SUMMARY
Nyanza Province, Kenya is characterized by poor water quality and high diarrhoea prevalence. To address these problems, nurses in a maternal and child health clinic in Homa Bay, Kenya were trained in household water chlorination with a locally available, social marketed product, and in six steps of proper hand washing. They were asked to communicate this information to their clients. Interviews immediately following the training by nurses were conducted on 220 clients, of whom 168 (76%) reported being taught both procedures during their clinic visit. After 2 weeks, free chlorine residuals were present in stored drinking water in 67 out of 98 (68%) clients' homes and, 1 year later, in 36 out of 51 (71%) clients' homes. After 2 weeks, all six hand-washing steps were correctly demonstrated by 41 (44%) out of 93 clients, and by 17 out of 51 (34%) 1 year later. This brief, practical intervention shows promise for vulnerable populations.
INTRODUCTION
Over one sixth of the world's population lacks access to safe drinking water sources. Unsafe water supplies, along with deficient sanitary infrastructure and inadequate personal hygiene, contribute substantially to the burden of 2·2 million annual deaths from diarrhoeal diseases [1].
Although the definitive solution to the problem of access to safe water is the universal provision of piped, treated water, this option remains elusive because of the enormous expenditure of money and time that is required [2]. In response to a need for interim measures to protect health, the Centers for Disease Control and Prevention (CDC) developed the Safe Water System (SWS), a household-based approach for making drinking water safe. The SWS involves three components: (1) point-of-use disinfection with a locally produced sodium hypochlorite solution, (2) safe water storage, and (3) behaviour change communications [3]. In field trials, use of the SWS resulted in a reduction of risk of diarrhoea of 26–85% [4–7].
In 2000, the non-governmental organization (NGO), CARE, implemented the SWS in 72 rural villages in southern Nyanza Province, Kenya, a region characterized by poor source water quality and high diarrhoea prevalence [8]. In May 2003, another NGO, Population Services International (PSI), expanded access to the SWS through a social marketing campaign in which the bottled disinfectant solution was distributed through the commercial sector under the brand name WaterGuard¯. An evaluation of WaterGuard adoption, conducted in December 2003 in Homa Bay, a town of 30 000 in southern Nyanza Province, found that 14% of the population was using the product (P. Ogutu, unpublished data).
To boost adoption of the SWS, CARE explored alternative implementation strategies, one of which was training nurses in the Maternal and Child Health (MCH) clinic in Homa Bay, to motivate their clients to adopt the SWS as part of regular nursing practice. Since the SWS can be used as a platform to facilitate the promotion of related diarrhoea prevention interventions [9], we incorporated instruction on proper hand washing into the nurse training sessions. Hand washing with soap has been shown to reduce diarrhoea risk by over 40% [10]. However, many hand-washing interventions are expensive and labour intensive, and can be difficult to scale up and sustain [11, 12]. In this report, we describe the results of an evaluation of the impact of this low-cost, brief nursing intervention on the utilization of the SWS and knowledge of proper hand-washing practices among clinic clients.
METHODS
Project design
The project had six components: (1) nurse training sessions on the SWS and hand-washing techniques, (2) a follow-up survey of nurses to measure retention of the educational material 2 weeks after the training, (3) client education by the nurses on the SWS and hand-washing techniques, (4) client exit interviews immediately following the educational intervention, (5) follow-up interviews in clients' homes 2 weeks after the exit interviews, and (6) follow-up interviews in clients' homes 1 year following the initial home visit to measure adoption of recommended water treatment practices and knowledge retention of proper hand-washing steps.
Informed consent
This protocol was approved by the Emory University Institutional Review Board (IRB). The CDC IRB determined that this work represented programme evaluation of a proven public health intervention; accordingly, approval of the protocol by the CDC IRB was unnecessary. Informed consent was obtained from all participants.
Nurse training
Between 29 June and 9 July 2004, all 11 nurses employed in the MCH clinic attended a 4-hour training session on how to incorporate the SWS and hand-washing instruction into their regular clinical practice. We taught nurses about the components and appropriate use of the SWS and proper hand-washing techniques using a six-step process: (1) use soap and water; (2) rub hands together for 10–15 s; (3) rub between fingers; (4) clean under nails; (5) rinse; and (6) air dry, if no clean towel is available. All nurses were provided teaching materials, which included a laminated guide to proper use of the SWS and hand-washing procedures, as well as a pocket guide summarizing the same information to use with their clients. Each nurse completed a post-test following the training course to measure comprehension of the material.
Nurse follow-up survey
A knowledge, attitudes, and practice (KAP) survey was administered to the nurses between 21 and 23 July 2004. The survey consisted of 51 questions about knowledge of the SWS and hand-washing, whether they had taught the information to their clients, and their personal hand-washing and water-treatment practices. Post-test questions from the training session were also included to assess knowledge retention.
Client education
On 12 July 2004, the nurses initiated client education sessions on the SWS, hand-washing techniques, and diarrhoea prevention messages at the MCH clinic in the local language, Dholuo. These sessions were incorporated as part of daily nursing responsibilities, lasting 5 min for one-to-one encounters and ∼30 min for groups (varying from eight to 50 individuals). The instruction consisted of lectures, demonstrations, discussions, and question-and-answer sessions. We encouraged the nurses to teach the material to all persons visiting the MCH clinic, which served about 220 clients per day.
Post-training client interviews
Upon leaving the clinic, every fourth MCH client was selected to participate in a post-training interview. The interview, which consisted of 50 questions, including some open-ended queries with pre-coded responses, was designed to obtain information on current water-treatment, storage, and hand-washing practices, beliefs about diarrhoea prevention, information learned during their clinic appointment, and attitudes about the newly acquired information.
Client 2-week follow-up surveys
Ninety-eight (53%) of the 186 clients who had received education on the SWS at the clinic were selected using a random-numbers table for follow-up at home. The visits, which took place from 19 to 29 July 2004, were conducted on a surprise basis in order to reduce the likelihood that respondents would prepare for the enumerator's arrival. Due to time and budget constraints, 33 (18%) clients who lived beyond a 30-km radius of the MCH clinic were excluded.
Client interviews, which were conducted by trained bilingual enumerators, elicited information about household demographic characteristics; knowledge, attitudes, and practices regarding the SWS and hand washing; and possession of certain household items that were used to calculate wealth indices as a proxy measure of socioeconomic status through principal component analysis (PCA) methodology developed by the World Bank [13]. Observations were made of the presence of WaterGuard bottles, soap, and a hand-washing station in the home. Stored water was tested for residual free chlorine using the N, N-diethyl-p-phenylenediamine (DPD) colorimetric method (Free and Total Chlorine kits, Hach Company, Loveland, CO, USA); any level above 0·1 mg/l was considered adequate treatment (no water sources in Homa Bay are chlorinated). Ninety-three (95%) of the 98 clients who had also been taught hand washing at the clinic were asked to demonstrate hand-washing techniques.
Client 1-year follow-up surveys
In July 2005, a random sample of 51 (52%) of 98 clients from the 2-week follow-up survey was selected using a random-numbers table for a 1-year follow-up interview that included questions and observations regarding WaterGuard use and knowledge of hand-washing techniques.
Data analysis
Epi-Info version 2002 (CDC, Atlanta, GA, USA) and SAS version 9.1 (SAS Institute Inc., Cary, NC, USA) software were used to analyse the data. χ2 tests, Fisher's exact tests, and analysis of variance (ANOVA) were conducted to examine associations between selected independent variables and outcome measures. PCA was used to group the evaluation population into socioeconomic quintiles by calculating a total asset score derived from the analysis of selected household asset variables [13]. ANOVA was used to compare different scores for knowledge and use of WaterGuard across quintiles.
RESULTS
Nurses
The median age of the 11 nurses in the MCH Clinic was 49 years (range 36–56 years); six (54·5%) were female. The median number of years they had worked as nurses was 26 years (range 6–32 years). All MCH nurses received the SWS and hand-washing training. Immediately following the training, seven nurses scored 100% on the post-test, three scored 91%, and one scored 62%.
In the KAP survey 2 weeks later, five (46%) of the 11 nurses reported that they had heard of the SWS before the training from a variety of other sources, including radio (2), newspaper (1), school (1), and the supermarket (1). The majority of nurses (55%) reported spending <5 min with individual clients during an average clinic visit. All nurses reported teaching the SWS and hand washing, and 10 (91%) reported using the SWS and hand-washing teaching materials that they received during the training session. All 11 nurses reportedly told their clients where to purchase WaterGuard. Two weeks after the training sessions, the nurses' median score on the same post-test was 92% (range 85–100%).
Clients
Post-training client interviews
A total of 220 (20%) of ∼1100 clients were interviewed upon leaving the MCH clinic over a 1-week period. The reasons for visit included: well-child or immunizations for 111 (51%), antenatal services for 31 (14%), and family planning for 14 (6%); 64 (29%) visits were for a sick child, including 27 (42%) with diarrhoea. Of the 220 clients, 186 (85%) reported that they had received information from a nurse on the SWS, 176 (80%) on hand washing, and 168 (76%) on both the SWS and hand washing.
Client 2-week follow-up surveys
Demographics
Follow-up visits were conducted in the homes of 98 (53%) of 186 clients who had acknowledged receiving SWS instruction. The median age of clients was 24 years (range 15–42 years); 92 (94%) were women. Seven (7%) could not read and 51 (52%) had a primary school education or less. The occupational categories of the heads of the 98 respondents' households included business people such as carpenters and tailors (38%), salaried workers such as social worker or water department employee (14%), teachers (13%), civil servants (7%), farmers (7%), fishermen (7%), taxi drivers (6%), bicycle/rickshaw drivers (6%), and unemployed (3%).
Water sources, storage, and treatment
The primary water source used by interviewees was piped water from public taps (61%). All 98 respondents stored water in their homes, 89 (91%) of whom used clay pots (Table 1).
Table 1.
Water sources, storage, and treatment
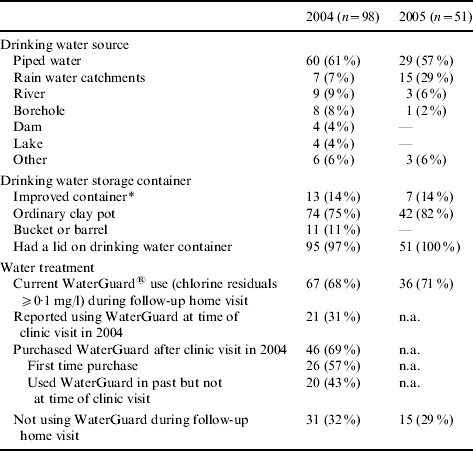
n.a., Not applicable.
Improved container is a modified clay pot or a jerrycan.
Of 98 respondents, free chlorine residuals (indicating the presence of WaterGuard) were found in the home drinking-water storage containers of 67 (68%), 21 (31%) of whom reported that they were already using WaterGuard at the time of the educational session at the clinic (Table 1). Forty-six (69%) of the 67 WaterGuard users reported purchasing a bottle of WaterGuard after their clinic visit; 26 (57%) had never before purchased the product while the other 20 respondents had not been using it at the time of their clinic visit (Table 1). The reasons given for purchasing WaterGuard included importance of treating water (48%), diarrhoea prevention (46%), unclean water (46%), ease of use (35%), and less expensive than their current method (26%).
Of 31 respondents not currently treating their water with WaterGuard, 14 (45%) reported having no WaterGuard in their home, 10 (32%) used another method, 5 (16%) had no money to buy the product, and 2 (7%) did not like the smell or taste of WaterGuard.
Of the 98 respondents, 60 (61%) reported that they taught SWS information they had learned in the clinic to their neighbours, families, friends, or co-wives. Of these 60, 41 (68%) had detectable chlorine levels in their water storage vessels and 19 did not. There was no significant difference in whether or not clients reported teaching others the information based upon whether they themselves were using the product at the time of the home visit.
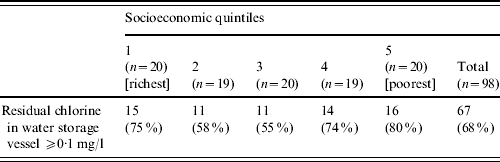
Educational level, occupational category, and water source were not associated with use of WaterGuard. There were no significant differences in knowledge about WaterGuard by socioeconomic status. Moreover, there was no significant difference in WaterGuard usage by socioeconomic status, as calculated by quintiles determined through PCA (Table 2).
Table 2.
WaterGuard usage according to socioeconomic status (calculated by quintiles determined by PCA)
Hand washing
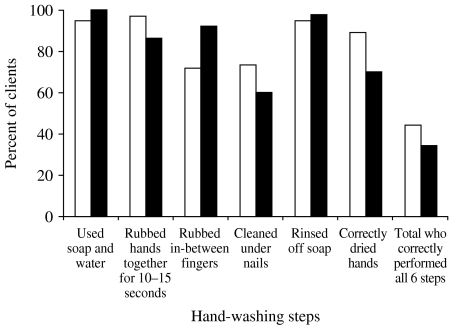
Of the 98 respondents, 93 (95%) reported that they were taught hand washing during their clinic visit. Of these 93 clients, 41 (44%) correctly performed all six hand-washing steps in a demonstration during the home visit (Fig.). Fifty-five clients (59%) performed at least five of the six steps correctly, and 75 (81%) performed at least four of the six steps correctly. The steps most frequently missed were rubbing in-between fingers (28%) and cleaning under fingernails (27%).
Fig.
Clients' performance on the six hand-washing steps demonstrated during a home visit. □, 2004; ■, 2005.
When asked to indicate when one should wash hands, respondents reported the following: after using the latrine (97%), before eating (94%), and after cleaning up a child who has defecated (53%). With regards to hand-washing attitudes, 86 (88%) reported that hand washing is very important in diarrhoea prevention. Of 93 respondents who were taught hand washing by the nurses, 86 (93%) had hand soap and 85 (91%) had wash basins.
Client 1-year follow-up surveys
WaterGuard use remained high 1 year after the initial follow-up home visit, with detectable chlorine residuals in 36 out of 51 (71%) client water storage vessels (Table 1). Retention of knowledge about hand-washing techniques among respondents also remained high after 1 year, with 17 (34%) of 51 clients able to demonstrate all six hand-washing steps (Fig.), and 50 (98%) correctly demonstrating at least four steps. A wash basin and soap were present in all 51 (100%) of the clients' homes.
DISCUSSION
Clients of the Homa Bay MCH clinic who received instruction from nurses on proper use of the SWS and hand washing with soap exhibited consistently high levels of WaterGuard use and hand-washing knowledge retention over a 1-year period. The adoption of WaterGuard, which included purchasing and using the solution correctly, was nearly as high as in efficacy studies in which WaterGuard was given away [4, 5]. The retention of knowledge of hand-washing steps was also greater than expected, given the low intensity of this intervention, which typically involved only one 5–10 min instructional session, much less than has been implemented in other hand-washing intervention trials [11, 14–16].
This clinic-based intervention was effective irrespective of variation in client age, educational level, and socioeconomic status. Other studies have suggested that younger age, less schooling, and lower socioeconomic status can be barriers to the adoption of the SWS [5, 17]. Factors that may have contributed to the high levels of WaterGuard use and hand-washing knowledge 1 year after the clinic-based intervention include nurse competency in SWS and hand-washing instruction, a high client-reported frequency of having received instruction on both interventions, culturally appropriate educational methods, and concomitant social marketing of WaterGuard which reinforced the nurses' messages. Since nurses are among the most trusted sources of health advice [18, 19], clients may have been more motivated to try the SWS and hand-washing interventions promoted by nurses than by social marketing messages. Further evaluation will be necessary to determine which, if any, of the above factors are important determinants of the impact of this intervention.
Social marketing cannot be ruled out as a factor in WaterGuard adoption in this population because most individuals had been previously exposed to WaterGuard through PSI's social marketing campaign. However, it is not likely that prior exposure to WaterGuard marketing alone would have led to the high product utilization rates found in this evaluation. Previous community-based studies of the SWS suggest that social marketing alone does not typically lead to high utilization rates [17, 20, 21]. A population-based evaluation of WaterGuard use in Homa Bay in December 2003 showed a utilization rate of 14% only 6 months before the clinic-based intervention was implemented (P. Ogutu, unpublished data).
In spite of the apparent success of the clinic-based SWS intervention, the evaluation had several limitations. First, we did not collect baseline data on WaterGuard knowledge or use because the evaluation population was selected at the time of the clinic visit, which would have made it likely that baseline interviews on these topics just before the training session would have influenced their post-training questionnaire responses. Although the lack of baseline data prevented a measurement of the magnitude of the effect of the intervention, it is plausible that the nursing intervention had an impact, because 46 (69%) of 67 clients who had free chlorine residuals in their home water-storage containers at the 2-week follow-up visit reported that they purchased the product following their educational session with the nurse; of these, 26 were new users of WaterGuard, while 20 reported not using the product at the time of the clinic visit.
Second, the population was drawn from clinic attendees who were probably not representative of the general Homa Bay population, as suggested by the high percentage of clients with businesses or salaried jobs in a community where many work in the informal economy. Clinic attendees may have had more disposable income, better access to health services than the general population, and a higher health awareness and disposition towards preventive behaviour. As a result, this population may have been more likely to purchase WaterGuard or be exposed to hand-washing instruction.
Third, the high percentage of clients trained by nurses, as well as the high SWS adoption and hand-washing knowledge retention among clients could be at least partly explained by the Hawthorne effect [22]. However, the risk of the Hawthorne effect on the follow-up evaluations was reduced by making unscheduled visits to clients' homes. Furthermore, surprise visits to the hospital after clinic-based data collection was completed verified that nurses continued to teach the material.
On a broader scale, a potential limitation for a clinic-based intervention is the global nursing shortage which has drastically reduced the nursing workforce, especially in Africa [23, 24]. The nursing shortage caused by the out-migration of professional nurses from low-income to high-income countries, and by deaths from AIDS among nurses in Africa, limits the capacity for those who remain to provide preventive services [23–26]. However, by training other categories of health workers which are not recognized by the developed world and, therefore, do not have the option of out-migrating, the capacity to deliver preventive services like the SWS and hygiene training could be enhanced and help offset the nursing shortage. This strategy would require investigation into whether other health-worker categories would elicit the same degree of trust, and perform as effectively, as nurses.
Although the persistently high rates of WaterGuard use and hand-washing knowledge retention demonstrated by MCH clinic clients cannot be directly attributed to the nursing intervention they received, it is plausible that the intervention did contribute at least in part to this outcome. As such, this intervention is particularly promising because, unlike many interventions that successfully promote preventive behaviours, it is brief in duration, which could make it practical in resource-poor settings. To further explore its potential, additional evaluations of this approach to disease prevention are being planned in Kenya and other countries.
ACKNOWLEDGEMENTS
This research could not have been possible without the support of the CARE-Kenya staff, including John Migele, Mary Ayole, and Ajode Meshak who assisted with the development of the survey tools, translation, and supervision of the data collection; Paul Ogutu, who provided population-based data from his Homa Bay study on SWS usage; the Homa Bay District Clinic staff, especially Dickens Odhiambo, Gordon Ohunga, and Charles Gwalla who allowed the researchers to conduct the evaluation in their facility and assisted with random sampling; the Kenyan Ministry of Health; and the four enumerators, Cindy Omondi, Jullie Akiri, Eric Ngutu, and Erick Odhiambo, who collected the data. We are grateful to Pamela McQuide, Ph.D., of Emory University, who critically reviewed the evaluation proposal. We are also appreciative of the contributions made by Richard Rheingans, Ph.D., of Emory University, who served as a technical advisor, specifically regarding the PCA methodology. Finally, we express our gratitude to the Eugene Gangarosa Foundation and the Office of Global Health at the CDC who provided financial support.
DECLARATION OF INTEREST
None.
Footnotes
Use of trade names is for identification only and does not constitute endorsement by the Centers for Disease Control and Prevention or by the Department of Health and Human Services.
REFERENCES
- 1.World Health Organization, United Nations Children's Fund, Water Supply and Sanitation Council New York, NY: UNICEF; 2000. . Global Water Supply and Sanitation Assessment 2000 Report. [Google Scholar]
- 2.WHO World Health Organization; . Managing water in the home: accelerated health gains from improved water supply, 2005. ). Accessed 4 November 2005. [Google Scholar]
- 3.CDC. Safe Water Systems for the Developing World: a handbook for implementing household-based water treatment and safe storage projects. Atlanta, GA: Centers for Disease Control and Prevention; 2000. [Google Scholar]
- 4.Quick RE et al. Diarrhea prevention through household-level water disinfection and safe storage in Zambia. American Journal of Tropical Medicine and Hygiene. 2002;66:584–589. doi: 10.4269/ajtmh.2002.66.584. [DOI] [PubMed] [Google Scholar]
- 5.Quick RE et al. Diarrhoea prevention in Bolivia through point-of-use water treatment and safe storage: a promising new strategy. Epidemiology and Infection. 1999;122:83–90. doi: 10.1017/s0950268898001782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Luby SP et al. Delayed effectiveness of home-based interventions in reducing childhood diarrhea, Karachi, Pakistan. American Journal of Tropical Medicine and Hygiene. 2004;71:420–427. [PubMed] [Google Scholar]
- 7.Crump J et al. Household based treatment of drinking water with flocculant-disinfectant for preventing diarrhoea in areas with turbid source water in rural western Kenya: cluster randomised control trial. British Medical Journal. 2005;331:478. doi: 10.1136/bmj.38512.618681.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Makutsa P et al. Challenges in implementing a point-of-use water quality intervention in rural Kenya. American Journal of Public Health. 2001;91:1571–1573. doi: 10.2105/ajph.91.10.1571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mintz E et al. Not just a drop in the bucket: expanding access to point-of-use water treatment systems. American Journal of Public Health. 2001;91:1565–1570. doi: 10.2105/ajph.91.10.1565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Curtis V, Cairncross S. Effect of washing hands with soap on diarrhoea risk in the community: a systematic review. Lancet Infectious Diseases. 2003;3:275–281. doi: 10.1016/s1473-3099(03)00606-6. [DOI] [PubMed] [Google Scholar]
- 11.Luby S et al. Effect of intensive hand washing promotion on childhood diarrhea in high-risk communities in Pakistan: a randomized controlled trial. Journal of the American Medical Association. 2004;291:2547–2554. doi: 10.1001/jama.291.21.2547. [DOI] [PubMed] [Google Scholar]
- 12.Cairncross S et al. What causes sustainable changes in hygiene behaviour? A cross-sectional study from Kerala, India. Social Science and Medicine. 2005;61:2212–2220. doi: 10.1016/j.socscimed.2005.04.019. [DOI] [PubMed] [Google Scholar]
- 13.Gwatkin D HNP/Poverty Thematic Group of the World Bank; 2000. . Socioeconomic Differences in Health, Nutrition, and Population in Kenya. [Google Scholar]
- 14.Stanton B, Clemens J. An educational intervention for altering water-sanitation behaviors to reduce childhood diarrhea in urban Bangladesh. II. A randomized trial to assess the impact of the intervention on hygienic behaviors and rates of diarrhea. American Journal of Epidemiology. 1987;125:292–301. doi: 10.1093/oxfordjournals.aje.a114529. [DOI] [PubMed] [Google Scholar]
- 15.Curtis V et al. Evidence of behaviour change following a hygiene promotion programme in Burkina Faso. Bulletin of the World Health Organization. 2001;79:518–527. [PMC free article] [PubMed] [Google Scholar]
- 16.Manun'Ebo M et al. Measuring hygiene practices: a comparison of questionnaires with direct observations in rural Zaire. Tropical Medicine and International Health. 1997;2:1015–1021. doi: 10.1046/j.1365-3156.1997.d01-180.x. [DOI] [PubMed] [Google Scholar]
- 17.Olembo L http://www.ehproject.org/PDF/Others/Zambia%20Report%20Format.pdf. http://www.ehproject.org/PDF/Others/Zambia%20Report%20Format.pdf . Safe water systems: an evaluation of the Zambia CLORIN program, 2004. Narrative Safe Water System Evaluation Report ( ). Accessed 4 November 2005.
- 18.Ulmer B. The image of nursing. AORN Journal. 2000;71:1124–1127. doi: 10.1016/s0001-2092(06)61427-0. [DOI] [PubMed] [Google Scholar]
- 19.World Health Organization Regional and global Trends in Nursing and Midwifery Geneva: 2000. . Global Advisory Group on Nursing and Midwifery: Report of the Sixth Meeting. ). Accessed 4 November 2005. [Google Scholar]
- 20.Thevos A et al. Adoption of safe water behaviors in Zambia: comparing educational and motivational approaches. Education for Health. 2000;13:366–376. doi: 10.1080/135762800750059480. [DOI] [PubMed] [Google Scholar]
- 21.Dunston C et al. Collaboration, cholera, and cyclones: improving point-of-use water quality in Madagascar. American Journal of Public Health. 2001;91:1577–1579. doi: 10.2105/ajph.91.10.1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Adair J. The Hawthorne effect: a reconsideration of the methodological artifact. Journal of Applied Psychology. 1984;69:334–345. [Google Scholar]
- 23.Peterson C. In short supply: around the world, the need for nurses grows. http://www.nursingworld.org/AJN/2001/sept/Issues.htm. American Journal of Nursing. 2001;101 ). Accessed 4 November 2005. [Google Scholar]
- 24.Trossman S. The global reach of the nursing shortage: the ANA questions ethics of luring foreign-educated nurses to the United States. American Journal of Nursing. 2002;102:85–87. doi: 10.1097/00000446-200203000-00031. [DOI] [PubMed] [Google Scholar]
- 25.Kingma M. Nursing migration: global treasure hunt or disaster-in-the-making. Nursing Inquiry. 2001;8:205–212. doi: 10.1046/j.1440-1800.2001.00116.x. [DOI] [PubMed] [Google Scholar]
- 26.Hamilton K, Yau J http://www.migrationinformation.org/Feature/display.cfm?id=271. http://www.migrationinformation.org/Feature/display.cfm?id=271 . The global tug-of-war for health care workers ( ). Migration Policy Institute, 2004. Accessed 4 November 2005.