SUMMARY
We used molecular subtyping to investigate an outbreak of listeriosis involving residents of 24 US states. We defined a case as infection with Listeria monocytogenes serotype 4b yielding one of several closely related patterns when subtyped by pulsed-field gel electrophoresis. Patients infected with strains yielding different patterns were used as controls. A total of 108 cases were identified with 14 associated deaths and four miscarriages or stillbirths. A case-control study implicated meat frankfurters as the likely source of infection (OR 17·3, 95% CI 2·4–160). The outbreak ended abruptly following a manufacturer-issued recall, and the outbreak strain was later detected in low levels in the recalled product. A second strain was recovered at higher levels but was not associated with human illness. Our findings suggest that L. monocytogenes strains vary widely in virulence and confirm that large outbreaks can occur even when only low levels of contamination are detected in sampled food. Standardized molecular subtyping and coordinated, multi-jurisdiction investigations can greatly facilitate detection and control of listeriosis outbreaks.
INTRODUCTION
Listeria monocytogenes is a foodborne pathogen that causes febrile gastroenteritis in healthy individuals and life-threatening invasive infections in neonates, elderly and immunocompromised persons [1–5]. The organism is widely distributed in the environment, and control is hampered by its ability to grow at refrigerator temperatures [6]. Many different foods have been identified as potential sources of human infection, especially processed meats, dairy products, and seafood [6–9]. Human cases are often dispersed geographically, complicating the detection, investigation, and control of outbreaks [9, 10].
We describe a nationwide outbreak of listeriosis linked to contaminated frankfurters and deli meats made at a single facility. With over 100 reported cases and 14 fatalities, this is the second largest outbreak of listeriosis in US history. The outbreak investigation combined for the first time molecular subtyping of L. monocytogenes isolates and an epidemiological approach in which patients infected with non-outbreak strains served as controls. Findings from the investigation helped prompt new regulations for the control of Listeria in ready-to-eat meat and poultry products in the United States [11].
METHODS
Case finding and laboratory investigation
In November, 1998, following reports of small clusters of listeriosis cases in Connecticut, New York, Ohio and Tennessee, the Centers for Disease Control and Prevention (CDC) alerted all US state health departments and requested that recent L. monocytogenes isolates be forwarded to CDC for molecular subtyping through the National Molecular Subtyping Network for Foodborne Pathogens (PulseNet). This request was later expanded to include all isolates from January 1998 to the end of July 1999. Isolates were confirmed by AccuProbe DNA probe test (Gen-probe, San Diego, CA, USA), serotyped using standard methods [12] and subtyped by pulsed-field gel electrophoresis (PFGE) using AscI and ApaI restriction endonucleases and a standard protocol [13]. For case finding and analytical purposes, the outbreak strain was defined as an isolate that yielded a specific pattern when digested with AscI (PulseNet pattern number GXA16.0002) and any of three closely related patterns when digested with ApaI (GXA12.002, GX6A12.0003, GX6A12.0057) [14]. In addition, a subset of isolates were subtyped at the Cornell University Food Safety Laboratory using automated ribotyping combined with a polymerase chain reaction restriction fragment polymorphism analysis of the hly virulence gene [15].
Epidemiological investigation
To identify risk factors for infection, we initiated a telephone survey on 12 November 1998. All living residents of Connecticut, New York, Ohio and Tennessee with culture-confirmed listeriosis since 1 August 1998, were interviewed using a written questionnaire. Respondents were asked about consumption of many foods, including frankfurters but not sliced deli meats. On 4 December, we initiated a second survey which included questions about sliced deli meats. The second survey was limited to persons who had not been interviewed during the first survey. For both surveys, responses of patients infected with the outbreak strain (cases) were compared with responses of patients infected with other strains (controls) as determined by PFGE. Perinatal infection was defined as culture-confirmed infection in a pregnant woman or a newborn. Statistical analyses for both surveys were performed by one of us (M.P.) using Epi-Info version 6.04 (CDC, Atlanta, GA, USA) and SAS version 6.12 (SAS Institute Inc., Cary, NC, USA). Fisher’s exact test was used for determining statistical significance when an expected cell size was <5. All reported P values are two-tailed.
Environmental investigation
An environmental investigation was conducted at Plant A, located in Michigan. The plant is one of several large facilities owned by Company S where frankfurters and deli meats of various brand names are produced. The environmental investigation included a review of production practices, maintenance and product distribution records, and the results of environmental microbiological monitoring by plant personnel. Environmental swabs and unopened packages of frankfurters and deli meat from the Plant A ‘shelf-life’ stock were collected and transported on ice to CDC. Food samples were cultured for L. monocytogenes using standard United States Department of Agriculture (USDA) methods [16]. L. monocytogenes isolates from foods were confirmed, serotyped; and subtyped as previously described [13]. Environmental swabs were cultured at CDC using enrichment and direct plating [16].
RESULTS
Case finding and laboratory investigation
Isolates from 447 cases of listeriosis with onset between 1 January 1998 and 31 July 1999 were tested in conjunction with this investigation; 108 (24%) yielded PFGE patterns consistent with the outbreak strain and all were serotype 4b, with the exception of one isolate that could not be serotyped [14]. The remaining 339 isolates submitted during this investigation were of various serotypes (1/2a, 1/2b, 1/2c, 3a, 3b, 4b) and yielded a diverse array of PFGE patterns.
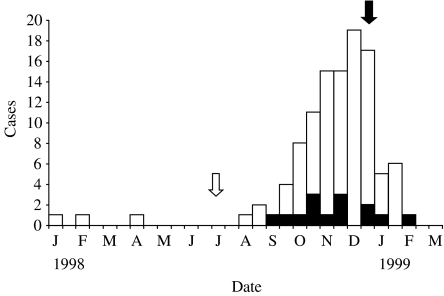
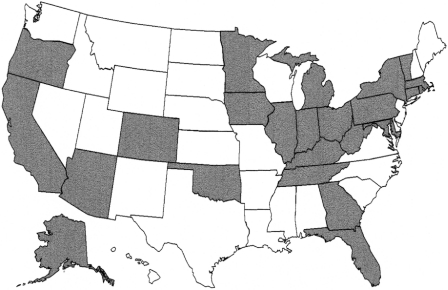
Among 108 patients infected with the outbreak strain, dates of illness onset ranged from 15 January 1998 to 8 February 1999, with most cases occurring between August 1998 and January 1999 (Fig. 1). Cases were reported among residents of 24 states (Fig. 2), including some states in which listeriosis was not officially designated a reportable condition. Perinatal infections accounted for 13 cases; patients with non-perinatal infection were a median of 70 years old (range 5–94 years) and 48% were female. Fourteen adult deaths and four miscarriages or stillbirths were reported among patients infected with the outbreak strain.
Fig. 1.
Dates of illness onset for fatal (■) and non-fatal (□) cases of listeriosis caused by the outbreak strain, United States, January 1998 to April 1999. Dark arrow indicates recall of frankfurters and deli meats. Light arrow indicates removal of refrigeration unit from the frankfurter production area of Plant A.
Fig. 2.
States with residents infected with the outbreak strain of Listeria monocytogenes, July 1998 to April 1999.
Information on underlying medical conditions was available for 43 patients with non-perinatal infection, including 25 infected with the outbreak strain and 18 infected with other strains. The most common underlying condition was hypertension, followed by diabetes and malignancy (Table 1). Only two (5%) of the 43 patients were younger than 65 years old and had no known immunocompromising condition. There were no marked differences between the two groups of patients with respect to underlying condition.
Table 1.
Underlying medical conditions among non-pregnant patients with Listeria monocytogenes infection; Connecticut, Ohio, New York, Tennessee, September–December 1998
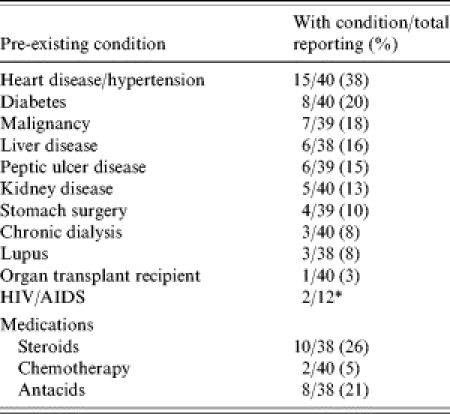
Percent not calculated due to low response rate.
Epidemiological investigation
Forty-one patients were interviewed in the first survey: 20 infected with the outbreak strain and 21 infected with other strains of L. monocytogenes. Case-patients were significantly more likely to report eating cooked frankfurters in the 4 weeks before becoming ill (OR 17·3, 95% CI 2·4–160·0, P<0·0004). Overall, 16 of 18 (89%) case-patients reported eating frankfurters, compared with 6 of 19 (32%) control patients (Table 2). By univariate analysis, case-patients were also more likely to report eating beef and ham; however, these associations were not statistically significant after controlling for frankfurter consumption. Although some control-patients reported eating frankfurters straight from the packet, all 16 case-patients specifically reported eating frankfurters that had been cooked or reheated.
Table 2.
Univariate analysis of food exposures among persons with listeriosis caused by the outbreak strain (cases) and other strains (controls)
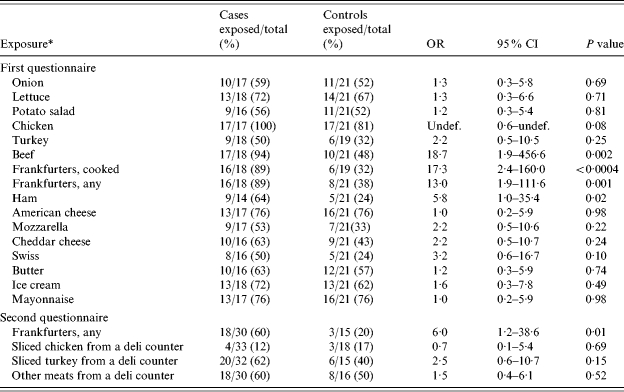
OR, Odds ratio; CI, confidence interval.
Data for foods eaten by <50% of persons infected with the outbreak strain not shown.
In the second survey, we interviewed 30 additional case-patients and 15 controls infected with other strains of L. monocytogenes. Infection with the outbreak strain was again associated with eating frankfurters (OR 6·0, 95% CI 1·2–38·6, P=0·01). Persons eating turkey cold cuts sliced at a deli were slightly more likely to be infected with the outbreak strain than with other strains; however, this association was not statistically significant (Table 2).
Among 16 case-patients interviewed in the first survey who remembered eating frankfurters, 14 (88%) recalled the brand name, and 11 (78%) of these reported eating brands made by Company S. A package of leftover Company S frankfurters recovered from one case-patient’s refrigerator bore the specific establishment number for the Company’s Michigan facility, Plant A. Including responses from both the first and second survey, 44 of 50 case-patients were interviewed before Company S announced a recall. Thirteen (30%) specifically reported eating brands of frankfurters or deli meats that are made at Plant A; nine (20%) could not remember the brand but reported eating frankfurters or deli meats purchased at a store that sold meats made at Plant A; 19 (43%) reported eating frankfurters or deli meats but could not identify the brand or a specific source; and two (4%) were unsure if they had eaten frankfurters or deli meats. Only one person (2%) denied eating frankfurters or deli meats in the 4 weeks before becoming ill.
Coincident with patient interviews, a review of L. monocytogenes isolates submitted to the Cornell Food Safety Laboratory identified two isolates from foods associated with human illness that matched the outbreak strain by PFGE and EcoRI ribotyping. These isolates had been obtained from two brands of deli meat eaten by members of the same family, three of whom developed severe febrile gastroenteritis the following day. Although a specific diagnosis was not made at the time of hospitalization, convalescent serum from one ill family member was later tested at CDC and yielded high titres of anti-listeriolysin O antibodies, consistent with acute illness due to L. monocytogenes [4, 17]. One of the deli meats was breast of chicken manufactured at Plant A; the second was smoked turkey made by another company but sliced on the same machine at the time of purchase.
Because many patients had recurrent exposures to implicated products, few data are available to determine the incubation period. In at least one case, an elderly man developed invasive listeriosis with the outbreak strain within 48 h of eating Plant A deli meat at a college reunion; cultures of the leftover meat yielded that outbreak strain [14]. Following the recall of the Plant A products, cases declined >60% within 1 week (Fig. 1). Among cases occurring after the recall, the median time period between recall and illness onset was 5 days for 12 cases involving non-pregnant individuals, compared with 25 days for four cases associated with pregnancy.
Environmental investigation
At Plant A, frankfurters are made by cooking a meat emulsion in casings, partially cooling, and slitting the casings. As the casings are removed, the bare frankfurters are collected on conveyor belts in a humid, refrigerated ‘hopper’ room before packaging. This room is the only area where the frankfurters have direct contact with machinery.
In early July 1998, a large ceiling refrigeration unit in the frankfurter hopper room was cut into pieces with a chain saw and removed as part of an equipment upgrade. Environmental monitoring records revealed that during the 6 weeks before removal of the refrigeration unit, only three (25%) of 12 swabs of food contact surfaces on the retail frankfurter line tested positive for psychrophilic organisms, a marker for potential L. monocytogenes contamination. In contrast, 11 (92%) of 12 swabs tested positive during the 6 weeks immediately following the demolition of the unit. The number of positive product contact surfaces continued to be high in subsequent weeks, with 16 (67%) of 24 samples collected between 20 August and 3 November testing positive. Positive tests also increased for several other production lines following the refrigeration unit removal, including lines used to produce deli meat. Results of environmental testing for the previous year were not available for comparison.
Fifteen packages of Plant A meats were ultimately available for culture, including eight packages of frankfurters and seven packages of deli meat. L. monocytogenes serotype 4b was isolated from six meat packages with sell-by-dates ranging from June to December 1998 (sell-by-dates for frankfurters are typically 60–90 days after the date of production): unopened package of frankfurters obtained from the manufacturer, four opened packages of frankfurters obtained from patients, and one opened package of deli meat. When subtyped, all six isolates yielded patterns consistent with the outbreak strain [14]. In addition, three serotype 1/2a isolates were recovered from packages of deli meat. PFGE patterns for these three isolates were indistinguishable from one another but distinct from the outbreak strain and all 447 clinical isolates tested during the investigation. In quantitative cultures, the serotype 1/2a strain was detected at levels as high as 3000 c.f.u./g meat, while the serotype 4b isolates were present in quantities of <0·3 c.f.u./g meat [14]. None of 31 environmental swabs yielded L. monocytogenes; these were collected after the facility had enhanced sanitation efforts.
DISCUSSION
This nationwide outbreak of listeriosis was caused by contaminated ready-to-eat meats produced at a single facility. Support for this conclusion includes (1) a statistical association between eating frankfurters and infection with the outbreak strain, (2) recovery of Plant A frankfurters from patients’ refrigerators, (3) isolation of the outbreak strain from unopened and opened packages of Plant A frankfurters and deli meats, and (4) abrupt termination of the outbreak after 35 million lb [18] of Plant A meat products were recalled. Overall, 108 persons were infected with the outbreak strain, resulting in 14 deaths and four miscarriages or stillbirths In addition, at least three persons developed acute febrile gastroenteritis after eating Plant A deli meats. It is likely that additional illnesses occurred but were not identified.
Demolition within the processing facility may have played an important role in triggering this outbreak (Fig. 1). We postulate that the outbreak strain had previously colonized a ceiling refrigeration unit in the frankfurter hopper room and that its removal led to increased contamination of production equipment, environmental surfaces, and the meats produced thereafter. Findings supporting this hypothesis include recovery of the outbreak strain from frankfurters produced well before the recognized outbreak, the marked and persistent increase in psychrophilic organisms on production equipment immediately following the demolition, and the subsequent surge in human cases detected. Persistence of L. monocytogenes strains within food production facilities has been documented [19, 20], and refrigeration units and environmental disturbances have been implicated in other listeriosis outbreaks (CDC, unpublished data).
As previous studies have linked listeriosis to eating frankfurters that have not been cooked or reheated [21, 22], it is noteworthy that all of our case-patients specifically reported eating frankfurters that had been cooked. One possible explanation is that they had not heated the frankfurters sufficiently to kill the organism. Alternately, it is possible that patients became infected by eating other foods cross-contaminated during preparation or storage in the home [22, 23]. The fluid in some frankfurter packages can support high concentrations of L. monocytogenes [24]. Unlike the bloody fluid in raw meat packages, this clear fluid may be perceived as safe by consumers, increasing the likelihood that cross-contamination will occur. Given that several control-patients reported eating uncooked frankfurters, we have no reason to believe that case-patients would be unwilling to admit this practice.
Our findings suggest that the average incubation period for invasive listeriosis is shorter than generally assumed. Much of the literature estimates the incubation period at 3–4 weeks, with a range of 11–70 days in one study [3, 25, 26]. However, these estimates rely heavily on studies involving pregnant women. In this investigation, new infections among non-pregnant patients ceased an average of 5 days following the recall of Plant A products, compared to 25 days for pregnant patients. In addition, one elderly man developed invasive listeriosis within 48 h of a single exposure to contaminated meat; other cases with similarly short incubation periods have been previously reported [27, 28]. It may be that pregnant women generally do not come to medical attention until fetal infection is advanced, whereas susceptible non-pregnant patients may progress promptly to sepsis or meningitis. If this hypothesis is correct, clinicians and health officials should focus on foods eaten recently when evaluating sources for non-pregnancy-associated cases.
Two strains of L. monocytogenes were recovered repeatedly from Plant A products during this investigation: the outbreak strain and a second strain, serotype 1/2a. The second strain was detected at higher levels and in deli meats that are routinely eaten without heating [14]; it is also a serotype that commonly causes human illness [3]. Nevertheless, and despite testing of nearly 450 clinical isolates from across the United States, the second strain was never associated with human illness. Although we do not know how many persons were exposed to this second strain and at what dose, our findings suggest that strains may differ widely in their virulence for humans, consistent with in vitro and in animal studies [29–33]. Regardless of potential differences in virulence, our findings clearly demonstrate a poor correlation between levels of contamination in food samples and the potential risk to public health. In this investigation, detection of extremely low levels of contamination in food samples was nevertheless associated with a large and deadly outbreak.
This investigation demonstrates the value of standardized molecular subtyping for linking cases of listeriosis, as well as the potential of using patients with other subtypes as controls in an analytical study [34]. This approach may be especially valuable for diseases such as listeriosis where well but susceptible controls can be difficult to enrol. The US Council of State and Territorial Epidemiologists has endorsed continued submission of L. monocytogenes isolates to PulseNet, which should result in greater availability of molecular subtyping data. Routine interviewing of listeriosis patients using a nationally standardized questionnaire would further enhance the utility of PulseNet data, allowing immediate comparison of food histories whenever a cluster is identified. Following our investigation, French health authorities have used this approach to rapidly implicate the source of two listeriosis outbreaks [35].
Listeriosis poses a unique challenge to clinicians, public health officials, and food producers. Although new food safety regulations have been introduced since this outbreak occurred [11], continued vigilance is needed. A large survey of frankfurter packages conducted after this outbreak indicated that 1–2% were contaminated [36], and in 2004 US producers recalled over 500 000 lb of food because of possible contamination with L. monocytogenes [37]. Clinicians and health officials should remind patients in high-risk groups to heat frankfurters and deli meats until steaming hot before eating. In addition, food handlers should be instructed to avoid cross-contaminating work surfaces or other foods with fluid from frankfurters packages or other meat products. Food producers should consider stringent safeguards to prevent contamination of food-processing equipment during renovation or construction activities, including enhanced in-plant environmental monitoring. A definitive pathogen-killing step after final packaging could help reduce the threat of listeriosis from processed meats.
APPENDIX. Listeria Outbreak Working Group members
Kathryn Boor, William Bibb, Tim Cote, Thomas Donkar, Sietske de Fitjer, Ruth Etzel, Elizabeth Koch, Stan Kondracki, Jeremy Miller, Forrest Smith, Robert Taylor, Shelley Zansky.
ACKNOWLEDGEMENTS
We thank Drs Robert Tauxe, Fred Angulo, Cindy Friedman, John Brooks, the New York State Department of Agriculture and Markets, and health officials in the following State Health Departments for their contributions of data or advice to this investigation: Arizona, California, Colorado, Connecticut, Florida, Georgia, Iowa, Illinois, Indiana, Kentucky, Massachusetts, Maryland, Michigan, Minnesota, New York, Ohio, Oregon, Pennsylvania, Rhode Island, Tennessee, Vermont, West Virginia.
DECLARATION OF INTEREST
None.
Footnotes
Members of the Group are given in the Appendix.
REFERENCES
- 1.McLauchlin J. Human listeriosis in Britain, 1967–85, a summary of 722 cases. 1. Listeriosis during pregnancy and in the newborn. Epidemiol Infect. 1990;104:181–189. doi: 10.1017/s0950268800059343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McLauchlin J. Human listeriosis in Britain, 1967–85, a summary of 722 cases. 2. Listeriosis in non-pregnant individuals, a changing pattern of infection and seasonal incidence. Epidemiol Infect. 1990;104:191–201. doi: 10.1017/s0950268800059355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Slutsker L, Schuchat A, Ryser E, Marth E. Listeria, listeriosis, and food safety. 2nd edn. New York: Marcel Dekker Inc.; 1999. Listeriosis in humans; pp. 75–97. [Google Scholar]
- 4.Dalton CB, Austin CC, Sobel J et al. An outbreak of gastroenteritis and fever due to Listeria monocytogenes in milk. N Engl J Med. 1997;336:100–105. doi: 10.1056/NEJM199701093360204. [DOI] [PubMed] [Google Scholar]
- 5.Aureli P, Fiorucci GC, Caroli D et al. An outbreak of febrile gastroenteritis associated with corn contaminated by Listeria monocytogenes. N Engl J Med. 2000;342:1236–1241. doi: 10.1056/NEJM200004273421702. [DOI] [PubMed] [Google Scholar]
- 6.Rocourt J, Jacquet C, Reilly A. Epidemiology of human listeriosis and seafoods. Int J Food Microbiol. 2000;62:197–209. doi: 10.1016/s0168-1605(00)00336-6. [DOI] [PubMed] [Google Scholar]
- 7.Schlech WF, 3rd, Lavigne PM, Bortolussi RA et al. Epidemic listeriosis – evidence for transmission by food. N Engl J Med. 1983;308:203–206. doi: 10.1056/NEJM198301273080407. [DOI] [PubMed] [Google Scholar]
- 8.Schuchat A, Deaver KA, Wenger JD et al. Role of foods in sporadic listeriosis. I. Case-control study of dietary risk factors. J Am Med Assoc. 1992;267:2041–2045. [PubMed] [Google Scholar]
- 9.Ryser E, Ryser E, Marth E. Listeria, listeriosis, and food safety. 2nd edn. New York: Marcel Dekker Inc.; 1999. Foodborne listeriosis; pp. 299–358. [Google Scholar]
- 10.McLauchlin J, Hall SM, Velani SK, Gilbert RJ. Human listeriosis and pate: a possible association. BMJ. 1991;303:773–775. doi: 10.1136/bmj.303.6805.773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.United States Department of Agriculture FSIS. Control of Listeria monocytogenes in Ready-to-Eat Meat and Poultry Products; Final Rule. Federal Register. 2003;68:34207–34254. [Google Scholar]
- 12.Seeliger HP. Serovariants of Listeria monocytogenes and other Listeria species. Acta Microbiol Acad Sci Hung. 1975;22:179–181. [PubMed] [Google Scholar]
- 13.Graves LM, Swaminathan B. PulseNet standardized protocol for subtyping Listeria monocytogenes by macrorestriction and pulsed-field gel electrophoresis. Int J Food Microbiol. 2001;65:55–62. doi: 10.1016/s0168-1605(00)00501-8. [DOI] [PubMed] [Google Scholar]
- 14.Graves L, Hunter S, Ong A et al. Microbiological aspects of the investigation that traced the 1998 outbreak of listeriosis in the United States to contaminated hot dogs and the establishment of molecular subtyping-based surveillance for Listeria monocytogenes in the PulseNet Network. J Clin Microbiol. 2005;43:2350–2355. doi: 10.1128/JCM.43.5.2350-2355.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jeffers GT, Bruce JL, McDonough PL, Scarlett J, Boor KJ, Wiedmann M. Comparative genetic characterization of Listeria monocytogenes isolates from human and animal listeriosis cases. Microbiology. 2001;147:1095–1104. doi: 10.1099/00221287-147-5-1095. [DOI] [PubMed] [Google Scholar]
- 16.Johnson J, Dey B, Lattuada C. USDA/FSIS Microbiology Laboratory Guide. 3rd edn. Washington, DC: US Government Printing Office; 1998. Isolation and incubation of Listeria monocytogenes from meat, poultry and egg products, chapter 8. [Google Scholar]
- 17.Salamina G, Dalle Donne E, Niccolini A et al. A foodborne outbreak of gastroenteritis involving Listeria monocytogenes. Epidemiol Infect. 1996;117:429–436. doi: 10.1017/s0950268800059082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.United States Department of Agriculture FSIS. http://www.fsis.usda.gov/OA/recalls/recdb/rec1998.htm. http://www.fsis.usda.gov/OA/recalls/recdb/rec1998.htm 2000 Recall Archives ( ). Accessed November 2002.
- 19.Tompkin RB. Control of Listeria monocytogenes in the food-processing environment. J Food Prot. 2002;65:709–725. doi: 10.4315/0362-028x-65.4.709. [DOI] [PubMed] [Google Scholar]
- 20.Wiedmann M. Molecular subtyping methods for Listeria monocytogenes. J AOAC Int. 2002;85:524–531. [PubMed] [Google Scholar]
- 21.Schwartz B, Ciesielski CA, Broome CV et al. Association of sporadic listeriosis with consumption of uncooked hot dogs and undercooked chicken. Lancet. 1988;2:779–782. doi: 10.1016/s0140-6736(88)92425-7. [DOI] [PubMed] [Google Scholar]
- 22.CDC. Listeriosis associated with consumption of turkey franks. Morb Mortal Wkly Rep. 1989;38:267–268. [PubMed] [Google Scholar]
- 23.Pinner RW, Schuchat A, Swaminathan B et al. Role of foods in sporadic listeriosis. II. Microbiologic and epidemiologic investigation. J Am Med Assoc. 1992;267:2046–2050. [PubMed] [Google Scholar]
- 24.Luchansky JB, Porto AC, Wallace FM, Call JE. Recovery of Listeria monocytogenes from vacuum-sealed packages of frankfurters: comparison of the U.S. Department of Agriculture (USDA) food safety and inspection service product composite enrichment method, the USDA Agricultural Research Service (ARS) product composite rinse method, and the USDA-ARS package rinse method. J Food Prot. 2002;65:567–570. doi: 10.4315/0362-028x-65.3.567. [DOI] [PubMed] [Google Scholar]
- 25.Linnan MJ, Mascola L, Lou XD et al. Epidemic listeriosis associated with Mexican-style cheese. N Engl J Med. 1988;319:823–828. doi: 10.1056/NEJM198809293191303. [DOI] [PubMed] [Google Scholar]
- 26.Riedo FX, Pinner RW, Tosca ML et al. A point-source foodborne listeriosis outbreak: documented incubation period and possible mild illness. J Infect Dis. 1994;170:693–696. doi: 10.1093/infdis/170.3.693. [DOI] [PubMed] [Google Scholar]
- 27.Azadian BS, Finnerty GT, Pearson AD. Cheese-borne listeria meningitis in immunocompetent patient. Lancet. 1989;1:322–323. doi: 10.1016/s0140-6736(89)91326-3. [DOI] [PubMed] [Google Scholar]
- 28.Junttila J, Brander M. Listeria monocytogenes septicemia associated with consumption of salted mushrooms. Scand J Infect Dis. 1989;21:339–342. doi: 10.3109/00365548909035707. [DOI] [PubMed] [Google Scholar]
- 29.Pine L, Malcolm GB, Plikaytis BD. Listeria monocytogenes intragastric and intraperitoneal approximate 50% lethal doses for mice are comparable, but death occurs earlier by intragastric feeding. Infect Immun. 1990;58:2940–2945. doi: 10.1128/iai.58.9.2940-2945.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Farber JM, Daley E, Coates F, Beausoleil N, Fournier J. Feeding trials of Listeria monocytogenes with a nonhuman primate model. J Clin Microbiol. 1991;29:2606–2608. doi: 10.1128/jcm.29.11.2606-2608.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lammerding AM, Glass KA, Gendron-Fitzpatrick A, Doyle MP. Determination of virulence of different strains of Listeria monocytogenes and Listeria innocua by oral inoculation of pregnant mice. Appl Environ Microbiol. 1992;58:3991–4000. doi: 10.1128/aem.58.12.3991-4000.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wiedmann M, Bruce JL, Keating C, Johnson AE, McDonough PL, Batt CA. Ribotypes and virulence gene polymorphisms suggest three distinct Listeria monocytogenes lineages with differences in pathogenic potential. Infect Immun. 1997;65:2707–2716. doi: 10.1128/iai.65.7.2707-2716.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vazquez-Boland JA, Kuhn M, Berche P et al. Listeria pathogenesis and molecular virulence determinants. Clin Microbiol Rev. 2001;14:584–640. doi: 10.1128/CMR.14.3.584-640.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McCarthy N, Giesecke J. Case-case comparisons to study causation of common infectious diseases. Int J Epidem. 1999;28:764–768. doi: 10.1093/ije/28.4.764. [DOI] [PubMed] [Google Scholar]
- 35.de Valk H, Vaillant V, Jacquet C et al. Two consecutive nationwide outbreaks of Listeriosis in France, October 1999–February 2000. Am J Epidemiol. 2001;154:944–950. doi: 10.1093/aje/154.10.944. [DOI] [PubMed] [Google Scholar]
- 36.Wallace FM, Call JE, Porto AC, Cocoma GJ, Luchansky JB. Recovery rate of Listeria monocytogenes from commercially prepared frankfurters during extended refrigerated storage. J Food Prot. 2003;66:584–591. doi: 10.4315/0362-028x-66.4.584. [DOI] [PubMed] [Google Scholar]
- 37.United States Department of Agriculture FSIS. http://www.fsis.usda.gov/fsis_recalls/Closed_Federal_Cases_2004/index.asp. http://www.fsis.usda.gov/fsis_recalls/Closed_Federal_Cases_2004/index.asp Recall Information Center. ( ). Accessed July 2005.