SUMMARY
The purpose of this study was to compare the occurrence of tuberculosis (TB) and the outcome of treatment between TB patients living in urban and rural areas. Cases of TB reported from 2001 to 2003 in England and Wales were assigned to a rural or urban area classification. The outcome of interest, non-completion of treatment, was investigated to determine the odds ratio for urban vs. rural residence. The effects of age, sex, ethnicity, place of birth, time since arrival in the United Kingdom, disease site, isoniazid resistance and previous diagnosis were adjusted for by multivariable logistic regression. Crude odds ratios showed a significantly higher level of treatment non-completion in rural areas. These results became non-significant (OR 1·02, 95% CI 0·83–1·26, P=0·82) after adjusting for the confounding effects of ethnic group and age. In England and Wales residence in a rural location is not an independent determinant of TB treatment outcome failure.
INTRODUCTION
The burden of disease in urban populations is generally considered to be greater than in rural populations. The evidence on quality of care, however, suggests that service accessibility is poorer in rural areas [1, 2]. While health services in urban settings may be within relatively easy reach, patients in rural areas often have to travel long distances. It is not known whether levels of access to tuberculosis (TB) services differ between urban and rural areas in the United Kingdom.
There are reasons why the outcome of care may be worse in urban or rural areas. Variation in the occurrence of TB between urban and rural areas has been reported from various countries [3, 4]. In the United Kingdom, TB is more common in urban areas [5]. The higher case load in urban areas may result in services based in cities generally having greater clinical experience in the management of TB when compared with rural services which may affect the overall quality of care available to patients in rural settings. In contrast, many TB patients in urban settings are from highly deprived communities. Social disadvantage in urban areas may contribute to a poorer outcome. This study was undertaken to determine whether a difference exists in treatment completion rates between urban and rural areas and to investigate the factors associated with any variation in outcome.
MATERIAL AND METHODS
Study subjects, definitions and data sources
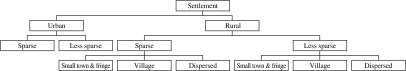
All patients reported to the national enhanced TB surveillance system from 2001 to 2003 in England and Wales were eligible for inclusion. TB cases include all patients whose diagnosis was confirmed by bacteriological culture or those who have clinical/radiological/histopathological features suggestive of TB and the clinician had taken the decision to treat the patient with a full course of anti-TB therapy. Outcome data were collected 12 months after the date of notification or start of treatment. Outcome was categorized as either treatment completed or treatment not completed. The ‘treatment not completed’ category includes patients whose reported outcome was death, lost to follow-up, transferred out, still on treatment, treatment stopped or ‘unknown’. The residential postcodes of all cases with an outcome reported were geo-coded. Cases were assigned to a rural or urban area based on the Rural and Urban Classification 2004 Office of National Statistics (ONS) (see Fig.). Data from the 2001 census were used to derive population denominator estimates for urban and rural areas.
Fig.
Office of National Statistics classification of urban and rural areas. (Source: Office of National Statistics.)
Patients with multidrug-resistant disease were excluded from the analysis because current treatment regimens recommend a course of therapy of at least 18 months for any patient with rifampicin resistance. Information on the treatment outcome of patients at 18 or 24 months is currently not collected by the national TB surveillance system.
Analysis
The relative risk of TB in urban compared to rural areas was determined. The outcome of interest, non-completion of treatment within 12 months of starting treatment or notification, was investigated by logistic regression to determine odds ratios for urban vs. rural residence. A multivariable model was fitted controlling for the effect of all factors significant in the univariable analysis. Bivariable analysis was used to sequentially examine the confounding effect of age, sex, ethnic group, place of birth/time since arrival in the United Kingdom, disease site, drug resistance and previous diagnosis.
RESULTS
A total of 19 836 cases were reported. Of these an outcome was reported on 16 784 (85%) patients. A residential postcode was available for 16 109 cases (96%) and they were mapped to a rural or an urban area. The median age of the population was 36 years (interquartile range 26–55 years). The majority of cases lived in urban areas (96·7%), were male (54·9%), of Indian, Pakistani, Bangladeshi (36·8%), or black African (21·5%) ethnicity and born outside the United Kingdom (68·5%).
The rate of TB in urban areas was 6·3-fold higher compared to rural areas. Forty-five per cent of cases living in rural areas did not complete treatment compared with 26% of cases in urban areas. Crude odds ratios [OR 1·72, 95% confidence interval (CI) 1·42–2·07, P<0·001] showed a significantly higher treatment non-completion level in rural areas compared to cases reported in urban areas.
Table 1 shows the results of univariable and multivariable logistic regression analysis. The effect was non-significant (OR 1·02, 95% CI 0·83–1·26, P=0·82) in the multivariable analysis after controlling for age, sex, ethnicity, time since arrival in the United Kingdom, disease site, isoniazid resistance and previous diagnosis. Bivariable analysis showed that ethnic group and age were the greatest effect modifiers with the urban–rural odds ratio declining to 1·18 (95% CI 0·97–1·44, P=0·09) when adjusting for ethnic group, 1·29 (95% CI 1·06–1·57, P=0·01) when adjusting for age and 1·07 (95% CI 0·88–1·31, P=0·49) when adjusting for both. Table 2 shows a breakdown of outcome categories for cases that have not completed treatment by urban–rural location. A large proportion of these cases die within 1 year of diagnosis in both urban and rural areas. There is also a larger proportion of cases in urban areas whose final outcome is not really known (such as lost to follow-up or transferred out) compared to those in rural areas.
Table 1.
Determinants of non-completion of treatment in cases reported in England and Wales in 2001–2003
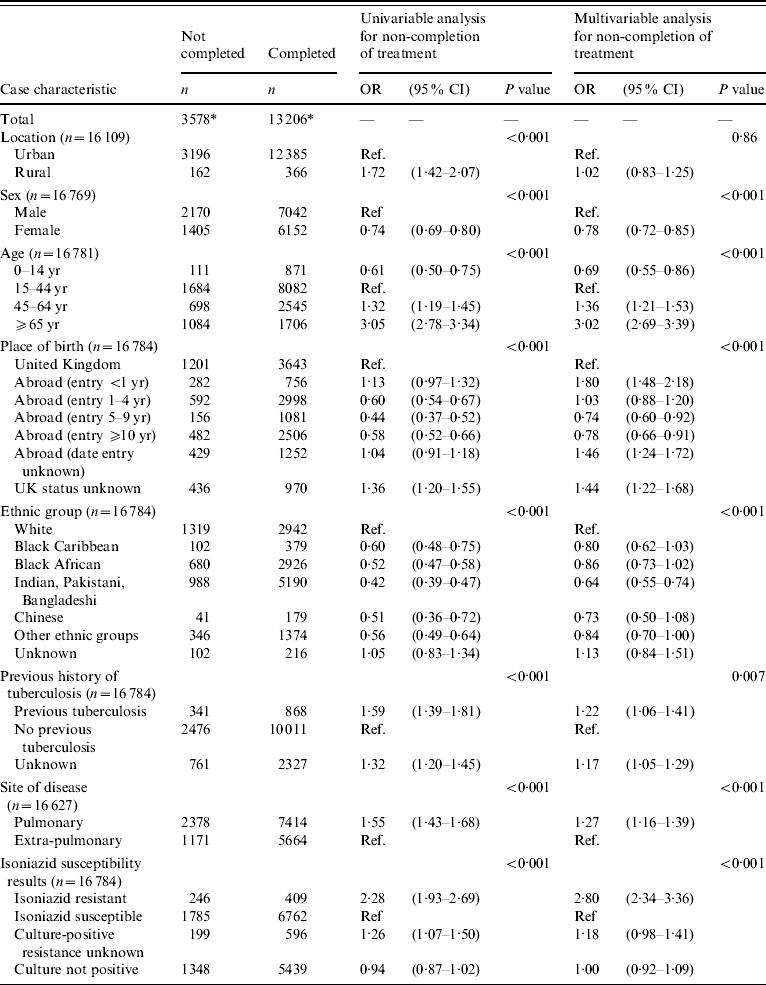
OR, Odds ratio; CI, confidence interval.
Note differences between totals (3578 and 13 206) and totals by case characteristics are due to missing information.
Table 2.
Reasons for non-completion of treatment for tuberculosis cases by urban or rural residence England and Wales, 2001–2003
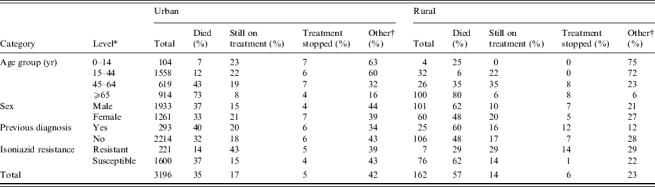
Excluding unknowns.
Other=Lost to follow up, transferred out or unknown.
DISCUSSION
TB is more common in urban compared to rural areas in England and Wales. This picture is similar to most low-incidence countries [6] and some high-incidence countries [3]. However, relatively higher incidence has been reported in rural populations in other high burden countries [4]. Our analysis shows that rural location is not an independent determinant of failure to complete TB treatment. The observed association in the univariable analysis was probably due to the confounding effects of age and ethnicity. Other factors known to predict non-completion of treatment such as isoniazid resistance and male gender were shown to be associated with poor outcome [7]. In addition, recent immigrants (<1 year since arrival) appear to have a lower treatment completion rate. This may be related to the higher proportion of such individuals being lost to follow-up or may reflect other differences in access to services.
Death is a common cause of treatment failure especially in the elderly white population living in rural areas. Mortality in many of these patients may be incidental to rather than the result of TB disease, partly explaining the confounding effect of age on the association. This contrasts with the higher proportion of young ethnic minority populations living in urban locations with lower mortality rates.
Previous studies have used place of residence and distance from treatment centre as a proxy measures of access to care [8–11]. Neither of these, however, may be an appropriate indicator. Access to care and treatment outcome is determined by a complex interplay of patient and health-provider-related factors including patient health belief model, significant others, language, socioeconomic status and availability of local health services [12].
These results should be interpreted with caution bearing in mind the following limitations. A number of potential confounding factors were examined and age and ethnic group found to explain the observed difference. The effect of deprivation requires further investigation in view of the known effects of socioeconomic disadvantage on TB treatment outcome. Homeless people in particular are known to experience poor treatment completion rates [7] and are more likely to be resident in a deprived urban setting. The collection of information on homelessness and other socioeconomic factors will improve understanding of the observed variations in treatment completion rates. Furthermore, information on changes in residence during therapy or duration of treatment was not available.
The information used for the analysis was derived from routine surveillance data. A proportion of cases, therefore, did not have an outcome reported and an assumption was made that the treatment completion rate in these patients is not different from the rate in those with an outcome reported. The proportion of patients without an outcome reported was 15%, suggesting that this may be a potential source of bias. Similarly, some cases had missing data on residential postcode and were assumed not to differ from those with information on location. Patients living in urban areas are more likely have complex social needs due to homelessness, imprisonment and problem drug use that have previously been associated with poor treatment outcome [7]. These characteristics could lower the likelihood of reporting residential postcode leading to a proportion of patients with an adverse outcome being excluded from the analysis. Residential postcode was, however, available for 96% of cases reducing the potential magnitude of this effect. In addition, despite the high prevalence of TB in socially complex groups, they only account for 17% of the overall proportion of reported TB patients in London [13].
Internationally there is some debate regarding the most appropriate classification of rural and urban residence [14]. The ONS classification which uses the size of settlements to classify areas was selected for this study because it is widely used, readily available, and applicable to the United Kingdom.
Living in a rural location is not an independent determinant of failure to complete TB treatment in England and Wales. Other factors such as the age of patients and ethnicity better explain the observed difference in outcome by place of residence. Further assessment of differences in outcome between hospitals comparing high TB burden and low-incidence areas and an investigation into the role of deprivation and drug resistance will improve our understanding of factors associated with outcome.
ACKNOWLEDGEMENTS
We acknowledge the contribution of TB nurses and clinicians who report cases to the enhanced surveillance system and the regional TB coordinators of the local and Regional Services of the HPA who collate the information. We are grateful to Chris Lane for geocoding the data and David Quinn for his work in maintaining the enhanced surveillance database.
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Watt IS, Franks AJ, Sheldon TA. Rural health and health care. British Medical Journal. 1993;306:1358–1359. doi: 10.1136/bmj.306.6889.1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reading R, Raybould S, Jarvis S. Deprivation, low birth weight, and children's height: a comparison between rural and urban areas. British Medical Journal. 1993;307:1458–1462. doi: 10.1136/bmj.307.6917.1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Banerjee A, Harries AD, Salaniponi FM. Differences in tuberculosis incidence rates in township and in rural populations in ntcheu district, Malawi. Transactions of the Royal Society of Tropical Medicine and Hygiene. 1999;93:392–393. doi: 10.1016/s0035-9203(99)90128-1. [DOI] [PubMed] [Google Scholar]
- 4.Vorokhobkin IS. Age sex related and social characteristics of patients with new-onset tuberculosis in urban and rural areas. Problem Tuberkuleza i Boleznei Legkikh. 2005;12:26–29. [PubMed] [Google Scholar]
- 5.Health Protection Agency Health Protection Agency; London: 2004. . Tuberculosis Section. Annual report on tuberculosis cases reported in 2001 in England, Wales and Northern Ireland. Communicable Disease Surveillance Centre, [Google Scholar]
- 6.Raviglione MC. The TB epidemic from 1992 to 2002. Tuberculosis. 2003;83:4–14. doi: 10.1016/s1472-9792(02)00071-9. [DOI] [PubMed] [Google Scholar]
- 7.Diel R, Niemann S. Outcome of tuberculosis treatment in hamburg: A survey, 1997–2001. International Journal of Tuberculosis and Lung Disease. 2003;7:124–131. [PubMed] [Google Scholar]
- 8.Liff JM, Chow WH, Greenberg RS. Rural-urban differences in stage at diagnosis. Possible relationship to cancer screening. Cancer. 1991;67:1454–1459. doi: 10.1002/1097-0142(19910301)67:5<1454::aid-cncr2820670533>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 9.Greenberg ER et al. Referral of lung cancer patients to university hospital cancer centers. A population-based study in two rural states. Cancer. 1988;62:1647–1652. doi: 10.1002/1097-0142(19881015)62:8<1647::aid-cncr2820620832>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 10.Campbell NC et al. Rural and urban differences in stage at diagnosis of colorectal and lung cancers. British Journal of Cancer. 2001;84:910–914. doi: 10.1054/bjoc.2000.1708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barker RD, Nthangeni ME, Millard FJ. Is the distance a patient lives from hospital a risk factor for death from tuberculosis in rural South Africa? International Journal of Tuberculosis and Lung Disease. 2002;6:98–103. [PubMed] [Google Scholar]
- 12.Goddard M, Smith P. Equity of access to health care services: theory and evidence from the UK. Social Science and Medicine. 2001;53:1149–1162. doi: 10.1016/s0277-9536(00)00415-9. [DOI] [PubMed] [Google Scholar]
- 13.Story A, Roberts W, Hayward A. Tuberculosis in London: results of the 2003 TB case load profile. International Journal of Tuberculosis and Lung Disease. 2004;8:S197. [Google Scholar]
- 14.Hall SA, Kaufman JS, Ricketts TC. Defining urban and rural areas in U.S. epidemiologic studies. Journal of Urban Health: Bulletin of the New York Academy of Medicine. 2006;83:162–175. doi: 10.1007/s11524-005-9016-3. [DOI] [PMC free article] [PubMed] [Google Scholar]