SUMMARY
This investigation was undertaken to provide detailed information on the epidemiology of human parvovirus B19 (B19) infection during pregnancy and childhood in the western part of Germany. Between 1997 and 2004, 40 517 sera from pregnant women aged 17–45 years and 6060 sera from children and young adults were tested for B19 IgG and IgM in our laboratory. In pregnant women, both the history of a ‘specific’ (OR 7·7, 95% CI 5·2–11·4) and a ‘non-specific’ rash (OR 3·3, 95% CI 1·5–7·1) was predictive for B19 IgM positivity. The B19 IgG prevalence was 69·2% (4097/5924) in a subgroup of asymptomatic pregnant women screened for B19 antibodies. In children, the age-specific IgG-positivity rate increased from 12·2% (66/541) at 2 years of age to 71·9% (396/551) in those older than 10 years. In conclusion, the prevalence of B19 IgG in pregnant women from the western part of Germany is higher then previously reported. Contact with children aged 3–10 years is a major risk factor for exposure to B19. Pregnant women with the history of a ‘non-specific’ rash should also be evaluated for acute B19 infection.
INTRODUCTION
Human parvovirus B19 (B19) infection commonly causes erythema infectiosum, a rash illness of childhood [1] and may be responsible for transient aplastic crises in persons with increased erythrocyte turnover and for prolonged anaemia in immunocompromised subjects. In adults, B19 infection more commonly causes a non-specific febrile illness. Pregnant women with acute B19 infection report symptoms of polyarthralgia in about 30% and a rash in 30–40% of cases. Symptomatic disease is often very short-lived (2–5 days). In total 30–50% of acutely infected pregnant women are entirely asymptomatic [2–6]. In pregnancy, acute B19 infection is an important cause of fetal morbidity (fetal anaemia and hydrops) and mortality predominantly in the second trimester [6–10]. Thus, infection during the first 20 weeks' gestation is associated with a 6–9% excess fetal loss rate [6, 9]. Knowledge about the current epidemiology of parvovirus B19 is essential for the management of, and exposure to, rash illness in pregnant women.
METHODS
Samples
Between 1997 and 2004, a total of 40 517 sera from pregnant women aged 17–45 years and a total of 6060 sera from children and (non-pregnant) adolescents aged 0–18 years have been investigated for the presence of parvovirus B19 IgG and IgM. The majority of sera were collected and sent to our laboratory by private practitioners – namely general practitioners, paediatricians and gynaecologists – residing mainly in the western part of Germany. Since there is only a small fluctuation in private practitioners that cooperate with our laboratory, the geographic area and patient population under investigation were stable. Samples submitted from other laboratories and multiple samples from the same patient have been excluded. In Germany, parvovirus B19 antibody screening in pregnancy is not generally advised, but it is mandatory for pregnant employees at risk of B19 infection (primarily those with daily occupational contact with children aged <7 years, e.g. in the kindergarten or day-care centre). Furthermore, the general awareness of possible B19-related complications in pregnancy has increased during recent years. Therefore, determination of B19 immune status following confirmation of pregnancy is often requested. Because acute B19 infection is frequently asymptomatic, pregnant women are usually screened for both B19 IgG and IgM.
In the present analysis, three subgroups of sera (patients) were further selected from the total population by the availability of data on week of gestation, symptoms and contact history:
-
(i)
subgroup A: sera from asymptomatic pregnant women attending antenatal care during the first trimester (B19 IgG and IgM screening) (n=5924);
-
(ii)
subgroup B: sera from pregnant women investigated for B19 IgG and IgM antibodies because of symptoms (e.g. rash, arthropathy) or contact to a suspected case of erythema infectiosum (n=15 715);
-
(iii)
subgroup C: sera from children and adolescents investigated amongst others for B19 IgG and IgM antibodies because of symptomatic disease (e.g. rash, fever, arthropathy, lymphadenopathy, haematological abnormalities, respiratory tract symptoms) (n=3186).
Antibody test
Parvovirus B19 VP2 (viral capsid 2)-specific IgM was determined by the μ-capture EIA of Biotrin (Biotrin International, Dublin, Ireland) and VP2-specific IgG was determined by an indirect EIA (Biotrin International) as described previously [11]. Patient sera that gave equivocal test results were excluded from the evaluation of subgroups A–C.
Statistical analysis
Statistical tests included the χ2 test with Yates correction and, when appropriate, Fisher's exact test (Epi-Info 2000, CDC, Atlanta, GA, USA) for analysis of categorical data.
RESULTS
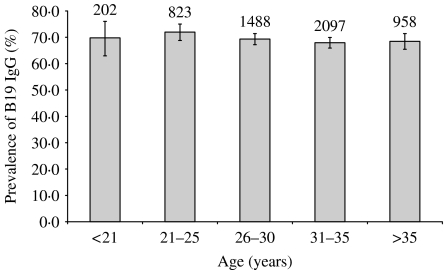
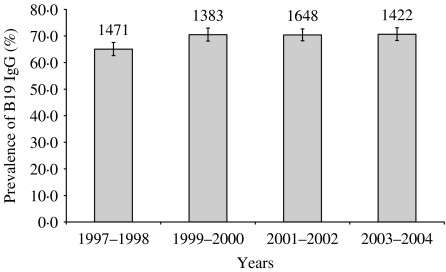
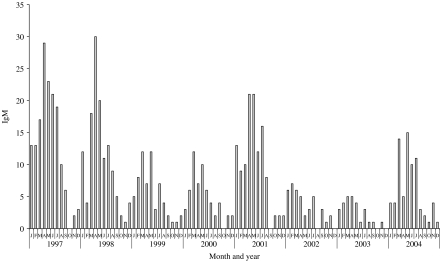
The positivity rates of B19 IgG and IgM in pregnant women aged 17–45 years as well as children and adolescents aged 0–18 years are given in Table 1. Analysis of subgroup A revealed the following results. Forty-three of 5924 specimens (0·7%) tested B19 IgM positive. The B19 IgG prevalence was 69·2% (4097/5924). The prevalence of B19 IgG in the different age groups was very similar (Fig. 1). The B19 IgG prevalence was higher in the years 1999 and 2000 (70·5%, 95% CI 68·0–72·9) compared to 1997 and 1998 (65·1%, 95% CI 62·6–67·5) (P<0·002) (Fig. 2). To demonstrate differences in the seasonal and year-to-year epidemic pattern of B19, test results from patients of subgroup B were analysed. A total of 665 of 15 715 serum specimens (4·2%) was B19 IgM positive. The B19 epidemic curve according to B19 IgM positivity is presented in Figure 3. Each year, about 75% of IgM-positive cases were recorded between January and June. During the study period there was no significant difference in the IgM-positivity rate between the first and the second half of each year (data not shown). Nevertheless, between some years the IgM-positivity rates differed significantly [e.g. 6·3% (156/2480) in 1997 and 2·3% (28/1232) in 2003].
Table 1.
B19 IgG and IgM test results from pregnant women aged 17–45 years and children aged 0–18 years, 1997–2004
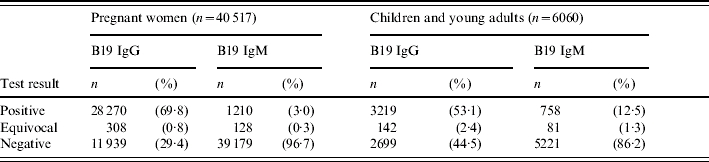
Fig. 1.
Age-specific B19 IgG prevalence in asymptomatic pregnant women (n=5924) screened for B19 antibodies during the first trimester, 1997–2004 (subgroup A). The numbers above the columns represent the total number of sera tested per age group.
Fig. 2.
Crude B19 IgG prevalence in asymptomatic pregnant women (n=5924) screened for B19 antibodies during the first trimester, 1997–2004 (subgroup A). The numbers above the columns represent the total number of sera tested per time period.
Fig. 3.
Epidemic pattern of parvovirus B19 infection in pregnant women as defined by detection of B19 IgM from diagnostic specimens at the Stuttgart laboratory, 1997–2004 (subgroup B).
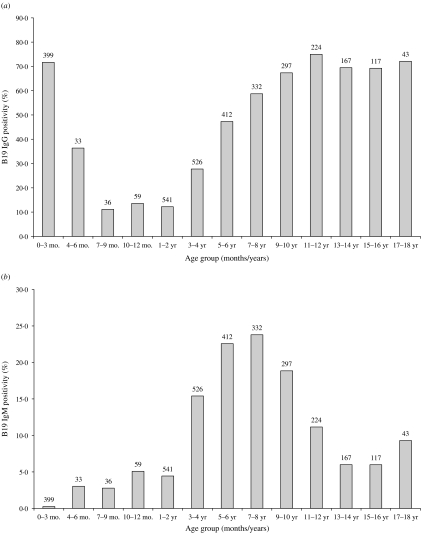
Of the 15 715 pregnant women of subgroup B, 42 were investigated because of the presence of arthropathy and rash as the leading symptom, 108 because of arthropathy, 1797 because of rash and 13 768 because of contact with a suspected case of erythema infectiosum. The proportions of B19 IgM positivity in the latter ‘categories’ were 47·6% (20/42), 12·0% (13/108), 4·7% (84/1797) and 4·0% (548/13 768) respectively. The history of a contact with a case of erythema infectiosum or the presence of symptoms (subgroup B) was significantly associated with a positive B19 IgM finding in the patient when compared to pregnant women screened for B19 antibodies (subgroup A) (Table 2). Interestingly, the history of a non-specific rash was still predictive for B19 IgM positivity. Age-specific B19 IgG- and IgM-positivity rates in children and young adults (n=3186) amongst others investigated for B19 antibodies because of symptomatic disease are given in Figure 4(a, b).
Table 2.
Association between reason for B19 testing and B19 IgM positivity in pregnant women with a history of symptoms or contact
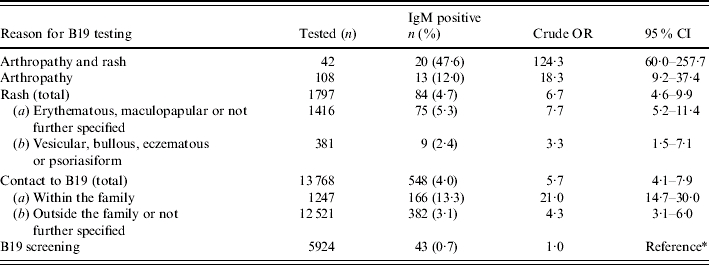
OR, Odds ratio; CI, confidence interval.
Reference refers to the comparison group.
Fig. 4.
B19 IgG-positivity (a) and IgM-positivity (b) rates in children and young adults (n=3186) amongst others investigated for B19 antibodies because of symptomatic disease (subgroup C). The numbers above the columns represent the total number of sera tested per age group.
DISCUSSION
In the present study we observed a higher prevalence of B19 IgG in pregnant women (69·2%) than previously reported from Germany (50–55%) [12, 13]. The findings of our analysis are in line with recently published studies from Denmark, Ireland, The Netherlands, Victoria (Australia) and Montreal (Canada) [14–18] which report a B19 IgG prevalence of about 63·0–70·0% in women of childbearing age. A lower prevalence (35–50%) of parvovirus B19 IgG has been noted in pregnant women from tropical regions [15, 17]. Among the pregnant women screened for B19 antibodies during the first trimester between 1997 and 2004, there was no significant change in B19 IgG prevalence as maternal age increased, indicating that primary B19 infection occurred in most cases prior to childbearing age. Following the epidemic years 1997 and 1998 (Fig. 3), we found an increase in B19 seroprevalence in 1999 and 2000 (Fig. 2). From that time on no significant variation in B19 IgG prevalence occurred.
There are few published reports on the seasonal activity of B19 infection in temperate climates. In accordance with others [19, 20], we observed a seasonal peak in late winter and spring. Each year, about 75% of IgM-positive cases were recorded between January and June. The epidemic cycle of parvovirus B19 appeared to be around 4 years with 1 or 2 epidemic years followed by 2 or 3 years where infection was less frequent. However, since there was some variation in the IgM-positivity rate between years, the significance of our assumptions concerning the relative size of the epidemic in different years may be limited. Nevertheless, the epidemic cycle observed in our study resembled the epidemic cycles reported from England and Wales as well as The Netherlands [19–21].
If a pregnant woman is exposed to a suspected case of erythema infectiosum or presents with signs or symptoms of acute B19 infection, testing for both B19 IgG and IgM is generally recommended [20, 22, 23]. According to our findings antibody testing should not be restricted to patients presenting with a typical rash since the presence of a non-specific rash was also associated with B19 IgM positivity. The presence of both rash and arthropathy was the strongest predictor of a positive B19 IgM result. However, the presence of a rash alone was no more predictive for B19 IgM positivity than the history of exposure to B19. In addition, our data substantiate previous findings that exposure to an index case within the family is significantly more associated with B19 IgM positivity than exposure to an index case outside the family.
Analysis of B19 antibody test results of neonates and infants showed a B19 IgG-positivity rate of 71·7% in the early postnatal period (0–3 months) which dropped to about 13·6% at age 1 year. The B19 IgM-positivity rate in the early postnatal period was <1·0%. Therefore, B19 IgG antibodies detected during the early postnatal period represent in most cases passively acquired maternal antibodies. The age-specific IgG-positivity rate increased from around 12·2% (66/541) at 2 years of age to 71·9% (396/551) in those older than 10 years. Cohen & Buckley [24] and Eis-Hübinger et al. [25] reported similar findings. The B19 IgM-positivity rate was highest in symptomatic children aged 3–10 years (Fig. 4 b). Our observations overestimate the age-specific IgG-positivity rates to some extent since all children were tested because of symptomatic disease. Nevertheless they correspond very well with previous publications that report the highest B19 attack rate in the 5–9 years age group [26], and the finding that having children aged 6–7 years is a major risk factor for B19 seroconversion in non-immune pregnant women [27].
In Germany, there is an ongoing debate on the right to preventive reassignment and routine exclusion of seronegative pregnant employees from the workplace where B19 infection is present, and respective recommendations differ between federal states. If reassignment to other duties is not possible, withdrawal from work is mandatory. This may be limited to the duration of a B19 outbreak or can last until the start of regular maternity leave (usually 6 weeks before delivery). According to German legislation, general health insurance is currently obliged to continue the wage payment during preventive exclusion from work. The recommendations in Germany differ largely from those in the United Kingdom or the United States, where exclusion of B19-susceptible pregnant women from the workplace, which may suggest a higher rate of exposure, is not mandatory [22, 28]. Primarily, this is because the risk of infection in the workplace may be similar to or less than that in the community or at home.
The economic burden of such recommendations depends largely on the seronegativity rate of women of childbearing age. In a recent publication, Gilbert and co-workers [18] report a high rate of B19-susceptible women working in day-care centres in Montreal (Canada) that reached 50% in those aged <25 years. In contrast, we observed a B19 IgG prevalence of 71·5% (733/1025) in pregnant women aged <26 years and a B19 IgG-positivity rate of 70% (112/160) in non-pregnant adolescents aged 15–18 years. However, our data do not refer to occupational risk groups. Thus, further studies are needed (e.g. in Germany) to better define the age-specific rate of B19-susceptible women of reproductive age in occupational groups at high risk for acquiring B19 infection.
ACKNOWLEDGEMENTS
We gratefully acknowledge the excellent cooperation of all gynaecologists, general practitioners and paediatricians. We also thank Carola Baisch and Sabine Helbig for excellent technical assistance as well as Frank Knotek for database management and Karen Searle for her editorial assistance in the preparation of the manuscript.
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Anderson MJ et al. Human parvovirus, the cause of erythema infectiosum (fifth disease)? Lancet. 1983;1:1378. doi: 10.1016/s0140-6736(83)92152-9. [DOI] [PubMed] [Google Scholar]
- 2.Gillespie SM et al. Occupational risk of human parvovirus B19 infection for school and day-care personnel during an outbreak of erythema infectiosum. Journal of the American Medical Association. 1990;263:2061–2065. [PubMed] [Google Scholar]
- 3.Gratacós E et al. The incidence of human parvovirus B19 infection during pregnancy and its impact on perinatal outcome. Journal of Infectious Diseases. 1995;171:1360–1363. doi: 10.1093/infdis/171.5.1360. [DOI] [PubMed] [Google Scholar]
- 4.Harger JH et al. Prospective evaluation of 618 pregnant women exposed to parvovirus B19: risks and symptoms. Obstetrics and Gynecology. 1998;91:413–420. doi: 10.1016/s0029-7844(97)00701-1. [DOI] [PubMed] [Google Scholar]
- 5.Maksheed M et al. The prevalence of antibody to human parvovirus B19 in pregnant women in Kuwait. Acta Tropica. 1999;73:225–229. doi: 10.1016/s0001-706x(99)00033-9. [DOI] [PubMed] [Google Scholar]
- 6.Enders M et al. Fetal morbidity and mortality after acute human parvovirus B19 infection in pregnancy: prospective evaluation of 1018 cases. Prenatal Diagnosis. 2004;24:513–518. doi: 10.1002/pd.940. [DOI] [PubMed] [Google Scholar]
- 7.Brown T et al. Intrauterine parvovirus infection associated with hydrops fetalis. Lancet. 1984;2:1033–1034. doi: 10.1016/s0140-6736(84)91126-7. [DOI] [PubMed] [Google Scholar]
- 8.PHLS. Prospective study of human parvovirus (B19) infection in pregnancy. Public Health Laboratory Service Working Party on Fifth Disease. British Medical Journal. 1990;300:1166–1170. doi: 10.1136/bmj.300.6733.1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Miller E et al. Immediate and long term outcome of human parvovirus B19 infection in pregnancy. British Journal of Obstetrics and Gynaecology. 1998;105:174–178. doi: 10.1111/j.1471-0528.1998.tb10048.x. [DOI] [PubMed] [Google Scholar]
- 10.Yaegashi N. Pathogenesis of nonimmune hydrops fetalis caused by intrauterine B19 infection. Tohoku Journal of Experimental Medicine. 2000;190:65–82. doi: 10.1620/tjem.190.65. [DOI] [PubMed] [Google Scholar]
- 11.Searle K, Guilliard C, Enders G. Parvovirus B19 diagnosis in pregnant women – quantification of IgG antibody levels (IU/ml) with reference to the international parvovirus B19 standard serum. Infection. 1997;25:32–34. doi: 10.1007/BF02113504. [DOI] [PubMed] [Google Scholar]
- 12.Enders G, Biber M. Parvovirus B19 infections in pregnancy. Behring Institute Mitteilungen. 1990;85:74–78. [PubMed] [Google Scholar]
- 13.Wiersbitzky S et al. Seroprevalence of human parvovirus B 19 antibodies (Sticker's disease/erythema infectiosum) in the DRG population [in German] Kinderärztliche Praxis. 1990;58:185–189. [PubMed] [Google Scholar]
- 14.Jensen IP et al. An epidemic of parvovirus B19 in a population of 3,596 pregnant women: a study of sociodemographic and medical risk factors. British Journal of Obstetrics and Gynaecology. 2000;107:637–643. doi: 10.1111/j.1471-0528.2000.tb13306.x. [DOI] [PubMed] [Google Scholar]
- 15.Knowles SJ et al. Susceptibility to infectious rash illness in pregnant women from diverse geographical regions. Communicable Disease and Public Health. 2004;7:344–348. [PubMed] [Google Scholar]
- 16.van Gessel PH et al. Incidence of parvovirus B19 infection among an unselected population of pregnant women in the Netherlands: A prospective study. European Journal of Obstetrics, Gynecology and Reproductive Biology. doi: 10.1016/j.ejogrb.2005.11.042. [DOI] [PubMed] [Google Scholar]
- 17.Kelly HA et al. The age-specific prevalence of human parvovirus immunity in Victoria, Australia compared with other parts of the world. Epidemiology and Infection. 2000;124:449–457. doi: 10.1017/s0950268899003817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gilbert NL et al. Seroprevalence of parvovirus B19 infection in daycare educators. Epidemiology and Infection. 2005;133:299–304. doi: 10.1017/s0950268804003474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bremner JA, Cohen BJ. Parvovirus B19 as a cause of anemia in human immunodeficiency virus-infected patients. Journal of Infectious Diseases. 1994;169:938–940. doi: 10.1093/infdis/169.4.938a. [DOI] [PubMed] [Google Scholar]
- 20.Crowcroft NS, Cohen BJ, Miller E. Human parvovirus B19 infection in pregnancy. Perinatology. 1999;1:61–72. [Google Scholar]
- 21.Bosman A, Wallinga J, Kroes AMC. Fifth disease every four years: parvovirus B19. Infectieziekten Bulletin. 2002;13:215–219. [Google Scholar]
- 22.Morgan-Capner P, Crowcroft NS. Guidelines on the management of, and exposure to, rash illness in pregnancy (including consideration of relevant antibody screening programmes in pregnancy) Communicable Disease and Public Health. 2002;5:59–71. [PubMed] [Google Scholar]
- 23.Crane J. Parvovirus B19 infection in pregnancy. Journal of Obstetrics and Gynaecology Canada. 2002;24:727–743. [PubMed] [Google Scholar]
- 24.Cohen BJ, Buckley MM. The prevalence of antibody to human parvovirus B19 in England and Wales. Journal of Medical Microbiology. 1988;25:151–153. doi: 10.1099/00222615-25-2-151. [DOI] [PubMed] [Google Scholar]
- 25.Eis-Hübinger AM et al. The prevalence of antibody to parvovirus B19 in hemophiliacs and in the general population. Zentralblatt Bakteriologie. 1996;284:232–240. doi: 10.1016/s0934-8840(96)80098-3. [DOI] [PubMed] [Google Scholar]
- 26.Kelly HA et al. Fifth disease in a small rural community. What are the consequences? Australian Family Physician. 1999;28:139–144. [PubMed] [Google Scholar]
- 27.Valeur-Jensen AK et al. Risk factors for parvovirus B19 infection in pregnancy. Journal of the American Medical Association. 1999;281:1099–1105. doi: 10.1001/jama.281.12.1099. [DOI] [PubMed] [Google Scholar]
- 28.CDC. http://www.cdc.gov/ncidod/diseases/parvovirus/B19&preg.htm http://www.cdc.gov/ncidod/diseases/parvovirus/B19&preg.htm