SUMMARY
Systematic national surveillance of outbreaks of infectious intestinal disease (IID) was introduced in England and Wales in 1992 to provide comprehensive information on causative organisms, sources or vehicles of infection and modes of transmission. We compared information from this system with that published in the peer-reviewed literature between 1 January 1992 and 31 January 2003 to assess the potential effect of publication bias on food-safety policy. During the study period 1763 foodborne outbreaks of IID were reported to national surveillance. Fifty-five were published in the peer-reviewed literature. The peer-reviewed literature overestimated the impacts of milk/milk products, miscellaneous foods (e.g. sandwiches) and desserts and underestimated those of poultry, fish and shellfish, red meat/meat products and eggs/egg products. Without systematic surveillance, knowledge of causative organisms, sources or vehicles of infection and modes of transmission, as gleaned from the peer-reviewed literature, would potentially distort food-safety policy.
INTRODUCTION
The United Kingdom (UK) Food Standards Agency has set a target for a 20% reduction in foodborne illness by April 2006 [1]. To achieve this it needs robust information on the vehicles and causes of food poisoning. The majority of foodborne infectious intestinal disease (IID) is sporadic and so the identification of sources of infection in these instances is often unavailable [2]. Thus, epidemiological and microbiological evidence gained in foodborne outbreaks can provide some of the strongest information linking food to illness. The routine surveillance of such outbreaks provides a powerful tool available to policy-makers (including the Food Standards Agency), as well as the wider public health community.
The system for the surveillance of IID in England and Wales was introduced in 1992 [3]. The objectives were to:
identify routes of transmission;
identify trends in pathogens causing outbreaks;
identify trends in food vehicles;
detect new pathogens/vehicles;
assess the impact of outbreaks in different settings.
This dataset has been interrogated regularly to provide information for individuals from a variety of organizations; from university students on the one hand to policy-makers on the other. Indeed the majority of requests for information are from government agencies – the Food Standards Agency, the Department of Health, and the Department for the Environment, Food and Rural Affairs. It is imperative, therefore, that the data used to provide this information are as complete as possible.
Alternative sources of intelligence include the peer-reviewed literature. Outbreaks that are published in the literature are likely to be unusual, for example highlighting novel food vehicles. Therefore, we compared foodborne general outbreaks reported to the surveillance system with those appearing in the peer-reviewed literature to assess the potential effect of publication bias on food-safety policy.
METHODS
Surveillance of general outbreaks of IID
The national system for the surveillance of general outbreaks of IID has been described in detail elsewhere [3, 4]. It is focused on a standard questionnaire which is sent to the lead investigator, who is requested to complete it when the outbreak is over. The questionnaire seeks data on the outbreak setting, the mode of transmission, the causative organism and details of epidemiological and laboratory investigations. Data from returned questionnaires (response rate >70% [5]) are stored in a dynamic database (GSURV) which is derived from Epi-Info [6]. For the purposes of this paper, outbreaks were included initially where the mode of transmission was described as mainly foodborne.
Literature search strategy
Relevant literature was obtained by interrogating the online PubMed database [7]. English-language articles published from 1992 to 2003 were considered. Searches of the title word ‘outbreak’ and the expanded Medical Subject Headings (MeSH) terms ‘disease outbreaks’ and ‘food’ were undertaken. Furthermore, a search of Medline was undertaken by a professional librarian. A search on the MeSH subheadings ‘food poisoning’, ‘epidemiology’, ‘aetiology’, ‘food handling’, ‘food’ and ‘beverages’ was combined with searches of the MeSH term ‘disease outbreaks’ and then limited by the MeSH subheading ‘Great Britain’. Reference lists were used to identify additional outbreak papers.
Papers relating to family outbreaks, or those which took place outside England and Wales were excluded, as were those where the mode of transmission was not described as foodborne. Initial reports of outbreaks, published in the Communicable Disease Report (CDR) Weekly [8], were excluded, as were outbreak reviews or papers which discuss outbreaks in scant detail (e.g. discussing decreased susceptibility to ciprofloxacin in an outbreak of Salmonella enterica serovar Typhimurium definitive phage type (DT) 104 associated with a pasteurization failure at an on-farm dairy [9]).
Two members of the research team (I.A.G. and M.A.S.) reviewed all the output from each search independently of each other in order to identify articles to be included and agreed a common list. Transcription errors when creating the publication dataset were minimized at two stages by highlighting data for inclusion on the manuscripts and a process of rigorous data-checks once these data had been transcribed. Routine validation of the national outbreak dataset takes place as part of ongoing surveillance procedures.
Data collected on general outbreaks (described above) were extracted where available and recorded in a database.
Calculation of lag periods
Where the date of publication and the last date of onset of symptoms in an outbreak were available, the publication lag period was calculated. The last date of onset in an outbreak and date of questionnaire completion were used to define the reporting lag for general outbreaks of IID.
Calculation of Publication Bias Index (PBI)
We calculated a publication bias index (PBI) to provide a direct measure of the impact of the publication bias for characteristics of interest. The PBI was expressed as the ratio of the percentages of outbreaks by type of report. For example, if 10/50 outbreaks published in the peer-reviewed literature were set on farms, compared with 49/1500 general outbreaks then the PBI would be 20%/3%=6·1. Where the PBI was >1, outbreaks were over-represented in the literature compared with the outbreak surveillance dataset. Conversely where the PBI was <1, outbreaks were under-represented in the literature compared with the outbreak surveillance dataset.
Statistical analysis
The datasets were analysed using Microsoft Excel 2000 (Microsoft Corp., USA), Epi-Info version 6.04b (CDC, Atlanta, GA, USA) and stata version 8 (StataCorp LP, College Station, TX, USA). Relative proportions were compared using the χ2 test. For smaller samples Fisher’s exact test was used. Medians and means were compared using the non-parametric K-sample test on the equality of medians and Student’s t test respectively.
RESULTS
Between 1 January 1992 and 31 December 2003, 1784 potential foodborne general outbreaks of IID in England and Wales were identified in the peer-reviewed literature. Initially, 66 outbreaks were considered eligible for inclusion [9–69]. Upon closer scrutiny, one outbreak occurred outside England and Wales [64], in five outbreaks initial foodborne transmission was followed by person-to-person transmission [17, 38, 52, 57, 67] three described the outbreak in insufficient detail for analysis [9, 69, 70], one was an outbreak review [28] and one was a news report [55]. These outbreaks were excluded from further analysis, leaving 55 foodborne general outbreaks identified in the literature (‘literature outbreaks’). During the same time period, 7658 general outbreaks of IID were reported to the Health Protection Agency (HPA) Centre for Infections (CfI). In 1763 (23%) of these outbreaks the mode of transmission was described as ‘mainly foodborne’.
Lag period
The date of publication was available for all the literature outbreaks, and the last onset date of the outbreak was described in 34 outbreaks (65%). The lag-time period from outbreaks taking place to their appearance in the peer-reviewed literature ranged from 7 to 169 months, and the median length was 23 months. The date of entry of data was unavailable for outbreaks before 1996 in GSURV, so these outbreaks were excluded from the calculation of the reporting lag period. It was, therefore, possible to calculate the reporting lag time for 707/939 general outbreaks (75%). The time period between the occurrence of an outbreak and the completion of the national surveillance system questionnaire ranged from 1 to 44 months, and the median length was 13 months. The median publication lag period in literature outbreaks was significantly longer than the median reporting lag in general outbreaks (P<0·001).
Completeness of data
There were interesting differences between the sources of data in terms of their completeness. In general, outbreak dynamics and impact (numbers of cases hospitalized or died, month of onset and outbreak duration) were more complete in the outbreak surveillance dataset compared with outbreaks reported in the peer-reviewed literature. More complete in the published reports were data on pathogens, food vehicles, the evidence implicating a food vehicle, as well as the food-handling/hygiene faults that were thought to have contributed to the outbreak.
Dynamics and impact
In the 52 literature outbreaks, 2443 people were affected (range 4–361), with 199 hospital admissions (range 0–33) and nine deaths (range 0–3) reported. This corresponds with 39 842 people affected (range 2–530), 1537 hospital admissions (range 0–42) and 68 deaths (range 0–10) in the 1528 general outbreaks. Literature outbreaks were larger than general outbreaks with regard to the mean number of people affected (44 vs. 23, P<0·001), admitted to hospital (6·9 vs. 1·3, P<0·001) or reported to have died (0·6 vs. 0·07, P<0·001). Furthermore, the duration of literature outbreaks (range 2–393 days, mean 31) was significantly longer than general outbreaks (range 1–373 days, mean 8) (P<0·001).
Outbreak setting
The various settings for literature and general outbreaks of IID are summarized in Table 1. The majority (55%) of general outbreaks took place in, or were linked to, commercial catering premises (canteens, halls or caterers, hotels, public houses or bars, restaurants, shop caterers), but these premises accounted for less than one fifth of literature outbreaks (18%) (PBI 0·6, χ2P<0·001). Literature outbreaks were more likely to occur in the community (20% vs. 2%, PBI 10·7, P<0·001) or were linked to shops (20% vs. 7%, PBI 2·8, P=0·002) compared with general outbreaks.
Table 1.
‘General outbreaks’ and ‘literature outbreaks’ of infectious intestinal disease, England and Wales, 1992–2000. Outbreaks by setting
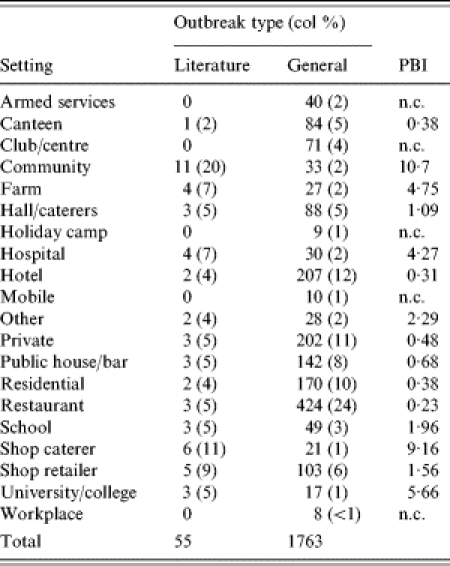
PBI, Publication Bias Index; n.c., not calculable.
Pathogens and toxins
Bacterial pathogens predominated in both literature (88%) and general outbreaks (76%, Table 2). Literature outbreaks reported outbreaks of campylobacteriosis (16% vs. 4%, PBI 4·3, P<0·001) and Shiga toxin-producing Escherichia coli O157 (STEC O157) infection (13% vs. 3%, PBI 5·0, P<0·001) more often than general outbreaks. Outbreaks of Clostridium perfringens gastroenteritis were reported relatively commonly in general outbreaks (12%), but were not reported in literature outbreaks.
Table 2.
‘General outbreaks’ and ‘literature outbreaks’ of infectious intestinal disease, England and Wales, 1992–2002. Outbreaks by pathogen/toxin
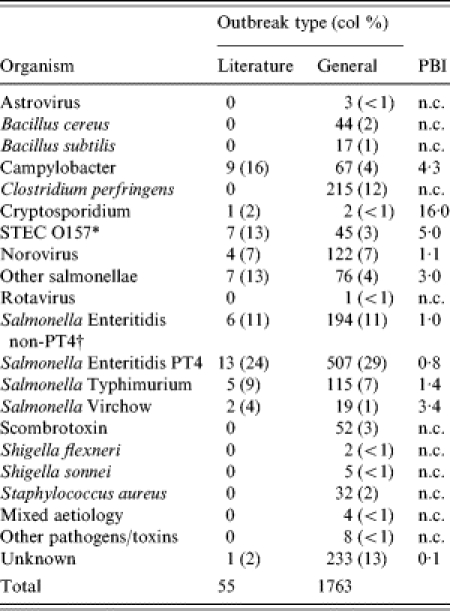
PBI, Publication Bias Index; n.c., not calculable.
Shiga-toxin-producing E. coli O157.
Food vehicles
In the majority (45/55, 82%) of literature outbreaks only one food vehicle was reported. In four (7%) and five (9%) outbreaks two and three vehicles were reported respectively and in only one outbreak (2%) were the investigators unable to identify the foodborne vehicle of infection. In just over half (1030/1763, 58%) of the general outbreaks one vehicle of infection was reported. In 162 outbreaks (9%) two vehicles were identified and in 87 outbreaks (5%) three vehicles were reported. It is notable that in over a quarter (484, 27%) of general outbreaks the investigators were unable to identify a vehicle of infection.
The distribution of foodborne vehicles for literature and general outbreaks is shown in Table 3. Miscellaneous foods (e.g. sandwiches), desserts and milk/milk products appeared to be over-represented in literature outbreaks, whereas poultry, fish and shellfish, red meat/meat products and eggs/egg products appeared to be under-represented.
Table 3.
‘General outbreaks’ and ‘literature outbreaks’ of infectious intestinal disease, England and Wales, 1992–2002. Reported vehicles of infection
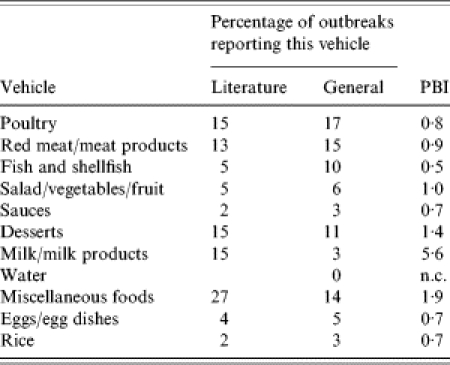
PBI, Publication Bias Index; n.c., not calculable.
Evidence implicating food vehicles
The evidence implicating foodborne vehicles of infection was available for the vast majority (51/55, 98%) of literature outbreaks, but for only two thirds (1169/1763, 66%) of general outbreaks. In most outbreaks [literature (29, 53%) and general (962, 55%)], only one form of evidence was supplied. However, more than one form of evidence was reported more often in literature outbreaks (25/55, 45%) compared with general outbreaks (207/1763, 12%) (P=0·02). Statistical evidence, from a case-control or a cohort study, was more likely to be reported in literature outbreaks (43/55, 78%) than in general outbreaks (427/1763, 24%) (P<0·001).
Contributory faults
The faults, thought to have contributed to an outbreak, were available for almost all (53/55, 96%) of the literature outbreaks but only two thirds (1170/1763, 66%) of the general outbreaks (P<0·001). Furthermore, on average, more faults were reported in literature outbreaks (1·7) than in general outbreaks (1·1, P<0·001). Inadequate heat treatment (PBI 1·7) and cross contamination (PBI 1·8) were over-represented in literature outbreaks (Table 4).
Table 4.
‘General outbreaks’ and ‘literature outbreaks’ of infectious intestinal disease, England and Wales, 1992–2002. Faults thought to have contributed to outbreaks
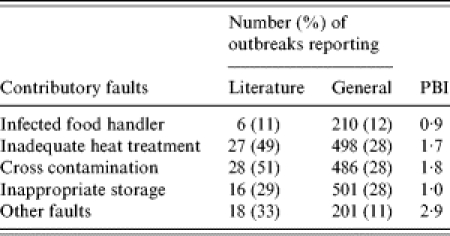
PBI, Publication Bias Index.
DISCUSSION
We have compared foodborne general outbreaks reported to the surveillance system with those appearing in the peer-reviewed literature to assess the potential effect of publication bias on food-safety policy. Few of the foodborne outbreaks reported to CfI led to peer-reviewed publication. Publications in peer-reviewed journals tended to favour the unusual or novel event, which is not necessarily surprising since peer-reviewed journals favour articles providing original findings. However, in order to develop rational policies, policy-makers, enforcers and risk assessors need to know what usually causes people to become ill, as well as what is unusual, because it is in dealing with commonly occurring problems that the greatest health gains are to be made.
It is possible that we might have missed some articles that had been published, underestimating the visibility of the information base. However, two searches were conducted, one by a professional medical librarian. Furthermore, we scanned the references at the end of peer-reviewed articles to identify any that we might have missed.
We applied very stringent criteria for defining papers for inclusion in this study and this might also have underestimated dissemination of the results of outbreak investigations in the public domain. In particular, one potential source of data, not included in our search strategy was the weekly surveillance bulletin produced by the HPA (CDR Weekly) [71]. The reason for this was that although preliminary reports of foodborne outbreak investigations sometimes appear for the purposes of alerting other colleagues to their occurrence and for case-finding, follow-up reports containing the outcome of the investigations are rare. The fact that the same analytical strategy was applied to both datasets means that the results should be fully comparable.
Six papers appeared in the peer-reviewed literature describing outbreaks that were not already reported to the national surveillance scheme [24, 25, 31, 33, 56, 62]. We acknowledge that linking the two datasets is not a simple process, especially as key fields (e.g. details of the outbreak setting) might be omitted from peer-reviewed publications. National outbreak surveillance is a passive system, relying on local investigators (consultants in communicable disease control, environmental health officers or microbiologists) to trigger a report. There is a fail-safe mechanism for the foodborne zoonoses, the majority of which are referred to national reference laboratories. National reference microbiologists also report to the system. The response rate for these known outbreaks is consistently high [5]. However, for non-zoonotic foodborne disease outbreaks, e.g. Norovirus, this fail-safe mechanism is not as robust so that the national surveillance dataset might underestimate the true incidence of all foodborne disease outbreaks in England and Wales. The forthcoming European Union Zoonoses Regulations [72], which come into force in 2007, will help to strengthen national foodborne disease outbreak surveillance since there will be a duty to investigate and report centrally all suspected outbreaks of foodborne disease.
Those outbreaks that are published tend to be those where the evidence, microbiological, environmental and epidemiological, is the strongest. The national dataset comprises outbreaks where one or two of those three strands of evidence might be missing. The danger in only considering information for policy-making from the peer-reviewed literature is that the influence of unusual organisms/food vehicles might be over-emphasized. We must acknowledge that the discussion sections of all peer-reviewed papers should place the novel observations in the context of what is already known and how the new findings contribute further to our understanding of the epidemiology of foodborne diseases. This means that while the topics published may be biased, a critical appraisal of the papers need not necessarily lead to a biased assessment of food-safety policy issues. However, the importance of certain pathogens in foodborne disease outbreak causation in England and Wales might be overlooked. For example, during the study period no peer-reviewed papers describing outbreaks of Gram-positive bacteria, Staphylococcus aureus and C. perfringens, appeared in the literature, despite the latter being recorded as the pathogen responsible for some 12% of outbreaks during the surveillance period. Indeed the fact that C. perfringens is one of the Food Standard Agency’s five target pathogens reflects its importance in the outbreak dataset [1]. Relying solely on the literature might lead to an over-emphasis on controlling the milk supply and a failure to pay enough attention to the role of contaminated fish and shellfish in outbreak causation.
The main drawback of only considering information from the outbreak surveillance dataset is that some of the evidence implicating food vehicles and contributory faults is weaker than that which would be accepted for publication. However, the advantage of data collection for the national dataset is that levels of evidence implicating particular food vehicles are available. This means that the quality of evidence linking organisms to food vehicles supplied to policy-makers is transparent.
Our work has shown that, in the absence of systematic national surveillance, knowledge of causative organisms, sources or vehicles of infection and modes of transmission in foodborne disease outbreaks gleaned from the peer-reviewed literature might have the potential to distort food-safety policy. In practice, both types of data are needed so that novel and unusual peer-reviewed findings can be contextualized. Our study emphasizes the need for routine systematic surveillance of outbreaks.
ACKNOWLEDGEMENTS
The authors thank the consultants in communicable disease control, public health physicians, microbiologists, environmental health officers, infection control nurses, and all the staff at the HPA and NHS laboratories, without whose work this surveillance scheme would not function, and also Mrs S. Le Baigue, Mrs C. Hopcroft and Miss C. Penman who maintain the outbreak database at CfI.
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Food Standards Agency. www.foodstandards.gov.uk/pdf_files/business_plan.pdf. www.foodstandards.gov.uk/pdf_files/business_plan.pdf Business plan 2000/01. ). Accessed 10 March 2004.
- 2.Committee on the Microbiological Safety of Food. London: HMSO; 1990. The Microbiological Safety of Food. . Part 1, [Google Scholar]
- 3.Djuretic T et al. General outbreaks of infectious intestinal disease in England and Wales 1992 to 1994. Communicable Disease Report. CDR Review. 1996;6:R57–R63. [PubMed] [Google Scholar]
- 4.Evans HS et al. General outbreaks of infectious intestinal disease in England and Wales: 1995 and 1996. Communicable Disease and Public Health. 1998;1:165–171. [PubMed] [Google Scholar]
- 5.Gillespie IA et al. Milkborne general outbreaks of infectious intestinal disease, England and Wales, 1992–2000. Epidemiology and Infection. 2003;130:461–468. [PMC free article] [PubMed] [Google Scholar]
- 6.Dean AG Georgia: USD Inc.; 1990. Epi-Info, version 5: a word processing, database, and statistics programme for epidemiology on microcomputers. [Google Scholar]
- 7.National Library of Medicine. http://www.ncbi.nlm.nih.gov/PubMed/ http://www.ncbi.nlm.nih.gov/PubMed/ PubMed. ). Accessed 10 March 2004. [DOI] [PubMed]
- 8.Anon http://www.hpa.org.uk/cdr/CDR Weekly. Accessed 10 March 2004.
- 9.Walker RA et al. Decreased susceptibility to ciprofloxacin in outbreak-associated multiresistant Salmonella typhimurium DT104. Veterinary Record. 2000;147:395–396. doi: 10.1136/vr.147.14.395. [DOI] [PubMed] [Google Scholar]
- 10.Holtby I, Stenson P. Food poisoning in two homes for the elderly. Communicable Disease Report. CDR Review. 1992;2:R125–R126. [PubMed] [Google Scholar]
- 11.Patterson T, Hutchings P, Palmer S. Outbreak of SRSV gastroenteritis at an international conference traced to food handled by a post-symptomatic caterer. Epidemiology and Infection. 1993;111:157–162. doi: 10.1017/s0950268800056776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Riordan T, Humphrey TJ, Fowles A. A point source outbreak of campylobacter infection related to bird-pecked milk. Epidemiology and Infection. 1993;110:261–265. doi: 10.1017/s0950268800068187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Synnott M et al. An outbreak of Salmonella mikawasima associated with doner kebabs. Epidemiology and Infection. 1993;111:473–481. doi: 10.1017/s0950268800057204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ayres P et al. Food poisoning associated with a self-catered wedding reception. Communicable Disease Report. CDR Review. 1994;4:R62–R63. [PubMed] [Google Scholar]
- 15.Bonner D, Schweiger M. Apple pie: an unusual vehicle for food poisoning. Communicable Disease Report. CDR Review. 1994;4:R60–R61. [PubMed] [Google Scholar]
- 16.Dryden MS et al. Asymptomatic foodhandlers as the source of nosocomial salmonellosis. Journal of Hospital Infection. 1994;28:195–208. doi: 10.1016/0195-6701(94)90102-3. [DOI] [PubMed] [Google Scholar]
- 17.Lo SV et al. The role of the pre-symptomatic food handler in a common source outbreak of food-borne SRSV gastroenteritis in a group of hospitals. Epidemiology and Infection. 1994;113:513–521. doi: 10.1017/s0950268800068527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Morgan D et al. An outbreak of Campylobacter infection associated with the consumption of unpasteurised milk at a large festival in England. European Journal of Epidemiology. 1994;10:581–585. doi: 10.1007/BF01719576. [DOI] [PubMed] [Google Scholar]
- 19.Willshaw GA et al. Vero cytotoxin-producing Escherichia coli O157 in beefburgers linked to an outbreak of diarrhoea, haemorrhagic colitis and haemolytic uraemic syndrome in Britain. Letters in Applied Microbiology. 1994;19:304–307. doi: 10.1111/j.1472-765x.1994.tb00461.x. [DOI] [PubMed] [Google Scholar]
- 20.Wright JP et al. Food poisoning at a Masonic lodge. Communicable Disease Report. CDR Review. 1994;4:R58–R60. [PubMed] [Google Scholar]
- 21.Brugha RF et al. Chaos under canvas: a Salmonella enteritidis PT 6B outbreak. Epidemiology and Infection. 1995;115:513–517. doi: 10.1017/s0950268800058672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Evans MR, Parry SM, Ribeiro CD. Salmonella outbreak from microwave cooked food. Epidemiology and Infection. 1995;115:227–230. doi: 10.1017/s0950268800058350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fahey T et al. An outbreak of Campylobacter jejuni enteritis associated with failed milk pasteurisation. Journal of Infection. 1995;31:137–143. doi: 10.1016/s0163-4453(95)92160-5. [DOI] [PubMed] [Google Scholar]
- 24.Holtby I et al. Outbreak of Salmonella enteritidis phage type 4 infection associated with cheese and onion quiche. Communicable Disease Report. CDR Review. 1995;5:R118–R119. [PubMed] [Google Scholar]
- 25.Murphy O et al. An outbreak of campylobacter food poisoning in a health care setting. Journal of Hospital Infection. 1995;30:225–228. doi: 10.1016/s0195-6701(95)90318-6. [DOI] [PubMed] [Google Scholar]
- 26.Perrett K, Kudesia G. Gastroenteritis associated with oysters. Communicable Disease Report. CDR Review. 1995;5:R153–R154. [PubMed] [Google Scholar]
- 27.Davies A et al. An outbreak of Salmonella typhimurium DT104 food poisoning associated with eating beef. Communicable Disease Report. CDR Review. 1996;6:R159–R162. [PubMed] [Google Scholar]
- 28.Djuretic T, Wall PG, Nichols G. An outbreak of Salmonella infection from ice cream. New England Journal of Medicine. 1996;335:824–825. doi: 10.1056/NEJM199609123351118. [DOI] [PubMed] [Google Scholar]
- 29.Evans MR et al. A milk-borne campylobacter outbreak following an educational farm visit. Epidemiology and Infection. 1996;117:457–462. doi: 10.1017/s0950268800059112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Evans MR et al. Consecutive salmonella outbreaks traced to the same bakery. Epidemiology and Infection. 1996;116:161–167. doi: 10.1017/s0950268800052390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hastings L et al. Salm-Net facilitates collaborative investigation of an outbreak of Salmonella tosamanga infection in Europe. Communicable Disease Report. CDR Review. 1996;6:R100–R102. [PubMed] [Google Scholar]
- 32.Jakubovic MO, Hochuli VK. Food poisoning among clients of a meals on wheels service. Communicable Disease Report. CDR Review. 1996;6:R186–R188. [PubMed] [Google Scholar]
- 33.Killalea D et al. International epidemiological and microbiological study of outbreak of Salmonella agona infection from a ready to eat savoury snack – I: England and Wales and the United States. British Medical Journal. 1996;313:1105–1107. doi: 10.1136/bmj.313.7065.1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lewis DA et al. Marshmallows cause an outbreak of infection with Salmonella enteritidis phage type 4. Communicable Disease Report. CDR Review. 1996;6:R183–R186. [PubMed] [Google Scholar]
- 35.Stevenson J, Hanson S. Outbreak of Escherichia coli O157 phage type 2 infection associated with eating precooked meats. Communicable Disease Report. CDR Review. 1996;6:R116–R118. [PubMed] [Google Scholar]
- 36.Wight JP et al. Four outbreaks of Salmonella enteritidis phage type 4 food poisoning linked to a single baker. Communicable Disease Report. CDR Review. 1996;6:R112–R115. [PubMed] [Google Scholar]
- 37.Willocks LJ et al. Salmonella virchow PT 26 infection in England and Wales: a case control study investigating an increase in cases during 1994. Epidemiology and Infection. 1996;117:35–41. doi: 10.1017/s0950268800001102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chapman PA et al. An outbreak of infection due to verocytotoxin-producing Escherichia coli O157 in four families: the influence of laboratory methods on the outcome of the investigation. Epidemiology and Infection. 1997;119:113–119. doi: 10.1017/s0950268897007991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Clark A et al. A community outbreak of Vero cytotoxin producing Escherichia coli O157 infection linked to a small farm dairy. Communicable Disease Report. CDR Review. 1997;7:R206–R211. [PubMed] [Google Scholar]
- 40.Gelletlie R et al. Cryptosporidiosis associated with school milk. Lancet. 1997;350:1005–1006. doi: 10.1016/S0140-6736(05)64071-8. [DOI] [PubMed] [Google Scholar]
- 41.Holtby I et al. Outbreak of Salmonella enteritidis phage type 6 infection associated with food items provided at a buffet meal. Communicable Disease Report. CDR Review. 1997;7:R87–R90. [PubMed] [Google Scholar]
- 42.McDonnell RJ et al. An outbreak of Vero cytotoxin producing Escherichia coli O157 infection associated with takeaway sandwiches. Communicable Disease Report. CDR Review. 1997;7:R201–R205. [PubMed] [Google Scholar]
- 43.Patterson W et al. Outbreak of small round structured virus gastroenteritis arose after kitchen assistant vomited. Communicable Disease Report. CDR Review. 1997;7:R101–R103. [PubMed] [Google Scholar]
- 44.Stuart J et al. Outbreak of campylobacter enteritis in a residential school associated with bird pecked bottle tops. Communicable Disease Report. CDR Review. 1997;7:R38–R40. [PubMed] [Google Scholar]
- 45.Ang LH. An outbreak of viral gastroenteritis associated with eating raw oysters. Communicable Disease and Public Health. 1998;1:38–40. [PubMed] [Google Scholar]
- 46.Cornell J, Neal KR. Protracted outbreak of Salmonella typhimurium definitive phage type 170 food poisoning related to tripe, ‘pig bag’, and chitterlings. Communicable Disease and Public Health. 1998;1:28–30. [PubMed] [Google Scholar]
- 47.Dodhia H, Kearney J, Warburton F. A birthday party, home-made ice cream, and an outbreak of Salmonella enteritidis phage type 6 infection. Communicable Disease and Public Health. 1998;1:31–34. [PubMed] [Google Scholar]
- 48.Evans MR et al. A campylobacter outbreak associated with stir-fried food. Epidemiology and Infection. 1998;121:275–279. doi: 10.1017/s0950268898001204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Greenwood M, Winnard G, Bagot B. An outbreak of Salmonella enteritidis phage type 19 infection associated with cockles. Communicable Disease and Public Health. 1998;1:35–37. [PubMed] [Google Scholar]
- 50.Hansell AL et al. An outbreak of Salmonella enteritidis phage type 5a infection in a residential home for elderly people. Communicable Disease and Public Health. 1998;1:172–175. [PubMed] [Google Scholar]
- 51.Llewellyn LJ, Evans MR, Palmer SR. Use of sequential case-control studies to investigate a community Salmonella outbreak in Wales. Journal of Epidemiology and Community Health. 1998;52:272–276. doi: 10.1136/jech.52.4.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Maguire HC et al. Shigella outbreak in a school associated with eating canteen food and person to person spread. Communicable Disease and Public Health. 1998;1:279–280. [PubMed] [Google Scholar]
- 53.Rushdy AA et al. National outbreak of Salmonella senftenberg associated with infant food. Epidemiology and Infection. 1998;120:125–128. doi: 10.1017/s0950268897008546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Synnott MB et al. An outbreak of Salmonella agona infection associated with precooked turkey meat. Communicable Disease and Public Health. 1998;1:176–179. [PubMed] [Google Scholar]
- 55.Anon. E coli O157 food poisoning outbreak linked to milk. Veterinary Record. 1999;144:274. [PubMed] [Google Scholar]
- 56.Evans MR et al. An outbreak of Salmonella typhimurium DT170 associated with kebab meat and yogurt relish. Epidemiology and Infection. 1999;122:377–383. doi: 10.1017/s0950268899002253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fone DL, Lane W, Salmon RL. Investigation of an outbreak of gastroenteritis at a hospital for patients with learning difficulties. Communicable Disease and Public Health. 1999;2:35–38. [PubMed] [Google Scholar]
- 58.Gent RN, Telford DR, Syed Q. An outbreak of campylobacter food poisoning at a university campus. Communicable Disease and Public Health. 1999;2:39–42. [PubMed] [Google Scholar]
- 59.Threlfall EJ et al. Pulsed field gel electrophoresis identifies an outbreak of Salmonella enterica serotype Montevideo infection associated with a supermarket hot food outlet. Communicable Disease and Public Health. 1999;2:207–209. [PubMed] [Google Scholar]
- 60.Wilson D et al. Common source outbreak of salmonellosis in a food factory. Communicable Disease and Public Health. 1999;2:32–34. [PubMed] [Google Scholar]
- 61.Ejidokun OO et al. Four linked outbreaks of Salmonella enteritidis phage type 4 infection – the continuing egg threat. Communicable Disease and Public Health. 2000;3:95–100. [PubMed] [Google Scholar]
- 62.Maguire H et al. Hospital outbreak of Salmonella virchow possibly associated with a food handler. Journal of Hospital Infection. 2000;44:261–266. doi: 10.1053/jhin.1999.0712. [DOI] [PubMed] [Google Scholar]
- 63.Pearson AD et al. Continuous source outbreak of campylobacteriosis traced to chicken. Journal of Food Protein. 2000;63:309–314. doi: 10.4315/0362-028x-63.3.309. [DOI] [PubMed] [Google Scholar]
- 64.Metz R et al. Outbreak of Salmonella enteritidis gastrointestinal infections among medical staff due to contaminated food prepared outside the hospital. Journal of Hospital Infection. 2001;48:324–325. doi: 10.1053/jhin.2001.0989. [DOI] [PubMed] [Google Scholar]
- 65.Holtby I et al. Outbreak of Norwalk-like virus infection associated with salad provided in a restaurant. Communicable Disease and Public Health. 2001;4:305–310. [PubMed] [Google Scholar]
- 66.Mason BW et al. Outbreak of Salmonella indiana associated with egg mayonnaise sandwiches at an acute NHS hospital. Communicable Disease and Public Health. 2001;4:300–304. [PubMed] [Google Scholar]
- 67.Steel N, Myers L, Bailey J. An outbreak of viral gastro-enteritis at a charity function. Communicable Disease and Public Health. 2001;4:68–70. [PubMed] [Google Scholar]
- 68.Goh S et al. E. coli O157 phage type 21/28 outbreak in North Cumbria associated with pasteurized milk. Epidemiology and Infection. 2002;129:451–457. doi: 10.1017/s0950268802007835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ward LR et al. Collaborative investigation of an outbreak of Salmonella enterica serotype Newport in England and Wales in 2001 associated with ready-to-eat salad vegetables. Communicable Disease and Public Health. 2002;5:301–304. [PubMed] [Google Scholar]
- 70.Duncanson P, Wareing DR, Jones O. Application of an automated immunomagnetic separation-enzyme immunoassay for the detection of Salmonella spp. during an outbreak associated with a retail premises. Letters in Applied Microbiology. 2003;37:144–148. doi: 10.1046/j.1472-765x.2003.01365.x. [DOI] [PubMed] [Google Scholar]
- 71.Anon. http://www.hpa.org.uk/cdr/CDR Weekly. Accessed 10 March 2004.
- 72.Anon. Directive 2003/99/EC of the European Parliament and of the Council of 17 November, 2003 on the monitoring of zoonoses and zoonotic agents, amending Council Decision 90/424/EEC and repealing Council Directive 92/117/EEC. Official Journal of the European Union. 2003;46:L325/31–L325/40. [Google Scholar]


