182. doi: 10.1080/00365540110080359. [DOI] [PubMed] [Google Scholar]
- 47.Kosunen TU, Seppala K, Sarna S, Sipponen P. Diagnostic value of decreasing IgG, IgA, and IgM antibody titres after eradication of Helicobacter pylori. Lancet. 1992;339:893–895. doi: 10.1016/0140-6736(92)90929-w. [DOI] [PubMed] [Google Scholar]
- 48.Sobala GM, Crabtree JE, Dixon MF et al. Acute Helicobacter pylori infection: clinical features, local and systemic immune response, gastric mucosal histology, and gastric juice ascorbic acid concentrations. Gut. 1991;32:1415–1418. doi: 10.1136/gut.32.11.1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cutler AF, Prasad VM, Santogade P. Four-year trends in Helicobacter pylori IgG serology following successful eradication. Am J Med. 1998;105:18–20. doi: 10.1016/s0002-9343(98)00134-x. [DOI] [PubMed] [Google Scholar]


