SUMMARY
In the summer of 2001 an outbreak of Escherichia coli O157 gastroenteritis affected staff and residents of a care home for the elderly in the West Midlands, UK. E. coli O157 phage type 2 was isolated from faeces in eight patients and 12 staff members. Thirty-five staff and 40 residents met the case definition for clinical gastrointestinal infection. Serological testing identified a further 14 possible cases of infection amongst asymptomatic staff and residents. The outbreak was atypical, as the disease seemed to be milder than has been observed in past outbreaks in similar settings. The index case, a member of staff, developed bloody diarrhoea and haemolytic–uraemic syndrome (HUS), but only one resident developed bloody diarrhoea and required hospitalization. No deaths occurred, despite the high-risk nature of the affected population. The source of the outbreak could not be identified. The prolonged nature of the outbreak and observed lapses in infection control practices indicated that person-to-person spread was the likely route of transmission. This outbreak illustrates the importance of observing appropriate infection control measures in the institutions providing residential and nursing care to the elderly.
INTRODUCTION
Since 1982, Escherichia coli O157:H7 has emerged as the major human pathogenic serotype of Vero cytotoxic E. coli (VTEC) in the United Kingdom and North America [1]. Infection with E. coli O157 may cause no symptoms or abdominal pain and a diarrhoeal illness, which may result in haemorrhagic colitis. The incubation period ranges from 2 to 8 days with a median of 3–4 days. The infectious dose is very low. About 5% of cases progress to haemolytic–uraemic syndrome (HUS) with renal failure. The overall case-fatality rate in outbreaks is between 0 and 2%, but rates from 16 to 35% have been reported in nursing homes [2]. Other complications are haemolytic anaemia and thrombotic thrombocytopaenic purpura (TTP).
The largest outbreak in the United Kingdom occurred in Scotland and affected 490 people, 18 of whom, all elderly, died [3]. Outbreaks of infection with E. coli O157 have been associated with a variety of foods such as meat and dairy products, contaminated vegetables, mayonnaise and non-fermented apple cider [4–8]. E. coli O157 has also been isolated from farm animals, wild birds and household pets [9–11]. Direct spread has been shown to occur from animals to their keepers and to members of the public at farm visitor centres [12–16]. Person-to-person transmission, particularly relevant in outbreaks associated with day-care nurseries and nursing homes, is well recognized [17–23], as are water-borne outbreaks, due mainly to faecal contamination of drinking water or recreational bathing water [24–30]. This report describes an outbreak of E. coli O157 infection in a care home for the elderly in the West Midlands, United Kingdom.
METHODS
On 13 July 2001, North Staffordshire Hospital (Stoke-on-Trent, UK) informed the Public Health Department of North Staffordshire Health Authority of a patient with HUS with a positive stool culture for E. coli O157. The patient, and index case, was a member of staff at a local nursing and residential home for the elderly. This individual developed diarrhoea on 9 July 2001, and the isolation of E. coli O157 here initiated the investigation, with another member of the staff who also developed diarrhoeal illness on 9 July having a positive stool culture for E. coli O157.
The care home provided social and nursing care facilities for 139 elderly residents, and consisted of five nursing units, two for elderly mentally ill and three for frail elderly residents. Staff worked and rotated across all units in the home, and over the period of the outbreak, a total of 181 individuals were employed. One main kitchen provided residents and night staff with meals. Satellite kitchens in the five units were used for preparing toast and beverages and serving pre-prepared food. The home did not provide meals to staff working during the day.
An outbreak control team (OCT) was convened on 20 July 2001. A confirmed case was defined as any person with a stool culture found to be positive for E. coli O157 since 1 July 2001 residing or working in the home. An epidemiologically linked clinical (probable) case was a person with:
three or more loose stools in 24 h;
or any episode of blood in the stool;
or two out of three of the following symptoms: vomiting, abdominal pain, fever.
A possible (asymptomatic) case was defined as a person identified later by non-culture laboratory investigations after the outbreak concluded.
Case finding
Case finding was conducted by routine surveillance throughout North Staffordshire, and reports of any cases arising in the community from General Practitioners, hospital clinical and microbiology staff. Environmental Health Officers interviewed symptomatic staff and completed a standard VTEC O157 ‘trawling’ questionnaire. This questionnaire covered a range of potential exposures over the 7 days prior to the onset of symptoms in the index case, and included questions on foods eaten and places recently visited such as farms or food venues. This was later replaced by a case-finding questionnaire developed by the OCT. Faecal samples were also requested from all staff, as well as family members of the confirmed cases, and from symptomatic residents identified from nursing notes.
Environmental investigation
The environmental health investigation included inspection of the institution's sanitary conditions. Facilities for food storage and preparation were inspected and kitchen staff were observed whilst preparing food. The home did not keep the samples of food served to residents or staff, and information about menus was incomplete. Samples of water and swabs from a milk dispenser and kitchen surfaces were collected and sent to the public health laboratory. The audit of infection control practices was undertaken at a very early stage in the outbreak. This included observing for hand-washing facilities, environmental cleanliness, safe handling and disposal of clinical waste, disinfection standards and clinical practices to reduce the risk of cross infection [31].
Microbiological investigations
Faeces, food and water samples were tested for common enteric pathogens including E. coli O157, using Sorbitol–MacConkey medium at the Stoke-on-Trent Public Health Laboratory. Isolates of presumptive E. coli O157 were sent to Public Health Laboratory Service (now Health Protection Agency) Laboratory of Enteric Pathogens (LEP), Colindale, London, where stool specimens were also examined by immunomagnetic bead enrichment culture (IMBEC), with confirmation of E. coli O157 by verotoxin polymerase chain reaction (PCR). The assays and primers used were the same as reported in an earlier outbreak investigation elsewhere [32].
An experimental salivary antibody test was being evaluated by LEP for its usefulness in the management of outbreaks of E. coli O157 infection [33].
Ethics Committee approval was obtained, and blood and salivary specimens were collected between 21 and 29 August 2001 from staff and residents who gave consent.
RESULTS
Epidemiology
The analysis of the questionnaires failed to identify the source of the infection in the care home. The outbreak affected all units in the home and both staff and residents. Twenty cases met the definition for confirmed cases of E. coli O157, of these 12 were staff and eight residents. Seventy-five clinical cases were identified within the duration of the outbreak, 1 July to 18 August 2001. Of these 35 were staff members and 40 residents. Attack rates appeared to be higher amongst residents compared to staff, but the difference was not statistically significant. None of the kitchen staff were included amongst the confirmed, probable or possible cases.
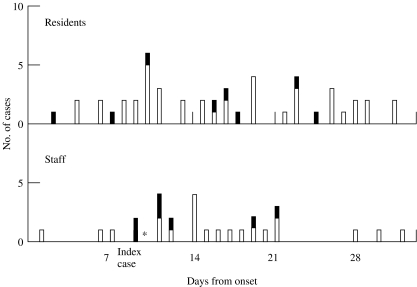
Fourteen possible cases were identified through serological investigations after the conclusion of the outbreak. The Table summarizes the symptom profile of the cases, and the epidemic curve (Fig.) shows the 15 confirmed and 62 clinical cases with known dates of onset of illness. The date of onset for confirmed cases range from 2 to 25 July, and clinical cases from 1 July to 1 August 2001. The date of onset (2 July) of illness in the first retrospectively confirmed case, a resident, preceded the date of onset of illness of the index case (a staff member) by 7 days. The two confirmed cases in residents before the index case (Fig.) were retrospectively identified by the case-finding exercise, with subsequent collection of stool specimens from which E. coli O157 was identified. The assumption was that the organism was present at the time the clinical symptoms were recorded. The mean age of affected staff was 38 years (minimum 18 years, maximum 61 years), whereas the mean age of residents was 80 years (minimum 45 years, maximum 94 years).
Table.
Cases identified during the outbreak of E. coli O157 in the care home in North Staffordshire
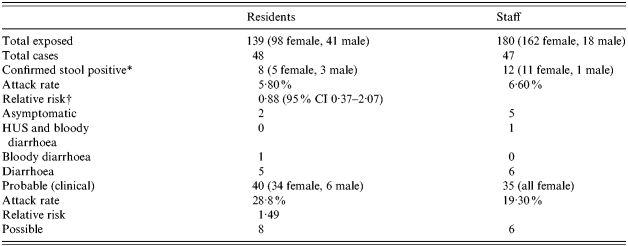
HUS, Haemolytic–uraemic syndrome.
Positive for the outbreak strain by culture, IMBEC and PCR.
Residents vs. staff.
Fig.
Epidemic curve of 15 confirmed (■) and 62 clinical cases (□) in this outbreak, for which there were known dates of onset of symptoms, with the first case retrospectively identified on 1 July 2001. The index case (staff member) is indicated by the asterisk (*).
One staff member (the index case, aged 41 years) and one resident (aged 70 years), both females, required hospitalization. There were no deaths attributable to the outbreak (one resident died during the outbreak of unrelated causes). No cases were identified at the time in the community or amongst the family members of staff who were tested.
Environmental investigation
The food preparation standards were generally good. However, a potential for cross contamination was observed when the same preparatory surface was used for handling raw and cooked foods in the main kitchen. The infection control audits identified poor facilities for hand washing for staff, their rotation from clean to dirty jobs along with the practice of hanging clean and used uniforms side by side as significant lapses in infection control measures.
Microbiological investigations
The outbreak strain, phage type (PT) 2 was isolated from 20 cases, 13 by enrichment culture and seven by IMBEC and verotoxin gene PCR.
Serological testing detected evidence of infection with E. coli O157 in 26% (22/85) of serum samples and 10% (7/66) of salivary specimens. Fourteen additional cases were identified by this method. Five of these cases were serum and saliva lipopolysaccharide (LPS) antibody positive, seven only serum antibody positive and two only saliva antibody positive. None of the environmental or food and water samples grew E. coli O157. The cultures for rotavirus, salmonella, shigella, and campylobacter were negative.
DISCUSSION
This report describe a large outbreak of E. coli O157 in a care home for the elderly affecting both staff and residents. The symptoms were unusually mild with only two cases developing bloody diarrhoea, of which one proceeded to develop HUS. There were no deaths. The identification of a single strain of E. coli O157 in stool specimens is highly suggestive of an E. coli O157 outbreak, as was the lack of any identified infection in the local community. It was not possible to determine how the infection was introduced into the home, although raw beef and lamb were used in the kitchen and inspection did reveal the potential for cross contamination to other foods that would not be cooked [35]. The prolonged nature of the outbreak and observed lapses in infection control would support person-to-person transmission [18, 19, 21, 24, 34]. Transmission of the infection by asymptomatic individuals is possible; previous reports have described evidence of E. coli O157 in stool specimens of asymptomatic patients [19]. The most unusual feature of this outbreak is the relatively small number of cases with severe complications in contrast to those observed in published outbreaks involving elderly people where case fatalities ranged from 3 to 36% [3, 21–24]. The reason for this is not clear.
The number of cases identified by serological testing is probably due to the transient nature of excretion of the organism. The yield from serum and saliva antibody testing was similar to that described in earlier reports [32, 33]. The value of saliva testing in the investigation of outbreaks remains uncertain.
The OCT employed the measures recommended by the then, PHLS, guidelines to prevent person-to-person spread of the disease. These included adequate hand washing, avoiding shared towels, written regimens for frequent cleaning of toilets, changing rooms and dealing with environmental contamination due to accidents. Care staff with diarrhoea were excluded from work until they were asymptomatic and had two consecutive negative faecal specimens taken after recovery and at least 48 h apart [36].
The home administration was advised to avoid movement of staff between units and their rotation from dirty to clean jobs. Agency staff was discouraged from working in other health or social care establishments. Training in infection control was provided to all staff in the care home. The home was closed for new admissions and social events were cancelled. One week after the implementation of control measures there were no confirmed cases. However, it is not possible to ascertain whether this was due to the intervention of the OCT or the natural course of the outbreak.
The Consultant in Communicable Disease Control and the OCT had limited power over the administration of the home in expediting environmental cleaning and essential training of all staff in principles of infection control. A complicating factor was that the exclusion of symptomatic staff critically reduced staff numbers and the home administration was slow to mobilize staff from other sites to make up for the shortfalls. There was anecdotal evidence that staff were reluctant to report the symptoms for the risk of losing wages due to sickness absence. This home was inspected by the nursing home inspectorate in the week preceding the outbreak [37]. The inspection failed to identify any of the lapses in infection control practices that were later recognized through the infection control audits employed during the investigation of the outbreak. A summary of the recommendations made to the Health Authority and the Care Standards Commission are shown in the Appendix.
APPENDIX
Recommendations for the management of the Care Home and Care Home Standards Commission (responsible for monitoring standards in Care Homes)
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Riley LW et al. Hemorrhagic colitis associated with a rare Escherichia coli serotype. New England Journal of Medicine. 1983;308:681–685. doi: 10.1056/NEJM198303243081203. [DOI] [PubMed] [Google Scholar]
- 2.Guerrant RL, Bobak DA, Mandell GL, Bennett JE, Dolin R. Mandell, Douglas and Bennett's Principles and Practice of Infectious Diseases. 5th ed. Philedelphia: Churchill Livingstone; 2000. Nausea, vomiting and non-inflammatory diarrhoea; pp. 965–978. , pp. [Google Scholar]
- 3.Cowden JM et al. Epidemiological investigation of the Central Scotland outbreak of Escherichia coli O157 infection, November to December 1996. Epidemiology and Infection. 126:335–341. doi: 10.1017/s0950268801005520. 2001; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tilden J et al. A new route of transmission for Escherichia coli infection from dry fermented salami. American Journal of Public Health. 1996;86:1142–1145. doi: 10.2105/ajph.86.8_pt_1.1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Michino H et al. Massive outbreak of Escherichia coli O157:H7 infection in school children in Sakai city, Japan, associated with consumption of white radish sprouts. American Journal of Epidemiology. 1999;150:787–796. doi: 10.1093/oxfordjournals.aje.a010082. [DOI] [PubMed] [Google Scholar]
- 6.CDC. Outbreaks of Escherichia coli O157-H7 infection Morbidity and Mortality Weekly Report. 1997;46:4–8. . Association with drinking unpasteurized apple cider – Connecticut and New York, October 1996. [PubMed] [Google Scholar]
- 7.CDC . Outbreaks of Escherichia coli O157:H7 infection. Association with eating alfalfa sprouts – Michigan and Virginia, June–Jul 1997 Morbidity and Mortality Weekly Report 199746741–744. [Google Scholar]
- 8.Upton P, Coia JE. Outbreak of Escherichia coli O157:H7 infection associated with pasteurised milk supply. Lancet. 1994;344:1015. doi: 10.1016/s0140-6736(94)91670-5. [DOI] [PubMed] [Google Scholar]
- 9.Chapman PA et al. A one year study of Escherichia coli O157 in cattle, ship, pigs and poultry. Epidemiology and Infection. 1997;119:245–250. doi: 10.1017/s0950268897007826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Trevena WB et al. Verocytotoxin-producing Escherichia coli O157 associated with companion animals. Veterinary Record. 1996;138:400. [PubMed] [Google Scholar]
- 11.Wallace JS, Cheasty T, Jones K. Isolation of verocytotoxin producing Escherichia coli O157 from wild birds. Journal of Applied Microbiology. 1997;82:399–404. doi: 10.1046/j.1365-2672.1997.00378.x. [DOI] [PubMed] [Google Scholar]
- 12.Chalmers RM et al. Verocytotoxin producing Escherichia coli O157 in a farmer handling horses. Lancet. 1997;349:1816. doi: 10.1016/s0140-6736(05)61697-2. [DOI] [PubMed] [Google Scholar]
- 13.Trevena WB et al. Verocytotoxin producing Escherichia coli O157 infection associated with farms. Lancet. 1996;347:60–61. doi: 10.1016/s0140-6736(96)91593-7. [DOI] [PubMed] [Google Scholar]
- 14.Shukla R et al. Escherichia coli O157 infection associated with a farm visitors centre. Communicable Disease Report Review. 1995;5:86–90. [PubMed] [Google Scholar]
- 15.Parry SM et al. Haemorrhagic colitis in child after a visit to farm visitor centre. Lancet. 1995;346:572. doi: 10.1016/s0140-6736(95)91407-2. [DOI] [PubMed] [Google Scholar]
- 16.Payne CJet al. Vero cytotoxin producing Escherichia coli O157 gastroenteritis in farm visitors, North Wales. Emerging Infectious Diseases 2003; 9526–530. [DOI] [PMC free article] [PubMed]
- 17.Parry SM, Salmon RL. Sporadic STEC O157 infection: secondary household transmission in Wales. Emerging Infectious Diseases. 1998;4:657–661. doi: 10.3201/eid0404.980419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Allaby MAK, Mayon-White RT. Escherichia coli O157 outbreak in a day nursery. Communicable Diseases Report Review. 1995;5:4–6. [PubMed] [Google Scholar]
- 19.Al-Jader L et al. Outbreak of Escherichia coli O157 in a nursery: lessons for prevention. Archives of Diseases in Children. 1999;81:60–63. doi: 10.1136/adc.81.1.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Swerdlow DL, Griffin PM. Duration of faecal shedding of Escherichia coli O157:H7 among children in day care centres. Lancet. 1997;349:745–746. doi: 10.1016/S0140-6736(05)60196-1. [DOI] [PubMed] [Google Scholar]
- 21.Kohli HS et al. A severe outbreak of Escherichia coli O157 in two psychogeriatric wards. Journal of Public Health Medicine. 1994;16:11–15. doi: 10.1093/oxfordjournals.pubmed.a042911. [DOI] [PubMed] [Google Scholar]
- 22.Ryan CA et al. Escherichia coli O157:H7 diarrhoea in a nursing home: clinical, epidemiological, and pathological findings. Journal of Infectious Diseases. 1986;154:631–638. doi: 10.1093/infdis/154.4.631. [DOI] [PubMed] [Google Scholar]
- 23.Laboratory Centre for Disease Control. Hemorrhagic colitis in a home for the aged – Ontario. Canadian Disease Weekly Report. 1983;9:29–32. [Google Scholar]
- 24.Carter AO et al. A severe outbreak of Escherichia coli O157:H7-associated hemorrhagic colitis in a nursing home. New England Journal of Medicine. 1987;317:1496. doi: 10.1056/NEJM198712103172403. [DOI] [PubMed] [Google Scholar]
- 25.Hildebrand JM et al. An outbreak of Escherichia coli O157 infection linked to paddling pools. Communicable Diseases Report Review. 1996;6:33–36. [PubMed] [Google Scholar]
- 26.Jones IG, Roworth M. An outbreak of Escherichia coli O157 and Campylobacteriosis associated with contamination of a drinking water supply. Public Health. 1996;110:277–282. doi: 10.1016/s0033-3506(96)80089-8. [DOI] [PubMed] [Google Scholar]
- 27.Dev VJ, Main M, Gould I. Waterborne outbreak of Escherichia coli O157. Lancet. 1991;337:41. doi: 10.1016/0140-6736(91)93092-n. [DOI] [PubMed] [Google Scholar]
- 28.Brewster DH et al. An outbreak of Escherichia coli O157 associated with a children's paddling pool. Epidemiology and Infection. 1994;112:441–447. doi: 10.1017/s0950268800051141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Public Health Dispatch. Outbreak of Escherichia coli O157:H7 and Campylobacter among attendees of the Washington County Fair – New York 1999. Morbidity and Mortality Weekly Report. 1999;48:803. [PubMed] [Google Scholar]
- 30.Salmon R. Outbreak of verotoxin producing Escherichia coli O157 infections involving forty schools in South Wales, September 2005. www.eurosurveillance.org/ew/2005/051006. Eurosurveillance. 2005;10 doi: 10.2807/esw.10.40.02804-en. : 051006 ( ). Accessed 19 January 2006. [DOI] [PubMed] [Google Scholar]
- 31.Millward S, Barnett J, Thomlinson D. A clinical infection control audit program: evaluation of an audit tool used by infection control nurses to monitor standards and assess effective staff training. Journal of Hospital Infection. 1993;24:219–232. doi: 10.1016/0195-6701(93)90051-z. [DOI] [PubMed] [Google Scholar]
- 32.Cheasty T et al. The use of serodiagnosis in the retrospective investigation of a nursery outbreak associated with Escherichia coli O157:H7. Journal of Clinical Pathology. 1998;51:498–501. doi: 10.1136/jcp.51.7.498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chart H et al. Analysis of saliva for antibodies to the LPS of Escherichia coli O157 in patients with serum antibodies to Escherichia coli O157 LPS. Journal of Medical Microbiology. 2003;52:569–572. doi: 10.1099/jmm.0.05126-0. [DOI] [PubMed] [Google Scholar]
- 34.Spika JS. Haemolytic uraemic syndrome and diarrhoea associated with Escherichia coli O157:H7 in a day care centre. Journal of Paediatrics. 1986;109:287–291. doi: 10.1016/s0022-3476(86)80386-9. [DOI] [PubMed] [Google Scholar]
- 35.Pennington Group . Report on the circumstances leading to the 1996 outbreak of infection with Escherichia coli O157 in Central Scotland. The implications for food safety and the lessons to be learned. Stationery Office, Edinburgh [Google Scholar]
- 36.Sub-Committee of the PHLS Advisory Committee on Gastrointestinal Infections. Guidelines for the control of infection with Vero cytotoxin producing Escherichia coli (VTEC) Communicable Disease and Public Health. 2000;3:14–23. [PubMed] [Google Scholar]
- 37.Department of Health http://www.doh.gov.uk/ http://www.doh.gov.uk/ . Care homes for older people: national minimum standards. The Stationery Office ( ). Accessed 19 January 2006.