SUMMARY
Salmonella is one of the most common causes of foodborne infection in Europe with Salmonella enterica serovar Enteritidis (S. Enteritidis) being the most commonly identified serovar. The predominant phage type for S. Enteritidis is phage type (PT) 4, although PT 8 has increased in incidence. Within these phage types, pulsed-field gel electrophoresis (PFGE) provides a method of further subdivision. The international project, Salm-gene, was established in 2001 to develop a database of PFGE profiles within nine European countries and to establish criteria for real-time pattern recognition. It uses DNA fingerprints of salmonellas to investigate outbreaks and to evaluate trends and emerging issues of foodborne infection within Europe. The Salm-gene database contains details of about 11 700 S. Enteritidis isolates, demonstrating more than 65 unique PFGE profiles. The clonal nature of S. Enteritidis is evidenced by the high similarity and distribution of PFGE profiles. Over 56% (6603/11 716) of the submitted isolates of several different phage types were profile SENTXB.0001, although this profile is most closely associated with PT 4. The next most common profiles, SENTXB.0002 and SENTXB.0005, were closely associated with PT 8 and PT 21 respectively. Studies to investigate the relationship of profile types with outbreaks and possible vehicles of infection suggest that the incidence of PFGE profile SENTXB.0002, and thus PT 8, in some countries may be due to importation of foods or food production animals from Eastern Europe, where PT 8 is amongst the most frequently identified phage types. Collation of subtyping data, especially in the commonly recognized phage types, is necessary in order to evaluate trends and emerging issues in salmonella infection.
INTRODUCTION
Salmonella is a major cause of foodborne infection in Europe where 194 270 cases of human salmonellosis were reported in 2004 by the 15 Member States of the European Union and Norway [1]. It is a zoonotic pathogen with poultry, cattle and pigs being the primary reservoirs. Humans can acquire salmonella infections through the consumption of contaminated foods as well as contaminated drinking water. The food categories considered to pose the greatest hazard to public health include raw or undercooked food products of animal origin, especially poultry, eggs and products containing raw eggs, unpasteurized milk and milk products [2]. Also fresh produce has been implicated in salmonella transmission [3, 4]. International trade both in food animals and food products ensures that salmonella organisms are widely distributed throughout the European Union and worldwide.
Within Western Europe S. Enteritidis is the serovar most commonly identified by the national reference laboratories of the International Surveillance Network for Enteric Infections (Enter-net) [5, 6]. As this serovar forms a major subset of all the identified salmonella serotypes it has been necessary to further subtype S. Enteritidis in order to identify outbreaks of infection. The internationally standardized method for subtyping salmonellas in Europe and most Commonwealth countries is phage-typing based on the method of Ward et al. [7], with DNA fingerprinting being used as an adjunct in outbreak investigations in which enhanced strain discrimination is needed. A number of DNA-based methods, including pulsed-field gel electrophoresis (PFGE), are currently in use to supplement phage-typing [8, 9]. Of these, PFGE has been used as the principal method for subtyping of salmonellas in the United States since 1996 [10]. The European Community DG Research-Funded initiative (Project No. QLRT-2000-01940), Salm-gene, an international project that was established in 2001, developed a searchable database of PFGE profiles from human isolates within nine European countries aimed at establishing criteria for real-time pattern recognition and enhanced surveillance.
METHODS
Participants in the Salm-gene project included the Health Protection Agency, Centre for Infections, England and Wales (acting as Project Coordinator), together with eight other national reference laboratories within Europe. The other participants included Bakteriologisch-serologische Untersuchungsanstalt (Austria), Statens Serum Institut (Denmark), National Public Health Institute (Finland), Robert Koch-Institut (Germany), Instituto Superiore di Sanita (Italy), National Institute of Public Health & the Environment (The Netherlands), Scottish Salmonella Reference Laboratory (Scotland), and Instituto de Salud Carlos III (Spain).
Serotyping, phage-typing for epidemiologically important serotypes [7], antibiogram determination [11] and PFGE [12] have all been harmonized in the countries participating in the Salm-gene project.
Study design
From 2001 until the end of 2004 an agreed subset of data was sent to the coordinating centre on a monthly basis [13]. Using the harmonized methods, human isolates were subtyped locally in each of the participating countries. The PFGE images, in tag image file format (TIFF), together with additional microbiological and epidemiological information on each isolate were submitted to the coordinating centre. The data were entered into the central Salm-gene database and analysed using BioNumerics software (v.3.1, beta; Applied Maths, Sint-Martens-Latem Belgium). Only gels considered of acceptable quality in terms of image clarity, band definition and using the PulseNet universal size standard, S. Braenderup H9812 [14] were analysed. PFGE profiles in the Salm-gene database were designated using an agreed nomenclature and by comparison to a library of unique strain profiles created from the background strains in circulation in Western Europe at the start of the project. Initially all nine laboratories retrospectively subtyped a selection of isolates, using PFGE in order to create this library. Strains of S. Enteritidis entered into the database therefore represent a subset of isolates reported to each of the national laboratories between January 2000 and December 2004.
Typing and analysing the strains
The laboratory protocols used in Salm-gene have been developed to be compatible with those of PulseNet USA. This is a national subtyping network for foodborne pathogens in the United States. Similar networks have been extended in Canada, the Asia-Pacific region, Latin America and Europe [15]. PFGE was performed using the Bio-Rad CHEF system (Bio-Rad Laboratories Ltd, Hemel Hempstead, Herts, UK). Cells from overnight bacterial cultures were resuspended in cell suspension buffer (CSB), (100 mm Tris, 100 mm EDTA; pH 8·0) to a density of 0·38–0·44 at 450 nm. Agarose plugs were then prepared using an equivalent volume of resuspended cells to molten agarose containing Proteinase K (0·5 mg/ml final concentration). Cells were lysed in lysis buffer (50 mm Tris, 50 mm EDTA, 1% Sarkosyl, 0·1 mg/ml Proteinase K; pH 8·0) for 2 h (minimum) in a shaking waterbath (54°C). Plugs were washed twice in sterile distilled water and then washed 2–3 times in TE buffer at 50°C in a shaking waterbath. Sections (3 mm) from each agarose plug were placed in 50–100 μl reaction buffer with 0·2–0·8 U/μl of a rare cutting restriction endonuclease (XbaI) and incubated at 37°C, for 4 h (minimum). DNA macrorestriction fragments were resolved on 1% agarose gels using the preferred electrophoresis conditions of 6·0 V/cm (200 volts) at 14°C for 22 h (CHEF DRII), 20 h (CHEF DRIII), or 18 h (CHEF Mapper). Pulse times were ramped from 2 s (initial switch) to 64 s (final switch) during the run.
Comparisons between profiles were made using algorithms available within the BioNumerics program and dendrograms were produced using the unweighted pair-group method using arithmetic means (UPGMA). A profile differing by at least one band to a profile of another strain was assigned a new name [13].
RESULTS
The Salm-gene database contains details of over 11 716 S. Enteritidis isolates of which 96% (11 219/11 716) have been designated with a PFGE profile name. To date the library shows 65 unique PFGE profiles with a further 497 (4%) isolates requiring a final designation. While most of these remaining isolates demonstrate unique profiles they are awaiting validation before a final PFGE designation is entered into the database. Thus, the final number of unique profiles is expected to exceed the 65 demonstrated so far.
Of the S. Enteritidis isolates within the database, 95% (10 937/11 716) also have a designated phage type. The most common phage type was S. Enteritidis phage type (PT) 4, making up 30·4% (3566/11 716). S. Enteritidis PT 1 was the second most common phage type at 17·6% (2056/11 716) followed by S. Enteritidis PT 8 at 11·1% (1305/11 716), S. Enteritidis PT 21 at 8·9% (1045/11 716) and S. Enteritidis PT 14b at 5·7% (670/11 716). In total there were 82 different phage types for S. Enteritidis within the database, many of these had only one or two representatives.
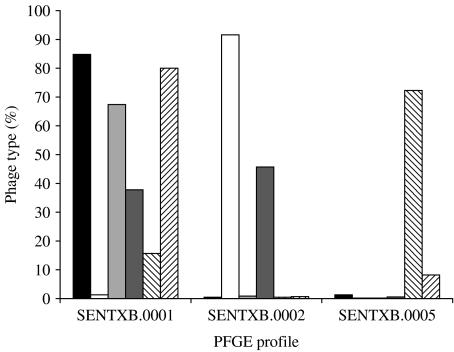
The predominant PFGE profile in all countries, regardless of phage type, was SENTXB.0001 with over 56% (6603/11 716) of all S. Enteritidis isolates demonstrating this profile. SENTXB.0001 was also the predominant, but not exclusive, PFGE profile for S. Enteritidis PT 4 (85%, 3027/3566) as this phage type was seen across a wide range of different PFGE profiles. There were 39 other PFGE profiles within the database that were linked to one or more isolates of S. Enteritidis PT 4 but the second most common profile (SENTXB.0014) only accounted for a further 5% (177/3566). PT 1 and PT 6 also shared SENTXB.0001 as their predominant profile at 80% (1645/2056) and 67% (390/579) respectively (Fig. 1).
Fig. 1.
Relationship between the most common phage types and their pulsed-field gel electrophoresis profiles. ■, PT 4; □, PT 8; , PT 6;
, PT 6; , PT 14b;
, PT 14b; , PT 21;
, PT 21; , PT 1.
, PT 1.
Overall, within the database the next most common profile at 16% was SENTXB.0002 (1877/11 716) followed by SENTXB.0005 (9·5%, 1108/11 716) but there were differences between each of the countries. Finland, Italy, Germany and The Netherlands all had SENTXB.0005 as the second most common profile, while for the remaining countries (Austria, Denmark, Scotland, Spain, England and Wales) it was SENTXB.0002. Similarly, most countries demonstrated the next most common profile to be SENTXB.0014 (2·7%, 311/11 716) but for two countries (Scotland and The Netherlands) SENTXB.0007 (1·8%, 206/11 716) was more common than SENTXB.0014.
The relationship between S. Enteritidis PT 8 and PFGE profile SENTXB.0002 was almost exclusive with approximately 92% (1195/1305) of these isolates demonstrating this profile (Fig. 1). The range of PFGE profiles was also narrower as S. Enteritidis PT 8 was only linked to 10 other profiles, of which the second most common profile (SENTXB.0009) represented only 2% (26/1305) of all the PT 8 isolates. The remaining profiles each accounted for less than 1% of the PT 8 isolates submitted. A strong association was also seen between PT 21 and profile SENTXB.0005 with more than 72% (756/1045) of this phage type sharing the same profile. PT 21 was also linked to 20 other PFGE profiles within the database of which the second most predominant link was to SENTXB.0001 (15·7%, 164/1045). The relationship between profile SENTXB.0002 and PT 14b was less dramatic but still accounted for almost 46% (306/670) of this phage type.
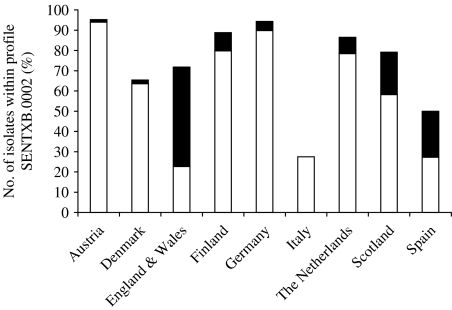
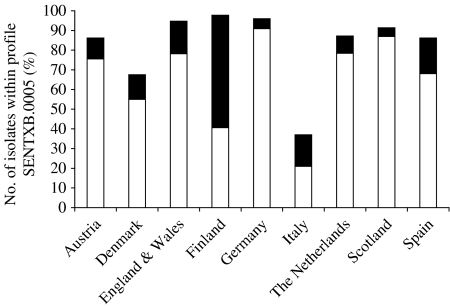
The distribution of phage types for all countries within the three most common PFGE profiles can be seen in the Table. Again, there was a strong association between SENTXB.0001 and PT 4, PT 1 and PT 6; SENTXB.0002 with PT 8 and PT 14b; and SENTXB.0005 with PT 21 and PT 1. For SENTXB.0001 the predominant phage type for all countries, except Spain, was PT 4. The second most common type was PT 1. The reverse was seen for Spain, where PT 1 predominated within SENTXB.0001 followed by PT 4. For SENTXB.0002 and SENTXB.0005, however, the distribution pattern for phage types varies more between countries. While PT 8 was the predominant type associated with SENTXB.0002 for most countries (Austria, Denmark, Finland, Germany, Italy, The Netherlands and Scotland) in England and Wales, PT 14b was the dominant phage type within this profile (Fig. 2). In Spain there was an almost equal distribution between PT 8 and PT 14b within SENTXB.0002. PT 21 was the most common PT within SENTXB.0005 except for Finland where PT 1 predominated (Fig. 3). PT 1 was the second most common phage type linked to this profile for all other countries.
Table.
Distribution, by country, of the three most common PFGE profiles and their related four most common phage types
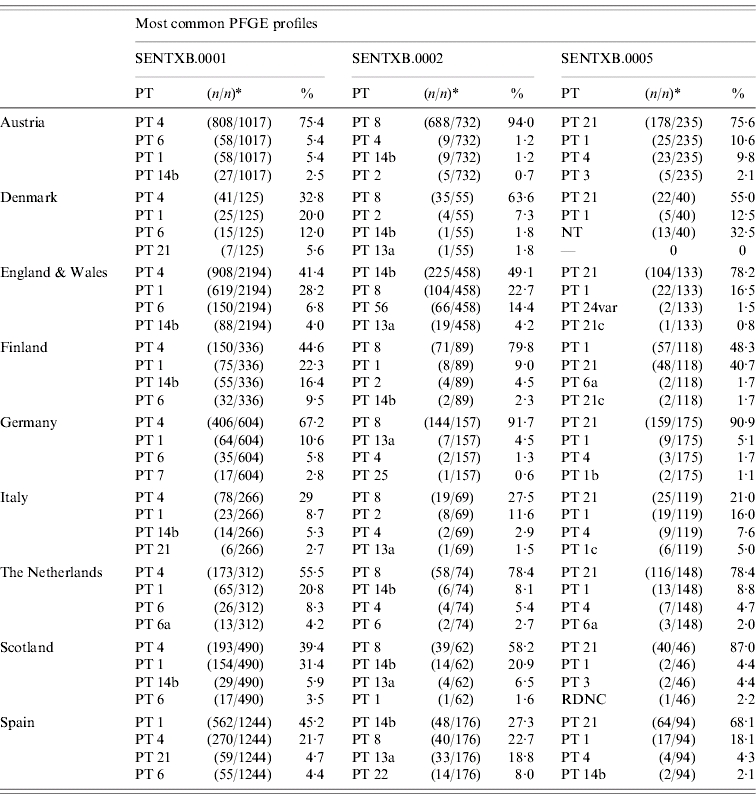
PT, Phage type; NT, not typed; RDNC, reacts but does not conform.
n/n, Number of isolates of a particular phage type/total number of isolates within a specific profile.
Fig. 2.
Relationship between PFGE profile SENTXB.0002 and phage types 8 (□) and 14b (■).
Fig. 3.
Relationship between PFGE profile SENTXB.0005 and phage types 21 (□) and 1 (■).
DISCUSSION
Major changes in the serotype and phage-type distribution of non-typhoidal salmonellas have occurred during the last 20 years in many European countries. The number of human S. Enteritidis infections has increased dramatically. During this time S. Enteritidis replaced S. Typhimurium as the predominant Salmonella serovar and remains the most commonly isolated serovar in humans today. While phage-typing has proven vital for improving outbreak ascertainment and for outbreak investigations in the countries where it is used, especially within the more common serovars, further discriminatory methods are sometimes necessary to differentiate within types of S. Enteritidis such as PT 4. As PFGE is currently the gold-standard molecular-typing method for Salmonella the Salm-gene project was established, in part, to develop a searchable database of PFGE profiles within Europe to enhance outbreak investigations. The two most common profiles, SENTXB.0001 and SENTXB.0002, accounted for almost 75% of all the Enteritidis isolates submitted to the database. This is comparable with other smaller studies where the most prevalent type accounted for 64% of both animal and human isolates [16]. Thus, the apparent lack of diversity in PFGE patterns seen within this project was not an unexpected finding for S. Enteritidis. Previous studies appear to have shown greater diversity for S. Enteritidis by using a second restriction enzyme such as BlnI [17] or by combining more than one technique. Although this was beyond the original remit of the project, the use of a second restriction enzyme would appear useful for discriminating particular serovars and phage types, e.g. PT 4.
The clonal nature of S. Enteritidis within the database has been previously evidenced by the high similarity and distribution of PFGE profiles from all the participating countries [13]. It was noted that strains generating different phage reactions shared a common genotype, particularly for PT 4. However, while the distribution of PFGE profiles did not always correspond with a single phage type, there was a strong association between SENTXB.0001 and PT 4, PT 1 and PT 6. There were also strong associations between PT 8 and SENTXB.0002, and PT 21 and SENTXB.0005. S. Enteritidis is so well known as having various animals as reservoirs for the disease that the Zoonosis Control Regulation (2160/2003) considers salmonellosis to be a disease that has a high impact on human health in the European Union. This directive regulates the control of salmonella and other specified foodborne zoonotic agents [18]. The results of a recent study looking at the comparative burden of salmonellosis, shows a high, linear correlation between salmonella prevalence in laying hens and human illness [19].
Across Europe, S. Enteritidis PT 4 is currently the main subtype in both animals and humans and is the most frequently isolated phage type in poultry. However, local variation between countries has also been seen and other phage types such as S. Enteritidis PT 8 are more common in Austria and Denmark than in other Western European countries [20].
Data from the European Union and Norway for 2002 have shown that overall S. Enteritidis was also the dominating serovar in chicken (Gallus gallus) breeding flocks, layers and broilers, representing 38% of isolates tested, and it has emerged as a major egg-associated pathogen. Approximately 70% of outbreaks caused by S. Enteritidis in Europe during the 1990s were related to eggs and egg products [20]. Previous studies in Denmark, during the period 1980–1990, of strains from poultry flocks [21] demonstrated that PT 1, followed by PT 4, were the most common types among the isolates that were tested, while isolates belonging to PT 8 were found exclusively in imported birds. However, data from Denmark for 2002 showed that PT 8 was the dominant phage type, being the main causative agent of salmonellosis in humans and also frequently isolated in laying hens. Similarly, in Germany, 12% of isolates in 2002 were PT 8 compared to only 4·5% in 1994 [22], although PT 4 still predominated at approximately 70%. On the other hand, in some countries, e.g. Finland, there is no known domestic reservoir of S. Enteritidis, and the infections caused by this serovar are mostly of foreign origin [23]. Both PT 4 and PT 8 were among those most frequently seen in this study and were closely associated with SENTXB.0001 and SENTXB.0002 respectively. In this study the emergence of SENTXB.0002 as the second most common profile would appear to reflect the trend seen in Western Europe, where PT 8 is becoming a type of increasing epidemiological relevance. This may be due to niches created by the decrease of one serotype or phage type being filled by others [24] although it is equally plausible that the new strains have displaced the old strains, possibly as a result of the movement of stock between countries. In this respect, data from the Enter-net database has identified a recent decrease in the proportion of PT 4 together with a significant increase in non-PT 4 phage types in Western Europe [6]. This increase in non-PT 4 S. Enteritidis may be due to importation of foods or food production animals from Eastern Europe, where PT 8 is amongst the most frequently identified phage type. In the Czech Republic, PT 8 was reported as the most common type in humans (92%) and in animals (79%) [25] while data from Poland show that in 2001, 22% of all S. Enteritidis isolates were identified as PT 8 [26]. In 1997 the Slovak Republic reported that PT 8 was the phage type most frequently identified (73%) [27] where it still accounted for 74% of all Enteritidis isolates in this republic in 2000 [28]. A recent study of S. Enteritidis infections in Swedish travellers found that PT 8 seemed to be more common among travellers returning from central European countries to Sweden while PT 4 dominated among travellers returning from most other European countries [29]. These authors also noted that in travellers returning from some countries in southern Europe, a previously rare phage type (PT 14b) became one of the more commonly observed types.
Thus, the incidence of profile SENTXB.0002 in the Salm-gene database may not only be due to rapidly growing international trade between countries in the European Union but may also reflect other factors such as travel. This would have facilitated the spread of PT 8 and PT 14b to countries where its incidence was previously low, although this requires verification. It was interesting to note that in England and Wales, although SENTXB.0002 was still the second most common profile this was largely due to PT 14b followed by PT 8. The only other country with a similar SENTXB.0002/PT 14b association was Spain. Within Western Europe, since 2000, the incidence of S. Enteritidis non-PT 4 infection has almost doubled with two phage types, PT 1 and PT 14b, accounting for most of the increase. Much descriptive, statistical and microbiological evidence supplied by investigators points to the use of eggs imported from Spain as a cause of the increase in these phage types in England and Wales [30]. The proportion of imported shell eggs from Spain had increased since 2000 to the extent that Spain was the largest exporter of eggs to the United Kingdom between 2003 and 2004. Thus, it is not unexpected to see these countries showing similar associations between SENTXB.0002 and PT 14b.
For the SENTXB.0005 associated phage types (PT 21 and PT 1) the general trend was the same for all countries, with the exception of Finland. Over the past 6 years, both these types have shown dramatic increases that are reflected in this study by profile SENTXB.0005 being the third most common profile in the database. PT 1 is often found in travellers returning from Mediterranean countries where the principal source of S. Enteritidis is chickens and egg products. Thus, it is likely that the occurrence in travellers also reflects contamination of these foods within these countries [6].
A prominent finding of our study was the considerable similarity, often regardless of country, in the association of specific PFGE profiles and particular phage types. This information would be particularly useful for those countries that do not routinely perform phage-typing but are able to perform PFGE. Italy appears to show much lower percentages for associations between PFGE profiles and phage types. This is probably due to the lower proportion of isolates (approximately 60%) that had phage-type data supplied to the database. The results suggest that PFGE analysis is still potentially a valuable tool for the characterization of S. Enteritidis. However, for several of the most common phage types causing infections in humans, it may be necessary to combine results obtained for two or more enzymes, to enhance the discriminatory power of the method.
There is a need for further differentiation and surveillance if we are to identify the sources of infection and possible routes of transmission allowing certain strains to proliferate and circulate in Western Europe. This would include information on the animal reservoirs of these phage types/PFGE profiles together with any other contributing factors such as food imports or travel history. It is therefore important to continually evaluate trends in Salmonella infection and to rapidly communicate surveillance information between countries in the European Union and worldwide. Where further discrimination may be required, it is especially important to include information on PFGE profiles of phage types that are common or appear to be increasing in numbers. To this end, data from the Salm-gene database has been transferred to the PulseNet Europe database in order to continue a real-time linked surveillance database system to detect disease clusters and investigate outbreaks of Salmonella. The Salm-gene project, not only created the large database of Salmonella DNA profiles but also harmonized the electronic transmission of exact microbiological data between countries. Thus, it has formed a steady basis that PulseNet Europe can exploit in the future.
ACKNOWLEDGMENTS
This project was funded by the European Community DG Research-Funded initiative (Project no. QLRT-2000-01940).
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Anon 2005. http://www.efsa.eu.int/science/monitoring_zoonoses/reports/1277_en.html. http://www.efsa.eu.int/science/monitoring_zoonoses/reports/1277_en.html . European Food Safety Authority (EFSA): Zoonoses reports, ). Accessed 5 September 2006.
- 2.Anon. EFSA Working group on opinion of the Scientific Panel on Biological Hazards related to the use of antimicrobials for the control of Salmonella in poultry. European Food Safety Authority Journal. 2004;115:1–76. [Google Scholar]
- 3.Lindsay EA et al. Role of electronic data exchange in an international outbreak caused by Salmonella enterica serotype Typhimurium DT204b. Emerging Infectious Diseases. 2002;8:732–734. doi: 10.3201/eid0807.010414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ward LR et al. A collaborative investigation of an outbreak of Salmonella enterica serotype Newport in England and Wales in 2001 associated with ready-to-eat salad vegetables. Communicable Disease & Public Health. 2002;5:301–304. [PubMed] [Google Scholar]
- 5.Fisher IST. The Enter-net international surveillance network – how it works. Eurosurveillance. 1999;4:52–55. doi: 10.2807/esm.04.05.00073-en. [DOI] [PubMed] [Google Scholar]
- 6.Fisher IST. Dramatic shift in the epidemiology of Salmonella enterica serotype Enteritidis phage types in Western Europe, 1998–2003 – results from the Enter-net international salmonella database. Eurosurveillance. 2004;9:43–45. [PubMed] [Google Scholar]
- 7.Ward LR, de Sa JD, Rowe B. A phage-typing scheme for Salmonella Enteritidis. Epidemiology and Infection. 1987;99:291–294. doi: 10.1017/s0950268800067765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Threlfall EJ et al. Application of pulsed-field gel electrophoresis to an international outbreak of Salmonella agona. Emerging Infectious Diseases. 1996;2:130–132. doi: 10.3201/eid0202.960209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Threlfall EJ et al. Molecular fingerprinting defines a strain of Salmonella enterica serotype Anatum responsible for an international outbreak associated with formula-dried milk. Epidemiology and Infection. 1998;121:289–293. doi: 10.1017/s0950268898001149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Swaminathan B et al. PulseNet: the molecular subtyping network for foodborne bacterial disease surveillance, United States. Emerging Infectious Diseases. 2001;7:382–389. doi: 10.3201/eid0703.010303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Threlfall EJ et al. Harmonisation of antibiotic susceptibility testing for Salmonella – results of a study by 18 national reference laboratories within the European Union-funded Enter-net group. Microbial Drug Resistance. 1999;5:195–200. doi: 10.1089/mdr.1999.5.195. [DOI] [PubMed] [Google Scholar]
- 12.Peters TM et al. The Salmgene project – a European collaboration for DNA fingerprinting for food-related salmonellosis. Eurosurveillance. 2003;8:46–50. doi: 10.2807/esm.08.02.00401-en. [DOI] [PubMed] [Google Scholar]
- 13.Gatto AJ et al. Distribution of molecular subtypes within Salmonella enterica serotype Enteritidis phage type 4 and S. Typhimurium definitive phage type 104 in nine European countries, 2000–2004: results of an international multi-centre study. Epidemiology and Infection. 2006;134:729–736. doi: 10.1017/S0950268805005820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hunter SB et al. Establishment of a universal size standard strain for use with the PulseNet standardized pulsed-field gel electrophoresis protocols: converting the national databases to the new size standard. Journal of Clinical Microbiology. 2005;43:1045–1050. doi: 10.1128/JCM.43.3.1045-1050.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Swaminathan B et al. Building PulseNet International: an interconnected system of laboratory networks to facilitate timely public health recognition and response to foodborne disease outbreaks and emerging foodborne diseases. Foodborne Pathogens and Disease. 2006;3:36–50. doi: 10.1089/fpd.2006.3.36. [DOI] [PubMed] [Google Scholar]
- 16.Liebana E et al. Multiple genetic typing of Salmonella Enteritidis phage-types 4, 6, 7, 8 and 13a isolates from animals and humans in the UK. Veterinary Microbiology. 2004;100:189–195. doi: 10.1016/j.vetmic.2004.01.020. [DOI] [PubMed] [Google Scholar]
- 17.Fernandez J et al. Analysis of molecular epidemiology of Chilean Salmonella enterica serotype enteritidis isolates by pulsed-field gel electrophoresis and bacteriophage typing. Journal Clinical Microbiology. 2003;41:1617–1622. doi: 10.1128/JCM.41.4.1617-1622.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.de Jong B, Ekdahl K. Human salmonellosis in travellers is highly correlated to the prevalence of salmonella in laying hen flocks. Eurosurveillance. 2006;11:7. doi: 10.2807/esw.11.27.02993-en. [DOI] [PubMed] [Google Scholar]
- 19.Anon http://europa.eu.int/smartapi/cgi/sga_doc?smartapi!celexapi!prod!CELEXnumdoc&lg=EN&numdoc=32003R2160&model=guichett. http://europa.eu.int/smartapi/cgi/sga_doc?smartapi!celexapi!prod!CELEXnumdoc&lg=EN&numdoc=32003R2160&model=guichett . European Commission. Regulation (EC) No 2160/2003 of the European Parliament and of the Council of 17 November 2003 on the control of salmonella and other specified foodborne zoonotic agents ( ). Accessed 5 September 2006.
- 20.Anon http://europa.eu.int/comm/food/food/biosafety/salmonella/zoonoses_reps_2001_en.htm. http://europa.eu.int/comm/food/food/biosafety/salmonella/zoonoses_reps_2001_en.htm . European Commission: Trends and sources of zoonotic agents in animals, feeding stuffs, food and man in the European Union and Norway in 2001. ( ). Accessed 1 March 2004.
- 21.Brown DJ et al. The characterization of Danish isolates of Salmonella enterica serovar Enteritidis by phage typing and plasmid profiling: 1980–1990. Acta Pathologica, Microbiologica et Immunologica Scandinavica. 1994;102:208–214. doi: 10.1111/j.1699-0463.1994.tb04866.x. [DOI] [PubMed] [Google Scholar]
- 22.Schroeter A et al. Salmonella enteritidis phage types in Germany. European Journal of Epidemiology. 1994;10:645–648. doi: 10.1007/BF01719587. [DOI] [PubMed] [Google Scholar]
- 23.Lukinmaa S et al. Genomic diversity within phage types of Salmonella enterica ssp. enterica serotypes Enteritidis and Typhimurium. Foodborne Pathogens and Diseases. 2006;3:97–105. doi: 10.1089/fpd.2006.3.97. [DOI] [PubMed] [Google Scholar]
- 24.van Duijkeren E et al. Serotype and phage type distribution of Salmonella strains isolated from humans, cattle, pigs, and chickens in the Netherlands from 1984 to 2001. Journal Clinical Microbiology. 2002;40:3980–3985. doi: 10.1128/JCM.40.11.3980-3985.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Karpiskova R, Mikulaskova M. Salmonella phage types distribution in the Czech Republic in 1991–1994. Central European Journal Public Health. 1995;3:161–162. [PubMed] [Google Scholar]
- 26.Cieslik A et al. Phage types and plasmid profiles of plasmid DNA strains of Salmonella enterica subsp. enterica ser. Enteritidis (S. Enteritidis) isolated from food poisoning outbreaks in 2001. Medycyna Doswiadczalna Mikrobiologia. 2002;54:325–334. [PubMed] [Google Scholar]
- 27.Majtanova L. Occurrence of Salmonella enterica serotype Enteritidis phage types in the Slovak Republic. European Journal Epidemiology. 1997;13:243–245. doi: 10.1023/a:1007313320486. [DOI] [PubMed] [Google Scholar]
- 28.Majtanova L. Occurrence of phage types of non-typhoid Salmonella serovar in the Slovak Republic 2000–2003. Epidemiologie Mikrobiologie Imunologie. 2004;53:70–73. [PubMed] [Google Scholar]
- 29.Nygård K et al. Emergence of new Salmonella Enteritidis phage types in Europe? Surveillance of infections in returning travellers. BMC Medicine. 2004;2:32. doi: 10.1186/1741-7015-2-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gillespie I.Salmonella Enteritidis non-phage type 4 infections in England and Wales 2000–2004: Report from a multi-agency national outbreak control team. Eurosurveillance Weekly200410http://www.eurosurveillance.org/ew/2004/041014.asp#2