SUMMARY
A resurgence of Mycobacterium bovis infections in cattle in the United Kingdom since the 1980s has raised concern about risks to human health. Enhanced surveillance data for England, Wales and Northern Ireland between 1993 and 2003 of culture-positive human M. bovis cases identified 315 M. bovis infections; the mean annual number of cases was 28 (range 12–41). The most frequently reported exposures were consumption of unpasteurized dairy products 41/83 (49%) and exposure to cattle 45/123 (37%). Of all cases, 249 (83%) were born before 1960. Of 50 cases born after 1960, only 14 were born in the United Kingdom. Over the same time period the annual number of new herd infections increased from 332 to 1749 as derived from the UK State Veterinary Service database. In conclusion, despite a more than fivefold increase in cattle herd infections during the 1990s, there was no increase in reported human cases.
INTRODUCTION
Mycobacterium bovis is a zoonotic bacterium that can infect a wide host range, primarily cattle, but also wildlife (badgers, deer, foxes and ferrets), and humans [1]. It can cause disease in both animals and humans, which may become infectious to others. The main mode of transmission to humans is believed to be from cattle by consumption of unpasteurized dairy products [2]. Close contact with infectious cattle [3–5] or wildlife, and human-to-human transmission may also play a role [1].
Public health measures to prevent M. bovis transmission from animals to humans include pasteurization of milk, testing both dairy and beef cattle herds at regular intervals and meat inspection in the slaughterhouses [1]. These measures have been fully in place in the United Kingdom since 1960 and although pasteurization is only compulsory in Scotland, only 1·7% of dairy farms in England and Wales were registered to produce unpasteurized milk in 2002 [6]. Furthermore, if any officially tuberculosis-free herd is found to be infected with M. bovis, the milk from the herd is compulsorily heat-treated [7]. Pasteurization, including heat treatment of milk from infected herds, is regulated by the Dairy Product (Hygiene) Regulations (1995) [6]. Testing and culling of animals for M. bovis in the United Kingdom is a statutory requirement under European Union legislation [8, 9] and is determined by local incidence at intervals of 1–4 years [8]. Cattle are normally tested for M. bovis using the Single Intradermal Cervical Comparative Test (SICCT), including two injections with bovine and avian (control) tuberculin. A scientific advisory group on bovine tuberculosis has made recommendations to reduce bovine tuberculosis in the United Kingdom [10].
M. bovis epidemiology in cattle in the United Kingdom has substantially changed over the last century. Due to a stringent eradication programme, the level of herd infections declined from 40% in the 1930s to 0·2% by the 1980s [11], although there has been a resurgence of M. bovis in cattle since the 1980s, particularly in South West England and Wales [12, 13]. Human infections are, however, rare in England, Wales and Northern Ireland, and only 1% of microbiologically confirmed tuberculosis cases are attributed to M. bovis [14–16]. Molecular typing methods have nonetheless revealed that there is an association between animal infection and human disease [17–19].
Culture-positive human cases of M. bovis have been reported through Mycobnet (UK Mycobacterial Resistance Network) since 1993 from the whole of the United Kingdom. Enhanced surveillance for human M. bovis infections was initiated in 1998 for England, Wales and Northern Ireland with the aim of collecting information on risk factors for M. bovis infection in humans [14, 15]. Monthly data on M. bovis in cattle have been collected since 1986 through the UK State Veterinary Service VetNet electronic database, which was established for managing incidents of notifiable animal disease and facilitating epidemiological analysis.
The aim of this study was to assess the impact of trends in cattle infections in the United Kingdom on human health in England, Wales and Northern Ireland between 1993 and 2003, and to describe the disease characteristics and risk factors for human cases of M. bovis.
MATERIAL AND METHODS
Surveillance of human cases
A case was defined as a culture-positive M. bovis case reported through Mycobnet (UK Mycobacterial Resistance Network) since 1993 or through enhanced surveillance of M. bovis since 1998 [14, 15]. Matched data on sex, ethnicity, date of birth and the country of origin were obtained from Mycobnet and enhanced surveillance. Data on specimen date, disease type, smear positivity and resistance pattern were obtained from Mycobnet. Potential exposures such as contact with a human tuberculosis case, cattle and wild animal contacts, occupational hazards and consumption of unpasteurized dairy products were identified from the enhanced questionnaires. ONS (Office for National Statistics) census population data from 2001 were used for calculating rates. As cases born outside the United Kingdom might have had different exposures and public health measures were in place in the United Kingdom by 1960, cases born in the United Kingdom after 1960 were of most interest. UK-born cases pre- and post-1960 were described separately. The data were analysed using Microsoft® Excel 2000 (Microsoft, Washington, USA).
Animal surveillance
The number of M. bovis cattle herds testing positive for M. bovis were obtained by the Veterinary Laboratory Agency (VLA) from the tuberculosis section of the UK State Veterinary Service VetNet electronic database. The data used here included number and location of infected cattle herds, number of new and confirmed herd incidents of bovine tuberculosis (defined as any breakdown of control where one or more slaughtered animal shows typical gross lesions of bovine tuberculosis or from which M. bovis can be cultured) and costs of the bovine tuberculosis control programme in the United Kingdom.
RESULTS
Description of human cases between 1993 and 2003
Total cases
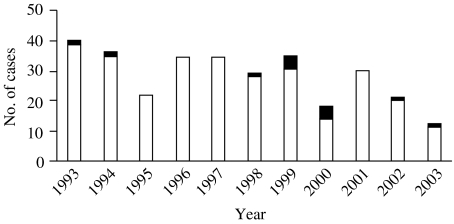
A total of 315 M. bovis cases in humans were identified in England, Wales and Northern Ireland between 1993 and 2003. Matched data were obtained for 170 (54%) cases from both Mycobnet and enhanced questionnaires, and unmatched data for 137 (43%) cases from Mycobnet only and for eight (3%) cases from enhanced questionnaires only. The average number of cases per year was 28 (range 12–41) (Fig. 1). In total 272 cases were reported from England, 21 from Wales and 22 from Northern Ireland. Overall 5·8 cases occurred per million inhabitants in England, Wales and Northern Ireland over this 11-year period. The highest numbers of cases were reported from London (55 cases), the South West (39 cases) and the East Midlands (38 cases).
Fig. 1.
Human M. bovis infections in England, Wales and Northern Ireland between 1993 and 2003. ■, Born in the United Kingdom after 1960; □, Others.
The completeness of reporting patient, disease and exposure characteristics varied as shown in the Table. Of all cases, 166 (54%) were male and 249 (83%) were born before 1960. In total, 127 cases were born in the United Kingdom (81%), but only 14 of them after 1960. A total of 197 (63%) cases occurred in the white ethnic group. Respiratory infection was diagnosed in 120 (49%) of the cases and 60 (45%) were sputum smear-positive on microscopic examination. Of 291 M. bovis isolates, 252 (86%) were sensitive to isoniazid, 289 (99%) to rifampicin and all were sensitive to ethambutol.
Table.
The patient, disease and exposure characteristics of human M. bovis cases between 1993 and 2003

Where information was available, 41 (49%) of the cases reported consumption of unpasteurized dairy products and 30 (46%) had occupational contact with cattle. Contact with a farm was reported for 39 (38%) cases and 24 (22%) had contact with a human tuberculosis case. When combining any cattle contact (living, working or staying in a farm or occupational contact), 45 (37%) of the cases had such exposure history. Of the 40 cases that had consumed unpasteurized dairy products, 25 (63%) had also some form of contact with cattle.
Cases born in the United Kingdom pre- and post-1960 compared
Where information was available, among 110 cases born in the United Kingdom before 1960, 22 (56%) reported consumption of unpasteurized dairy products, 23 (43%) some form of contact with cattle, and 11 (22%) had contact with a human tuberculosis case. Forty (48%) had non-respiratory infection. Among the 14 cases born in the United Kingdom after 1960, two of eight had consumed unpasteurized dairy products, five of eight had some form of contact with cattle and two of nine had contact with a human tuberculosis case. Respiratory infection was reported in 10 of 11 cases.
Animal data
There were 332, 1137 and 1749 new confirmed herd incidents in 1993, 2000 and 2003, respectively, representing an increase of 19% per annum. Most of the new herd incidents occurred in South West and Wales (Fig. 2). The proportion of herds that test positive for M. bovis in South West England increased from 3% (1993) to 10% (2003); elsewhere in England and Wales the proportion of herds with one or more reactors was no more than 3% in 2003. The main direct financial costs of bovine tuberculosis result from routine testing and retesting of herds for infection, compensation for culled animals and contact tracing. The losses from disease through poor performance or through meat condemned at meat inspection are relatively small. The costs from testing, culling, slaughter and compensation have increased from £21 million (1996–2000) to £74 million (2003–2004).
Fig. 2.
Incidence of confirmed bovine tuberculosis by skin test reactors and slaughterhouse findings in England and Wales in (a) 1993 and (b) 2003.
 , Present, but in <1% of animals;
, Present, but in <1% of animals;  , in 1–10% of animals; ■, >10% of animals.
, in 1–10% of animals; ■, >10% of animals.
DISCUSSION
There was a substantial increase in the number of new confirmed M. bovis herd incidents in the United Kingdom between 1993 and 2003. The test protocol for M. bovis in cattle remained unchanged during this period so this is likely to reflect a true increase. By contrast the overall number of cases of human M. bovis disease in England, Wales and Northern Ireland remained low and stable during the same period, comparable to that between 1975 and 1990 [20]. There may be some under-ascertainment of human M. bovis disease as a result of difficulties in obtaining samples or speciation of cultures. This under-ascertainment is, however, likely to have remained the same over the study period so the findings presented here probably reflect actual trends. The increase seen in animal infection has, therefore, not been associated with any increase in human disease.
Most of the UK-born cases in the present and previous studies [20–22] were among older people and were likely to represent late onset disease secondary to latent infections acquired in the era predating control measures in this country. Interestingly, recent surveillance data from central Europe demonstrated no human M. bovis cases aged <30 years [23]. Most of the disease seen in people born after 1960 was in those born abroad in whom exposure in their country of birth cannot be ruled out.
The most frequently reported exposures in people with M. bovis disease in this study included regular consumption of raw dairy products and frequent contact with cattle, particularly among those born before 1960. Pasteurization of milk is undoubtedly an important public health measure for the prevention, not only of M. bovis, but also for other zoonotic infections.
M. bovis infection has been recognized as a potential occupational risk for farm and abattoir workers [3], and guidance on management of the public health consequences of tuberculosis in cattle has been given by the Department of Health [24]. Those working with cattle, or living on farms may also however be more likely to consume unpasteurized dairy products, so there may be some confounding between these two risk factors and it is difficult to ascertain the exact mode of transmission. As observed in other studies [25], half of the total cases in this study had respiratory disease, but there was a difference observed between those born in the United Kingdom before and after 1960. The proportion of cases with respiratory disease was greater in those born after the widespread implementation of pasteurization, and this different distribution may reflect a change in predominant mode of transmission (e.g. from ingestion to inhalation).
The findings from this study imply that the combination of measures taken in the United Kingdom to prevent M. bovis disease in humans as a result of transmission of infection from cattle have been highly effective. The relative importance to public health and the cost effectiveness of each of the control measures used does, however, warrant further studies. This descriptive study has suggests that exposure to cattle or unpasteurized milk may be the most significant risk factors for human M. bovis disease, therefore, protecting those working with cattle and ensuring the microbiological safety of dairy products may be the most important public health measures. To improve understanding it is, however, important to further strengthen surveillance of human cases of M. bovis disease born in the United Kingdom after 1960 and a case-control study of these cases would be needed to adequately estimate the significance of these exposures as risks for disease.
ACKNOWLEDGEMENTS
We thank Pam Sonnenberg for reviewing the manuscript and Charlotte Anderson for technical assistance with the enhanced human M. bovis database.
DECLARATION OF INTEREST
None.
REFERENCES
- 1.O'Reilly LM, Daborn CJ. The epidemiology of Mycobacterium bovis infections in animals and man: a review. Tuberculosis and Lung Disease. 1995;76:1–46. doi: 10.1016/0962-8479(95)90591-x. (Suppl 1): [DOI] [PubMed] [Google Scholar]
- 2.Moda G et al. The zoonotic importance of Mycobacterium bovis. Tuberculosis and Lung Disease. 1996;77:103–108. doi: 10.1016/s0962-8479(96)90022-2. [DOI] [PubMed] [Google Scholar]
- 3.Ritacco V, de Kantor IN. Zoonotic tuberculosis in Latin America. Journal of Clinical Microbiology. 1992;30:3299–3300. doi: 10.1128/jcm.30.12.3299-3300.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Collins C et al. Is bovine, atypical or resistant tuberculosis a problem? Irish Medical Journal. 1987;80:66–67. [PubMed] [Google Scholar]
- 5.Collins CH, Crange JM. Zoonotic implications of Mycobacterium bovis infection. Irish Veterinary Journal. 1987;41:363–366. [Google Scholar]
- http://www.food.gov.uk/foodindustry/Consultations/completed_consultations/completconsultwales/rawmilkcream. http://www.food.gov.uk/multimedia/pdfs/rm.annB.pdf. 2002. http://www.food.gov.uk/foodindustry/Consultations/completed_consultations/completconsultwales/rawmilkcreamhttp://www.food.gov.uk/multimedia/pdfs/rm.annB.pdf Anon. Sale of unpasteurised drinking milk and cream. Food Standards Agency. ( . Annexe B. Accessed 10 October 2005.
- http://www.defra.gov.uk/animalh/diseases/notifiable/disease/tb.htm. 2005. http://www.defra.gov.uk/animalh/diseases/notifiable/disease/tb.htm Anon. Disease factsheet: Bovine tuberculosis. ( . Accessed 10 October 2005.
- 8.Temple M, Tuer SM 2000. http://www.defra.gov.uk/animals/tb/forum/papers/tbf34.pdf http://www.defra.gov.uk/animals/tb/forum/papers/tbf34.pdf . The cost at farm level of consequential losses from tuberculosis control measures,
- 2003. Anon. Directive of the European Parliament and the Council [2003/99/EY],
- 10.Krebs JR London: 1997. . Bovine tuberculosis in cattle and badgers. Report to the Rt Hon Dr Jack Cunningham, MP. : Ministry of Agriculture, Fisheries and Food, [Google Scholar]
- London: 1991. Anon. Animal Health UK – 1990. The Report of the Chief Veterinary Officer, Ministry of Agriculture, Fisheries and Food, Scottish Agriculture, Environment and Fisheries Department and Welsh Office Agriculture Department. : HMSO, [Google Scholar]
- London: 2000. p. 118. Anon. Animal Health 1999, The Report of the Chief Veterinary Officer, Ministry of Agriculture, Fisheries and Food, Scottish Agriculture, Environment and Fisheries Department and Welsh Office Agriculture Department. : HMSO, , p. [Google Scholar]
- 13.Delahay RJ et al. The status of Mycobacterium bovis infection in UK wild mammals: a review. Veterinary Journal. 2002;164:90–105. doi: 10.1053/tvjl.2001.0667. [DOI] [PubMed] [Google Scholar]
- Enhanced surveillance of Mycobacterium bovis disease in humans in England and Wales from January 2001. Communicable Disease Report. CDR Weekly. 2001;11:2–3. [Google Scholar]
- Enhanced surveillance of Mycobacterium bovis in humans. Communicable Disease Report. CDR Weekly. 1998;8:281, 284. [PubMed] [Google Scholar]
- 16.Gibson AL et al. Molecular epidemiology of disease due to Mycobacterium bovis in humans in the United Kingdom. Journal of Clinical Microbiology. 2004;42:431–434. doi: 10.1128/JCM.42.1.431-434.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cousins D et al. Evaluation of four DNA typing techniques in epidemiological investigations of bovine tuberculosis. Journal of Clinical Microbiology. 1998;36:168–178. doi: 10.1128/jcm.36.1.168-178.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yang ZH et al. Spoligotyping and polymorphic GC-rich repetitive sequence fingerprinting of mycobacterium tuberculosis strains having few copies of IS6110. Journal of Clinical Microbiology. 2000;38:3572–3576. doi: 10.1128/jcm.38.10.3572-3576.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zumarraga MJ et al. Usefulness of spoligotyping in molecular epidemiology of Mycobacterium bovis-related infections in South America. Journal of Clinical Microbiology. 1999;37:296–303. doi: 10.1128/jcm.37.2.296-303.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hardie RM, Watson JM. Mycobacterium bovis in England and Wales: past, present and future. Epidemiology and Infection. 1992;109:23–33. [PMC free article] [PubMed] [Google Scholar]
- 21.Lesslie IW, Magnus K, Stewart CJ. The prevalence of bovine type tuberculous infection in man in the English rural population. Tubercle. 1972;53:198–204. doi: 10.1016/0041-3879(72)90016-5. [DOI] [PubMed] [Google Scholar]
- 22.Grange JM, Yates MD. Zoonotic aspects of Mycobacterium bovis infection. Veterinary Microbiology. 1994;40:137–151. doi: 10.1016/0378-1135(94)90052-3. [DOI] [PubMed] [Google Scholar]
- 23.Pavlik Iet al. Occurence of bovine tuberculosis in animal and human populations in seven Central European countries during 1990–1999 and potential sources of infection. Third International Conference on Mycobacterium bovis , 14 August 2000
- 2000. Anon. Guidance on management of the public health consequences of tuberculosis in cattle in England and Wales. Department of Health and the National Assembly for Wales,
- 25.Cousins DV, Dawson DJ. Tuberculosis due to Mycobacterium bovis in the Australian population: cases recorded during 1970–1994. International Journal of Tuberculosis and Lung Disease. 1999;3:715–721. [PubMed] [Google Scholar]