SUMMARY
Aboriginal Australians in remote communities have high rates of rheumatic heart disease (RHD); yet pharyngitis is reportedly rare whilst pyoderma is common. Some strains of group A streptococci (GAS) have preference for the throat and others for the skin depending on M protein type. A study in three remote communities provided 350 GAS isolates for emm sequence typing, 244 were also emm pattern typed. There was 100% correlation between emm sequence and pattern type. Patterns D and E (non-throat tropic) made up 71% of throat and 87% of skin isolates although patterns A–C (throat tropic) were more common in the throat than the skin (RR 2·3, 95% CI 1·4–3·8) whilst the opposite was found for pattern D (RR 2·2, 95% CI 1·7–3·0). Pattern E favoured the throat (RR 1·4, 95% CI 1·1–1·8). Where environmental factors predispose to skin infection, emm pattern types D and E prevail, whatever the recovery site.
INTRODUCTION
The burden of disease due to group A streptococcus (GAS; Streptococcus pyogenes) varies widely from place to place and population to population. The relative incidence of GAS pharyngitis appears to be higher in temperate climate regions whilst pyoderma is less common [1–3]. In some tropical settings and minority indigenous populations, GAS skin infection predominates and symptomatic pharyngitis is relatively rare [4–6]. Nevertheless, these populations may still have high rates of acute rheumatic fever (ARF) and rheumatic heart disease (RHD) [7]. Aboriginal Australians in remote tropical communities have some of the highest reported rates of ARF/RHD in the world [8] and it has been hypothesized that skin infection plays a pathogenic role in ARF in this population [9].
The variable potential of different stains of GAS to cause post-streptococcal sequelae was observed more than 60 years ago [10, 11]. In the 1950s, Rammelkamp and others observed that GAS with specific M serotypes appeared to cause acute post-streptococcal glomerulonephritis (APSGN) and these were not serotypes associated with ARF [12]. ARF was also seen to follow GAS throat infection alone whilst APSGN occurred after either throat or skin infection [13]. This gave rise to the concept of separate skin and throat GAS types.
In the early 1970s, Widdowson and others demonstrated the presence of an M-associated protein that separated GAS into two antigenic groups (I and II) matching the known skin and throat types [14]. This was subsequently shown to be due to a cell surface lipoproteinase on skin GAS types that binds fibronectin and causes opacity in horse serum [serum opacity factor (SOF) or streptococcal fibronectin binding protein II – SfbII] [15, 16]. Known rheumatogenic M types were predominantly SOF-negative. In 1989, Bessen and co-workers differentiated two distinct classes of M protein, based on the C repeat region. Class I correlated with SOF-negative strains and contained serotypes associated with outbreaks of ARF, whereas Class II strains were associated with skin tropism [17]. A molecular typing method for GAS was developed in the 1990s based on the nucleotides that determine the variable amino terminus of the M protein on the emm gene. M serotypes and emm types were shown to be concordant [18, 19]. Subsequently, a polymerase chain reaction (PCR)-based mapping technique further differentiated five patterns of emm and related genes; patterns A–C were associated with the throat, pattern D with the skin and pattern E was found in isolates from both throat and skin [20]. With few exceptions, GAS isolates of a given emm sequence type (emmST) were found to have a predictable emm pattern type [21]. An additional genetic marker for skin preference is plasminogen-binding group A streptococcal M protein (PAM) [22] that is found in many GAS isolates with pattern type D; it has also been associated with invasive infection [23].
The relationship between emmST, emm pattern type and site of GAS infection for the most part appears to hold in studies published from temperate climates and relatively low incidence settings for ARF [20, 24]. Yet, this is not the case for all tropical and high-incidence settings. For example, a study of GAS isolates from a remote Australian Aboriginal island community found that pattern types D and E were predominant, whatever the site of recovery [25]. The study was limited by the paucity of throat isolates (16/141) because GAS throat carriage was so uncommon.
This study characterizes GAS isolates recovered from throat and skin swabs as part of a prospective surveillance project conducted in remote mainland Aboriginal communities with exceptionally high rates of ARF/RHD [26]. The aim was to confirm the relationship between emmST, emm pattern type, PAM and SOF in these remote settings and to assess whether emm pattern type correlates with the site of GAS recovery. Finding a predominance of emm pattern types D and E would also lend support to the skin infection hypothesis in ARF.
MATERIALS AND METHODS
Source of GAS isolates
GAS isolates came from a longitudinal surveillance study of streptococcal skin infection, pharyngitis and throat carriage in three remote mainland Aboriginal communities in the tropical Top End of the Northern Territory, Australia. The communities (1, 2 and 3) were separated by at least 400 km. The aim of the study was to investigate the association of GAS isolates with ARF in these settings [4]. The study protocol was approved by the local ethics committee and informed consent was obtained. Researchers then endeavoured to visit enrolled households on a monthly basis, for 2 years in the case of community 1 and for 1 year each in communities 2 and 3. Each individual was asked about sore throat (in the local language) and each throat was inspected for erythema, pus and tonsillar enlargement. Throat swabs were then taken from every person present according to a throat swab protocol, regardless of throat symptoms. Children and parents were asked about the presence of skin sores before limbs, exposed areas and the trunk were carefully inspected. Pyoderma was defined as one or more pustular, crusted, or vesicular lesions or dry and inflamed skin ulcers >1 cm in diameter. Non-infected insect bites and non-inflamed partly healed pyoderma lesions were excluded [4]. Swabs were taken from any skin sores. Additional clinical and demographic information was also collected.
Because we were unable to obtain blood samples for serological testing, individuals were considered to be carrying GAS in the throat if GAS was recovered from the throat swab and they were asymptomatic at the time.
Recovery and identification of GAS isolates
Culture methods have been described in more detail elsewhere [26]. Plates were incubated at 37°C in 5% CO2 and examined after 24 h and 48 h. Large colony-forming beta-haemolytic streptococci (BHS) were subcultured for identification using a Streptococcal Grouping kit (Oxoid Diagnostic Reagents, England, UK). Isolates were then stored in tryptone soya broth (Oxoid) with 15% glycerol at −70°C.
emm sequence type determination
The procedure for emm sequence typing followed that recommended on the Centers for Disease Control and Prevention (CDC) website [27] with minor modifications. We used InstaGeneTM matrix (Bio-Rad, Hercules, CA, USA) for DNA sample preparation; 20 colonies were harvested directly from culture plates and re-suspended in 200 μl. All other steps were according to manufacturer's instructions. PCR was conducted in 50 μl reaction volumes with 5 μl of the InstaGeneTM preparation, 10 nmol dNTPs, 25 pmol each of primers 1 and 2, 2·5 U Taq (Qiagen, Hilden, NRW, Germany), 5 μl 10× Taq buffer, sdH2O to 50 μl. PCR clean-up was done using QIAquick 96 PCR purification kit (Qiagen), eluting in 60 μl sdH2O.
For the sequencing reaction undiluted BigDye terminator version 3.1 (Applied Biosystems, Foster City, CA, USA) premix in half volume (10 μl) with 2 μl purified PCR product, 12·5 pmol emmseq2, 4 μl premix and 3·5 μl sdH2O was used and the reaction program was as per protocol. Clean up was achieved by adding 10 μl sdH2O and using DyeEx96 (Qiagen). The product was desiccated and sent to a commercial sequencing facility for separation. For sequence analysis, electropherograms were viewed with DNAstar Seqman software (Madison, WI, USA) and sequences were blasted against the CDC Streptococcus pyogenes emm sequence database [27]. Novel emm sequences were submitted to the administrator for assignment.
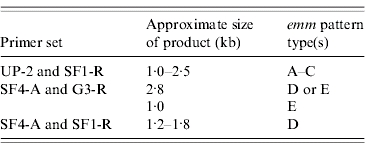
emm pattern type determination
The emm pattern type was determined according to the protocol described by Bessen et al. [25], with a restricted set of primers as shown in Table 1.
Table 1.
Primer set used for emm pattern typing [25]
Presence of PAM and SOF
PAM-positive emmST were differentiated by identifying sequences with homology to the plasminogen-binding A repeats of PAM within the deduced amino-acid sequence of the translated emm sequence data [22, 23]. Information regarding the presence of the SOF phenotype for each emm sequence type was obtained from the CDC website and published sources [27, 28].
Data analysis
Data were analysed using stata 8 (Stata Corporation, College Station, TX, USA). Relative risks (RR) for emm pattern types were calculated by comparing the proportions for each site of GAS recovery and confidence intervals (CI) were calculated by standard methods.
RESULTS
Surveillance and recovery of GAS isolates
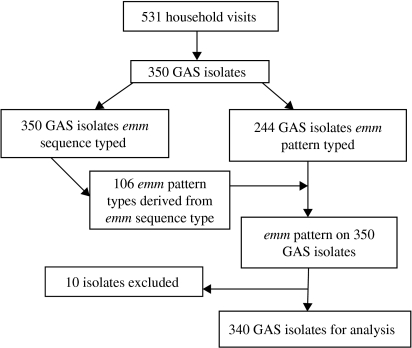
Forty-nine households and 1173 people were enrolled. There were 531 household visits and 4842 consultations. Some of the epidemiological data have been documented in a previous report; symptomatic pharyngitis was extremely rare in study children and pyoderma was common [4]. Three hundred and fifty GAS isolates were available for molecular typing, 222 from the throat and 128 from pyoderma lesions. All isolates were emm sequence typed. The first 244 GAS isolates, 150 throat and 94 skin isolates, were also emm pattern typed (Fig. 1).
Fig. 1.
Flow diagram of GAS isolates: determination of emm pattern type.
Long-term throat carriage of a specific GAS emmST was uncommon and there were only six people in the study who had the same emmST recovered from the throat on more than one occasion (providing an extra nine isolates). If GAS of a specific emmST was recovered from multiple skin sites from a person on the same day, they were not counted as multiple isolates. However, one child had emm100 recovered from skin sores for two consecutive months (providing one extra isolate). Otherwise we did not recover GAS from skin sores in a serial manner from anyone else. As a result 10 GAS isolates were removed from the analysis (Fig. 1). There were eight instances where GAS was recovered from the skin and the throat from one individual at the same visit; on four occasions they had a different emmST in the throat from that on the skin and four had the same emmST at both sites. These were left in the analysis. On 61 occasions more than one person in a household was colonized with a specific emmST at the same time or at a subsequent visit.
Correlation of emm sequence type, emm pattern type and site of recovery
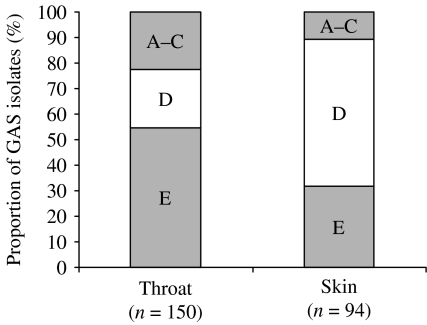
Consistent with published data [21, 25], we found 100% concordance between emm sequence type and emm pattern type in the first 244 GAS isolates from this study. We were therefore confident about predicting the emm pattern type for the remaining 106 GAS isolates where we knew the emm sequence type (Fig. 1). Summary data for emm sequence type, emm pattern type and site of recovery are shown in Table 2. The combined emm pattern data for skin and throat isolates are shown in Figure 2. Of 213 isolates recovered from the throat, 61 were pattern types A–C (29%) whilst 16/127 skin isolates were types A–C (13%) (RR for throat 2·3, 95% CI 1·4–3·8). Pattern type D accounted for 67/127 (53%) skin isolates and 51/213 throat isolates (24%) (RR for skin 2·21, 95% CI 1·7–3·0). Pattern type E was also more common in throat isolates (101/213, 47%), than skin isolates (44/127, 35%) (RR for throat 1·4, 95% CI 1·1–1·8). GAS was recovered from the throat of only two people in the study with symptomatic pharyngitis (both adults); the emm sequences types were 11 and 87 (both emm pattern type E).
Table 2.
emm sequence types and emm pattern types from three remote communities
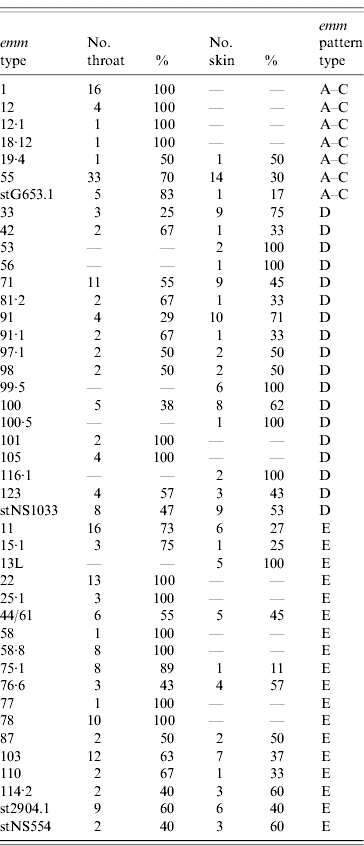
Fig. 2.
Percentage of emm pattern types by site of recovery.
Outbreak of emm55
The data were skewed by an outbreak during February 2005 when the prevalence of pyoderma in children of community 3 jumped to 18% compared to the median point prevalence of 6·1%. It coincided with the sudden appearance of GAS emm55 (pattern types A–C) in both skin sores (n=5) and throat (n=18). The strain had not previously been seen in the study. There was no discernible increase in the incidence of sore throat or proven GAS pharyngitis, but there was a subsequent community outbreak of APSGN [29]. The same emm sequence type (emm55) then appeared in community 1 during April 2005 (skin=2 and throat=15); it was not accompanied by a detectable increase in pyoderma or pharyngitis, but it did appear to precipitate another outbreak of APSGN (Northern Territory Centre for Disease Control, Darwin, unpublished data). Up to the time of the appearance of emm55, pattern types A–C had accounted for only 12/179 (6·7%, 95% CI 4–11) of GAS isolates. In the first 6 months of 2005, types A–C accounted for 65/162 (40%, 95% CI 33–48) of GAS isolates, 72% (47/65) of those were emm55. Overall, this sequence type accounted for 47/61 (77%) of pattern A–C throat isolates and 14/16 (88%) of A–C skin isolates.
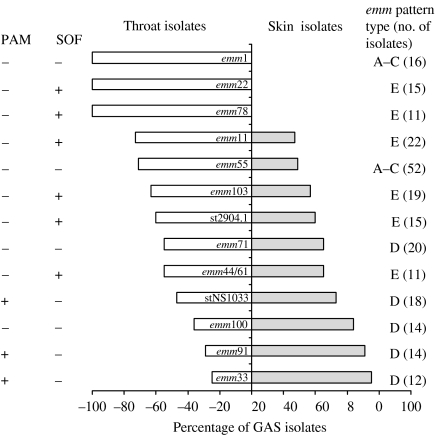
Gradation of tissue tropism
Thirteen of the most common emm sequence types (with >10 isolates) and site of recovery are shown in Figure 3, together with PAM and SOF patterns. A transition from pattern types A–C, through pattern type E, and then to pattern type D can be seen as the GAS isolates move from throat tropic to more skin tropic. One exception is the outbreak strain, emm55. Three of the five most common pattern D isolates were PAM positive and SOF was positive in all six of the common pattern E types. Pattern A–C types (emm1 and emm55) were negative for both PAM and SOF.
Fig. 3.
The most common GAS emm sequence types (>10 isolates) showing the percentages recovered from the throat and from the skin together with emm pattern type. PAM, Presence of the plasminogen-binding group A streptococcal M protein genotype; SOF, serum opacity factor.
DISCUSSION
The findings of this study confirm that emm pattern type can be predicted by emm sequence type in GAS isolates from these remote communities. This matches the findings of McGregor et al. who studied 495 GAS isolates collected from many parts of the world [21] including several tropical countries. The emm gene codes for M protein, a key anti-phagocytic virulence factor that forms the basis of M serological typing and is responsible for evoking serotype-specific host immunity. For the most part, specific emm types are clonally related, when compared by multilocus sequence typing (MLST) using bacterial housekeeping genes, although there are some exceptions where one MLST sequence type is associated with more than one emm sequence type [21]. This mainly occurs in skin types (emm pattern D) and suggests recombinatorial replacement of emm type. Such recombination may be most likely to occur at skin sites, such as in pyoderma, where multiple GAS strains can be present together and accompanied by selective pressure from the host immune response.
The distinction between types associated with throat and skin appears to be most marked in temperate regions of the northern hemisphere. M serotypes or emm sequence types corresponding to pattern types A–C or E predominate in throat isolates from the United Kingdom, continental Europe and the United States [2, 24, 30, 31]. By contrast, pyoderma was found to be the dominant manifestation of GAS infection in a remote Aboriginal island community and was mainly attributable to pattern types D (43%) and type E (40%); one reason may be that skin isolates outnumbered throat isolates by 10:1 [25]. A–C was the most abundant pattern type in throat isolates, but the numbers were small with only three emmST identified. This study covered a much larger population and produced a high proportion of throat isolates, providing the GAS emm pattern type distribution in widely separated mainland Aboriginal communities that was similar to that described in the remote island population. It is reasonable to suggest that this emm pattern type distribution is likely to be the norm rather than the exception across the region.
A previous US study of serological response had shown that patients with ARF have an elevated response to the specific class I epitope but little response to class II epitope [32]. In Australian Aboriginal populations, raised levels of antibodies to class I and class II epitopes have not been associated with any specific disease but probably indicate the burden of GAS exposure [33]. In this setting, it has been suggested that the high rates of impetigo in childhood engender non-type specific protective immunity against later throat colonization and pharyngitis. This has yet to be proven.
A similar picture to that seen here has been observed in a study from Ethiopia where 78 different emm sequence types were found in 217 GAS isolates [34]. Pattern type E was responsible for 38% of isolates, pattern D for 28% and patterns A–C for 18%. Patterns A–C accounted for 3% of skin isolates and 24% of throat isolates. Pattern D was also responsible for 28% of GAS pharyngitis and 4/7 of the isolates associated with ARF. Likewise pattern types D and E dominate in populations of north and south in India, although the rates of throat and skin infection are markedly different; the south Indian population has high rates of pyoderma and the north Indian has high rates of pharyngitis [35, 36].
Despite prevalence rates of RHD >25/1000 in the three communities of this study (Northern Territory Rheumatic Heart Disease Prevention Program, unpublished data), pyoderma was the outstanding manifestation of GAS infection in children and emm pattern types D and E of GAS predominated. This study had a much higher proportion of throat isolates (222/350, 63%) than did a previous study conducted among Aboriginal people living on a remote island (16/141, 11%) [25] and provides a broader view. The data suggest that the background rate of pattern types A–C in the three mainland communities was <7% but the proportion was subsequently inflated by outbreaks in the two large communities of emm55 having emm pattern type A–C. Ironically, the outbreaks involved GAS skin infections (in community 3), not pharyngitis, and were also accompanied by outbreaks of APSGN rather than ARF. GAS M serotype 55 has previously been associated with similar outbreaks of APSGN in the Top End of the Northern Territory, Trinidad and elsewhere [37–39]. Another emm pattern type A–C, M/emm 12, has been associated with outbreaks of APSGN [40] and raises additional questions about the specificity of emm pattern as a predictor of disease.
It has previously been pointed out that emm pattern type is an imperfect marker of tissue tropism and does not preclude infection at other sites [25]. Indeed, the factors that determine tissue preference seem to be complex; they include SOF and PAM for the skin [15, 22] and maltodextrin utilization conferring the ability to survive in saliva for the throat [41]. Much remains a mystery. In this study (Fig. 3), PAM provided some indication of tissue preference; SOF provided none. The three most throat tropic emmST were exclusively isolated from the throat, whereas even the most skin tropic emmST were able to colonize the throat. Colonization of the throat following skin infection is not uncommon [42]. These results suggest that throat colonization is the default condition and that the ability to cause skin infection is probably due to the presence of one or more skin tropic factors that are absent in throat strains.
Our study reaffirms that where ecological and epidemiological factors predispose to skin infection, as occurs in overcrowded tropical environments with poor hygiene conditions [43], emm pattern types D and E prevail and even account for the majority of throat GAS isolates. Pyoderma is likely to remain the predominant GAS infection in remote tropical Australian Aboriginal communities in the absence of effective interventions [43]. There is evidence for extensive genetic recombination between GAS strains and this is more likely to occur where there is a high burden of GAS colonization and infection, especially where more than one strain occupies the same site [44]. Despite this recombination, our study confirms concordance between emm sequence type and emm pattern type when compared with the published data [5, 21, 25]. We therefore also conclude that emm pattern typing in these tropical settings, which is labour intensive and difficult to interpret, offers no useful information in addition to that provided by emm sequence typing when investigating the epidemiology of GAS.
ACKNOWLEDGEMENTS
We thank the families in the communities, the Aboriginal research officers and community health centre staff for their participation and support. We are also grateful to Dr Bernard Beall of the Centers of Diseases Control and Prevention (Atlanta) for his helpful advice. Hamish Cameron assisted with the emm sequence and pattern typing.
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Danchin MH et al. The burden of group A streptococcal pharyngitis in Melbourne families. Indian Journal of Medical Research. 2004;119:S144–147. [PubMed] [Google Scholar]
- 2.Martin JM et al. Group A streptococci among school-aged children: clinical characteristics and the carrier state. Pediatrics. 2004;114:1212–1219. doi: 10.1542/peds.2004-0133. [DOI] [PubMed] [Google Scholar]
- 3.Kumar Ret al. Epidemiology of group A streptococci in a north Indian community. Proceedings of the XVIth Lancefield International Symposium on Streptococci and Streptococcal Diseases. Palm Cove, Queensland, Australia: 2005 [Google Scholar]
- 4.McDonald M et al. Low rates of streptococcal pharyngitis and high rates of pyoderma in communities where rheumatic fever is hyperendemic. Clinical Infectious Diseases. 2006;43:683–689. doi: 10.1086/506938. [DOI] [PubMed] [Google Scholar]
- 5.Brahmadathan KNet al. Molecular epidemiology of group A streptococcal infections in south Indian children. Proceedings of the XVIth Lancefield International Symposium on Streptococci and Streptococcal Diseases. Palm Cove, Queensland, Australia: 2005 [Google Scholar]
- 6.Ogunbi O, Lasi Q, Lawal S.An epidemiological study of beta-hemolytic streptococcal infections in a Nigerian (Lagos) urban population Streptococcal Disease and the Community Proceedings of the Fifth International Symposium on Streptococcus pyogenes. Amsterdam, the Netherlands: Excerpta Medica; 1972, pp. 144–147. [Google Scholar]
- 7.Carapetis JR et al. The global burden of group A streptococcal diseases. Lancet Infectious Diseases. 2005;5:685–694. doi: 10.1016/S1473-3099(05)70267-X. [DOI] [PubMed] [Google Scholar]
- 8.Carapetis JR, Currie BJ, Mathews JD. Cumulative incidence of rheumatic fever in an endemic region: a guide to the susceptibility of the population. Epidemiology and Infection. 2000;124:239–244. doi: 10.1017/s0950268800003514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carapetis J, Currie B. Group A streptococcus, pyoderma, and acute rheumatic fever. Lancet. 1996;347:1271–1272. doi: 10.1016/s0140-6736(96)90797-7. [DOI] [PubMed] [Google Scholar]
- 10.Coburn A, Pauli R. Studies on the immune response of rheumatic subject and its relationship to activity of the rheumatic process IV. Characteristics of strains of hemolytic streptococci, effective and non-effective in initiating rheumatic fever. Journal of Clinical Investigation. 1935;14:755–762. doi: 10.1172/JCI100723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Seegal D, Earle D. A consideration of certain biological differences between acute glomerulonephritis and rheumatic fever. American Journal of Medical Sciences. 1941;201:528–539. [Google Scholar]
- 12.Rammelkamp CH. Epidemiology of streptococcal infections. Harvey Lectures. 1955;51:113–142. [PubMed] [Google Scholar]
- 13.Stollerman G. Nephritogenic and rheumatogenic group A streptococci. Journal of Infectious Diseases. 1969;120:258–263. doi: 10.1093/infdis/120.2.258. [DOI] [PubMed] [Google Scholar]
- 14.Widdowson JP, Maxted WR, Pinney AM. An M-associated protein antigen (MAP) of group A streptococci. Journal of Hygiene (Cambridge) 1971;69:553–564. doi: 10.1017/s0022172400021823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maxted WR et al. The use of serum opacity reaction in the typing of group A streptococci. Journal of Medical Microbiology. 1973;6:83–90. doi: 10.1099/00222615-6-1-83. [DOI] [PubMed] [Google Scholar]
- 16.Rakonjac J, Robbins J, Fischetti V. DNA sequence of the serum opacity factor of group A streptococci: identification of a fibronectin-binding domain. Infection and Immunity. 1995;63:622–631. doi: 10.1128/iai.63.2.622-631.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bessen D, Jones K, Fischetti V. Evidence for two distinct classes of streptococcal M protein and their relationship to rheumatic fever. Journal of Experimental Medicine. 1989;169:269–283. doi: 10.1084/jem.169.1.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Beall B, Facklam R, Thompson T. Sequencing emm-specific PCR products for routine and accurate typing of group A streptococci. Journal of Clinical Microbiology. 1996;34:953–958. doi: 10.1128/jcm.34.4.953-958.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bessen D, Fischetti V. Differentiation between two biologically distinct classes of group A streptococci by limited substitutions of amino acids within the shared region of M protein-like molecules. Journal of Experimental Medicine. 1990;172:1757–1764. doi: 10.1084/jem.172.6.1757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bessen D et al. Genetic correlates of throat and skin isolates of group A streptococci. Journal of Infectious Diseases. 1996;173:896–900. doi: 10.1093/infdis/173.4.896. [DOI] [PubMed] [Google Scholar]
- 21.McGregor KF et al. Multilocus sequence typing of Streptococcus pyogenes representing most known emm types and distinctions among subpopulation genetic structures. Journal of Bacteriology. 2004;186:4285–4294. doi: 10.1128/JB.186.13.4285-4294.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Svensson MD, Sjobring U, Bessen DE. Selective distribution of a high-affinity plasminogen-binding site among group A streptococci associated with impetigo. Infection and Immunity. 1999;67:3915–3920. doi: 10.1128/iai.67.8.3915-3920.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McKay FC et al. Plasminogen binding by group A streptococcal isolates from a region of hyperendemicity for streptococcal skin infection and a high incidence of invasive infection. Infection and Immunity. 2004;72:364–370. doi: 10.1128/IAI.72.1.364-370.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dicuonzo G et al. Group A streptococcal genotypes from pediatric throat isolates in Rome, Italy. Journal of Clinical Microbiology. 2001;39:1687–1690. doi: 10.1128/JCM.39.5.1687-1690.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bessen DE et al. Contrasting molecular epidemiology of group A streptococci causing tropical and nontropical infections of the skin and throat. Journal of Infectious Diseases. 2000;182:1109–1116. doi: 10.1086/315842. [DOI] [PubMed] [Google Scholar]
- 26.McDonald M et al. Recovering streptococci from the throat in remote tropical communities: a practical alternative to direct plating. Journal of Clinical Microbiology. 2006;44:547–551. doi: 10.1128/JCM.44.2.547-552.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Centers of Diseases Control and Prevention http://www.cdc.gov/ncidod/biotech/strep/strepindex.htm. http://www.cdc.gov/ncidod/biotech/strep/strepindex.htm . Streptococcus laboratory ( ). Accessed 10 December 2006.
- 28.Johnson DR et al. Characterization of group A streptococci (Streptococcus pyogenes): correlation of M-protein and emm-gene type with T-protein agglutination pattern and serum opacity factor. Journal of Medical Microbiology. 2006;55:157–164. doi: 10.1099/jmm.0.46224-0. [DOI] [PubMed] [Google Scholar]
- 29.Binns P, Markey P, Krause V. An outbreak of acute post-streptococcal glomerulonephritis in a remote Aboriginal community in 2005. Northern Territory Disease Control Bulletin. 2005;12:12–15. [Google Scholar]
- 30.Colman G et al. The serotypes of Streptococcus pyogenes present in Britain during 1980–1990 and their associations with disease. Journal of Medical Microbiology. 1993;39:165–178. doi: 10.1099/00222615-39-3-165. [DOI] [PubMed] [Google Scholar]
- 31.Fiorentino T et al. A genetic-based evaluation of the principal tissue reservoir for group A streptococci isolated from normally sterile sites. Journal of Infectious Diseases. 1997;176:177–182. doi: 10.1086/514020. [DOI] [PubMed] [Google Scholar]
- 32.Bessen D et al. Serologic evidence for a Class 1 group A streptococcal infection among rheumatic fever patients. Journal of Infectious Diseases. 1995;172:1608–1611. doi: 10.1093/infdis/172.6.1608. [DOI] [PubMed] [Google Scholar]
- 33.Brandt ER et al. Antibody levels to the class I and II epitopes of the M protein and myosin are related to group A streptococcal exposure in endemic populations. International Immunology. 2001;13:1335–1343. doi: 10.1093/intimm/13.10.1335. [DOI] [PubMed] [Google Scholar]
- 34.Tewodros W, Kronvall G. M protein gene (emm type) analysis of group A beta-hemolytic streptococci from Ethiopia reveals unique patterns. Journal of Clinical Microbiology. 2005;43:4369–4376. doi: 10.1128/JCM.43.9.4369-4376.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sharma M, Sriprakash KS Streptococci – New Insights into an Old Enemy. Amsterdam: Elsevier; 2006. Heterogeneity of community based pediatric GAS isolates from India: challenges to the multivalent vaccine; pp. 49–53. , pp. [Google Scholar]
- 36.Dey N et al. High diversity of group A Streptococcal emm types in an Indian community: the need to tailor multivalent vaccines. Clinical Infectious Diseases. 2005;40:46–51. doi: 10.1086/426443. [DOI] [PubMed] [Google Scholar]
- 37.Kearns T, Evans C, Krause V. Outbreak of acute post streptococcal glomerulonephritis in the Northern Territory-2000. Northern Territory Disease Control Bulletin. 2001;8:6–13. [Google Scholar]
- 38.Potter E et al. Tropical acute rheumatic fever and associated streptococcal infections compared with concurrent acute glomerulonephritis. Journal of Pediatrics. 1978;92:325–333. doi: 10.1016/s0022-3476(78)80036-5. [DOI] [PubMed] [Google Scholar]
- 39.Dillon H. Post-streptococcal glomerulonephritis following pyoderma. Reviews of Infectious Diseases. 1979;1:935–945. doi: 10.1093/clinids/1.6.935. [DOI] [PubMed] [Google Scholar]
- 40.Majeed HA et al. The concurrent associations of group A streptococcal serotypes in children with acute rheumatic fever or pharyngitis-associated glomerulonephritis and their families in Kuwait. Zentralblat Bakteriologie Mikrobiologie Hygiene. 1986;262:346–356. doi: 10.1016/s0176-6724(86)80007-4. [DOI] [PubMed] [Google Scholar]
- 41.Shelburne SA et al. Maltodextrin utilization plays a key role in the ability of group A streptococcus to colonize the oropharynx. Infection and Immunity. 2006;74:4605–4614. doi: 10.1128/IAI.00477-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Anthony B et al. The dynamics of streptococcal infections in a defined population of children: serotypes associated with skin and respiratory infections. American Journal of Epidemiology. 1976;104:652–666. doi: 10.1093/oxfordjournals.aje.a112344. [DOI] [PubMed] [Google Scholar]
- 43.Currie B. Group A streptococcal infections of the skin: molecular advances but limited therapeutic progress. Current Opinion in Infectious Diseases. 2006;19:132–138. doi: 10.1097/01.qco.0000216623.82950.11. [DOI] [PubMed] [Google Scholar]
- 44.Kalia A et al. Influence of recombination and niche separation on the population genetic structure of the pathogen Streptococcus pyogenes. Infection and Immunity. 2002;70:1971–1983. doi: 10.1128/IAI.70.4.1971-1983.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]