SUMMARY
Humoral and cell-mediated immunity (CMI) against B. pertussis was assessed in a sample of adolescent, adult and senior subjects distributed in five different geographical areas in Italy. Most (99·1%) subjects had IgG anti-pertussis toxin (PT) antibodies exceeding the minimum detection level [⩾2 ELISA units (EU)/ml]. There were no significant differences between the genders; 6·2% samples recorded titres ⩾100 EU/ml. CMI was positive [stimulation index (SI) ⩾5] against PT in 39·0% of all samples. This study suggests that B. pertussis continues to circulate in age groups that have been previously considered to be uninvolved in the circulation of this pathogen and that adolescent and adult pertussis boosters may be of value in these populations. Nevertheless, over the last 10 years, large increases in vaccination coverage rates have contributed to reduce the spread of the aetiological agent, especially in the immunized population.
INTRODUCTION
Pertussis is a respiratory infection caused by Bordetella pertussis, a Gram-negative coccobacillus [1] that, once inside the respiratory tract, adheres to cells of the epithelium with adhesins and accomplishes its pathogenic action through the production of different toxins, most of which are strongly immunogenic [2–8].
Pertussis toxin (PT) is predominantly responsible for the pathogenesis of the disease by damaging respiratory tract cells, interfering with host defences and causing cellular toxicity [4]. Antibodies against PT are produced after natural infection and vaccination. Transmission of pertussis occurs through Flugge's droplets. The bacteria are highly infective and people living in contact with affected subjects, if not adequately protected, have a high probability of contagion [9].
In unvaccinated children, pertussis has a typical course and can cause severe symptoms and complications. In vaccinated children, adolescents and adults, the disease has a mild and often non-specific course [10].
In the pre-vaccination era the paucity of pertussis cases in adolescents and adults prompted the belief that infection as well immunization conferred lifelong immunity. Since the beginning of the vaccination era, reports of cases in young infants, adolescents, and adults has increased indicating the changing epidemiology of pertussis under the immunological pressure produced by vaccination [11–16]. Currently, it is well established that immunity against pertussis, whether natural or induced by vaccination, does not last a lifetime, and that immune protection tends to decay after about 10 years. These data are confirmed by epidemic outbreaks, especially in adolescents and adults, in geographical areas where vaccination coverage is high [17].
It is believed that antibodies produced against different antigens of B. pertussis play a key role in protection from the disease [8]. Unlike other vaccine-preventable diseases, no antibody level against a single antigen or a combination of antigens is definitively related to clinical protection. Nevertheless, some clinical trials using acellular vaccines containing three and five antigens, have shown that subjects with high antibody levels against PT, pertactin (PRN) and fimbriae (FIM) are less likely to develop the disease in a clinically evident form when exposed to the pathogen [18–20].
Cell-mediated immunity (CMI) also has a key role in protection against the infection; the development of this type of immune response can be very important in the clearance of the microorganism and in subsequent protection. Indeed, some authors claim that the proliferation of mononuclear cells of peripheral blood when stimulated by B. pertussis antigens [PT, PRN and filamentous haemagglutinin (FHA)] is inversely correlated to the clinical appearance of the disease [21, 22].
Epidemiologically, pertussis is a ubiquitous endemic/epidemic disease; a characteristic cyclical pattern could be observed in the pre-vaccination era with epidemic outbreaks occurring typically every 3–5 years and with a summer–autumn seasonality. In the pre-antibiotic and pre-vaccination era, incidence and mortality were extremely high especially in children aged <5 years. Although the introduction of antibiotics and vaccination has been associated with a large decrease in both incidence and mortality, pertussis, nevertheless, currently remains one of the most important vaccine-preventable paediatric diseases because of the high number of cases and the possibility of serious complications [23]. Important data have been recorded in many countries where high vaccination coverage rates have been reached. In these areas the reduced incidence of pertussis disease in children, contributes to a decreased opportunity of acquiring natural boosting. For these reasons, the disease is now increasingly registered in adolescents or adults who have lost their immunological protection and in infants that have not yet begun or completed their primary vaccination course. For the latter, the source of infection is predominantly through adolescents and adults [9].
Despite the increase in registered adult cases and the improved knowledge about the effects and complications of the disease, to date few studies have been conducted on adolescents and adults. Therefore, the true incidence of infection in these age groups remains largely unknown. The purpose of this study was to assess the humoral and CMI against B. pertussis in a sample of adolescent, adult and senior subjects distributed in five different geographical areas in Italy.
METHODS
Study design and subjects
This observational, cross-sectional, multicentre study was performed in six regions in Italy [North West (Genoa, Turin), North East (Ferrara), Centre (Florence), South East (Lecce) and South West (Messina)], representing 38·9% of the Italian resident population in 2004 when the study was performed. The study was approved by the Ethics Committees at each centre. Each subject, or their legally authorized representative, provided written consent for the collection of personal data and blood samples.
Male and female subjects aged ⩾12 years that had either applied for a health check or were donating blood were eligible for the study. Subjects aged <12 years, or those individuals affected by congenital or acquired immune deficiencies, or who did not provide written consent were excluded from the study. A case report form was completed for each subject, which included demographic, anamnestic, clinical and vaccination details.
For anamnestic analysis, data appertaining to the number of children in the family, residence (urban or rural), former B. pertussis infection, previous vaccination against pertussis and tetanus, persistent cough over the previous 12 months, and attendance at closed communities (e.g. schools, barracks, nursing homes, hospices, etc.) was collected.
Immunological assessment
A single blood sample was taken from each subject. IgG anti-PT antibodies were evaluated at the Hygiene and Microbiology Department of the University of Palermo, using an enzyme-linked immunosorbent assay (ELISA) method with a minimum level of detection of >2 ELISA units (EU)/ml [24, 25].
The assessment of CMI was performed at the CEBR (Centre of Excellence for Biomedical Research) at the University of Genoa. The stimulation index (SI; cut-off >5) on peripheral blood mononuclear cells was assessed using a lymphocytic proliferation test against specific antigens, mitogen and control antigens [PT, tetanus toxoid (TT), and phytohaemagglutinin (PHA)] [26, 27].
Statistical analysis
The primary objectives of the study were to assess the prevalence of IgG anti-PT in an Italian population aged >12 years stratified by age, gender and geographical area, and to evaluate CMI in half of this sample population. The secondary objectives were to study any trends between humoral and CMI and age, geographical area, type of residence, vaccination status, former infection and persistent cough in the previous 12 months.
The study required a total sample size of 1500 subjects; 300 subjects for each age group (12–14, 15–24, 25–44, 45–64, ⩾65 years); 250 subjects for each centre (50 per age group per centre).
Statistical analysis was performed using Stata 9 software (StataCorp LP, College Station, TX, USA). The association among qualitative variables was performed with Pearson's χ2 test. Geometric mean titres (GMTs) were calculated on each sample and a value of 1 (half of the cut-off) was given arbitrarily to negative sera. GMTs at each centre, stratified according to gender and age, were studied using ANOVA (with Bonferroni test for multiple comparisons). Therefore, a logistic regression model was used to verify the joint influences of enrolling centre, gender, age on the CMI response and on the IgG PT antibodies response.
RESULTS
A total of 1304 subjects (590 males, 687 females; 27 not determined) were enrolled between November 2004 and November 2005, of whom 616 were also included in the CMI analysis.
Humoral immunity
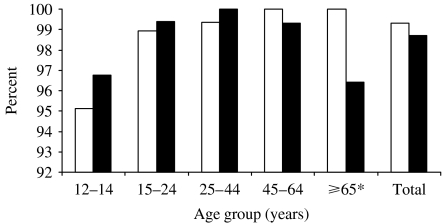
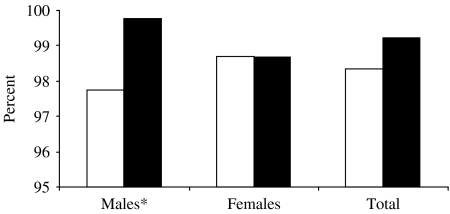
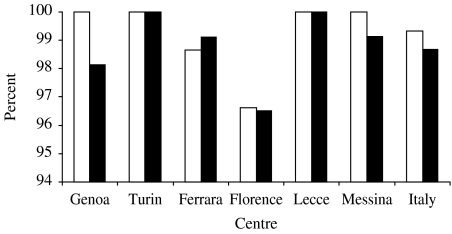
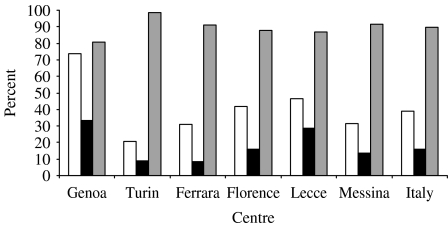
A total of 99·1% of subjects recorded IgG anti-PT antibodies ⩾2 EU/ml. Overall, there were no significant differences between the genders (99·3% males vs. 98·7% females; Fig. 1). When stratified according to age, the percentage of positive samples for IgG anti-PT was similar in the different age groups; the only statistically significant difference was found in subjects aged ⩾65 years (males vs. females, χ2=4·23, P<0·05). When stratified according to gender and age ⩽24 and >24 years, significantly fewer males in the younger age group were seropositive for IgG anti-PT antibodies (χ2 =6·24, P<0·05; Fig. 2). The seroprevalence by gender was similarly high at all the centres (Fig. 3).
Fig. 1.
Percentage of subjects with IgG anti-pertussis toxin ⩾2 EU/ml by gender and age group (n=1274). □, Males; ■, females. * P<0·05 for the ⩾65 years age group.
Fig. 2.
Percentage of subjects with IgG anti-pertussis toxin ⩾2 EU/ml by gender and age group (n=1274). □, Aged ⩽24 years; ■, aged >24 years. * P<0·05 for males.
Fig. 3.
Percentage of subjects with IgG anti-pertussis toxin ⩾2 EU/ml by gender and region (n=1274). □, Males; ■, females.
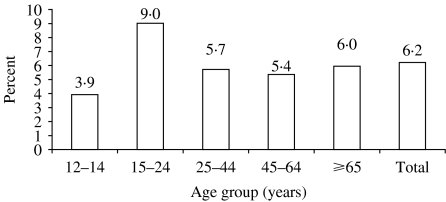
Further analysis of the positive samples revealed that 23·4%, 57·3%, 13·0% and 6·3% included titres in the range 2–8, 9–49, 50–99 and ⩾100 EU/ml, respectively. At the different centres, most samples had antibody titres in the range 9–49 EU/ml. When stratified according to age, no significant statistical difference was found. Age-specific distribution of PT IgG high titres (⩾100 EU/ml) in Italy is shown in Figure 4.
Fig. 4.
Age-specific distribution of IgG anti-pertussis toxin high titres (⩾100 EU/ml) in Italy.
Table 1 presents the GMTs recorded at each centre, stratified by gender and age group. The overall GMT was 19·2 EU/ml, ranging between 9·7 EU/ml (Florence) and 35·0 EU/ml (Lecce). After stratifying the sample by age, the only statistically significant difference observed was between the 12–14 years and 15–24 years age groups. No significant difference in GMTs was found after stratifying the data by gender.
Table 1.
Geometric mean titre (EU/ml) stratified by gender and age group and region (n=1301)
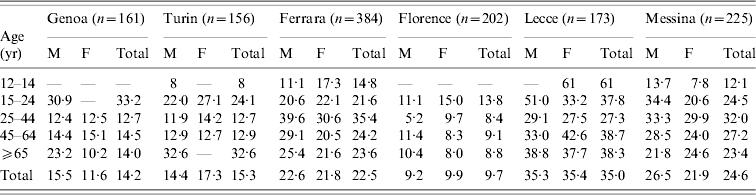
M, Males; F, females; —, sera not collected.
CMI
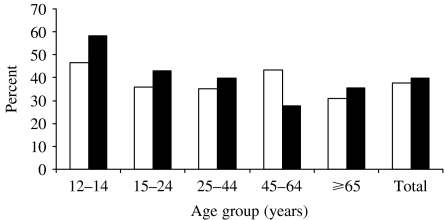
Positive CMI results (SI ⩾5) against PT, TT and PHA were recorded in 39·0%, 16·1% and 89·8% of samples, respectively (Fig. 5). The average SI of the positive samples was 21·0, 11·7 and 74·2 for PT, TT and PHA, respectively.
Fig. 5.
Percentage of subjects with a stimulation index value of ⩾5 against pertussis toxin (□; n=616), tetanus toxoid (■; n=596) and phytohaemagglutinin ( ; n=609).
; n=609).
After comparing the percentage of subjects with positive CMI data according to age, statistically significant differences were observed in the following age groups: 12–14 years vs. 25–44 years (χ2=5·31, P<0·05); 12–14 years vs. 45–64 years (χ2=5·38, P<0·05); 12–14 years vs. ⩾65 years (χ2=8·00, P<0·01). There were no significant differences between the genders in any age group (Fig. 6), but a significant difference was shown in the female population aged ⩾24 years (⩽24 years vs. ⩽24 and >24 years, χ2=4·89, P<0·05). The logistic regression model, used for the analysis of the CMI response in our sample, reveals a statistical trend in decreasing CMI with increasing age.
Fig. 6.
Percentage of subjects with a stimulation index value of ⩾5 against pertussis toxin, stratified by gender and age group (n=608). □, Males; ■, females.
Anamnestic analysis
Results of the anamnestic analysis are presented in Table 2. A total of 39% of subjects lived with children (no children, 59%; not determined, 2%), but this factor was not associated with significant differences in either the rate of IgG anti-PT positivity or of CMI against PT positivity. Similarly, no significant difference in humoral or CMI was shown on the basis of residential location (urban, 68·6%; rural, 22%; not determined, 9·4%).
Table 2.
Number and percentage of positive samples: IgG anti-PT (n=1301) and stimulation index against PT (n=616), stratified according to anamnestic data
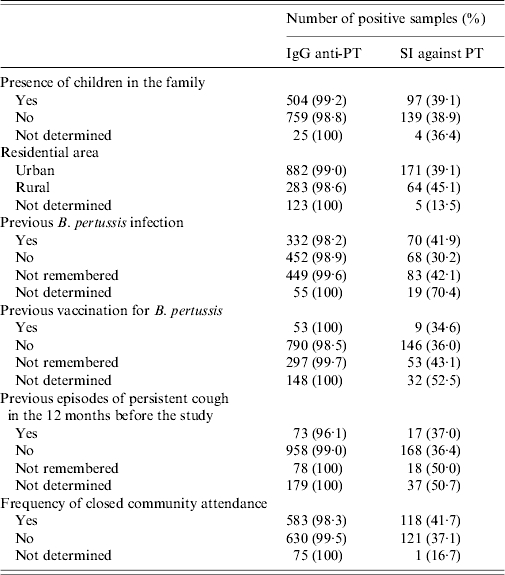
PT, Pertussis toxin; SI, stimulation index.
A previous B. pertussis infection was declared by 25·8% of subjects (35·1% had no previous infection, 34·7% could not remember, 4·2% no data available). Although no significant difference in humoral immunity was observed between these groups, a significant difference (P<0·05) was shown for CMI in subjects who had been infected vs. those who had not or could not remember (infection vs. no infection, χ2=5·75, P<0·05; no infection vs. infection not remembered, χ2=6·48, P<0·05).
Previous pertussis vaccination (4·1% previous vaccination, 61·7% no vaccination, 22·9% could not remember, 11·3% not determined) was not associated with any significant differences in humoral or CMI.
Anti-tetanus vaccination was declared by 59·8% of the enrolled subjects; 14·4% did not report any immunization (did not remember, 17·3%; not determined, 8·5%).
The majority of subjects (74·3%) did not report a persistent cough in the previous 12 months before the study (persistent cough, 5·9%; did not remember, 6·1%; not determined, 13·7%). A significant difference in humoral immunity was shown in those who had experienced a persistent cough compared with those who did not (cough vs. no cough, χ2=4·87, P<0·05). No other significant difference in the levels of humoral or CMI was observed.
Attendance at closed communities was declared by 45·6% of subjects (not declared, 48·6%; no information for one subject; data not available, 5·7%). A significant difference for humoral immunity was found for those who lived in a closed community vs. those who did not (χ2=4·29, P<0·05).
DISCUSSION
In Italy, pertussis is a mandatory notifiable disease and the epidemiological trend has shown important changes related to the introduction and use of pertussis vaccine. The average incidence rate fell from 38·4/100 000 in the period 1956–1959 to 12·4/100 000 in the period 1971–1974, as a consequence of vaccine introduction in 1961. However, from the mid-1970s until the end of the 1980s, there was an increase in the incidence rate (27·2/100 000 in the period 1986–1989) related to an insufficient vaccination coverage rate and wide differences among regions [28]. The introduction in 1994, of new acellular pertussis vaccines and the start of the pertussis project in 1996, together with the availability of combined vaccines for newborns, has greatly changed the national situation making vaccination more widespread (national vaccination coverage in 2003, 95%). [29].
Recent epidemiological studies performed in Italy have shown that despite a decrease in the total incidence rate, the number of cases in age groups 5–9 years and 10–14 years, and the average age of cases are increasing. Notably, no epidemic peak has been registered since 1998, probably reflecting the high vaccination coverage rate reached in the last few years [30].
The expected increase in the incidence of pertussis in adolescents and young adults poses a new problem as these subjects can become a reservoir of infection and contribute to the transmission of B. pertussis [31]. In adolescents, adults, and typically in vaccinated subjects, pertussis generally has an atypical clinical form, with episodes of parossistic cough for short periods, or simply episodes of persistent cough. In these cases, pertussis diagnosis is not routinely considered, and therefore it is difficult to acquire precise epidemiological data about the actual diffusion of B. pertussis in the different age groups in the population [32].
Despite the attainment and maintenance of high vaccination coverage in infants and young children, pertussis remains endemic in many countries and has re-emerged as an important public health problem. This observation supports the relatively short period of induced immunity following both natural infection and vaccination [33].
This polycentric study conducted in different geographical areas of Italy was performed in order to evaluate the humoral and CMI against B. pertussis in a sample of adolescent, adult, and senior subjects.
The analysis of demographic-anamnestic information collected from subjects participating in our study, allowed us to evaluate a number of variables which are known to be important for the epidemiological dynamics of B. pertussis infection. Despite incomplete data for many of the studied variables, due to unavailable anamnestic memory by the subjects or to non-registration, the information collected can nevertheless contribute to our understanding of the persistent circulation of the aetiological agent. Notably, 39% subjects lived with children, and 68·8% were urban residents. Persistent cough in the 12 months preceding the study was reported by 5·9% subjects and attendance at closed communities was present in 45·6% of the cases. A total of 25·8% subjects recalled a previous B. pertussis infection while only 4·1% had received pertussis vaccination. Stratification of this last criterion by age, indicates that vaccination is limited almost exclusively to subjects aged <24 years, and that in the past pertussis vaccination was not regularly administered and that coverage has only significantly increased over recent years. Data about pertussis vaccination can be usefully compared with that of tetanus immunization which, on the contrary, was reported by 59·8% of subjects.
With respect to the assessment of humoral immunity, specific IgG anti-PT antibodies were recorded in 99·1% of the examined samples. In 1988–1989, during a period of low vaccination coverage, the seroprevalence of IgG anti-PT in unvaccinated 19-year-old subjects was >80% [34], while in 1994–1995 a prevalence of 71·6% was recorded in students aged 17–25 years [21]. A more recent national study in 1996–1997 found a 77·6% prevalence of positive subjects to IgG anti-PT [30]. Thus, data collected in this study, even if higher, are in line with former studies and confirm the existence of immune priming in each studied age group. Nevertheless, it is important to remember that there is a non-uniform agreement about the existence of a serological marker of protection against B. pertussis [8] and this also represents a limit for seroepidemiological studies in evaluating the rate of susceptibility in the population. Some authors have assumed that high anti-PT antibody titres are indicative of a recent or ongoing infection [10, 35]. This hypothesis was supported by the group that undertook the European seroepidemiological study on vaccine-preventable diseases (ESEN) [25]. In this study 6·3% of samples had IgG anti-PT titres ⩾100 EU/ml and 13·0% had a titre between 50 EU/ml and 99 EU/ml; the overall average GMT approached 20 EU/ml. High antibody titres were recorded in 4% of subjects in the 1994–1995 study and in 4·7% of subjects in the 1996 research; the highest percentage of samples with high titres was recorded in subjects aged 7–11 months and 1 year, which relates to the high rates of vaccination in newborns. In the age groups up to 19 years, the percentage of samples with high titres remained stable at 5–7·9%, reflecting natural boosting and limited vaccination of the 5–9 years age group. The data from this study seem to confirm the circulation of B. pertussis in age groups not generally considered to be involved in the circulation of this pathogen, because of vaccination or natural immunity, and support previous reports in Italy and in other countries [36, 37].
The mechanism of the immune response to B. pertussis involves not only humoral, but also cellular-mediated pathways [23, 38–40]. According to some authors, the cell-mediated response persists longer than the humoral response and thus CMI can represent an important marker to assess priming against B. pertussis [16, 35]. In our study, a total of 39% of samples were CMI positive against PT (SI ⩾5). In general, the highest values of CMI-positive samples against PT were found in the 12–14 years and 15–24 years age groups (55·8% and 41·7%, respectively). The level of positivity decreased progressively in the subsequent age groups, and the differences were significant when compared with the relative value of subjects aged 12–14 years. In fact the CMI response decreases with increasing age.
The research performed in Italy in 1994–1995 showed a particularly high rate of CMI-positive subjects against PT (82%) in the 17–25 years age group [21], practically double that recorded in the present study in subjects aged 15–24 years (41·7%). The data from the old study may reflect the persistent and high circulation of the aetiological agent in a geographical area with low vaccination coverage. The results of our present research, taken with epidemiological surveillance data and trends in incidence rates, seem to indicate that during the last 10 years the great increase in vaccination coverage rates has contributed to reduce the spread of the aetiological agent, especially in the immunized population. It is known that whilst vaccination protects against disease, it also reduces the opportunity for natural recall of immunity. Indeed, the attainment and maintenance of high vaccination coverage rates increases susceptibility to infection of adolescents and adults, in whom the persistence of immune response to the disease has failed. Our data support the persistent circulation of the aetiological agent, albeit at decreased levels than in the past, in adolescent subjects, young adults and adults, in a country with a high childhood vaccination coverage rate.
In conclusion, this study seems to confirm that the epidemiology of pertussis in Italy is changing similarly to what has already occurred in other countries where high vaccination coverage rates have been achieved and maintained for many years [25].
In these countries, as an immunological consequence of vaccination, the number of back-susceptible adolescents, young adults, and adults is increasing due to the decay of immunity, no longer sustained by natural boosting. For these reasons, the use of booster vaccination in order to avoid the decay of immunity against pertussis has been proposed or adopted [15, 41]. Such active prophylactic intervention can be facilitated by using acellular pertussis vaccines, which can be used in subjects aged >7 years, and low antigen-content tetanus and diphtheria combination vaccines, that are suitable for adolescents and adults [42, 43].
If we wish to avoid the increasing average age of pertussis acquisition, it is essential to vaccinate adolescents with a booster dose of a reduced antigenic dosage vaccine, and possibly to also vaccinate specific groups of adults at risk of exposure or transmission (e.g. teachers, parents with young children, etc.) [44]. The possibility of using low dosage pertussis acellular vaccine to concomitantly boost against tetanus or diphtheria, as already recommended by many countries, including Italy [45], will permit optimum action against these three important infectious vaccine-preventable diseases.
ACKNOWLEDGEMENTS
This work was partly supported by an educational grant from GlaxoSmithKline SpA, Verona, Italy.
APPENDIX. Collaborative Group for the Study of Pertussis
Turin: S. Ditommaso, M. Gentile, G. Lanci. Genoa: P. Durando, L. Sticchi, A. Renzoni, P. Fuliano, G. Tripodi. Ferrara: A. Cavallaro. Florence: G. Pesavento, T. Silei Secchini, B. Innocenti. Messina: R. Squeri, V. La Fauci, S. Calimeri, D. Lo Giudice. Lecce: A. De Donno, M. Quattrocchi, F. Sanapo, G. C. Pasanisi. Palermo: S. Taormina, C. Bonura, C. Calà. CEBR Genoa: A. Ferrera.
DECLARATION OF INTEREST
F. Bamfi is employed by GSK Italy.
REFERENCES
- 1.Mortimer EA, Jr., Evans AS, Brachman PS. Bacterial Infections of Humans. 3rd edn. New York and London: Plenum Medical Book Co.; 1998. Pertussis; pp. 529–543. , pp. [Google Scholar]
- 2.Hewlett EL, Halperin SA. Serological correlates of immunity to Bordetella pertussis. Vaccine. 1998;16:1899–1900. doi: 10.1016/s0264-410x(98)00228-x. [DOI] [PubMed] [Google Scholar]
- 3.Locht C, Antoine R, Jacob-Dubuisson F. Bordetella pertussis, molecular pathogenesis under multiple aspects. Current Opinion in Microbiology. 2001;4:82–89. doi: 10.1016/s1369-5274(00)00169-7. [DOI] [PubMed] [Google Scholar]
- 4.Tamura M et al. Subunit structure of islet-activating protein, pertussis toxin, in conformity with the A-B model. Biochemistry. 1982;21:5516–5522. doi: 10.1021/bi00265a021. [DOI] [PubMed] [Google Scholar]
- 5.Ladant D, Ullmann A. Bordetella pertussis adenylate cyclase: a toxin with multiple talents. Trends in Microbiology. 1999;7:172–176. doi: 10.1016/s0966-842x(99)01468-7. [DOI] [PubMed] [Google Scholar]
- 6.Robbins JB, Pittman M, Davis BD, Dulbecco R, Eisen HN, Ginsberg HS. Microbiologia. 1998. Bordetella; pp. 638–641. , pp. [Google Scholar]
- 7.Cookson BT et al. Biological activities and chemical composition of purified tracheal cytotoxin of Bordetella pertussis. Infection and Immunity. 1989;57:2223–2229. doi: 10.1128/iai.57.7.2223-2229.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mills KHG. Immunity to Bordetella pertussis. Microbes and Infection. 2001;3:655–677. doi: 10.1016/s1286-4579(01)01421-6. [DOI] [PubMed] [Google Scholar]
- 9.Campins-Martì M et al. Recommendations are needed for adolescent and adult pertussis immunisation: rationale and strategies for consideration. Vaccine. 2001;20:641–646. doi: 10.1016/s0264-410x(01)00393-0. [DOI] [PubMed] [Google Scholar]
- 10.Wirsing von Konig CH, Halperin S, Riffelmann M, Guiso N. Pertussis of adults and infants. Lancet Infectious Diseases. 2002;2:744–750. doi: 10.1016/s1473-3099(02)00452-8. [DOI] [PubMed] [Google Scholar]
- 11.Nelson JD. The changing epidemiology of pertussis in young infants. The role of adults as reservoirs of infection. American Journal of Diseases of Children. 1978;132:371–373. doi: 10.1001/archpedi.1978.02120290043006. [DOI] [PubMed] [Google Scholar]
- 12.Mink CA, Sirota NM, Nugent S. Outbreak of pertussis in a fully immunized adolescent and adult population. Archives of Pediatrics & Adolescent Medicine. 1994;148:153–157. doi: 10.1001/archpedi.1994.02170020039006. [DOI] [PubMed] [Google Scholar]
- 13.Wirsing von Konig CHet al. Pertussis in adults: frequency of transmission after household exposure Lancet 19953461326–1329.. [Erratum in Lancet 1995; 346: 1502]. [DOI] [PubMed] [Google Scholar]
- 14.Senzilet LD et al. Sentinel Health Unit Surveillance System Pertussis Working Group. Pertussis is a frequent cause of prolonged cough illness in adults and adolescents. Clinical Infectious Diseases. 2001;32:1691–1697. doi: 10.1086/320754. [DOI] [PubMed] [Google Scholar]
- 15.Pastore Celentano L et al. Resurgence of pertussis in Europe. Pediatric Infectious Disease Journal. 2005;24:761–765. doi: 10.1097/01.inf.0000177282.53500.77. , on behalf of the EUVAC-NET Group. [DOI] [PubMed] [Google Scholar]
- 16.Edelman K et al. Immunity to pertussis 5 years after booster immunization during adolescence. Clinical Infectious Diseases. 2007;44:1271–1277. doi: 10.1086/514338. [DOI] [PubMed] [Google Scholar]
- 17.Preston A. Bordetella pertussis: the intersection of genomics and pathobiology. Canadian Medical Association Journal. 2005;173:55–62. doi: 10.1503/cmaj.050105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Storsaeter J et al. Levels of anti-pertussis antibodies related to protection after household exposure to Bordetella pertussis. Vaccine. 1998;16:1907–1916. doi: 10.1016/s0264-410x(98)00227-8. [DOI] [PubMed] [Google Scholar]
- 19.Cherry JD et al. A search for serologic correlates of immunity to Bordetella pertussis cough illnesses. Vaccine. 1998;16:1901–1906. doi: 10.1016/s0264-410x(98)00226-6. [DOI] [PubMed] [Google Scholar]
- 20.Olin P et al. How to make sense of pertussis immunogenicity data. Clinical Infectious Diseases. 2001;33:S288–S291. doi: 10.1086/322564. [DOI] [PubMed] [Google Scholar]
- 21.Rota MC et al. Prevalence of markers of exposure to Bordetella pertussis among Italian young adults. Clinical Infectious Diseases. 1998;26:297–302. doi: 10.1086/516293. [DOI] [PubMed] [Google Scholar]
- 22.Tran Minh NN et al. Cell-mediated immune responses to antigens of Bordetella pertussis and protection against pertussis in school children. Pediatric Infectious Disease Journal. 1999;18:366–370. doi: 10.1097/00006454-199904000-00012. [DOI] [PubMed] [Google Scholar]
- 23.Mattoo S, Cherry JD. Molecular pathogenesis, epidemiology and clinical manifestations of respiratory infections due to Bordetella pertussis and other Bordetella subspecies. Clinical Microbiology Reviews. 2005;18:326–382. doi: 10.1128/CMR.18.2.326-382.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Giammanco A et al. European Seroepidemiology Network: standardisation of the assay results for pertussis. Vaccine. 2003;22:112–120. doi: 10.1016/s0264-410x(03)00514-0. [DOI] [PubMed] [Google Scholar]
- 25.Pebody RG et al. The seroepidemiology of Bordetella pertussis infection in Western Europe. Epidemiology and Infection. 2005;133:159–171. doi: 10.1017/s0950268804003012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zuercher AW et al. Cellular immunity in healthy volunteers treated with an octavalent conjugate Pseudomonas aeruginosa vaccine. Clinical and Experimental Immunology. 2005;143:132–138. doi: 10.1111/j.1365-2249.2005.02964.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Disis ML et al. Maximizing the retention of antigen specific lymphocyte function after cryopreservation. Journal of Immunological Methods. 2006;308:13–18. doi: 10.1016/j.jim.2005.09.011. [DOI] [PubMed] [Google Scholar]
- 28.Binkin NJ et al. Epidemiology of pertussis in a developed country with low vaccination coverage: the Italian experience. Pediatric Infectious Disease Journal. 1992;11:653–661. [PubMed] [Google Scholar]
- 29.Ciofi degli Atti ML et al. Do changes in policy affect vaccine coverage levels? Results of a national study to evaluate childhood vaccination coverage and reasons for missed vaccination in Italy. Vaccine. 2004;22:4351–4357. doi: 10.1016/j.vaccine.2004.04.026. [DOI] [PubMed] [Google Scholar]
- 30.Rota MC et al. How increased pertussis vaccination coverage is changing the epidemiology of pertussis in Italy. Vaccine. 2005;23:5299–5305. doi: 10.1016/j.vaccine.2005.07.061. [DOI] [PubMed] [Google Scholar]
- 31.Purdy KW et al. Evaluation of strategies for use of acellular pertussis vaccine in adolescents and adults: a cost-benefit analysis. Clinical Infectious Diseases. 2004;39:20–28. doi: 10.1086/421091. [DOI] [PubMed] [Google Scholar]
- 32.Cherry JD. The epidemiology of pertussis: a comparison of the epidemiology of the disease pertussis with the epidemiology of Bordetella pertussis infection. Pediatrics. 2005;115:1422–1427. doi: 10.1542/peds.2004-2648. [DOI] [PubMed] [Google Scholar]
- 33.Le T et al. Immune responses and antibody decay after immunization of adolescents and adults with an acellular pertussis vaccine: the APERT study. Journal of Infectious Diseases. 2004;190:535–544. doi: 10.1086/422035. [DOI] [PubMed] [Google Scholar]
- 34.Giammanco A et al. Seroepidemiology of pertussis in Italy. Reviews of Infectious Diseases. 1991;13:1216–1220. doi: 10.1093/clinids/13.6.1216. [DOI] [PubMed] [Google Scholar]
- 35.De Melker H et al. Specificity and sensitivity of high levels of immunoglobulin G antibodies against pertussis toxin in a single serum sample for diagnosis of infection with Bordetella pertussis. Journal of Clinical Microbiology. 2000;38:800–806. doi: 10.1128/jcm.38.2.800-806.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Polyzou A et al. Seroepidemiology of Bordetella pertussis immune responses in a healthy population in Northern Greece. Journal of Clinical Laboratory Analysis. 2004;18:211–214. doi: 10.1002/jcla.20025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nardone A et al. Sero-epidemiology of Bordetella pertussis in England and Wales. Vaccine. 2004;22:1314–1319. doi: 10.1016/j.vaccine.2003.08.039. [DOI] [PubMed] [Google Scholar]
- 38.Mills KHG et al. A murine model in which protection correlates with pertussis vaccine efficacy in children reveals complementary roles for humoral and cell-mediated immunity in protection against Bordetella pertussis. Infection and Immunity. 1998;66:594–602. doi: 10.1128/iai.66.2.594-602.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Leef M et al. Protective immunity to Bordetella pertussis requires both B cells and CD4+ T cells for key functions other than specific antibody production. Journal of Experimental Medicine. 2000;191:1841–1852. doi: 10.1084/jem.191.11.1841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Edelman KJ et al. Pertussis-specific cell-mediated and humoral immunity in adolescents 3 years after booster immunization with acellular pertussis vaccine. Clinical Infectious Diseases. 2004;29:179–185. doi: 10.1086/421943. [DOI] [PubMed] [Google Scholar]
- 41.Forsyth KD et al. New pertussis vaccination strategies beyond infancy: recommendations by the Global Pertussis Initiative. Clinical Infectious Diseases. 2004;39:1802–1809. doi: 10.1086/426020. [DOI] [PubMed] [Google Scholar]
- 42.American Academy of Pediatrics. Committee on Infectious Diseases. Prevention of pertussis among adolescent: recommendations for use of Tetanus toxoid, reduced diphtheria toxoid and acellular pertussis (Tdap) vaccine. Pediatrics 2005 doi: 10.1542/peds.2005-3038. . Published online 28 December . . doi: [DOI] [PubMed] [Google Scholar]
- 43.American Academy of Pediatrics. Committee on Infectious Diseases. Recommended childhood and adolescent immunization schedule – United States, 2006. Pediatrics. 2006;117:239–240. doi: 10.1542/peds.2005-2790. [DOI] [PubMed] [Google Scholar]
- 44.Bamberger ES et al. What is new in pertussis? European Journal of Pediatrics 2007 doi: 10.1007/s00431-007-0548-2. . Published online: 1 August . . doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.State Regional Conference . Agreement between the central Government, Regions and Autonomous Provinces of Trento and Bolzano regarding the New National Vaccine Plan 2005–2007. Determination 3 March 2005 in conformity with the fourth paragraph of Decree no. 281, 28 August 1997Official Bulletin (Gazzetta Ufficiale), no. 86, 14 April 2005, Ordinary Supplement no. 63.