SUMMARY
More people with hepatitis C virus pass through incarcerated settings each year than any other venue. The goal of this study was to assess inmates’ attitudes towards hepatitis C testing and treatment while incarcerated. We interviewed 153 male and female inmates at the Rhode Island Department of Corrections (RIDOC). Ninety-one per cent of inmates said they would agree to be tested for hepatitis C and 95% said that they would be willing to be treated for hepatitis C while incarcerated. Thirty-three per cent perceived themselves to be at risk for hepatitis C. Inmates were very interested in hepatitis C testing and, if indicated treatment. Inmates’ attitudes towards hepatitis C testing and treatment do not pose a major obstacle to implementing comprehensive hepatitis C screening and treatment programme in correctional settings.
INTRODUCTION
Hepatitis C virus (HCV) is the most common chronic bloodborne infection in the United States [1]. An estimated 3·9 million (1·8%) Americans have been infected with hepatitis C [2]. There are 35 000 new HCV infections, and 10 000–12 000 deaths due to HCV each year and a predicted fourfold increase in the number of adults diagnosed with chronic HCV infection from 1990 to 2015 [3].
Although the population-wide prevalence of HCV is 1·8%, reported prevalence of HCV in prisons in California, Texas, and Rhode Island range from 27% to 49% [4–7]. Incarcerated persons report a higher prevalence of unsafe sexual practices and injection drug use than the population at large [8], behaviours that put them at risk for many diseases including hepatitis B and C, and human immunodeficiency virus (HIV). Eighty-three per cent of state and 73% of federal inmates surveyed in 1997 reported past drug use, and a majority reported drug use in the month before their offence [9].
The 2002 NIH consensus guidelines for the treatment of hepatitis C call for the establishment of screening tests for all groups at high risk of HCV infection including injecting drug users (IDUs) and incarcerated individuals [3]. The 2003 CDC report on the Prevention and Control of Infections with Hepatitis Viruses in Correctional Settings recommends that all inmates reporting risk factors for hepatitis be tested and treated based on current guidelines [10].
Prisons are ideal settings to access and efficiently screen and treat high-risk adults for hepatitis C for several reasons. First, high-risk adults are frequently incarcerated: a recent study found that 29–43% of all those infected with the hepatitis C virus in the country passed through a correctional facility in 1997 [11]. Second, medical infrastructure within prisons already exists, and adding hepatitis C testing and treatment would be a logical extension of existing protocols. Third, with the ongoing ‘War on Drugs’, such programmes have the potential to reach an even larger number of individuals [12]. The last two decades have witnessed an epidemic of incarceration – in 2002, more than two million inmates were incarcerated in adult correctional facilities, a 71% increase since 1990 [13]. The strictly structured atmosphere of correctional settings helps ensure that patients adhere to treatment protocols. Finally, patients can be treated during a period of sobriety, an issue that has been a challenge in the community setting [14].
An important benefit of identifying and treating HCV-infected individuals in prison is the ability to reach many people co-infected with hepatitis B or HIV, or with heavy alcohol intake, all of which worsen the natural course of HCV infection [14, 15]. We have previously documented high rates of co-infection in the Rhode Island prison population [7].
A critical component of implementing screening and treatment programmes in correctional settings is the inmates’ willingness to accept the testing and treatment. Our objective in this study was to evaluate the inmates’ attitudes towards hepatitis C testing and treatment at the Rhode Island Department of Corrections (RIDOC).
METHODS
The RIDOC is the only correctional facility in the state and serves as both a prison, housing sentenced inmates and a jail, detaining accused persons awaiting trial or convicted persons serving short-term sentences. It processes 15 000 intakes per year and has an average daily population of 3300 inmates, serving both short- and long-term sentences. In 2002, the inmate population was 51% white, 28% black, and 19% Hispanic. Ninety-four per cent were men, the average age was 33 years, and most of the population was aged between 20 and 39 years [16]. From June to the end of August 2002 we recruited and interviewed male and female adult inmates at the RI DOC as described elsewhere [17].
Briefly, participants were randomly selected from a comprehensive daily roster at two RIDOC facilities. Male inmates were selected from the Intake Service Center, which houses ∼1000 male inmates including pre-trial detainees, newly sentenced inmates awaiting classification to other facilities, those in pre-trial protective custody, and sentenced protective custody. Female inmates were selected from the Gloria McDonald Center which houses all 200 female inmates not in minimum security. Each day, we started with the inmate whose serial number corresponded to that day’s three-digit state lottery number. Every 100th male inmate and every 10th female inmate on the roster after that inmate was a candidate for recruitment that day. Each interview took ∼30 min and an average of seven interviews were conducted per day.
Written informed consent was obtained from each participant. Data were collected through a face-to-face interviewer-administered questionnaire. The questionnaire included demographic data, questions regarding hepatitis C status, self-perception of risk for hepatitis C, and questions about the participants’ willingness to accept testing and treatment for hepatitis C. Additionally, we asked participants about their drug use in order to assess risk behaviour. All data were self-reported and were not confirmed with blood tests or medical records. Individuals were considered to be at risk for hepatitis C infection if they reported ever injecting drugs [2]. No information regarding hepatitis B and C infection or treatment was given prior to the interview, but the interviewer reviewed risk factors, modes of transmission, benefits of vaccination, and treatment options and efficacy with each participant at the end of the interview.
Means are presented with standard deviations throughout. To test for differences between groups, we employed the independent-samples t test and the Pearson χ2. We considered alpha probabilities of <0·05 as statistically significant in two-tailed comparisons. All statistics were performed with Stata version 7 (StataCorp, College Station, TX, USA).
The study was approved by The Miriam Hospital Human Subjects Institutional Review Board with a prisoner representative.
RESULTS
Demographics and descriptive characteristics
Of 173 prisoners approached, 153 (88%) agreed to participate in the study. Study participants had similar demographic characteristics to the overall RIDOC populations except that women were over-sampled (data not shown). Demographic and descriptive characteristics are presented in Table 1. Thirty-five per cent (53/153) were women, and 65% (100/153) were men. The mean age of participants was 30·4±8·9 years. Forty-two per cent (64/153) were white, 37% (57/153) had less than a high school education. The median number of times participants had been incarcerated was two (range 1–60). Seventy-six per cent (116/153) had been incarcerated more than once. Forty-one per cent (63/153) reported having been in a short-term detoxification programme or a residential drug/alcohol treatment programme and 33% (51/153) reported having attended a sexually transmitted disease (STD) clinic.
Table 1.
Prisoners surveyed about hepatitis C, Rhode Island 2002
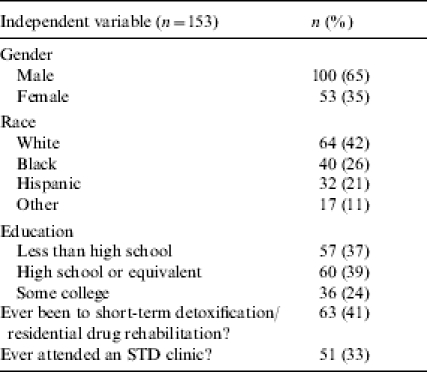
STD, Sexually transmitted disease.
Self-perception of risk vs. actual risk
When asked, ‘Do you perceive yourself to be at risk for hepatitis C?’, 33% (51/153) answered ‘yes’. Twenty-nine per cent (44/150) reported injecting drugs at some time in their lives, and 19% (28/150) had shared needles. Three participants did not complete the interview and, therefore, did not answer questions regarding drug use. Twelve per cent (18/153) of all inmates (44% of the 41 inmates who reported having been tested for hepatitis C) self-reported being HCV positive. Those who reported injecting drugs were more likely to perceive themselves at risk for hepatitis C (28/44; 64%) than those who did not report injecting drugs (22/106; 21%) (χ2=25·7, P<0·001).
Acceptance of hepatitis C testing and teatment
As presented in Table 2, 91% (139/153) of participants stated that they would be willing to be tested for hepatitis C while incarcerated. Three per cent (4/153) were undecided, and 6% (10/153) would not be willing to be tested while incarcerated. Of those who were unwilling, three stated that they knew they were not at risk, two already knew they were HCV positive, two had already been tested for HCV with negative results, two did not ‘trust the government’, and one did not want to know if he had a fatal illness.
Table 2.
Hepatitis C testing and treatment acceptance among Rhode Island prisoners, 2002
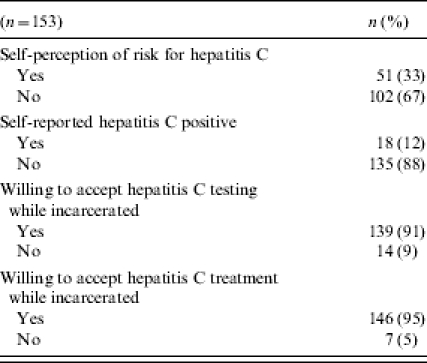
Ninety-five per cent (146/153) reported being willing to receive treatment for hepatitis C while incarcerated if they tested positive. One person was undecided and 4% (6/153) stated that they would not be willing to receive treatment for HCV while incarcerated. Among those who were not willing, two did not like the treatment, two did not trust the prison, one did not know enough about the treatment, and one did not give reasons. There were no significant differences between those who were willing to accept testing while incarcerated, and those who were not, in terms of age, gender, race, education, prior attendance at an STD clinic or drug use, or. However, those of a younger age, those with a college education, and those with a history of drug use were less likely to accept treatment for hepatitis C (See Table 3).
Table 3.
Characteristics of inmates accepting and not accepting hepatitis C testing and treatment, Rhode Island, 2002
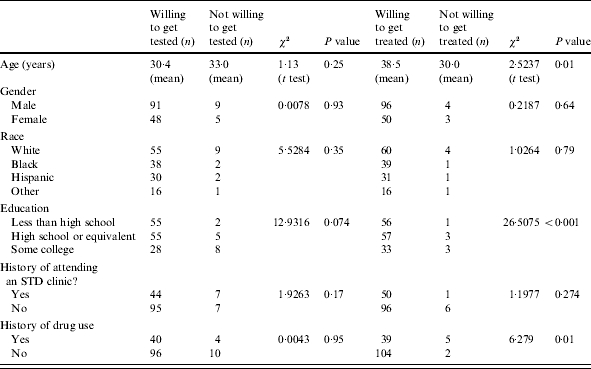
STD, Sexually transmitted disease.
DISCUSSION
This is the first study of inmates’ attitudes towards hepatitis C testing and treatment while incarcerated. The major finding of this study is that the vast majority of inmates reported a willingness to be tested and, if needed, subsequently treated for hepatitis C while incarcerated. This is important because of the high burden of disease among inmates and the tremendous opportunity to provide screening and treatment in correctional facilities. A study at a methadone maintenance programme where participants were informed of the specific risks, side-effects and efficacy of the treatment, found a lower acceptance rate (53%) for HCV treatment [18]. Increased knowledge of what the treatment entails may account for this difference in acceptance. However, acceptance levels may be higher in the correctional setting where daily survival needs such as housing, food, and drugs may be less pressing and inmates might be able to consider addressing a chronic infection such as hepatitis C.
A comprehensive testing, treatment, and prevention programme that includes education and counselling could have a substantial impact. Knowledge about hepatitis C could be increased simply by implementing testing and treatment programmes. A 2002 study conducted by Heimer et al. found that hepatitis C-associated knowledge among HIV-aware IDUs was low [19]. Participants in that study fared no better than random guessing on true/false questions with regards to their hepatitis knowledge. However, IDUs who received drug treatment services or hepatitis-specific medical care acquired and retained knowledge about hepatitis. Education and counselling complementary to testing and treatment can further aid in spreading primary and secondary prevention messages to both HCV-positive and HCV-negative inmates. Alcohol use is a major contributor to HCV-related cirrhosis. Screening coupled with alcohol-cessation counselling could aid in reducing the burden of liver disease related to HCV infection. Treatment programmes can address co-occurring disorders of mental illness and addiction, perhaps in a more controlled setting that in the community [14]. Implementation of such a comprehensive programme could take into account the characteristics of inmates less likely to accept treatment – younger age, higher education, and history of drug use – and could be tailored to address their concerns.
There are several potential obstacles to implementing hepatitis C testing and treatment programmes. First, correctional setting administrators might be reluctant to commit to a comprehensive programme for hepatitis C given the possibility of considerable costs to the prison system. However, HIV programmes, which were once thought of as too expensive for correctional systems have since been successfully implemented [20]. Additionally, recent lawsuits brought by prisoners against the correctional departments of Ohio and Oregon and elsewhere for failing to offer hepatitis C treatment might provide another impetus to implement such programmes [21, 22]. Second, treatment options for hepatitis C are costly, toxic, and have limited efficacy; however, better treatment may be coming soon. Third, finding out about their hepatitis C status in the incarcerated setting may cause further psychological distress in a population with an already high prevalence of mental illness. However, this study suggests that inmates are in fact willing and eager to learn of their HCV status, and if appropriate, consider treatment.
Limitations of this study include the fact that acceptance rates reported here may not reflect true acceptance rates because inmates were not actually offered the test or treatment – they were asked hypothetically if they would accept the test and treatment. Additionally, treatment acceptance rates might have been lower if the substantial side-effects and relatively low treatment efficacy had been discussed prior to administering the questionnaire. Despite acceptance, all those willing to undergo hepatitis C treatment may not receive treatment given limitations of length of incarceration and pre-existing comorbid conditions. However, as treatment options improve, these limitations may no longer play a significant role in the decision to treat inmates with hepatitis C. Our results may also be unique to the correctional setting in Rhode Island; however, since our sample was a random representation of the incarcerated population, no obvious bias seems to have been introduced. The validity of self-reported risk behaviour is often questioned, particularly in the prison setting, and we expect that levels of needle sharing reported here might be lower than actual levels, and as a result, our estimation of risk would in fact be conservative.
CONCLUSION
Hepatitis C infection among high-risk adults, including those who are incarcerated, is a significant problem. Correctional settings provide unique opportunities to offer testing, treatment, and preventive services to a substantial portion of high-risk adults. A major challenge to implementing screening and treatment for hepatitis C is the concern of correctional administration about the increased cost to correctional medical budgets to provide these services. Inmate attitudes towards accepting testing and treatment do not appear to pose major obstacles to implementing a screening, treatment, and prevention programme.
ACKNOWLEDGEMENTS
The project described was supported by a Brown Medical School Research Fellowship; by grant number P30-AI-42853 from the National Institutes of Health, Center for AIDS Research (NIH CFAR); and grant number U50 CUU119078 from the Centers for Disease Control (CDC). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the awarding agencies. The authors thank Scott Allen of the Rhode Island Department of Corrections for his assistance.
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Centers for Disease Control and Prevention. Recommendations for prevention and control of hepatitis C virus and infection and HCV related chronic disease. http://www.cdc.gov/mmwr/preview/mmwrhtml/00055154.htm. Morb Mortal Wkly Rep. 1998;47:1–39. ). Accessed 28 July 2003. [Google Scholar]
- 2.Centers for Disease Control and Prevention. http://www.cdc.gov/ncidod/diseases/hepatitis/c/fact.htm. http://www.cdc.gov/ncidod/diseases/hepatitis/c/fact.htm Viral hepatitis C fact sheet. ). Accessed 8 July 2003.
- 3.NIH Consensus Statement. 2002. http://consensus.nih.gov/cons/116/Hepc091202.pdf. pp. 10–12.http://consensus.nih.gov/cons/116/Hepc091202.pdf Management of hepatitis C. June 2002, vol. , no. ). Accessed 8 July 2003.
- 4.Spaulding A, Greene C, Davidson K, Schneidermann M, Rich J. Hepatitis C in state correctional facilities. Prev Med. 1999;28:92–100. doi: 10.1006/pmed.1998.0418. [DOI] [PubMed] [Google Scholar]
- 5.Baillargeon J, Wu H, Kelley MJ, Grady J, Linthicum L, Dunn K. Hepatitis C seroprevalence among newly incarcerated inmates in the Texas correctional system. Public Health. 2003;117:43–48. doi: 10.1016/s0033-3506(02)00009-4. [DOI] [PubMed] [Google Scholar]
- 6.Macalino GE, Salas CM, Towe CW Incidence and community prevalence of HIV and other blood borne pathogens among incarcerated women in Rhode Island. Presentation at 1999 National HIV Prevention Conference (Abstract 610)
- 7.Macalino G, Vlahov D, Sanford S et al. Prevalence and incidence of human immunodeficiency virus, hepatitis B and C virus infections among males in Rhode Island prisons. Am J Public Health. 2004;94:1218–1223. doi: 10.2105/ajph.94.7.1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Glasser J, Greifinger B. Correctional health care: a public health opportunity. Ann Intern Med. 1993;118:139–145. doi: 10.7326/0003-4819-118-2-199301150-00010. [DOI] [PubMed] [Google Scholar]
- 9.Mumola CJ. Substance abuse and treatment, state and federal prisoners. Washington, DC: US Department of Justice; 1997. Bureau of Justice Statistics Special Report. Office of Justice Programs, 1999. Publication No. NCJ 172871. [Google Scholar]
- 10.Centers for Disease Control and Prevention. Prevention and control of infections with hepatitis viruses in correctional settings. http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5201a1.htm. Morb Mortal Wkly Rep. 2003;52 ). Accessed 30 July 2003. [PubMed] [Google Scholar]
- 11.Hammett TM, Harmon MP, Rhodes W. The burden of infectious disease among inmates of and releases from US correctional facilities, 1997. Am J Public Health. 2002;92:1789–1794. doi: 10.2105/ajph.92.11.1789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Drucker E. Drug prohibition and public health: 25 years of evidence. Public Health Rep. 1999;114:14–29. doi: 10.1093/phr/114.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bureau of Justice Statistics. 2003. www.ojp.usdoj.gov/bjs/abstract/pjim02.htm. www.ojp.usdoj.gov/bjs/abstract/pjim02.htm Prison and jail inmates at midyear 2002, NCJ 198877. ). Accessed 15 December 2003.
- 14.Allen SA, Spaulding A, Osei AM, Taylor LE, Cabral AM, Rich JD. Treatment of chronic hepatitis C in a state correctional facility. Ann Intern Med. 2003;138:187–191. doi: 10.7326/0003-4819-138-3-200302040-00010. [DOI] [PubMed] [Google Scholar]
- 15.Thomas D. Hepatitis C and Human Immunodefeciency Virus infection. Hepatology. 2002;36:S201–S209. doi: 10.1053/jhep.2002.36380. (Suppl 1): [DOI] [PubMed] [Google Scholar]
- 16.Wall AT. http://www.doc.state.ri.us/pdf/2002yearend.pdf. http://www.doc.state.ri.us/pdf/2002yearend.pdf Rhode Island Department of Corrections year end report, calendar year 2002. Rhode Island Department of Corrections. ). Accessed 15 August 2003.
- 17.Vallabhaneni S, Macalino GE, Reinert SE, Schwartzapfel B, Wolf FA, Rich JD. Prisoners’ attitudes toward hepatitis B vaccination. Prev Med. 2004;38:828–833. doi: 10.1016/j.ypmed.2003.12.024. [DOI] [PubMed] [Google Scholar]
- 18.Stein MD, Maksad J, Clarke J. Hepatitis C disease among injection drug users: knowledge, perceived risk and willingness to receive treatment. Drug Alcohol Depend. 2001;61:211–215. doi: 10.1016/s0376-8716(00)00144-7. [DOI] [PubMed] [Google Scholar]
- 19.Heimer R, Clair S, Grau L, Bluthental R, Marshall P, Singer M. Hepatitis associated knowledge is low and risks are high among HIV-aware injection drug users in three US cities. Addiction. 2002;97:1277–1287. doi: 10.1046/j.1360-0443.2002.t01-1-00211.x. [DOI] [PubMed] [Google Scholar]
- 20.Desai AA, Latta ET, Spaulding A, Rich JD, Flanigan TP. The importance of routine HIV testing in the incarcerated population: the Rhode Island experience. AIDS Educ Prev. 2002;14:45–52. doi: 10.1521/aeap.14.7.45.23867. (5 Suppl B): [DOI] [PubMed] [Google Scholar]
- 21.Ludlow R. 2003. Federal Court filing: state sued over inmates’ health care. The Columbus Dispatch (Ohio), 27 August. . Sect. A:1.
- 22.Gustafson A. http://www.hivandhepatitis.com/hep_c/news/050703a.html. http://www.hivandhepatitis.com/hep_c/news/050703a.html Class-action lawsuit by inmates demands treatment for hepatitis C. Associated Press, 5 May 2003 ( ). Accessed 17 January 2004.


