SUMMARY
We examined the epidemiology of community-acquired bacterial meningitis among adults in England and Wales between 1991 and 2002. Among 3169 cases, meningococcal infection was predominant among young adults and pneumococcal meningitis among older adults. Whilst infection due to most causes decreased, the incidence of tuberculous (TB) meningitis doubled over the 12 years. The mortality rate among meningococcal and pneumococcal infections fell from 0·45/105 to 0·31/105 (P=0·0001). This study demonstrates important changes in the epidemiology of bacterial meningitis among UK adults. Improvements in clinical management, childhood vaccination programmes and the re-emergence of tuberculosis are likely to be drivers of these changes.
The introduction of meningococcal, pneumococcal and Haemophilus influenzae type b (Hib) vaccines in many industrialized countries has resulted in a marked decline of these infections in children. The spectrum of meningitis in adults may also have undergone changes due to an ageing population and to the recent resurgence of tuberculosis [1]. In addition, vaccination of the paediatric population may have reduced carriage of common causative pathogens and, therefore, also had an impact on adult disease. Recognition of these changes is important to inform clinical management and vaccination strategies, we therefore carried out a study of bacterial meningitis among adults in England and Wales.
Subjects included any adult (aged ⩾16 years) with community-acquired bacterial meningitis or meningococcal septicaemia diagnosed between January 1991 and December 2002 in England and Wales. Specifically we examined the following common causes of community-acquired bacterial meningitis: Neisseria meningitidis, Streptococcus pneumoniae, Haemophilus influenzae, Listeria monocytogenes, Mycobacterium tuberculosis, Group B streptococcus, and Escherichia coli [2]. In view of the considerable clinical overlap between meningitis and septicaemia in meningococcal infection [3], data on meningococcal septicaemia was also collected.
Data from laboratory reports and statutory notifications of meningitis and meningocccal septicaemia in England and Wales were obtained from the Health Protection Agency Centre for Infections. We also examined death registrations to the Office for National Statistics under the relevant ICD 9 and 10 codes from January 1993 to December 2002. Statutory notifications and death registrations, both based on reported clinical and/or laboratory diagnosis, were available for meningitis caused by S. pneumoniae, N. meningitidis. M. tuberculosis and H. influenzae. Differentiation between meningococcal meningitis and septicaemia was based on the reported diagnosis for notifications and death registrations, and on specimen (blood or CSF) for laboratory reports. Where blood and CSF were both positive, we recorded the diagnosis as meningitis.
We used the laboratory reports to examine the incidence of the disease as the main outcome measure and compared this to the incidence calculated using the clinical notifications for respective causative organisms. We calculated incidence rates using mid-year population data for each year. We used Poisson regression to examine changes in the incidence rate over time and by age groups; negative binomial regression was used with overdispersed data (Stata™ version 8, StataCorp, College Station, TX, USA). Case-fatality ratios were estimated by dividing number of death registrations by number of laboratory reports. Epi-Info version 3.2 (CDC, Atlanta, GA, USA) was used to test for trends between years and age group for fatality.
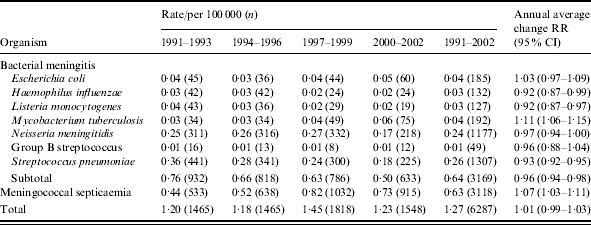
The mean annual incidence of community-acquired adult bacterial meningitis from laboratory reports was 0·6/105 (Table). S. pneumoniae and N. meningitidis together accounted for 78% of cases. Invasive disease (meningitis and septicaemia combined) due to N. meningitidis rose to a peak in 1997–1999 and then declined. Tuberculous (TB) meningitis doubled in incidence over the study period, whereas incidence of meningitis caused by S. pneumoniae, H. influenzae and L. monocytogenes decreased. The average annual incidence rates calculated using laboratory reports or clinical notifications as the numerator were similar for S. pneumoniae, H. influenzae, L. monocytogenes and meningococcal disease as a whole. However, the mean annual incidence rates for meningococcal meningitis were markedly different, such that meningococcal meningitis on clinical notifications showed over three times higher rates in contrast to laboratory reports (0·92/105vs. 0·24/105).
Table.
Incidence of bacterial meningitis and meningococcal septicaemia in adults in England and Wales 1991–2002
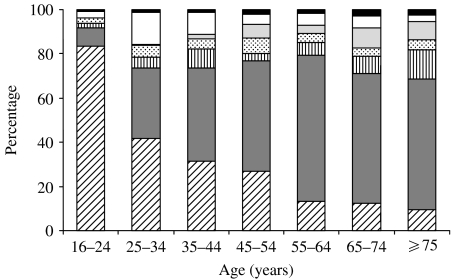
The main pathogen responsible for meningitis in young adults was N. meningitidis, comprising 84% (652/780) of cases in the 16–24 years age group (Fig.). This proportion decreased with increasing age to 10% (31/322) in >75 years age group (P<0·0001). By contrast, the equivalent proportions for S. pneumoniae increased from 8% (63/780) to 59% (190/322, P<0·0001), and for E. coli from 2% (16/780) to 13% (43/322, P<0·0001). Analysis of age-specific incidence revealed a significant increasing trend with age for E. coli, L. monocytogenes and S. pneumoniae and Group B streptococci (all P values <0·001).
Fig.
Proportionate distribution of causative organism of bacterial meningitis by age. ▪, Group B streptococcus; □, M. tuberculosis;  , L. monocytogenes;
, L. monocytogenes;  , H. influenzae;
, H. influenzae;  , E. coli;
, E. coli;  , S. pneumoniae;
, S. pneumoniae; , N. meningitidis.
, N. meningitidis.
Estimated case-fatality ratio for pneumococcal meningitis fell from 69% (172/250) in 1993–1994 to 52% (76/147) in 2001–2002 (P<0·0001). Mortality rates showed a similar downward trend to that for case fatality, falling from 0·21/105 to 0·09/105 in the same period (P<0·0001). Case fatality for meningococcal septicaemia also decreased over the same period [48% (162/340) to 27% (148/554), P<0·0001] but the ratio for meningococcal meningitis remained at about the same level (mean 18%). Combined mortality rates for pneumococcal and meningococcal meningitis (with meningococcal septicaemia) fell from 0·45/105 to 0·31/105 (P=0·0001) during a time when incidence rates for these infections were not falling. Case fatality for TB meningitis also fell, from 83% (20/24) in 1993–1994 to 34% (19/56) in 2001–2002 (P<0·0001), mainly due to falling mortality in the <65 years age group.
Apart from a peak of meningococcal disease during the recognized national epidemic in the late 1990s and a steady increase in TB meningitis, we found a falling incidence in bacterial meningitis among adults and falling mortality rates. The case-fatality figures were higher than expected [4]; the most likely explanation is an underestimate of the true number of cases in the laboratory surveillance data compared to that in death registration data. Over the last two decades there has been a global resurgence of tuberculosis [1]. The doubling in incidence of TB meningitis over the 12 years of this study is worrying. TB meningitis is more likely to be associated with HIV co-infection and those who survive have a high morbidity. Although multidrug-resistant tuberculosis remains uncommon in the United Kingdom, should this emerge amongst an enlarging population of meningitis cases, the results would be devastating. The decline in invasive H. influenzae infection after the introduction of routine Hib vaccination has been dramatic amongst paediatric populations. We showed a reduction in the incidence of H. influenzae meningitis amongst an adult population who would not have received Hib vaccine, probably due to herd immunity [5, 6].
This study provides evidence that the epidemiology of bacterial meningitis is changing among adults in the United Kingdom. Vaccination programmes in children and the re-emergence of tuberculosis appear to be making impacts in opposing directions. The falling mortality rate is encouraging and suggests that standards of clinical management may be improving, but still bacterial meningitis results in considerable morbidity and mortality. A high index of clinical suspicion for meningitis among adult patients should be maintained.
ACKNOWLEDGEMENTS
We thank Information officers at CDSC, Colindale London: Mrs H. Heine, Mr E. Yusuf, Ms U. Gungabissoon, and Mr D. Harding for providing us with the data. We are very grateful to Dr R George for his comments on the manuscript. The study received financial support from the Department of Health, UK. The Department of Health had no role in the design of the study; the data collection, analysis, or interpretation; or in the decision to publish the manuscript. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
DECLARATION OF INTEREST
None.
References
- 1.Rose AM, Watson JM, Graham C et al. Tuberculosis at the end of the 20th century in England and Wales: results of a national survey in 1998. Thorax. 2001;56:173–179. doi: 10.1136/thorax.56.3.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Durand ML, Calderwood SB, Weber DJ et al. Acute bacterial meningitis in adults: a review of 493 episodes. N Engl J Med. 1993;328:21–28. doi: 10.1056/NEJM199301073280104. [DOI] [PubMed] [Google Scholar]
- 3.Ramsay M, Kaczmarski E, Rush M, Mallard R, Farrington P, White J. Changing patterns of case ascertainment and trends in meningococcal disease in England and Wales. Commun Dis Rep CDR Rev. 1997;7:R49–R54. [PubMed] [Google Scholar]
- 4.Gjini A, Stuart JM, George RC et al. Under ascertainment of adult pneumococcal meningitis in England – implications for vaccine policy. Emerg Infect Dis. 2004;10:87–93. doi: 10.3201/eid1001.030123. [DOI] [PubMed] [Google Scholar]
- 5.Maclehose L, McKee M, Weinberg J. Responding to the challenge of communicable disease in Europe. Science. 2002;295:2047–2050. doi: 10.1126/science.1070025. [DOI] [PubMed] [Google Scholar]
- 6.McVernon J, Trotter CL, Slack MP, Ramsay ME. Trends in Haemophilus influenzae type b infections in adults in England and Wales: surveillance study. BMJ. 2004;329:655–658. doi: 10.1136/bmj.329.7467.655. [DOI] [PMC free article] [PubMed] [Google Scholar]