SUMMARY
In August–September 2004, a cryptosporidiosis outbreak affected >250 persons who visited a California waterpark. Employees and patrons of the waterpark were affected, and three employees and 16 patrons admitted to going into recreational water while ill with diarrhoea. The median illness onset date for waterpark employees was 8 days earlier than that for patrons. A case-control study determined that getting water in one’s mouth on the waterpark’s waterslides was associated with illness (adjusted odds ratio 7·4, 95% confidence interval 1·7–32·2). Laboratory studies identified Cryptosporidium oocysts in sand and backwash from the waterslides’ filter, and environmental investigations uncovered inadequate water-quality record keeping and a design flaw in one of the filtration systems. Occurring more than a decade after the first reported outbreaks of cryptosporidiosis in swimming pools, this outbreak demonstrates that messages about healthy swimming practices have not been adopted by pool operators and the public.
INTRODUCTION
During the past two decades, the number of gastrointestinal illness outbreaks associated with disinfected recreational water venues has increased [1–3]. The majority of these outbreaks were caused by Cryptosporidium contamination and are not easily preventable because of the parasite’s chlorine resistance, low infectious dose, and high infectious load. Moreover, although cryptosporidiosis is reportable in all 50 states in the United States, outbreaks are difficult to detect because the illness has a long incubation period (averaging 7 days); persons ill with diarrhoea rarely seek medical care; health-care providers rarely test for Cryptosporidium; and surveillance systems are neither sensitive nor timely [4–6]. Thus, outbreaks of cryptosporidiosis at recreational water venues frequently extend for multiple incubation periods or even months before they are recognized and controlled [4, 7–13]. Maintaining optimal conditions for preventing and detecting these outbreaks requires a multifaceted approach, with efforts coordinated among public health departments, pool operators, and the community.
On 30 August 2004, a concerned parent called a California county (County A) public health department (PHD) to report that her daughter and 11 of her daughter’s friends were ill with diarrhoea after attending an after-hours party held at a County A waterpark (Waterpark A). The following day, the health department received phone calls from two local physicians who reported diarrhoeal illness among patients who had attended Waterpark A, and on 1 September, the PHD received the first four laboratory reports of Cryptosporidium from stool samples of persons whose common exposure was Waterpark A. In the year before September 2004, only 10 cases of cryptosporidiosis had been reported in County A [14]. The following description of this outbreak of cryptosporidiosis underscores the need for improved prevention efforts.
SETTING
Waterpark A is a privately leased concession within a county park, and, according to the waterpark operator, was built in 1978 without permits or plans. Its water is supplied by three wells that supply the rest of the county park, including a lakeside marina store and restaurant. Waterpark A contains a snack bar selling mainly prepackaged foods, a water fountain, two restrooms, and three types of water attractions, (1) two waterslides (side-by-side slides with joined landing pools) on a single filtration/chlorination system; (2) two children’s wading pools (shallow pools joined by small slides) on another filtration/chlorination system; and (3) four whirlpool hot tubs, each on its own filtration/chlorination system. Although the operator could not provide the investigators with exact figures, he stated that >17 000 people visited the waterpark in August 2004.
METHODS
Case-finding
The investigative team made site visits to Waterpark A and interviewed the waterpark operator, manager, and personnel. County A PHD issued press releases and faxes describing an apparent outbreak of cryptosporidiosis associated with Waterpark A and asked persons who had experienced illness to contact the PHD. A hotline was set up to take calls related to the outbreak, and a questionnaire covering demographics, illness characteristics, and locations of recent swimming was administered to each ill caller.
Case-control study
A case-control study was performed to determine the specific risks for illness within the waterpark. For the case-control study, a confirmed case was defined as laboratory-confirmed cryptosporidiosis in a person who visited Waterpark A in August. A clinical case was defined as ⩾7 days of diarrhoea (⩾3 loose stools during a 24-h period), without laboratory confirmation of cryptosporidiosis, occurring in a person during 1–14 days after an August visit to Waterpark A. Excluded as cases were Waterpark A employees and persons who reported contact during the 1–14 days before their symptom onset with anyone with diarrhoea.
Control subjects were selected from visitors to Waterpark A in August who remained well after their visit. Control subject names and contact information were obtained from ill callers to the hotline who were asked to identify well persons with whom they had visited the waterpark. Control subjects were also recruited through outreach at three County A public schools, where flyers were sent home with students asking parents to call the investigative team if they or their children had remained well after visiting Waterpark A in August. We excluded well waterpark employees from the control group.
Trained interviewers administered standardized questionnaires to case-patients and control subjects. Demographic data, as well as data on exposures to waterpark food, drinking water, and recreational water, were collected. At the end of the interview, interviewees were offered the opportunity to provide comments about the waterpark.
For the analysis of the case-control study data, we used SAS version 9.1 (SAS Institute Inc., Cary, NC, USA) [15] to perform univariate analysis on all variables, and to perform multivariate analysis on variables that were identified as being significantly (P⩽0·05) associated with illness in the univariate analysis.
Laboratory investigation
All persons who reported illness were asked to submit stool samples to the health department for testing. County A Public Health Laboratories performed direct immunofluorescent assay (Merifluor® Cryptosporidium/Giardia, Meridian Biosciences, Cincinnati, OH, USA) on stool samples to detect Cryptosporidium and Giardia. Multiple samples that were determined positive for Cryptosporidium were sent to the Centers for Disease Control and Prevention’s (CDC’s) Division of Parasitic Diseases (DPD) Laboratory where polymerase chain reaction (PCR) was performed to identify the species and genotype of the Cryptosporidium isolates [16, 17].
Waterpark A water and filter sand samples were collected on 2 September 2004, a day after the waterpark superchlorinated all aquatic attractions on its own. The waterpark superchlorinated the entire park at >9600 CT, the contact time (product of chlorine in parts-per-million multipled by time in minutes) sufficient to eliminate Cryptosporidium from water. County A PHD collected water samples in fourteen 5-gallon containers from the waterpark’s children’s wading pools, waterslides, and whirlpool hot tubs. The PHD activated the backwash cycles for the children’s wading pools and the waterslides and collected 10 l of water from the discharge pipes of each of these attractions. The PHD collected the top two inches of filter sand from the filters of the wading pools and waterslides and sent these samples, along with water and backwash samples to CDC’s DPD Laboratory. At the DPD Laboratory, sand filter samples were suspended in an eluting solution [Teal buffer: 0·01 m Tris (pH 7·4), 0·01 m EDTA, 0·0125% anti-foam A, 0·1% Laureth-12] and agitated (200 rpm orbital shaker) for 5 min. After gravity settling for 30 s, the eluate/supernatant was carefully decanted. The eluting step was repeated and the eluate/supernatants pooled and filtered through sterile nylon mesh (70 μm porosity). Sand filter eluates, filter backwash samples and water samples were concentrated by centrifugation at 3200 g for 10 min using a swinging bucket rotor and plastic conical centrifuge bottles. Recovered sediment samples were processed for immunofluorescence microscopy and molecular analyses according to the U.S. Environmental Protection Agency (EPA) Method 1623 for detection of Cryptosporidium and Giardia [18].
Also on 2 September, County A’s public works department collected water samples from the county park’s lake and three wells. County A’s public works department water-quality laboratory tested all samples for Cryptosporidium and Giardia using EPA Method 1623 [18], and tested well-water samples additionally for faecal coliforms using the American Water Works Association Standard Method 9223 B, Enzyme Substrate Coliform test [19].
Environmental evaluation
Using a comprehensive collection tool designed by CDC for the environmental evaluation for swimming pools [20], County A’s PHD evaluated water flow, filtration, disinfection, and heating at the waterpark, as well as Waterpark A’s procedures for pool disinfection, water chemistry testing and management, record keeping, and waste disposal.
RESULTS
Case-finding
Waterpark A management and staff stated they were aware of a widespread diarrhoeal illness among Waterpark A personnel and thought the illness was caused by a common restaurant exposure in early August. No policies were in place for excluding ill employees from water contact or for contacting the health department to report an outbreak. Of 26 Waterpark A employees, we were able to contact 23, a total of 19 (83%) of whom reported diarrhoeal illness. These included a manager, a snack-bar worker, a cashier, and lifeguards. Of these 19 employees, 15 (79%) submitted stool samples, and seven (47%) of the 15 samples were identified as positive for Cryptosporidium.
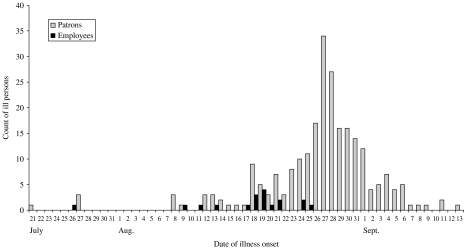
Of the 340 persons who called the health department and reported at least 1 day of diarrhoea, 273 (80%) reported exposure to Waterpark A. Forty-two (63%) of the 67 callers who stated they had not visited the waterpark reported close contact with an ill person who had visited the waterpark before illness onset, leaving 25 (7%) of the original 340 callers without a known connection to the waterpark. No ill persons were reported as being associated with the lakeside marina restaurant outside Waterpark A. The median onset date for ill patrons was 27 August, a total of 8 days after the median onset date (19 August) for ill employees (Fig. 1).
Fig. 1.
Number of ill patrons (n=244a) and waterpark employees (n=19b) by reported date of illness onset, 21 July–13 September 2004. (a Two patrons not represented on the graph gave their onset dates as 8 and 21 June; b one employee not represented on the graph gave an onset date of 4 July.)
The age range of the 273 ill waterpark visitors was 1–69 years (median 14 years). Ten percent were aged <4 years. Fifty-one percent were female. Persons reported duration of diarrhoea that ranged from 1 to 31 days (median 4 days). Eighty-three (30%) persons reported consulting a health-care provider for their illness, and three were hospitalized. Nineteen persons (7%), three of whom were Waterpark A employees, admitted to going into recreational water while ill with diarrhoea.
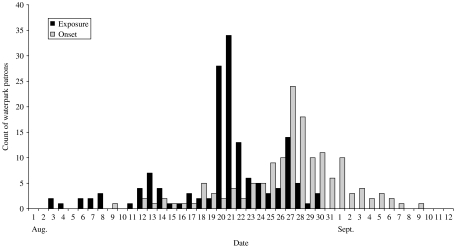
Of the 273 persons reporting illness, 151 (55%) who reported that they visited the waterpark only once during their incubation periods were able to give a date of visit (Fig. 2). The exposure date with the majority of case-patients was Saturday, 21 August, a date 34 ill persons cited as their only exposure to the waterpark. The second highest exposure date was Friday, 20 August, the date of the after-hours party described by the parent who first called the PHD. Twenty-one (75%) of 28 persons who cited 20 August as their only waterpark exposure date were party attendees. The investigative team was able to contact 41 of the 61 persons who were reported to have attended the party; of these, 39 (95%) reported diarrhoea, and 17 submitted stool samples, all of which were positive for Cryptosporidium. The party was attended by at least five waterpark employees. Two partygoers, one of whom was a waterpark lifeguard, dated their illness onsets before the party date (illness onsets of 18 and 19 August).
Fig. 2.
Reported exposure and onset dates by patrons (n=151) who reported visiting Waterpark A only once during the illness incubation period, 2004.
Case-control study
We enrolled the first eligible 34 case-patients and 57 control subjects. Of the 34 case-patients, 26 (76%) had laboratory-confirmed illness. Of the 57 control subjects, 38 (68%) had been identified by ill persons, and 19 (32%) had been identified through community outreach. By non-parametric tests, case-patients were significantly younger than control subjects, with a median age of 14 years for case-patients and 28 years for control subjects.
On univariate analysis, the exposures significantly related to illness were drinking water from the water fountain [25% of case-patients vs. 4% of control subjects; odds ratio (OR) 8·8, 95% confidence interval (CI) 1·7–44·8], and two exposures that were related to the waterslides, having one’s face splashed or dunked while on the waterslides (97% of case-patients vs. 58% of control subjects; OR 24·0, 95% CI 3·1–187·9) and getting water in one’s mouth on the waterslides (88% of case-patients vs. 26% of control subjects; OR 21·0, 95% CI 6·3–69·6) (Table 1).
Table 1.
Univariate analysis of significant Waterpark A exposures among persons who visited Waterpark A in August 2004
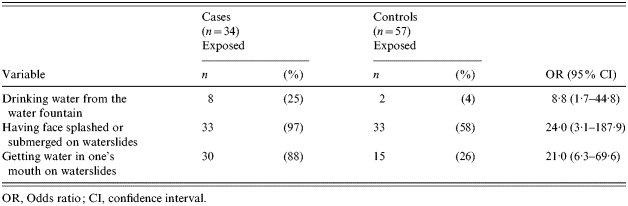
OR, Odds ratio; CI, confidence interval.
On multivariate analysis of the three variables associated with illness in the univariate analysis, and on categorizing the variable of age into four groups (⩽6, 7–14, 15–28 and ⩾29 years), only getting water in one’s mouth on the waterslides remained statistically significant [adjusted odds ratio (aOR) 7·4, 95% CI 1·7–32·2) (Table 2).
Table 2.
Multivariate analysis by age and Waterpark A exposures associated with illness among persons who visited Waterpark A in August 2004
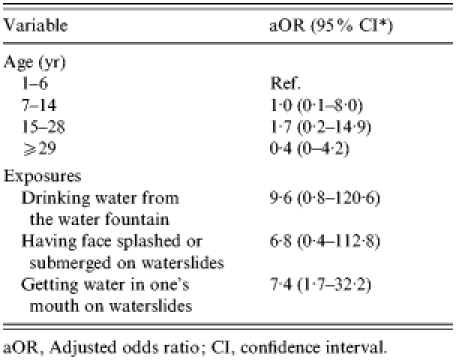
aOR, Adjusted odds ratio; CI, confidence interval.
Seven case-patients and 10 control subjects volunteered complaints about ‘dirty water,’ especially in the children’s wading pools and whirlpool hot tubs. One case-patient and three control subjects complained of dirty restrooms, and one control subject complained of overcrowding.
Laboratory investigation
Ninety-two (34%) of the 273 ill persons submitted stool samples for testing to the PHD laboratory, and 52 (56%) of these 92 persons had specimens identified as positive for Cryptosporidium. No stool samples were positive for Giardia. PCR on Cryptosporidium DNA from six positive stool samples identified the Cryptosporidium as subtype allele family IIc, an anthroponotic (i.e. human-adapted) C. parvum subtype, potentially indicating a human rather than animal source of the parasite.
Three Cryptosporidium oocysts were identified on sand from the waterslides’ filter, and six oocysts/10 l of water were identified in the backwash from the waterslides’ filter. No oocysts were identified in water samples from the children’s wading pools, waterslides, or whirlpool hot tubs, or from the sand or backwash from the wading pool filter. PCR on the oocysts from the filter sand and backwash was attempted but was unsuccessful.
No Cryptosporidium or Giardia was detected in samples collected from the county park lake and three wells. No faecal coliforms were identified in well-water samples.
Environmental evaluation
On evaluation of the waterpark’s equipment and procedures, County A PHD determined that Waterpark A kept sporadic and inconsistent water-chemistry records. Waterpark A did not record any faecal accidents for its 2004 season. On examination of Waterpark A’s filtering systems, County A PHD determined that 30% of the water piped through the wading pools was diverted around the wading pool water filter to be passed through the water heater.
DISCUSSION
In summary, we report an outbreak of diarrhoeal illness affecting >250 persons whose common exposure was a California waterpark. The outbreak persisted throughout August and into early September, peaking on August 27, and first coming to the attention of the PHD on 30 August. Laboratory, clinical, and environmental evidence indicated that the aetiological agent was Cryptosporidium. Case-control analysis and environmental studies support the hypothesis that this outbreak was associated with using the waterpark’s waterslides.
This outbreak is notable for going unreported to the local PHD for weeks, although ∼75% of the waterpark’s 26 employees were known to be ill with diarrhoea. Sixteen employees reported illness onsets before 21 August, and the median onset date for waterpark employees fell into the exposure period for illness for the majority of patrons, considering the median 7-day incubation period for cryptosporidiosis. Interviews with waterpark management indicated that waterpark personnel were aware of the illness among the staff, but ill persons stayed home only when too ill to work. That the majority of the lifeguards were ill before patrons became ill and that certain lifeguards admitted to going into the water while symptomatic demonstrates that contamination of water by ill personnel might have contributed to this outbreak.
Illness among lifeguards has been noted previously in reports of cryptosporidiosis outbreaks associated with recreational water. In the first reported outbreak of swimming pool-associated cryptosporidiosis in the United States, the authors noted that 75% of the lifeguards were ill [13]. Likewise, a swimming pool-associated cryptosporidiosis outbreak in Canada reported that 27% of the lifeguards had been ill [8]. However, neither of these reports included the illness-onset times of lifeguards relative to patrons, nor whether the lifeguards could have contributed to illness among patrons. In 2004, investigation of another Canadian swimming pool-associated cryptosporidiosis outbreak determined that a pool employee had a positive stool test for Cryptosporidium 1 month before the outbreak had been detected, and that this person and other employees had been in the pools during their symptomatic periods [11]. Pool operators and environmental and public health departments need to be particularly sensitive when hearing about diarrhoeal illness among pool staff, because staff, especially lifeguards and swimming instructors, who are regularly in the water as part of their jobs, can serve as sentinels for outbreaks of recreational waterborne cryptosporidiosis. If pool management does not quickly identify illness and exclude pool staff from the water, lifeguards and other pool employees might amplify or prolong the outbreak by going into the water while ill. A clear policy to keep lifeguards and bathers with diarrhoea out of pools and waterparks should be standardized, implemented, and enforced.
Outbreaks of cryptosporidiosis have occurred in aquatic venues even where pools were well-maintained [7, 21], but the outbreak described here as well as other outbreaks [9, 13, 22], occurred in the presence of correctable problems. Site visits, interviews, and environmental studies uncovered problems in procedures, system design, policies, and maintenance at the waterpark. The responsibility for some of these problems clearly falls with the pool operator, but lack of coherent and standardized pool regulations might also have contributed to the conditions that led to the outbreak.
The waterpark operator was in violation of California regulations requiring pool operators to keep daily water-chemistry records and to maintain these records for at least 1 year [23]. The waterpark operator may also have been in violation of California codes requiring cleanliness of the pools, showers, toilets, and dressing facilities, and water clarity of the wading pools. California regulations also specifically state that ‘No person having a communicable disease shall be employed at a public swimming pool’. However these regulations do not give guidance on how to identify communicable diseases, and Waterpark A management may not have recognized that the diarrhoeal illness in their staff was contagious.
In the United States there have been attempts to implement standards for the management of faecal accidents in swimming pools [24]. Although California regulations do not address faecal accidents, as early as 2002, County A PHD issued Waterpark A a protocol requiring maintenance of a faecal-accident log [25]. Nonetheless, Waterpark A recorded no faecal accidents in 2004 although faecal accidents are known to be common events in pools that cater to young children, even occurring on a daily basis at certain venues [1]. Faecal accidents probably occurred during the 2004 season at Waterpark A, which had a census of >500 persons/day in a park that featured wading pools for children wearing diapers, but their detection may have been difficult because cryptosporidiosis causes a watery diarrhoea that may not be apparent especially in a crowded pool. Under these conditions, public awareness about refraining from swimming with diarrhoea and about notifying pool operators as soon as faecal accidents occur is critical.
Although California regulations require that persons who intend to construct or alter swimming pools submit plans to an enforcing agency [23], no current California regulation gives specifications for the design and maintenance of pool filtration systems. Cryptosporidium oocysts are resistant to chlorine at the concentrations commonly used in pool disinfection, therefore pool filtration systems are critical in safeguarding against this parasite. This important safeguard was compromised in Waterpark A’s wading pools, where 30% of the water bypassed the filter in order to be routed through the heater.
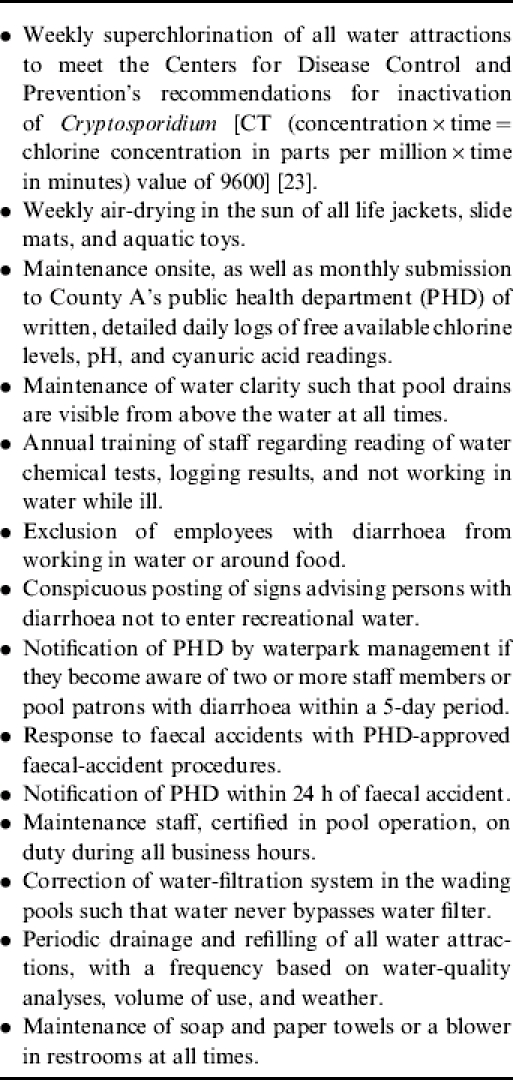
On 1 September 2004, the day County A received the first laboratory reports of Cryptosporidium, Waterpark A closed voluntarily for the 2004 season. For Waterpark A to reopen in 2005, County A required them to meet a set of standards that included weekly superchlorination of all water attractions (see Appendix). Such measures are only a beginning towards prevention of recreational waterborne illness. To ensure the safety of recreational water venues in the United States, a model pool code should be developed for use across all jurisdictions. Moreover, uniform pool standards need to be set for the training and certification of pool operators; pools need to post signs to keep persons with diarrhoea out of the water and to educate the public on safe swimming practices; and environmental and public health officials need to work closely with pool operators to encourage reporting of diarrhoeal clusters and recording of faecal accidents, and to enforce adherence to the pool maintenance standards.
AcknowledgEments
The authors thank the members of the San Luis Obispo Public Health Department, who worked tirelessly on this investigation; California Department of Health Services Sexually Transmitted Disease Control Branch, Disease Intervention Section for help with interviewing study subjects; and Vitaliano Cama, D. V. M., Ph.D. of the CDC Division of Parasitic Diseases Laboratory for assistance in genotyping and subtyping Cryptosporidium oocysts in stool specimens.
APPENDIX
Requirements for reopening Waterpark A in 2005
DECLARATION OF INTEREST
None.
REFERENCES
- Castor ML, Beach MJ. Reducing illness transmission from disinfected recreational water venues: swimming, diarrhea and the emergence of a new public health concern. Pediatric Infectious Disease Journal. 2004;23:866–870. doi: 10.1097/01.inf.0000138081.84891.30. [DOI] [PubMed] [Google Scholar]
- Yoder JS et al. Surveillance for waterborne-disease outbreaks associated with recreational water – United States, 2001–2002. Morbidity and Mortality Weekly Report Surveillance Summaries. 2004;53:1–22. (no. SS-8): [PubMed] [Google Scholar]
- Dillingham RA, Lima AA, Guerant RL. Cryptosporidiosis: epidemiology and impact. Microbes and Infection. 2002;10:1059–1066. doi: 10.1016/s1286-4579(02)01630-1. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Outbreak of cryptosporidiosis associated with a water sprinkler fountain – Minnesota, 1997. Morbidity and Mortality Weekly Report. 1998;47:856–860. [PubMed] [Google Scholar]
- Hellard ME et al. An outbreak of cryptosporidiosis in an urban swimming pool: why are such outbreaks difficult to detect. Australian and New Zealand Journal of Public Health. 2000;24:272–275. doi: 10.1111/j.1467-842x.2000.tb01567.x. [DOI] [PubMed] [Google Scholar]
- MacKenzie WR et al. A massive outbreak in Milwaukee of cryptosporidium infection transmitted through the public water supply. New England Journal of Medicine. 1994;331:161–167. doi: 10.1056/NEJM199407213310304. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Protracted outbreaks of cryptosporidiosis associated with swimming pool use – Ohio and Nebraska, 2000. Morbidity and Mortality Weekly Report. 2001;50:406–410. [PubMed] [Google Scholar]
- Bell A et al. A swimming pool-associated outbreak of cryptosporidiosis in British Columbia. Canadian Journal of Public Health. 1993;84:334–337. [PubMed] [Google Scholar]
- Joce RE et al. An outbreak of cryptosporidiosis associated with a swimming pool. Epidemiology and Infection. 1991;107:497–508. doi: 10.1017/s0950268800049190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim LS et al. Cryptosporidiosis outbreak in a recreational swimming pool in Minnesota. Journal of Environmental Health. 2004;67:16–20, 28, 27. [PubMed] [Google Scholar]
- Louie K et al. An outbreak of Cryptosporidium parvum in a Surrey pool with detection in pool water sampling. Canada Communicable Disease Report. 2004;30:61–66. [PubMed] [Google Scholar]
- McAnulty JM, Fleming DW, Gonzalez AH. A community-wide outbreak of cryptosporidiosis associated with swimming at a wave pool. Journal of the American Medical Association. 1994;272:1597–1600. [PubMed] [Google Scholar]
- Sorvillo FJ et al. Swimming-associated cryptosporidiosis. American Journal of Public Health. 1992;82:742–744. doi: 10.2105/ajph.82.5.742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- California Department of Health Services http://www.dhs.ca.gov/ps/dcdc/html/cdtables.htm. http://www.dhs.ca.gov/ps/dcdc/html/cdtables.htm . Communicable Disease Summaries, September 2003–August 2004 ( ). Accessed 14 February 2006.
- SAS Institute, Inc Cary, North Carolina: 2002. . SAS programming language. [Google Scholar]
- Sulaiman IM et al. Unique endemicity of cryptosporidiosis in children in Kuwait. Journal of Clinical Microbiology. 2005;43:2805–2809. doi: 10.1128/JCM.43.6.2805-2809.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao L et al. Identification of 5 types of Cryptosporidium parasites in children in Lima, Peru. Journal of Infectious Diseases. 2001;183:492–497. doi: 10.1086/318090. [DOI] [PubMed] [Google Scholar]
- US Environmental Protection Agency . Method 1623: Cryptosporidium and Giardia in water by filtration/IMS/FA (http://www.epa.gov/nerlcwww/1623ap01.pdf). Accessed 17 August 2005.
- American Public Health Association, American Water Works Association, Water Environment Federation. Standard Methods for the Examination of Water and Wastewater. 20th edn. American Public Health Association; Washington, DC: 1998. pp. 9–69. , pp. to 9–70. [Google Scholar]
- Centers for Disease Control and Prevention http://www.cdc.gov/healthyswimming/downloads/Pool_Systems_Tool_06-2005.doc. http://www.cdc.gov/healthyswimming/downloads/Pool_Systems_Tool_06-2005.doc . Environmental health systems approach to recreational water illness prevention: Information collection tool for understanding how the aquatic facility works. ( ). Accessed 7 March 2006.
- Hunt DA et al. Cryptosporidiosis associated with a swimming pool complex. Communicable Disease Report. CDR Review. 1994;4:R20–R22. [PubMed] [Google Scholar]
- Wilberschied L. A swimming-pool-associated outbreak of cryptosporidiosis. Kansas Medicine. 1995;96:67–68. [PubMed] [Google Scholar]
- California Office of Administrative Law http://www.calregs.com/ http://www.calregs.com/ . California code of regulations. Title 22, division 4, chapter 20, Public swimming pools ( ). Accessed 17 August 2005.
- Kebabjian RS. Disinfection of public pools and management of fecal accidents. Journal of Environmental Health. 1995;58:8–12. [Google Scholar]
- Centers for Disease Control and Prevention. Responding to fecal accidents in disinfected swimming venues. Morbidity and Mortality Weekly Report. 2001;50:416–417. [PubMed] [Google Scholar]