SUMMARY
In two prisons in Berlin, Germany, provision of sterile injection equipment for injecting drug users (IDUs) started in 1998. To assess the programme’s impact, the frequency of injecting drug use and syringe sharing, and the incidence of HIV, HBV, and HCV infection were determined in a follow-up study. Of all IDUs (n=174), 75% continued to inject. After the project start the level of syringe sharing declined from 71% during a 4-month period of previous imprisonment to 11% during the first 4 months of follow-up, and to virtually zero thereafter. Baseline seroprevalences for HIV, HBV, and HCV were 18, 53, and 82%. HIV and HCV seroprevalence at baseline was significantly associated with drug injection in prison prior to the project start. No HIV and HBV seroconversions, but four HCV seroconversions occurred. The provision of syringes for IDUs in appropriate prison settings may contribute to a substantial reduction of syringe sharing. However, the prevention of HCV infection requires additional strategies.
INTRODUCTION
Injection drug use in prison carries a substantial risk of infection with bloodborne viruses such as human immunodeficiency virus (HIV), hepatitis B virus (HBV) and hepatitis C virus (HCV) [1–7]. Prevention strategies are needed to reduce the risk of infection among incarcerated injecting drug users (IDUs). Outside prisons, syringe exchange programmes have played a key role in reducing the spread of the viruses among IDUs [8–11]. Data on the effectiveness of syringe exchange programmes implemented inside prisons are scarce [12, 13]. In these studies, laboratory tests to identify incident infections with HIV, HBV, and HCV were not systematically performed. Moreover, no data are available from large metropolitan areas where IDUs may differ significantly from those in other regions with respect to drug use patterns, behavioural characteristics, and prison experience.
In Berlin, Germany, the provision of sterile injection equipment was started in two prisons in 1998. The objectives of the study were to investigate the feasibility and safety of the project and to assess its effects on drug use patterns, risk behaviour, and the frequency of HIV, HBV, and HCV infection.
METHODS
Setting and study population
The project was implemented in a prison for females (October 1998) and a prison for males (February 1999). All new inmates received information leaflets and counselling on harm reduction issues, and on the project itself. In the prison for females, three automatic dispensers were installed. They provided a small package containing a sterile syringe and needle and a skin disinfection pad in exchange for a used syringe, or a dummy which is handed out to new entrants. The dispensers were installed in places generally not visible to prison staff. In the prison for males, social workers from a non-governmental organization exchanged sterile syringes and needles for used equipment three times a week. Anonymity and confidentiality was assured to the clients visiting the room where the syringe exchange took place.
All inmates who had ever used illicit drugs (injection, inhalational, or intranasal use of heroin or cocaine) were eligible for participation in the study. New entrants were consecutively recruited into the study. After informed consent had been received, data on sociodemographic and drug-use characteristics, and risk behaviour before and during imprisonment were obtained by trained external interviewers using standardized questionnaires. Laboratory testing for HIV, HBV, and HCV seromarkers was offered to all participants. Pre-test and post-test counselling was performed by members of the study team. After informed consent had been obtained interviews and laboratory tests were performed at baseline and at follow-up visits every 4 months and shortly before deferral. Questionnaires and blood samples were coded, and all personal identifiers were removed. These anonymized data were entered into an Access database and analysed.
The study received institutional review board approval from the Institute of Tropical Medicine, Humboldt University Berlin, and ethical clearance by the appropriate committee of the Department of Justice, Senate of Berlin. The research conformed to the principles embodied in the Declaration of Helsinki.
The study was carried out from October 1998 to June 2001. During this time period 213 persons were incarcerated in the two prisons, 174 of which participated in the study (response rate 82%). Respondents did not differ significantly by age and gender from non-respondents.
Laboratory methods
Enzyme-linked immunosorbent assay (ELISA) was used to detect HIV antibodies (Sanofi Pasteur, Freiburg, Germany), hepatitis B surface (HBs) antigen, and anti-HBc (Abbott, Wiesbaden, Germany). Anti-HBs was determined by radioimmunoassay (Abbott). Positive HIV results were confirmed by Western blot (Sanofi Pasteur). HCV antibodies were detected by a third-generation ELISA (Ortho, Neckargmünd, Germany). Positive or indeterminate HCV results were confirmed by immunoblot (Abbott).
Statistical methods
To analyse associations between categorical variables χ2 tests or χ2 tests for trend were used. For multivariate analysis (e.g. of determinants for HIV, HBV, and HCV infection at baseline) forward stepwise logistic regression was performed. The final models (e.g. for risk factors for HIV or HCV infection at baseline) were selected based on the likelihood ratio statistic. For statistical analysis SPSS version 11.5 was used (SPSS Inc., Chicago, IL, USA). In the follow-up study, HIV, HBV, and HCV incidence rates (infections by 100 person-years) were calculated.
RESULTS
Baseline characteristics
Of the 174 participants (117 females, 57 males), 166 (95%) reported previous injection drug use. Table 1 shows the basic sociodemographic and behavioural characteristics. The median age was 31 years (interquartile range 27–34 years). Of the IDUs, 72% had injected for  5 years. Injection drug use in the 6 months prior to imprisonment was reported by 91%. Two thirds of the IDUs had ever injected with syringes already used by another person (‘syringe sharing’), and 17% had done so in the 6 months prior to imprisonment. The majority of the IDUs (females 76%, males 88%) had previously been in prison.
5 years. Injection drug use in the 6 months prior to imprisonment was reported by 91%. Two thirds of the IDUs had ever injected with syringes already used by another person (‘syringe sharing’), and 17% had done so in the 6 months prior to imprisonment. The majority of the IDUs (females 76%, males 88%) had previously been in prison.
Table 1.
Demographic and behavioural characteristics of imprisoned injecting drug users (baseline)
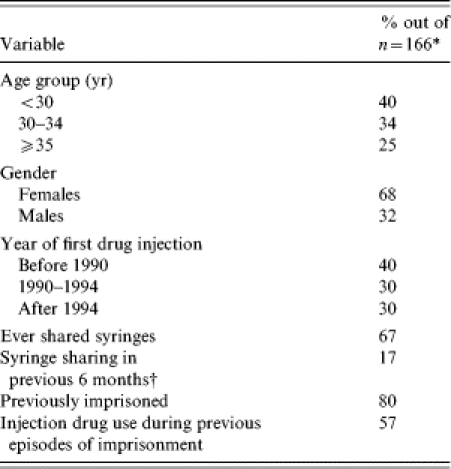
Participants reporting previous injection drug use.
Prior to current imprisonment.
At baseline, 71% of participants who had injected drugs during previous periods of imprisonment (i.e. before the project start) reported syringe sharing during an average 4-month period in prison (Table 2).
Table 2.
Characteristics of imprisoned injecting drug users before and after start of the syringe exchange programme in prison
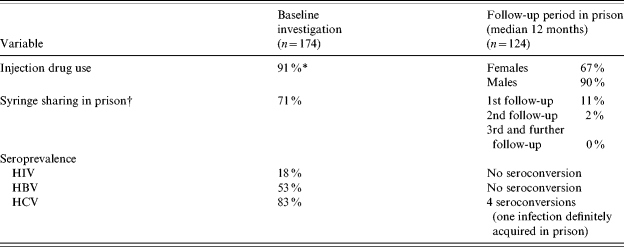
Injection drug use in previous 6 months (outside or inside prisons).
Referring to individuals (denominator) who injected drugs during previous 4-month periods of imprisonment (baseline investigation) or during 4-month follow-up periods.
Utilization of the syringe exchange programme and adverse events
Overall, 3383 syringes were delivered to the prison for females (October 1998 to June 2001), and 4571 syringes to the prison for males (February 1999 to June 2001). Substantial variations in the number of syringes delivered per month were observed in the prison for females although the number of incarcerated IDUs was relatively stable. Peak use of the automatic dispensers was in December 1999 (n=244 syringes) and December 2000 (n=372). The number of dispensed syringes was more constant over time in the prison for males (range 150–250 per month).
No adverse events possibly related to the project were observed (e.g. overall increase in injection drug use, violence involving needles against staff or other inmates).
Injection drug use and syringe sharing after project start
Follow-up data were available from 124 participants (81 females, 43 males) with a median follow-up time of 12 months. Drop-outs were mainly due to pre-term deferral or transfer to other institutions.
Injection drug use during follow-up was reported by 67% of the females, and 90% of the males (Table 2). Of the injectors, 95% used heroin, and 26% cocaine. The median frequency of injecting (in the most recent 4-month period) was eight in females (range 1–100), and 23 in males (range 4–200).
After the project start, 11% of the injectors reported any syringe sharing (Table 2). This proportion did not differ significantly by gender, age, or infection status at baseline. Apart from two single later events, syringe sharing only occurred during the first follow-up period.
Two of the eight individuals who had previously used illicit drugs only by routes other than injection started to inject drugs during follow-up. One person injected only once during a 12-month follow-up, while the other injected twice and was lost to follow-up.
Prevalence and determinants of HIV, HBV, and HCV infection
At baseline the seroprevalence rates among the IDUs were 18% for HIV, 53% for HBV, and 82% for HCV. Only 9% of the inmates had evidence of hepatitis B immunization (anti-HBs alone).
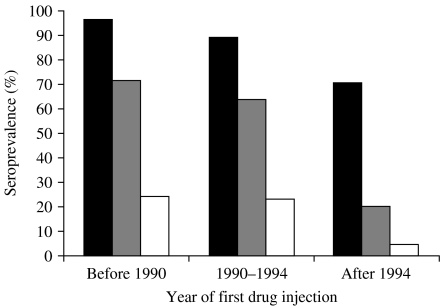
In univariate analysis, several variables such as year of first injection drug use, age, overall frequency of syringe sharing, previous imprisonment, and previous injection drug use in prison were significantly associated with HIV, HBV, and HCV infection (data not shown). Seroprevalences were inversely associated with date of first drug injection (Fig.). HIV antibody prevalence was 20% among participants who already injected before 1995, but was only 4% among those who started to inject after 1994 (P=0·02). In the latter group, HCV seroprevalence was already 71% and reached 97% among IDUs who started to inject before 1990 (P<0·001).
Fig.
Seroprevalence of HIV (□), HBV ( ), and HCV (■) infection among imprisoned injecting drug users according to year of first drug injection.
), and HCV (■) infection among imprisoned injecting drug users according to year of first drug injection.
In multivariate analysis, injecting drug use during previous imprisonment was found to be an independent predictor of HIV infection after adjusting for time since first injection, and syringe sharing [adjusted odds ratio (aOR) 2·3, 95% confidence interval (CI) 1·2–4·9], and of HCV infection (aOR 2·0, 95% CI 1·1–5·6). Year of first injection also remained a predictor of infection. The aOR in IDUs who started to inject after 1994 (baseline category: start of drug injection before 1990) was 0·2 (95% CI 0·04–0·8) for HIV, 0·1 (95% CI 0·01–0·2) for HBV (after exclusion of vaccinated IDUs), and 0·2 (95% CI 0·03–0·7) for HCV.
Incidence of HIV, HBV, and HCV infection
During follow-up no HIV or HBV seroconversions were observed. However, four out of 22 individuals who were seronegative at baseline developed HCV antibodies (incidence rate 18/100 person-years). In three cases, HCV antibodies were detected at the first follow-up (two males, one female). In another male IDU, seroconversion occurred between the third and fourth follow-up visit. All IDUs who seroconverted denied sharing syringes while in prison. However, three of them reported ‘frontloading’ (dividing up drug doses between two or more IDUs involving a used syringe) or sharing of spoons for drug preparation on several occasions in the months preceding seroconversion. Other risk factors such as tattooing, piercing or sexual risk behaviour were denied.
DISCUSSION
The study shows that the provision of sterile injection equipment in prisons is readily accepted by IDUs and may contribute to a significant reduction of syringe sharing over time. The baseline data underscore previous findings that injection drug use during incarceration is common, and may significantly increase the risk of bloodborne infections [1–3, 1–3, 6, 7]. The project was deliberately implemented in prisons were illicit drugs are available despite measures to control their inflow into prison. Therefore, the relatively high levels of injection drug use throughout the study period are not surprising.
Two individuals who had previously only inhaled heroin reported injecting drug use on single occasions during the study period. It cannot be ruled out that the availability of sterile equipment may have facilitated initiation of injecting drug use in these persons. However, it is more likely that this finding reflects the natural incidence of injection drug use among inhalational heroin users in settings where peers frequently inject [1, 5]. Overall, there was no evidence that the availability of sterile syringes led to an increase in drug consumption.
The implementation of the project was followed by an impressive reduction of syringe sharing. During 4-month periods of incarceration prior to the project start over 70% of drug injectors had shared syringes. Only a minority of the participants reported syringe sharing at the first follow-up, and during further observation periods it virtually disappeared. A substantial reduction in the frequency of syringe sharing among IDUs has also been reported from the projects in Switzerland and Lower Saxony, Germany [12, 13]. Socially desirable responding in such studies may be a problem, although efforts were made to minimize this phenomenon using anonymous questionnaires by external interviewers.
A strength of the study is the systematic testing for HIV, HBV, and HCV infection during follow-up to detect new infections. No HIV and HBV seroconversions were observed. There is strong evidence from routine data of medical departments in other prisons in Berlin, Germany that some IDUs have definitely acquired HIV infection or viral hepatitis while in prison [14]. Unfortunately, no systematic studies on incidence of HIV, HBV, and HCV infection among IDUs incarcerated in prisons without syringe exchange programmes have been published for Germany. However, studies from other industrialized countries reported relatively high incidences of these infections among IDUs in prisons where no sterile syringes are available [4]. Among Danish prisoners HBV incidence was 16/100 person-years [15], and a recent study in Scotland found an HCV incidence of 29/100 person-years in individuals having shared syringes during follow-up [7]. A limitation of our study is the fact that the median time of follow-up (12 months) was too short to demonstrate a long-term preventive effect. If new infections occurred at the end of the observation period the seroconversions would not have been detected in prison. Nevertheless, the lack of new infections in the project compares favourably with incidence of HIV and HBV among IDUs reported in previous studies inside and outside prisons [15–17].
The significant reduction of syringe sharing in our study is probably a result of the availability of sterile injection equipment in the prisons. However, because of lack of a control group it is not possible to directly ascribe the fact that no HIV and HBV seroconversions occurred due to this intervention. We cannot rule out that other factors such as intensified counselling of inmates about risks of parenterally transmitted infections may have played a role in risk reduction and lack of seroconversions in this study.
HCV antibody prevalence in our study was already high at baseline. In addition, four seroconversions were observed during follow-up, and at least one infection was acquired after the project start. In many places, HCV transmission is still a severe problem among IDUs outside and inside prisons. The existing prevention strategies including syringe exchange programmes may not be sufficient to contain the spread of HCV among IDUs [18]. Apart from syringe sharing the practice of frontloading/backloading and the sharing of other injection paraphernalia (e.g. spoons, cookers) have to be considered as risk factors [19–23].
In multivariate analysis, participants of our study who started to inject after 1994 were significantly less likely to test positive for HIV, HBV, or HCV markers. This indicates a preventive effect of the harm reduction measures, a full range of which have been in operation in Berlin since the beginning of the 1990s. However, the effect on hepatitis C was limited since 70% of IDUs who started to inject after 1994 still acquired HCV infection.
In many prisons the prevention of bloodborne infections among IDUs remains an important task. In settings where it is feasible the provision of sterile injection equipment may have its role among other measures including intensified counselling, diversification of treatment options (e.g. methadone maintenance), and hepatitis B immunization.
ACKNOWLEDGEMENTS
We thank all participants in the study. We are grateful to Volker Küster for support in the organization of the project. The study has been funded in part by the Senate of Berlin (Department of Justice, Department of Health) and by the Federal Ministry of Education and Research (Research Network on Viral Hepatitis, Hep-Net).
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Allwright S et al. Prevalence of antibodies to hepatitis B, hepatitis C, and HIV and risk factors in Irish prisoners: results of a national cross sectional survey. BMJ. 2000;321:78–82. doi: 10.1136/bmj.321.7253.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bird AG et al. Anonymous HIV surveillance with risk factor elicitation at Scotland’s largest prison, Barlinnie. AIDS. 1995;9:801–808. doi: 10.1097/00002030-199507000-00019. [DOI] [PubMed] [Google Scholar]
- 3.Crofts N et al. Spread of blood-borne viruses among Australian prison entrants. BMJ. 1995;310:285–288. doi: 10.1136/bmj.310.6975.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dolan K, Wodak A, Penny R. AIDS behind bars: preventing HIV spread among incarcerated drug injectors. AIDS. 1995;9:825–832. [PubMed] [Google Scholar]
- 5.Gore SM et al. Drug injection and HIV prevalence in inmates of Glenochil prison. BMJ. 1995;310:293–296. doi: 10.1136/bmj.310.6975.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Müller R et al. Imprisonment: a risk factor for HIV infection counteracting education and prevention programmes for intravenous drug users. AIDS. 1995;9:183–190. [PubMed] [Google Scholar]
- 7.Champion JK et al. Incidence of hepatitis C virus infection and associated risk factors among Scottish prison inmates: a cohort study. American Journal of Epidemiology. 2004;159:514–519. doi: 10.1093/aje/kwh061. [DOI] [PubMed] [Google Scholar]
- 8.Des Jarlais DC et al. HIV incidence among injecting drug users in New York City syringe-exchange programmes. Lancet. 1996;348:987–991. doi: 10.1016/s0140-6736(96)02536-6. [DOI] [PubMed] [Google Scholar]
- 9.Gibson DR, Flynn NM, Perales D. Effectiveness of syringe exchange programs in reducing HIV risk behavior and HIV seroconversion among injecting drug users. AIDS. 2001;15:1329–1341. doi: 10.1097/00002030-200107270-00002. [DOI] [PubMed] [Google Scholar]
- 10.Keene J et al. Evaluation of syringe-exchange for HIV prevention among injecting drug users in rural and urban areas of Wales. Addiction. 1993;88:1063–1070. doi: 10.1111/j.1360-0443.1993.tb02125.x. [DOI] [PubMed] [Google Scholar]
- 11.Van Ameijden EJC, van den Hoek JAR, Coutinho RA. Injecting risk behavior among drug users in Amsterdam 1986 to 1992, and its relationship to AIDS prevention programs. American Journal of Public Health. 1994;84:275–281. doi: 10.2105/ajph.84.2.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nelles J et al. Provision of syringes: the cutting edge of harm reduction in prison. BMJ. 1998;317:270–273. doi: 10.1136/bmj.317.7153.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meyenberg R, Stöver H, Jacob J. Prevention of infections in prisons in Lower Saxony, Germany [in German] Oldenburg: Bibliotheks- und Informationssystem der Universität Oldenburg; 1996. [Google Scholar]
- 14.Keppler K, Stöver H. Transmission of infectious diseases during imprisonment – results of a study and introduction of a model project for infection prevention in Lower Saxony. Gesundheitswesen. 1999;61:207–213. [PubMed] [Google Scholar]
- 15.Christensen PB et al. Prevalence and incidence of bloodborne viral infections among Danish prisoners. European Journal of Epidemiology. 2000;16:1043–1049. doi: 10.1023/a:1010833917242. [DOI] [PubMed] [Google Scholar]
- 16.Levine OS et al. Differences in the incidence of hepatitis B and human immunodeficiency virus infections among injecting drug users. Journal of Infectious Diseases. 1996;73:579–583. doi: 10.1093/infdis/173.3.579. [DOI] [PubMed] [Google Scholar]
- 17.Stark K et al. Methadone maintenance treatment and HIV risk-taking behaviour among injecting drug users in Berlin. Journal of Epidemiology and Community Health. 1996;50:534–537. doi: 10.1136/jech.50.5.534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Taylor A et al. Prevalence of hepatitis C virus infection among injecting drug users in Glasgow 1990–1996: are current harm reduction strategies working. Journal of Infection. 2000;40:176–183. doi: 10.1053/jinf.2000.0647. [DOI] [PubMed] [Google Scholar]
- 19.Des Jarlais DC et al. Variability in the incidence of human immunodeficiency virus, hepatitis B virus, and hepatitis C virus infection among young injecting drug users in New York City. American Journal of Epidemiology. 2003;157:467–471. doi: 10.1093/aje/kwf222. [DOI] [PubMed] [Google Scholar]
- 20.Hagan H et al. Sharing of drug preparation equipment as a risk factor for hepatitis C. American Journal of Public Health. 2001;91:42–46. doi: 10.2105/ajph.91.1.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hahn JA et al. Hepatitis C Virus Seroconversion among young injection drug users: relationships and risks. Journal of Infectious Diseases. 2002;186:1558–1564. doi: 10.1086/345554. [DOI] [PubMed] [Google Scholar]
- 22.Stark K et al. Frontloading: a risk factor for HIV and HCV infection among injecting drug users in Berlin. AIDS. 1996;10:311–317. [PubMed] [Google Scholar]
- 23.Thorpe LE et al. Risk of hepatitis C virus infection among young adult injection drug users who share equipment. American Journal of Epidemiology. 2002;155:645–653. doi: 10.1093/aje/155.7.645. [DOI] [PubMed] [Google Scholar]